Baby not feeding after immunisations
Common reactions | Sharing Knowledge about Immunisation
Some children could feel a little unwell or unsettled for a day or two after they get their vaccinations. Most of the common reactions will last between 12 and 24 hours and then get better, with just a little bit of love and care from you at home.
If your baby doesn’t seem to be getting better, or you are worried about your baby, you can get help from:
Download
Local pain, redness and swelling
Some babies and children have a sore, red spot where the needle went in for a few days after they get their vaccinations. It can feel hot and it could be a bit swollen. Sometimes it feels itchy.
What to do at home
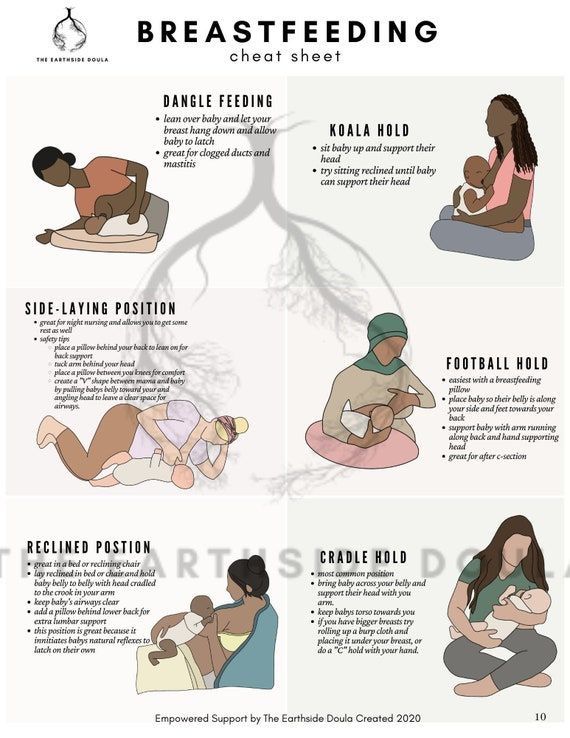
Putting a cool, damp cloth on the spot where the needle went in can help children feel more comfortable. Cuddling or breastfeeding really do relieve pain, too.
Download
Small, hard, painless bump (nodule)
Sometimes a small, hard, painless lump, also called a ‘nodule’, develops at the spot where the needle went in. The nodule may last for weeks or even months, but will eventually disappear on its own.
What to do at home
Nodules usually don't hurt and they usually go away after a few days or weeks without any treatment.
Loss of appetite
For a few days after a vaccination, some babies and children don't want to eat as much as they usually do.
What to do at home
Babies who aren't feeling well often want to breastfeed more often, and older babies sometimes refuse to eat solids for a day or two. Bottle-fed babies may prefer to have smaller bottles, more often than they usually do. Older babies and children may prefer to eat small meals throughout the day instead of at regular mealtimes.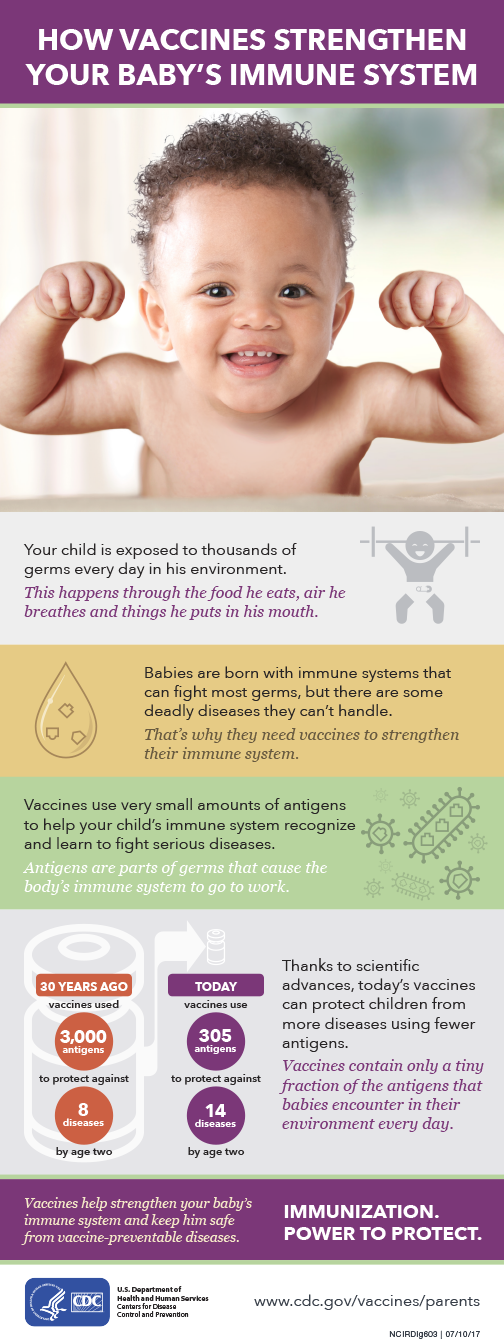 Reminding older children to drink water throughout the day will help them feel better, too.
Reminding older children to drink water throughout the day will help them feel better, too.
