Baby spitting milk out while feeding
Bottle-feeding problems and solutions | From Tiny Tot to Toddler
Babies can sometimes have trouble feeding. Usually, the problem is temporary. The first thing to do is observe your baby. Try to get a feel for her temperament as well as her feeding and sleeping routine.
Your baby sleeps a lot
If your baby sleeps a lot, you probably wonder whether you should wake her to feed. Knowing what’s best isn’t always easy. You can follow her routine and let her sleep if she
- Wakes up on her own to feed
- Is an active and effective feeder
- Pees at least 6 times and passes at least 3 stools a day
- Is calm and seems satisfied after feeding
- Has regained her birth weight and continues to put on weight
In this case, there is nothing to worry about. Babies each have their own routine that develops over time.
You may need to wake your baby up to feed her if she sleeps a lot.
Photo: Marie-Ève Bolduc
Some babies sleep so much they may skip some feedings, especially during the first 2 to 3 weeks. This means they will have a hard time getting all the milk they need. If your baby sleeps a lot and doesn’t show the signs described above, you need to stimulate her to drink more.
What to do?
- Keep an eye out for signs that she’s sleeping lightly (she’s moving, making sucking motions, or moving her eyes beneath her eyelids) when it will be easier to wake her up.
- Stimulate her: talk to her, massage her back, legs, arms, etc.
- Leave her in an undershirt or diaper: babies drink less when they are warm.
- See a professional if you’re worried or see no improvement after a few days.
Your baby drinks very slowly
Babies can’t always suck effectively at the start. This is more common among babies who were born a few weeks prematurely (between 35 and 37 weeks of pregnancy). Even full-term babies may need a few days or weeks to get the hang of things. This situation usually improves with time. Be patient: your baby is learning. Some babies, however, will continue to drink slowly even as they get older.
This situation usually improves with time. Be patient: your baby is learning. Some babies, however, will continue to drink slowly even as they get older.
What to do?
- Change to a faster nipple.
- Stimulate your baby as she feeds by rubbing her feet and tickling her back and sides.
- Run your finger under her chin and across her cheeks to stimulate her.
- Change her diaper or change her position for a few minutes.
Your baby often chokes while drinking
If the nipple you are using flows too quickly and your baby has too much milk in her mouth, she may choke (i.e., she swallows noisily, coughs and spits up a little milk).
What to do?
- Change to a slower nipple.
- Take short feeding breaks.
- Avoid laying your baby on her back during feeding since milk will flow into her mouth even when she’s not sucking. Try to feed her in a near-sitting position so that the bottle is tilted only slightly downward (just enough for the nipple to fill with milk and not air).
 Your baby will then be able to drink at her own pace.
Your baby will then be able to drink at her own pace.
Your baby regurgitates a lot
As long as your baby is happy and putting on weight, regurgitation (“spitting up”) is generally nothing to worry about (see Regurgitation).
Some babies drink very fast, and their stomachs expand too quickly. This makes it easier for them to regurgitate, especially if they are very active and start moving around right after feeding.
If milk is coming out of the bottle too quickly, your baby will drink too much just to satisfy her need to suck. If she regurgitates a lot, the nipple on the bottle may be too fast.
What to do?
If your baby is in good spirits and gaining weight, there’s nothing to worry about. You don’t need to do anything.
If regurgitation seems to be bothering her, watch her drink. If necessary, try these strategies:
- Change to a slower nipple.
- Take short feeding breaks.
- Try to burp her more.
- Avoid laying your baby on her back during feeding.
 Try to feed her in a near–sitting position so that milk will flow into her mouth more slowly.
Try to feed her in a near–sitting position so that milk will flow into her mouth more slowly. - Try to keep activity to a minimum right after feeding.
It’s best to see a doctor if your baby
- Seems to be in pain
- Projectile vomits several times a day
- Wets fewer diapers
- Isn’t putting on enough weight
Your baby refuses the bottle
Your baby normally breastfeeds, and you want to bottle‑feed her? If she has trouble bottle-feeding or refuses to altogether, see the tips on Combining breast and bottle.