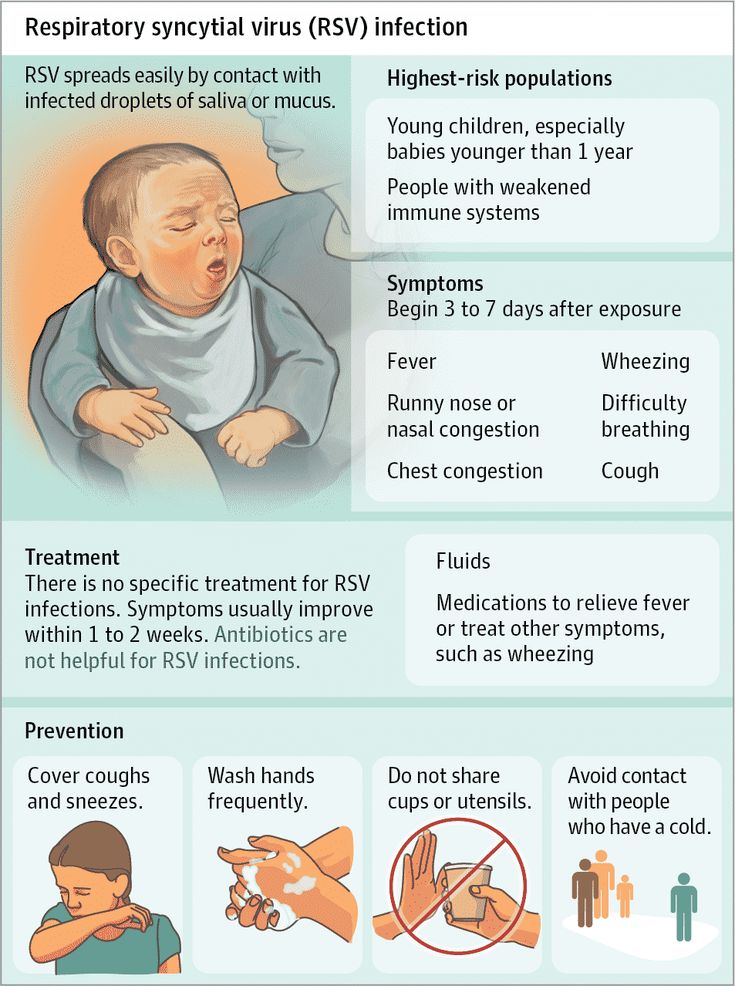
Fever
It is not unusual for babies and children to have a mild fever for a day or two after vaccination. A mild fever is a low-grade temperature of around 38.5C or less. Babies or children with a mild fever may be sweaty and warm to the touch and will sometimes look a bit red in the face. Some children can also develop fever 7-10 days after MMR or MMRV vaccine. In some children, fever can be high (>39.4°C). Fever on its own will not harm your child, but it can make them feel uncomfortable and unhappy.
What to do at home
If your baby or child has a fever, it helps to dress them in light (summer) clothes. Babies who aren't feeling well often want to breastfeed more often, and older babies sometimes refuse to eat solids for a day or two. Bottle-fed babies may prefer to have smaller bottles more often than they usually do. Reminding older children to drink water during the day, or offering crushed ice to suck, can help them feel a little better.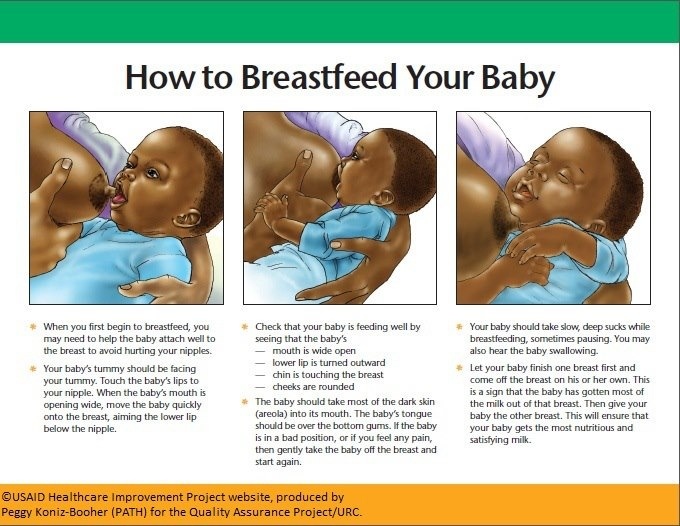 Holding your baby or child really does make them feel better, so if your child does have a mild fever plan for a few quiet, cuddly days if you can. Paracetamol (Panadol, Dymadon) can also help to ease a fever and relieve soreness. (Always follow the instructions on the packet.) Call your doctor if you feel like your child is getting worse, or if the fever lasts for more than three days.
Holding your baby or child really does make them feel better, so if your child does have a mild fever plan for a few quiet, cuddly days if you can. Paracetamol (Panadol, Dymadon) can also help to ease a fever and relieve soreness. (Always follow the instructions on the packet.) Call your doctor if you feel like your child is getting worse, or if the fever lasts for more than three days.
Grizzly or unsettled behaviour
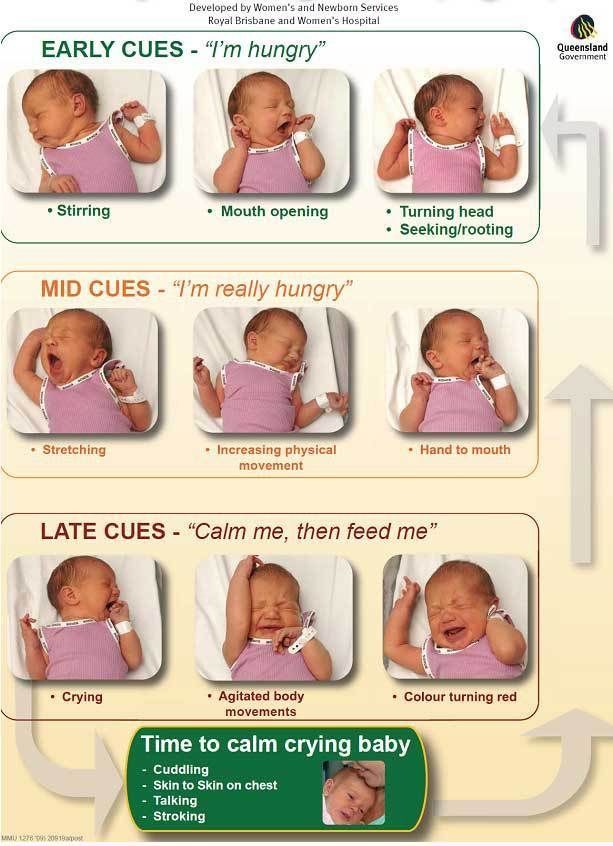
Even when they are not showing any particular symptoms, babies and children can feel a little unsettled and unhappy after vaccination.
What to do at home
Medical research has shown that cuddles actually trigger the release of pain-relieving hormones in children’s bodies1, so keep your child close and give them lots of extra cuddles.
Vomiting or diarrhoea
Babies who have had the rotavirus vaccine may develop vomiting and diarrhoea up to seven days after their vaccination.