Silent reflux, spitting milk, tongue tie?! HELP
Your browser cannot play this video.
4 answers /
Last post: 04/06/2016 at 10:07 am
Lauren C(467)
03/06/2016 at 3:46 pm
I have a 5wk old ds.
He's always had issues with spitting out milk as he's feeding. It's a lot that comes out - enough to soak through a bib and a Muslin and get on his clothes.
It's a lot that comes out - enough to soak through a bib and a Muslin and get on his clothes.
I've tried tommee tippee and avent bottles. Today I have tried a cheapy old fashioned style bottle. Hasn't made a difference.
Within the last week or so he's started to be unsettled after feeds (although not in the night - weirdly!) and will cry if you lay him flat, but will settle instantly when sat upright or help upright over my shoulder. It's not wind, he winds quite easily. The crying doesn't stop when you wind him.
Today for the first time the screaming has started during the feed. He is obviously hungry and so takes the milk but then it's like he realises oh yeah that hurts and cries until he is literally red in the face.
He is not often sick. Occasionally - but not nearly as much as a baby with 'normal' reflux.
Anyway, seen the health visitor who thought he had colic. I basically said I thought that was very unlikely and I thought it was reflux and explained why. She was with me until I said he wasn't often sick.
She was with me until I said he wasn't often sick.
Anyway I mentioned silent reflux and she didn't seem convinced, but reccomended infant gaviscon for the milk spitting out! (Weird, but seen as it works for reflux I thought I'd go with it)
So she couldn't prescribe it but told me to see doctors. I did. I practically had to force him to prescribe it because again when I mentioned the lack of sick he looked at me like I was a mad woman.
I and going to try the gaviscon in his next bottle and hope that helps.
The issue is I can only give it to him 6 times in 24 hours. Now anyone who has ever had heartburn or acid reflux knows that it is only a temporary relief!
What the hell do I do on the feeds where I can't give it?!
I was thinking perhaps comfort milk? As gaviscon thickens I wondered if comfort milk might be a good substitute for the other feeds?!
I don't even know whether the gaviscon will work yet though!
Another thing - potential tongue tie. Hv and GP said he doesn't have it. I am beginning to think that he has.
Hv and GP said he doesn't have it. I am beginning to think that he has.
When he cries - when he really goes for it - his tongue doesn't touch the top of his mouth. Is that normal? To be honest I haven't ever seen him sick his tongue out but I keep trying to make him do it but to no avail.
Are there any other things to look out for?!
I feel like health professionals think I'm completely bonkers and either making symptoms up or over reacting to a 'bit of milk' (as the GP put it. Er no mate it's a lot of milk!!)
Because he's gaining weight nobody is worried, but they don't hear the poor boy screaming. And because of the lack of sick they don't seem convinced of reflux
I find myself asking why has nobody ever heard of silent reflux?! I have heard of it why the hell haven't they!!
Does anyone have any experience / advice / anything?!
Has anyone got a baby with silent reflux and or tongue tie? Help me pleaaaaaase!!
Anonymous
03/06/2016 at 4:12 pm
Tongue tie signs
Heart shaped tongue
Restricted movement of tongue (often cant touch roof of mouth)
Trapped wind
Milk pouring from sides of mouth
Clicking noise
Less wet nappies
Poor weight gain
There are support groups on facebook.
Manon R
03/06/2016 at 4:32 pm
DD had silent reflux. As I bf gaviscon was not really possible as she was not taking a bottle at all.
We raised crib/cot with 2x400 page hardcover books under each front leg and had her upright after each feed for 30 minutes. A baby carrier was a necessity as it kept me free to walk around. Generally DD was more happy upright than lying down unless she was on her front.
She was also tongue tied. Only a bf councellor spotted it when she couldn't latch on when my milk came in. We managed feeding her and her weight gain was great but it was snipped when she was 9 months as she had issues with solids. She needed general anaesthetic by then so if you suspect it see ideally a bf clinic and get it done as soon as possible.
Similar threads
Anonymous
04/06/2016 at 10:07 am
In answer to
Lauren C(467)
I have a 5wk old ds.
He's always had issues with spitting out milk as he's feeding. It's a lot that comes out - enough to soak through a bib and a Muslin and get on his clothes.
I've tried tommee tippee and avent bottles. Today I have tried a cheapy old fashioned style bottle. Hasn't made a difference.
Within the last week or so he's started to be unsettled after feeds (although not in the night - weirdly!) and will cry if you lay him flat, but will settle instantly when sat upright or help upright over my shoulder. It's not wind, he winds quite easily. The crying doesn't stop when you wind him.
Today for the first time the screaming has started during the feed. He is obviously hungry and so takes the milk but then it's like he realises oh yeah that hurts and cries until he is literally red in the face.
He is not often sick. Occasionally - but not nearly as much as a baby with 'normal' reflux.
Anyway, seen the health visitor who thought he had colic. I basically said I thought that was very unlikely and I thought it was reflux and explained why. She was with me until I said he wasn't often sick.
She was with me until I said he wasn't often sick.
Anyway I mentioned silent reflux and she didn't seem convinced, but reccomended infant gaviscon for the milk spitting out! (Weird, but seen as it works for reflux I thought I'd go with it)
So she couldn't prescribe it but told me to see doctors. I did. I practically had to force him to prescribe it because again when I mentioned the lack of sick he looked at me like I was a mad woman.
I and going to try the gaviscon in his next bottle and hope that helps.
The issue is I can only give it to him 6 times in 24 hours. Now anyone who has ever had heartburn or acid reflux knows that it is only a temporary relief!
What the hell do I do on the feeds where I can't give it?!
I was thinking perhaps comfort milk? As gaviscon thickens I wondered if comfort milk might be a good substitute for the other feeds?!
I don't even know whether the gaviscon will work yet though!
Another thing - potential tongue tie. Hv and GP said he doesn't have it. I am beginning to think that he has.
Hv and GP said he doesn't have it. I am beginning to think that he has.
When he cries - when he really goes for it - his tongue doesn't touch the top of his mouth. Is that normal? To be honest I haven't ever seen him sick his tongue out but I keep trying to make him do it but to no avail.
Are there any other things to look out for?!
I feel like health professionals think I'm completely bonkers and either making symptoms up or over reacting to a 'bit of milk' (as the GP put it. Er no mate it's a lot of milk!!)
Because he's gaining weight nobody is worried, but they don't hear the poor boy screaming. And because of the lack of sick they don't seem convinced of reflux
I find myself asking why has nobody ever heard of silent reflux?! I have heard of it why the hell haven't they!!
Does anyone have any experience / advice / anything?!
Has anyone got a baby with silent reflux and or tongue tie? Help me pleaaaaaase!!
The two often go hand in hand. It's definitely worth getting it ruled out before you start medication. If you had trouble breastfeeding that could also be why! Your best bet is to go private to be honest - they are unlikely to treat u on nhs as baby is gaining weight. It's so ridiculous and short sighted because if he is tongue tied it can cause weaning and speech problems and tooth decay- lots of tongue tie babies are bottle fed because they can't breastfeed and then their tie isn't picked up-likely a major reason why 'bottle feeding' seems to cause tooth decay- actually because they can't swallow and get rid of al the milk in their mouths properly! Anyway have a look at association of tongue tie practitioners- it's about £150-200 for consultation and snip. Will be worth every penny if he has got it. GPs and health visitors are not difanosed to pass judgment - they are not trained so don't take Any notice of them! Frankly they have sod all training in infant nutrition in general- but as with anything sometimes you're lucky and they're ace- sometimes their rubbish! Here is a link to symptoms and they have a helpline
It's definitely worth getting it ruled out before you start medication. If you had trouble breastfeeding that could also be why! Your best bet is to go private to be honest - they are unlikely to treat u on nhs as baby is gaining weight. It's so ridiculous and short sighted because if he is tongue tied it can cause weaning and speech problems and tooth decay- lots of tongue tie babies are bottle fed because they can't breastfeed and then their tie isn't picked up-likely a major reason why 'bottle feeding' seems to cause tooth decay- actually because they can't swallow and get rid of al the milk in their mouths properly! Anyway have a look at association of tongue tie practitioners- it's about £150-200 for consultation and snip. Will be worth every penny if he has got it. GPs and health visitors are not difanosed to pass judgment - they are not trained so don't take Any notice of them! Frankly they have sod all training in infant nutrition in general- but as with anything sometimes you're lucky and they're ace- sometimes their rubbish! Here is a link to symptoms and they have a helpline
http://milkmatters. org.uk/2011 [...] your-baby/
org.uk/2011 [...] your-baby/
Can't find your answer?