What to do at home
Most babies recover within a few days.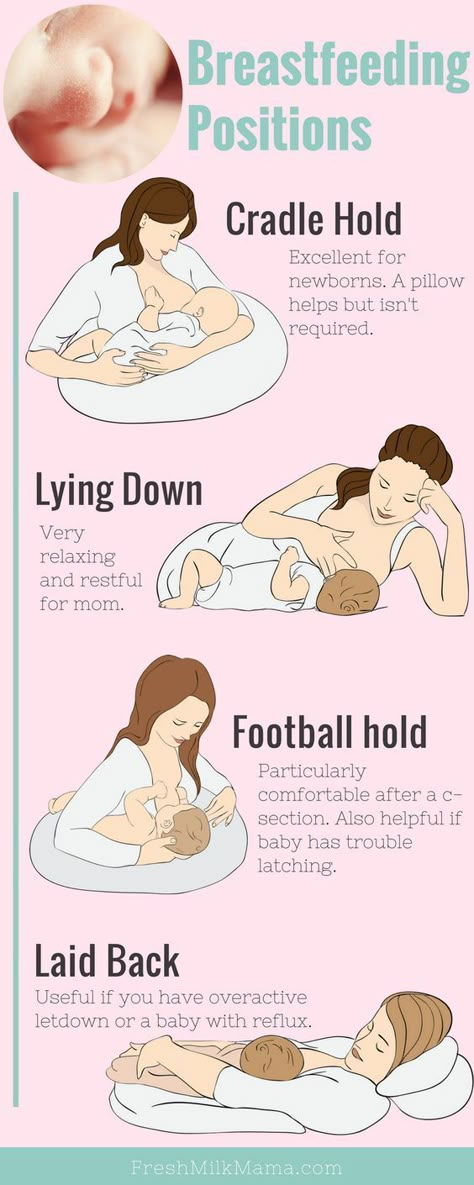 In the meantime, keep up breastfeeds or bottle feeds as normal, and offer additional clear fluids such as water. It is important for babies to keep on drinking fluids to make up for the fluids they lose through vomiting and diarrhoea. Dehydration can be dangerous for small babies.
In the meantime, keep up breastfeeds or bottle feeds as normal, and offer additional clear fluids such as water. It is important for babies to keep on drinking fluids to make up for the fluids they lose through vomiting and diarrhoea. Dehydration can be dangerous for small babies.
See a doctor if your baby is sick with vomiting and diarrhoea and you think they are not drinking enough, or if the vomiting and diarrhoea lasts for more than a few days without any sign of getting better.
Around 59 babies in every one million who get the rotavirus vaccine experience a blockage of the intestine called an ‘intussusception’2. The blockage gives babies strong bouts of pain in their abdomen which can make them look pale, weak and very sick. They may vomit. Babies who look pale and distressed and are drawing their legs up could have intussusception and should be taken to hospital quickly so they can get the help they need. Babies who are treated for intussusception usually don’t have any long-term health problems.
Faint rash
Some children develop a faint rash seven to ten days after they get the MMR vaccine which is given at 12 and 18 months.
What to do at home
The rash isn’t usually uncomfortable and is not infectious. It doesn’t need any treatment.
Red lumps or blisters
Around five to 26 days after they get the MMRV vaccine at 18 months of age, some children develop a few small red lumps and blisters (no more than five) that look like a mild form of chicken-pox, usually near the spot where the injection went in.
What to do at home
The rash isn’t usually uncomfortable and is not infectious. It doesn’t need any treatment.
What to do if baby stops breastfeeding after vaccination?
This is an automatically translated article.
Up to 90% of children have fever, fatigue leading to anorexia, even children stop breastfeeding after vaccination. What parents need to do when this is the case is to take care and supplement nutrition to stimulate the child's appetite.
1. Why do babies stop breastfeeding after vaccination?
The situation of children not eating after vaccination usually takes place in about 7-10 days. After this period, the child can eat and drink again. But in particular, there are some cases where the child does not want to eat for a long time or the child stops nursing and is fussy, affecting the health and development of the child.
According to experts, the reason why babies stop breastfeeding after vaccination may be because:
After vaccination, the child's immune system is responsible for recognizing, receiving the vaccine and creating antibodies to help the child fight against disease again. Therefore, when new vaccines enter the child's body, the immune system will have to work harder to "remember" them, causing the child to lose strength. This condition is manifested by fever, fatigue, diarrhea, loss of appetite... in children. For children with weak resistance, the immune system will work harder, making them feel tired and not want to eat anything.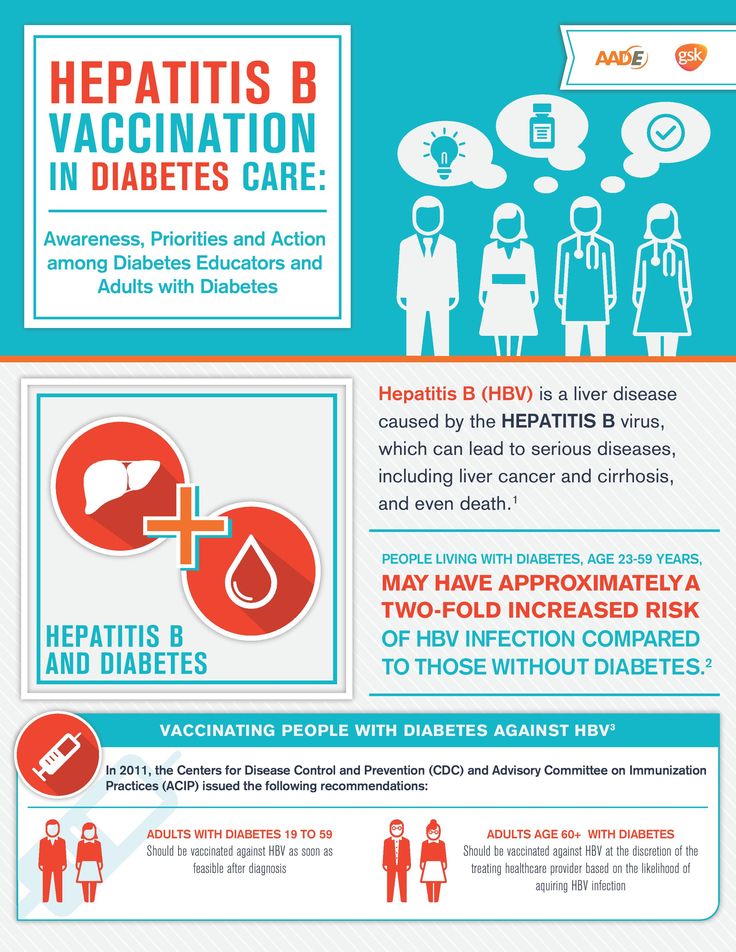 In addition, the situation that the child stops breastfeeding after receiving the injection may also be because the child is afraid of the injection and is tired of crying too much. For adults, vaccination just feels like an ant bite. However, for young children, most children are afraid and cry when they see the injection. Some children cry during the injection because of the pain and even when they go home the pain is still there. Not to mention the swelling at the injection site, causing pain, crying non-stop, leading to fatigue, so the child stopped feeding.