Popular Chat
Preventive measures against regurgitation in children
08.03.2017
Regurgitation is the spontaneous reflux of gastric contents into the esophagus and mouth. This condition is not uncommon in infants and is often a cause for concern for parents. The frequency of regurgitation syndrome in children of the first year of life is 18-50%: up to 4 months - 67%, up to 6 months 24%, up to 1 year 5%. In most cases, regurgitation is "benign" and disappears on its own after 12-18 months. At the same time, “benign” or physiological regurgitation characterizes:
-
the age of the child is up to 12 months;
-
spitting up 2 or more times a day for 3 or more weeks;
-
sufficient weight gain;
The child has no signs of metabolic disorders, diseases of the gastrointestinal tract or the central nervous system. The child does not experience difficulty in swallowing or feeding, there is no forced position of the body.
The child does not experience difficulty in swallowing or feeding, there is no forced position of the body.
Do not confuse regurgitation with vomiting. When a child burps, the abdominal muscles do not tense up. With vomiting, on the contrary, muscle tension occurs and food is ejected by pressure not only through the mouth, but also through the nose. In some cases, there may be general anxiety, pallor, cold extremities. Often with vomiting, the temperature rises, loose stools appear, which is a sign of an infectious disease. Vomit may contain unchanged milk, mucus, blood or bile.
What explains physiological regurgitation
What is the tendency of babies to spit up? This phenomenon is explained by the peculiarity of the structure of the gastrointestinal tract of young children. At the age of one year, the esophagus is shorter and wider, physiological narrowing is weakly expressed. The stomach is located horizontally, its capacity is small, and the muscles that close the entrance to the stomach and prevent the contents from being thrown back into the esophagus are poorly developed. As the child begins to walk, the axis of the stomach becomes more vertical. The capacity of the stomach increases by the year from 30-35 ml to 250-300 ml. The secretory apparatus matures, the work of the closing muscles (sphincters) improves, which leads to a gradual decrease in the frequency and disappearance of regurgitation. These features explain the predisposition of young children to regurgitation and even the inevitability of this condition. However, there are measures to help reduce the frequency of regurgitation.
As the child begins to walk, the axis of the stomach becomes more vertical. The capacity of the stomach increases by the year from 30-35 ml to 250-300 ml. The secretory apparatus matures, the work of the closing muscles (sphincters) improves, which leads to a gradual decrease in the frequency and disappearance of regurgitation. These features explain the predisposition of young children to regurgitation and even the inevitability of this condition. However, there are measures to help reduce the frequency of regurgitation.
Factors contributing to physiological regurgitation include:
-
Overfeeding. As a rule, actively sucking babies begin to suffer from overfeeding, with abundant milk secretion, as well as when switching to artificial or mixed feeding with an incorrect calculation of the required amount of milk formula. Regurgitation appears immediately or some time after feeding in the amount of 5-10 ml. Milk can flow out unchanged or curdled.
-
Swallowing air during feeding (aerophagia).