In addition, the situation that the child stops breastfeeding after receiving the injection may also be because the child is afraid of the injection and is tired of crying too much. For adults, vaccination just feels like an ant bite. However, for young children, most children are afraid and cry when they see the injection. Some children cry during the injection because of the pain and even when they go home the pain is still there. Not to mention the swelling at the injection site, causing pain, crying non-stop, leading to fatigue, so the child stopped feeding.
Trẻ bỏ ăn sau khi tiêm phòng thường chỉ diễn ra trong khoảng từ 7 – 10 ngày
2. Consequences of children refusing to breastfeed after vaccination
If it is not a chronic anorexia, the state of children who stop breastfeeding after vaccination is only temporary and will go away after 7-10 days. However, if after this time the child is still anorexic, you should not be subjective, you need to intervene immediately to avoid the following consequences:
Children lose weight rapidly, pale skin, fatigue because the child's body does not accept Get enough important nutrients from food.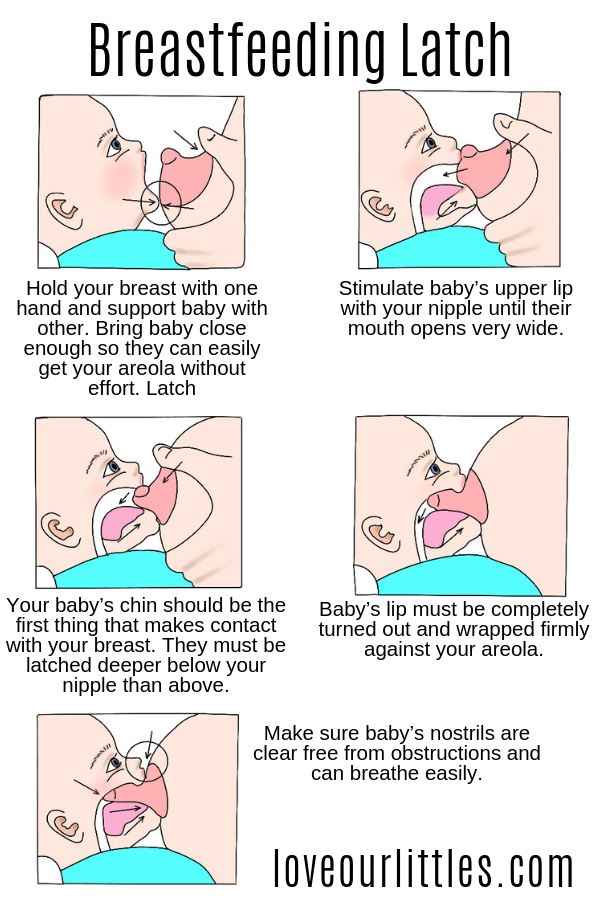 Anorexia after vaccination of children will become chronic anorexia if you do not have timely solutions to prevent children from constantly refusing to eat. Children are afraid of eating and are afraid of vaccinations, as a result, you will have a harder time in the future when taking your child for vaccinations and feeding them. Note, if the child stops breastfeeding after vaccination with fever, fussiness, you need to closely monitor and take the child to see a doctor immediately if the fever does not subside or the child refuses to eat or drink.
Anorexia after vaccination of children will become chronic anorexia if you do not have timely solutions to prevent children from constantly refusing to eat. Children are afraid of eating and are afraid of vaccinations, as a result, you will have a harder time in the future when taking your child for vaccinations and feeding them. Note, if the child stops breastfeeding after vaccination with fever, fussiness, you need to closely monitor and take the child to see a doctor immediately if the fever does not subside or the child refuses to eat or drink.
Tình trạng trẻ tiêm xong bỏ bú còn có thể do trẻ sợ tiêm và mệt mỏi vì khóc quá nhiều
3. How to reverse anorexia in children after vaccination?
Care and nutritional supplementation for children before and after vaccination is very necessary, because it helps children stay healthy and respond well to vaccines. Accordingly, in order to prevent children from skipping meals after vaccination, you should:
Prepare liquid and soft foods such as porridge, soup. .. for easy absorption by children, helping children's eating take place quickly. than. Give your child a variety of foods, especially foods they like to stimulate their appetite. Note, you should increase the amount of vitamins and minerals (found in green vegetables, fruits and tubers) in your child's daily menu to support absorption. Do not force your child to eat by any means, because doing so can backfire and make the child even more afraid to eat. Instead, you can give your child milk, eat extra snacks such as cheese, yogurt, smoothies... to make up for the amount of nutrients your child doesn't get enough in the main meals. Most children will feel tired after vaccination and eat very little or not want to eat. Therefore, you should divide the meals to ensure that the child is still provided with adequate nutrition after vaccination. Otherwise, the child's weight gain or weight loss is certain to occur. In addition, you can add probiotics and some micronutrients such as B vitamins, zinc, lysine.
.. for easy absorption by children, helping children's eating take place quickly. than. Give your child a variety of foods, especially foods they like to stimulate their appetite. Note, you should increase the amount of vitamins and minerals (found in green vegetables, fruits and tubers) in your child's daily menu to support absorption. Do not force your child to eat by any means, because doing so can backfire and make the child even more afraid to eat. Instead, you can give your child milk, eat extra snacks such as cheese, yogurt, smoothies... to make up for the amount of nutrients your child doesn't get enough in the main meals. Most children will feel tired after vaccination and eat very little or not want to eat. Therefore, you should divide the meals to ensure that the child is still provided with adequate nutrition after vaccination. Otherwise, the child's weight gain or weight loss is certain to occur. In addition, you can add probiotics and some micronutrients such as B vitamins, zinc, lysine. .. in 1-2 weeks after vaccination to stimulate appetite in children. In short, the situation of children refusing to eat after vaccination is quite common, but it is only temporary and will go away after 7-10 days. If after this period of time the child is still anorexic, you should not be subjective, consult a doctor to avoid affecting the health of the child.