 A similar situation arises if the child suckles greedily at the breast, and the mother's milk is not very plentiful; due to the retracted, flat nipple of the mother's breast, since the child fails to fully capture the nipple and areola; with artificial feeding, if the hole at the nipple of the bottle is large enough or the nipple is not completely filled with milk. Babies with aerophagia often experience anxiety after feeding, bulging of the abdominal wall (belly inflates). After 10-15 minutes, the swallowed milk flows out unchanged, which is accompanied by a loud sound of air eructation.
A similar situation arises if the child suckles greedily at the breast, and the mother's milk is not very plentiful; due to the retracted, flat nipple of the mother's breast, since the child fails to fully capture the nipple and areola; with artificial feeding, if the hole at the nipple of the bottle is large enough or the nipple is not completely filled with milk. Babies with aerophagia often experience anxiety after feeding, bulging of the abdominal wall (belly inflates). After 10-15 minutes, the swallowed milk flows out unchanged, which is accompanied by a loud sound of air eructation. -
Intestinal colic or constipation. These conditions lead to an increase in pressure in the abdominal cavity and a violation of the movement of food through the gastrointestinal tract, causing regurgitation.
Until the child is four months old, spitting up up to two teaspoons of milk after feeding, or one spitting up of more than three spoons during the day, is considered the norm. You can check the amount of spitting up in the following way: take a diaper, pour one teaspoon of water on its surface, and then compare this spot with the spot formed after the next spitting up.
You can check the amount of spitting up in the following way: take a diaper, pour one teaspoon of water on its surface, and then compare this spot with the spot formed after the next spitting up.
Pathological regurgitation may be due to:
-
surgical diseases and malformations of the digestive system;
-
diaphragmatic hernia;
-
pathology of the central nervous system, trauma of the cervical spine during childbirth;
-
food intolerance, lactase deficiency;
-
increased intracranial pressure.
Such regurgitation is characterized by intensity, systematicity, the child spits up a large amount of milk. At the same time, there is a violation of the general condition of the baby - the child is whiny, loses or does not gain weight, cannot eat the amount of food necessary for his age. In such a situation, a pediatrician, gastroenterologist, surgeon, allergist, neurologist should be examined. It also requires examination and exclusion of anomalies in the structure of the upper gastrointestinal tract, the preservation of regurgitation for more than 1 year.
It also requires examination and exclusion of anomalies in the structure of the upper gastrointestinal tract, the preservation of regurgitation for more than 1 year.
Scale for assessing the intensity of regurgitation:
-
Less than 5 regurgitations per day with a volume of not more than 3 ml - 1 point.
-
More than 5 regurgitations per day with a volume of more than 3 ml - 2 points.
-
More than 5 regurgitations per day up to half the amount of formula or breast milk, not more often than in half of the feedings - 3 points.
-
Spitting up a small amount of milk for 30 minutes or more after each feeding - 4 points.
-
Regurgitation from half to full volume of formula or breast milk in at least half of the feedings - 5 points.
Regurgitation with an intensity of 3 or more points requires a visit to a doctor.
Preventive measures against regurgitation in children
If regurgitation is physiological in nature, then it is not worth treating or correcting in this case.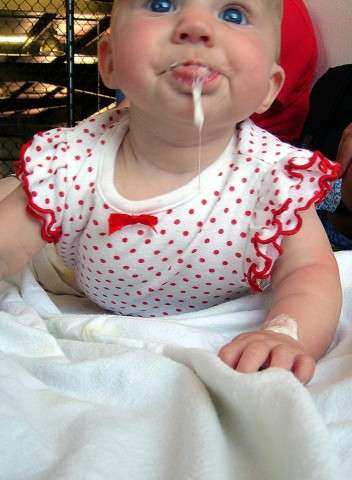 It is necessary to deal with the elimination of the cause, if possible, and carry out prevention.
It is necessary to deal with the elimination of the cause, if possible, and carry out prevention.