.. in 1-2 weeks after vaccination to stimulate appetite in children. In short, the situation of children refusing to eat after vaccination is quite common, but it is only temporary and will go away after 7-10 days. If after this period of time the child is still anorexic, you should not be subjective, consult a doctor to avoid affecting the health of the child.
Please dial HOTLINE for more information or register for an appointment HERE. Download MyVinmec app to make appointments faster and receive 15% off for consultation fee at the first appointment (applied from 17th October to 31th December, 2022). MyVinmec app is also available and convenient for your bookings management and Telehealth service with Vinmec doctors all in one.
XEM THÊM:
- 7 causes of anorexia in children and ways to prevent them
- When should the baby eat porridge?
- Emergency treatment in severely malnourished children
Tags: Biếng ăn Dinh dưỡng cho trẻ Trẻ tiêm xong bỏ bú Dinh dưỡng sau tiêm phòng Trẻ bỏ ăn sau tiêm phòng Nhi
Do's and don'ts before and after vaccination
Vaccination is an important step in a child's life and a serious test for parents.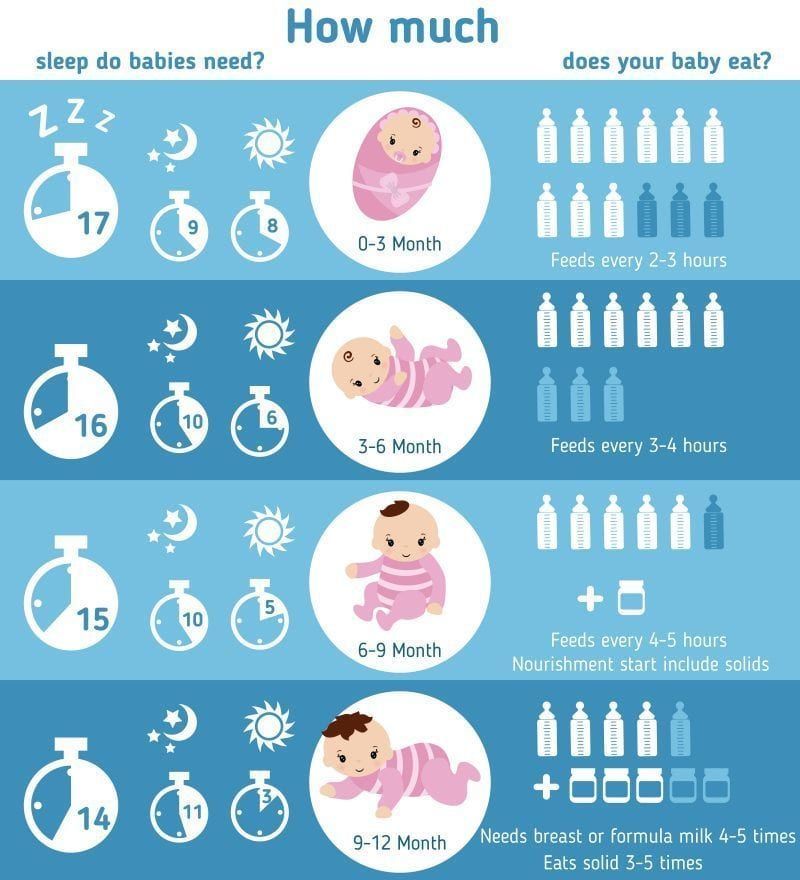 There are many myths that not only complicate caring for a child before and after vaccination, but also divert parents' attention from the really important moments associated with vaccinations.
There are many myths that not only complicate caring for a child before and after vaccination, but also divert parents' attention from the really important moments associated with vaccinations.
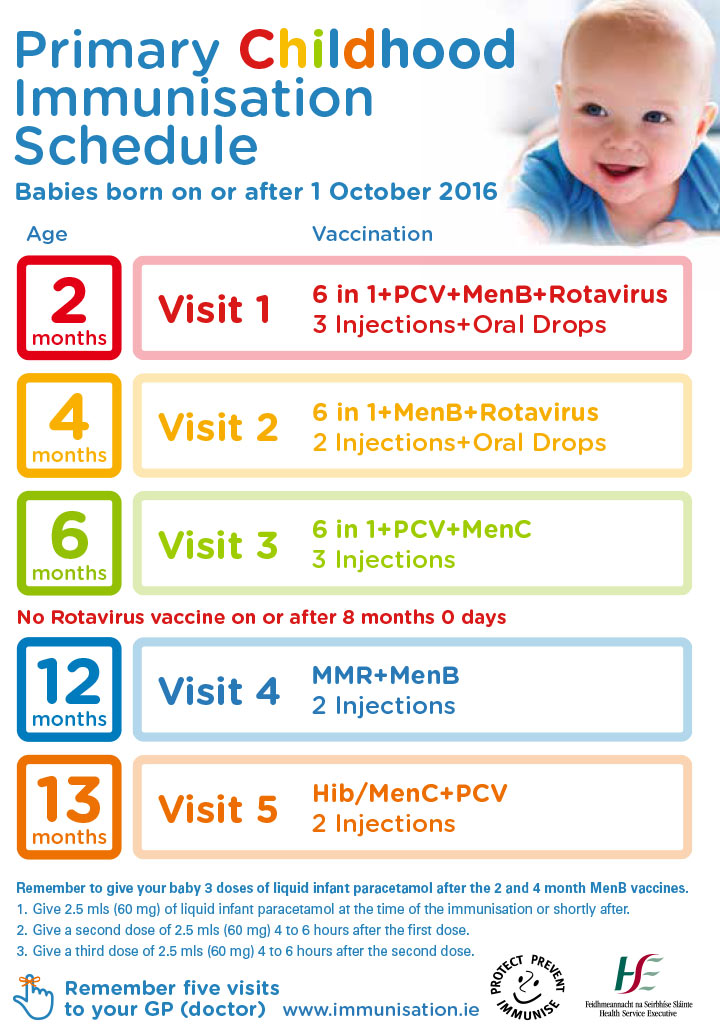
Before vaccination
Taking into account the fact that in the vast majority of cases, vaccinations are well tolerated by healthy children without any preparation and prior treatment, the most important point in preparing a child for vaccination is to determine the contraindications to vaccination, that is those cases of illness in a child in which the vaccine can cause serious adverse reactions. Contraindications and precautions for vaccination, in some cases, vaccination in children is either strictly prohibited or should be postponed to a later date. In order to correctly assess the contraindications and precautions for vaccinating a child, it is important to follow the vaccination calendar and know in advance which vaccination should be given to the child and when. Before you vaccinate your child and on the day of vaccination, read what contraindications and precautions are associated with the introduction of a particular vaccination and make sure that the child does not have any contraindications for vaccination.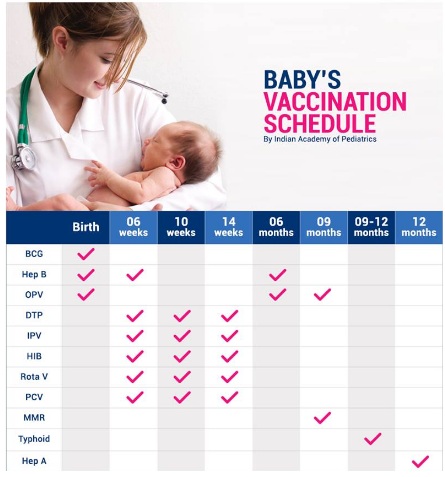 If you find it difficult to determine some contraindications or precautions (for example, how dangerous a cold or cough is in a child), show it to a doctor. Blindly refusing to vaccinate due to a slight runny nose or cough should not be - this will only derail the vaccination plan.
If you find it difficult to determine some contraindications or precautions (for example, how dangerous a cold or cough is in a child), show it to a doctor. Blindly refusing to vaccinate due to a slight runny nose or cough should not be - this will only derail the vaccination plan.
Preparing a child for vaccination The necessary preparation of a child for vaccination is usually much easier than is commonly believed. If the child is breastfed, it is better for the mother to refuse new foods and eat as usual. This will help avoid allergic reactions that could be confused with the effect of the vaccine. Prophylactic use of antihistamines and antipyretics Taking antihistamines (for example, Suprastin) the day before vaccination is recommended only in the case of children suffering from various manifestations of allergies (urticaria, atopic dermatitis, asthma), or in whom the previous dose of vaccination caused severe swelling, redness and pain at the injection site. The appointment of antihistamines to the child should be discussed with the doctor.
 In order for preventive treatment to be effective, it is important to choose the right dose of medication, depending on the strength of the allergy and the body weight of the child. Prophylactic use of antipyretics is not recommended. The only exceptions are children prone to febrile convulsions, who should be given an antipyretic immediately before vaccination or immediately after vaccination. Before you go for a vaccination, make sure that you have the medicines at home (Paracetamol in suppositories or in syrup at a dosage appropriate for the age of the child and Suprastin).
In order for preventive treatment to be effective, it is important to choose the right dose of medication, depending on the strength of the allergy and the body weight of the child. Prophylactic use of antipyretics is not recommended. The only exceptions are children prone to febrile convulsions, who should be given an antipyretic immediately before vaccination or immediately after vaccination. Before you go for a vaccination, make sure that you have the medicines at home (Paracetamol in suppositories or in syrup at a dosage appropriate for the age of the child and Suprastin). Immediately before vaccination
Immediately before vaccination, ask the doctor about what vaccination or vaccinations the child will receive and what adverse reactions may occur after such a vaccination and what should be done about them.
At the time of vaccination and immediately after vaccination
At the time of vaccination, try to hold the child and calm him down after the injection.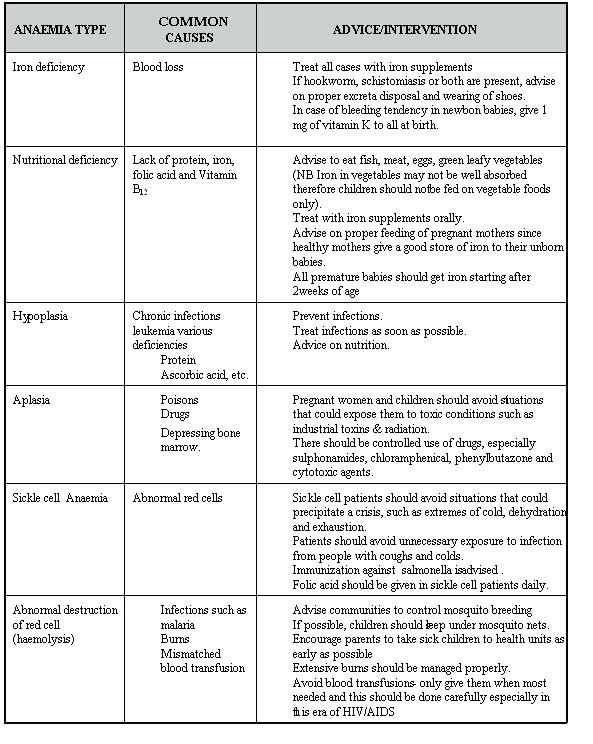 Usually, infants quickly calm down if they are breastfed (after a live oral polio vaccination, the child cannot be fed or watered for an hour), and older children if they are offered a toy (it is better to stock up on a toy from home).
Usually, infants quickly calm down if they are breastfed (after a live oral polio vaccination, the child cannot be fed or watered for an hour), and older children if they are offered a toy (it is better to stock up on a toy from home).
Immediately after vaccination
Immediately after vaccination, do not rush to leave the clinic. If the doctor did not offer you, you should, on your own initiative, stay in the clinic for another 10-15 minutes. This precaution is associated with the risk of collapse or severe allergic reactions to the vaccine (anaphylactic shock). Despite the fact that such reactions occur extremely rarely, the possibility of their development should always be borne in mind.