Prevention of regurgitation in children includes the following measures:
-
Postural therapy: when feeding, it is necessary to hold the baby at an angle of 45 °, make sure that he completely grasps the nipple with the areola; after feeding, hold the baby in an upright position ("column") for 20 minutes - to drain the swallowed air. Due to this, the air that has entered the stomach will be able to go out. If nothing happened, then put the baby down and after a minute or two, lift him upright again.
-
Make sure that the opening in the bottle is not too large and that the nipple is filled with milk. Experiment with nipples - perhaps the other will be better. Milk should come out in drops, not a trickle.
-
Before you start feeding your baby, lay him belly down on a solid base.
-
After feeding, try to minimize the baby's physical activity, do not disturb him unnecessarily, and change clothes only if there is an emergency.
-
Avoid squeezing diapers or clothes on the abdomen of the child.
-
If the baby's appetite is good, then it is better to feed him often, but in small portions, otherwise, due to the large amount of food, the stomach may overflow, and this, as a result, leads to regurgitation of excess food.
-
The surface in the bed on which the baby lies should rise 10 cm at the head.
-
In addition, it is possible to use special "thickeners" of milk or anti-reflux mixtures, which the doctor will help you choose.
In the event that regurgitation begins to become more frequent or becomes abundant, or first began after six months of the baby's life, or does not subside by one and a half to two years of life, the child should be consulted by a pediatrician. With a high probability, additional help from a gastroenterologist will be needed.
In our Family Medical Center you can always find highly professional help.
← Back to the list of articles
Why does the baby spit up after feeding?
How to distinguish normal regurgitation from vomiting?
Sometimes regurgitation is considered a manifestation of disorders in the digestive tract of children. Due to the constant reflux of acidic stomach contents into the upper sections, inflammation and other complications may develop, including growth retardation, a decrease in hemoglobin levels, and others. Therefore, it is important for parents to understand where the line is between physiological and pathological regurgitation 1 .
If the mother is worried that her baby is spitting up, keep track of when this happens and count the total number of spit ups per day. Normally, regurgitation usually occurs after eating (the child burps after each feeding), lasts no more than 20 seconds and repeats no more than 20-30 times a day. With pathology, the problem manifests itself at any time of the day, regardless of when the baby was fed. Their number can reach 50 per day, and sometimes more 1 .
Their number can reach 50 per day, and sometimes more 1 .
The amount of discharge during regurgitation also matters. With normal, physiological regurgitation, it is approximately 5 - 30 ml. If this volume fluctuates between 50 and 100 ml, it is already defined as profuse vomiting. When the range of the jet of vomit is up to 50 cm, doctors talk about "vomiting a fountain." A variant of atonic vomiting is possible, when the contents of the stomach flow "sluggishly". It occurs with atony of the stomach (decrease in muscle tone of the stomach wall) and disruption of the esophagus 1 .
Vomiting in babies is a warning sign. Doctors are especially alarmed by repeated vomiting, a fountain, with an admixture of bile, in combination with constipation. Vomiting can lead to the development of dehydration, acid-base imbalance and other consequences, therefore, if it occurs, you should urgently contact a pediatrician to find out the cause and begin treatment. A doctor's consultation is necessary if the child is spitting up a lot (more than 15-30 ml at a time), with a frequency of more than 50 episodes per day 1.3 .
A doctor's consultation is necessary if the child is spitting up a lot (more than 15-30 ml at a time), with a frequency of more than 50 episodes per day 1.3 .
Physiological regurgitation: symptoms
Regurgitation in newborns, which is considered normal and not of concern to pediatricians 3 :
- usually lasts for a certain period of time;
- is characterized by slow, "passive" outflow; if the baby spits up a fountain, it is better to consult a doctor;
- has a sour smell of curdled milk;
- occurs without the participation of muscles - the baby does not strain during regurgitation;
- does not affect the general well-being of the baby.
How to help a newborn who spit up often?
If the baby is healthy, no medication is prescribed for spitting up. To help the child allow simple measures based on lifestyle changes and feeding.
- Frequent feeding of the baby
It is known that babies are more prone to spit up if their stomach is full.