Child care in the following days after vaccination Child care after vaccination is as follows
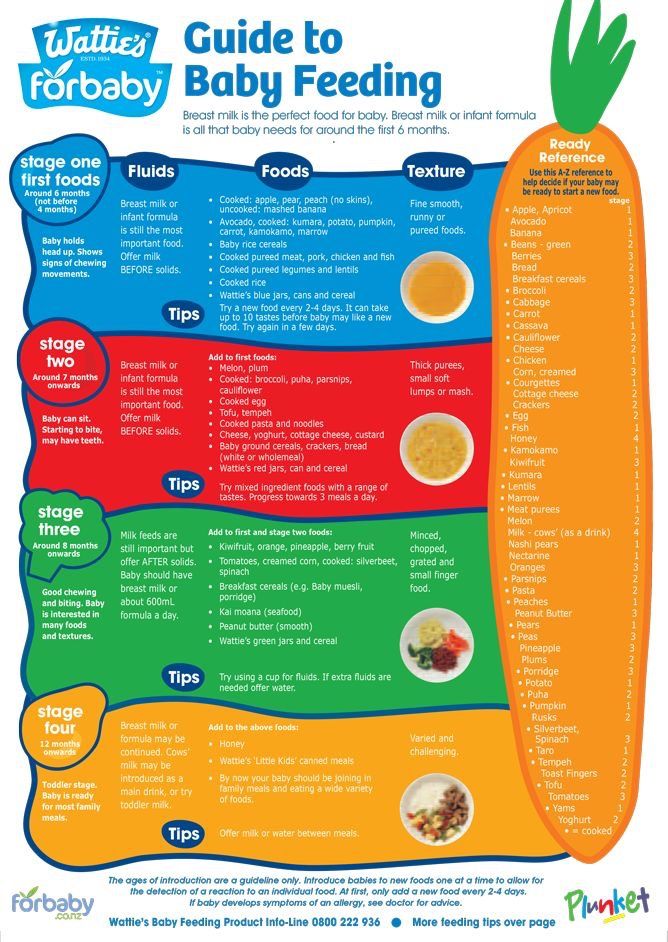
Feeding the child after vaccination For several days after vaccination, you should refrain from introducing new foods into the diet of a child or a nursing mother.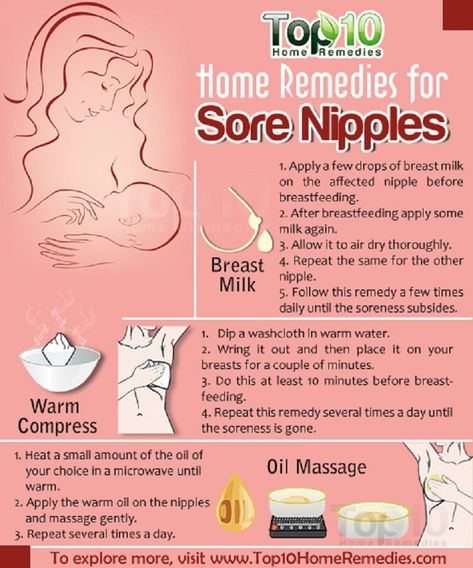 After vaccination, especially if the child has a fever, diarrhea or vomiting, make sure that the child receives enough fluids. Do not worry if your child does not have an appetite for 2-3 days after vaccination.
After vaccination, especially if the child has a fever, diarrhea or vomiting, make sure that the child receives enough fluids. Do not worry if your child does not have an appetite for 2-3 days after vaccination.
Treatment of fever and prevention of allergies after vaccination
Fever is a normal reaction of the child's body to the vaccine, which means that the immune system has reacted to the vaccine and begins to develop immunity (however, the absence of a fever after vaccination does not mean that the vaccine was ineffective) . In the case of perfectly healthy children, the temperature should not be brought down after vaccination if it does not exceed 38.5 ° C. In cases of a more significant increase in temperature, and also when the temperature is kept at 38.5 C in the evening, the child should be given an antipyretic. For the treatment of fever after vaccination, it is recommended to use Paracetamol. Aspirin should never be used as an antipyretic in children.
In the case of children with a tendency to febrile convulsions, treat the temperature above 37.5 or give the child an antipyretic until the temperature appears, if so advised by the neurologist observing the child.
Prevention of allergic reactions after vaccination is indicated only in the case of children prone to developing allergies. In such cases, it is recommended to use Suprastin or another antihistamine medicine as prescribed by a doctor.
Treatment of redness and swelling at the injection site
Most vaccinations result in more or less redness or swelling at the injection site. The most burned local reaction to the introduction of the vaccine is observed in the case of DPT (redness, swelling and soreness at the injection site) and BCG (formation of a long non-healing sore). In the case of all types of vaccinations, it is recommended to refrain from any local treatment of redness or swelling at the injection site. If the child scratches the injection site, it can be covered with a light gauze bandage. In place of DTP, a seal is often formed, located in the depths of the muscle - a “bump”. Often such a seal is painful, and the child easily limps on one leg (if the vaccine was injected into the thigh). The formation of a dense "bump" after DPT is considered a normal reaction and does not require any treatment. Within a few weeks, the bump resolves on its own.
In place of DTP, a seal is often formed, located in the depths of the muscle - a “bump”. Often such a seal is painful, and the child easily limps on one leg (if the vaccine was injected into the thigh). The formation of a dense "bump" after DPT is considered a normal reaction and does not require any treatment. Within a few weeks, the bump resolves on its own.
Is it possible to bathe a child after vaccination?
If after vaccination the child does not have a fever, he can be bathed, without any fear to wet the vaccination. The vaccination site, however, is best not to rub with a washcloth. The only exception is the Mantoux test (this is not a vaccination), which cannot be wetted or rubbed before reading the results.
Is it possible to walk with a child after vaccination?
Vaccination is not a contraindication for walking and playing outside. Walking after vaccinations is perfectly safe if the child does not have a fever and feels well.
Diarrhea and vomiting after vaccination
Due to the high sensitivity of the autonomic nervous system of children to any irritants, individual episodes of vomiting or short episodes of diarrhea are often observed after vaccination.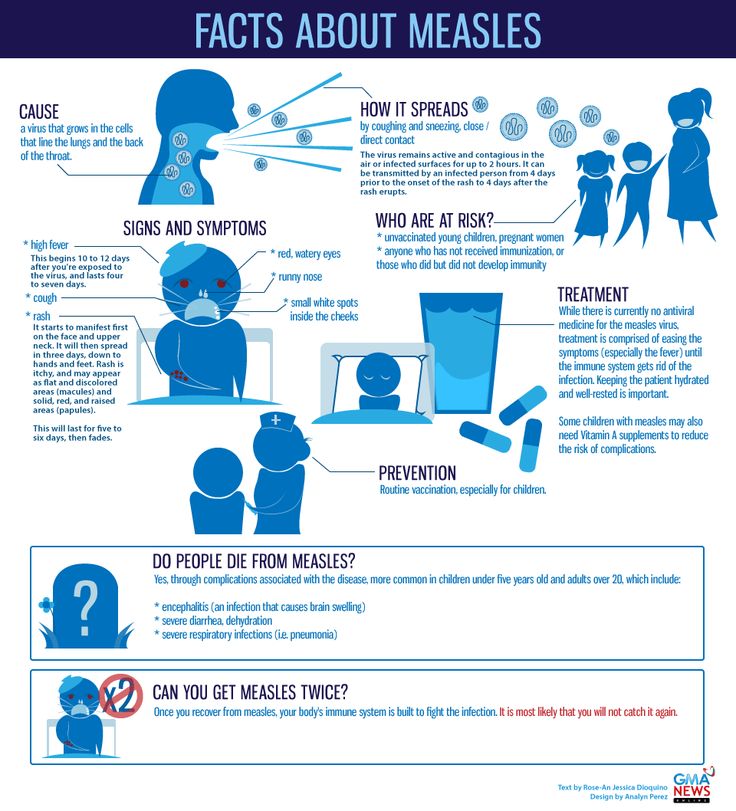 Neither single vomiting nor short-term diarrhea should be cause for concern and require no special treatment.
Neither single vomiting nor short-term diarrhea should be cause for concern and require no special treatment.
Advice for parents on vaccination of children (what to do before, during and after vaccination)
What to do before vaccination
Before vaccination
- Before the first vaccination with DTP vaccine, you must do a complete blood and urine test, and also obtain permission from a neurologist for vaccination.
- If the child has allergic disorders (diathesis, etc.), discuss with the doctor in advance the scheme for the prevention of allergy exacerbation . Usually it is taking antihistamines (suprastin, fenistil) for 2 days before vaccination and 2 days after.
- If you haven't already, buy Children's Antipyretics with Paracetamol. It is better to buy candles, since the flavorings in syrups themselves can cause adverse reactions. Buy analgin.
On the day of vaccination
- Do not introduce new complementary foods or new foods .
 If the baby is breastfed, do not introduce new foods into your diet.
If the baby is breastfed, do not introduce new foods into your diet. - Be sure to take your antihistamines and other medicines prescribed by your doctor.
- Make sure you have analgin at home (especially in the case of DTP vaccines) and children's suppositories with paracetamol (efferalgan, panadol). Do not rely solely on homeopathic remedies - they can be used, but they will not help with severe reactions to vaccinations.
- If the child is old enough - never, even jokingly scare the child with the vaccine.
- If the child asks about the injection, be honest, say that it may be a little painful, but it's only for a few seconds.
Before leaving home
- If you have a vaccination certificate that records your vaccinations, please take it with you.
- Be sure to bring your favorite toy or baby's diaper.
At the time of vaccination
Just before vaccination
- Check with the doctor that the child does not have a fever at the time of vaccination.
 This is the only universal contraindication to vaccination.
This is the only universal contraindication to vaccination. - Ask the doctor what and what kind of vaccine the child will be vaccinated against today.
- Do not hesitate to ask your doctor if you have any doubts about vaccination.
At the time of injection
- Don't worry . Your excitement and anxiety are transferred to the child. Be calm and confident - and the child will tolerate the vaccine much easier.
- Do not worry about the fact that you are still worried, just translate your excitement into a constructive channel.
- In order to distract the child (and yourself) - communicate with him, play, sing songs, look at interior items, play with a toy taken from home.
- Smile and be kind to your child.
- During the injection, the child should be in your arms - so he and you will be more comfortable.
- Let the child cry after the injection.
 Do not force the child to "be brave", do not say that it is shameful to cry.
Do not force the child to "be brave", do not say that it is shameful to cry. - If a child says that he is in pain, “blow out” the pain. Take a deep breath and slowly "blow out" the pain. Repeat this exercise several times.
. Be sure to ask about what and when reactions to the vaccine may occur and when to seek medical help.
When you return home after vaccination
- If you have been vaccinated with DPT vaccine: unless otherwise instructed by your doctor, give your child a dose (candle or syrup) of an antipyretic.
 This will avoid unpleasant reactions that occur in the first hours after vaccination.
This will avoid unpleasant reactions that occur in the first hours after vaccination. - If the child does not have a temperature, you can swim as usual. The presence of reactions at the injection site is not a contraindication to bathing, and even vice versa.
First night after vaccination
- Most often, temperature reactions to inactivated vaccines (DTP and others) occur on the first day after vaccination.
- In the case of DTP vaccines: prophylactically, be sure to give the child antipyretic at night, even if the temperature is currently normal. Keep analgin on hand.
- If severe temperature reactions occur (38.5°C or more), give a single dose of to the child one quarter of a 0.5 g analgin tablet. In children older than 2 years, the dose can be increased to one third of the same tablet.
- In case of temperature reactions, do not neglect wiping the child with warm water. Do not use vodka for rubdowns - it irritates and dries baby skin.

- Do not forget that the daily dosage of paracetamol is not unlimited . In case of overdose, severe complications are possible. Carefully read the instructions for the drug you are using (Panadol, Efferalgan, Tylenol).
- Never use aspirin . Its use in young children is fraught with serious complications.
First two days after vaccination
(DPT, DPT, hepatitis B, Hib vaccine, IPV)
- Take whatever medicine your doctor has prescribed to prevent allergic disorders.
- Continue taking your antipyretics as directed if your fever remains elevated.
- DTP vaccines. Monitor the child's body temperature . Try not to raise it above 38.5 ° C (under the arm). In some children, against the background of an increase in temperature, the appearance of the so-called. febrile seizures. Take antipyretics without waiting for the temperature to rise.
- You can and should walk with a child, you can and should bathe him.
 The exception is when the child has a fever due to or regardless of vaccination.
The exception is when the child has a fever due to or regardless of vaccination. - If a Mantoux test has been performed, when bathing, try not to get water on the test site. Remember that sweat is also a liquid, so be careful not to sweat your child's hand.
- Do not introduce new foods into your baby's diet (or yours if the baby is breastfeeding). This can be done on the 3rd day after vaccination and later.
- In the case of DTP, DTP, hepatitis B and ATP-M vaccines. If there are strong reactions at the injection site (swelling, induration, redness), make a warm compress or simply periodically apply a cloth moistened with water. If anti-inflammatory drugs are not yet taken, start giving them.
5-12 days after vaccination
- In the case of vaccination with live vaccines (polio OPV drops, measles, mumps, rubella), adverse reactions usually occur 5-12 days after vaccination.
- If there was any reaction, but the vaccination was not made with a live vaccine, then vaccination with a 99% probability has nothing to do with it.