Best position to bottle feed newborn baby
Bottle feeding advice - NHS
If you're planning to bottle feed with expressed breast milk or infant formula, these tips will help you feed your baby and keep them safe and healthy.
If you decide to use infant formula, first infant formula (first milk) should always be the first formula you give your baby. You can use it throughout the first year.
Buying bottle feeding equipment
You'll need several bottles, teats and a bottle brush, as well as sterilising equipment, such as a cold-water steriliser, microwave or steam steriliser.
There's no evidence that 1 type of teat or bottle is better than any other. Simple bottles that are easy to wash and sterilise are probably best.
Making up bottles for your baby
Make sure you sterilise bottles and teats until your baby is at least 12 months old. Wash your hands thoroughly before handling sterilised bottle and teats.
If you're using infant formula, follow the instructions on the packaging carefully when you make up the feed.
See how to make up baby formula.
How to bottle feed your baby
Bottle feeding is a chance to feel close to your baby and get to know and bond with them. Babies will feel more secure if most feeds are given by you, your partner or their main caregiver.
Make sure you're sitting comfortably with your baby close to you. Enjoy holding your baby, look into their eyes and talk to them as you feed them.
Hold your baby in a semi-upright position for bottle feeds. Support their head so they can breathe and swallow comfortably.
Brush the teat against your baby's lips and when they open their mouth wide let them draw in the teat.
Always give your baby plenty of time to feed.
Do not leave your baby alone
Never leave your baby alone to feed with a propped-up bottle as they may choke on the milk.
Keep the bottle horizontal
Gently place the teat into the baby’s mouth. Keep the bottle in a horizontal position (just slightly tipped). This will allow the milk to flow steadily and help prevent your baby from taking in air.
If the teat goes flat while you're feeding, pull gently on the corner of your baby's mouth to release the suction.
If the teat gets blocked, replace it with another sterile teat.
Be guided by your baby
All babies are different. Your baby will know how much milk they need. Some want to feed more often than others. Just follow your baby's lead.
Feed your baby when they seem hungry and do not worry if they do not finish the bottle.
Winding your baby
Your baby may take short breaks during a feed and may sometimes need to burp.
When your baby has had enough milk, hold them upright and gently rub or pat their back to bring up any wind.
Throw away unused milk
Throw away any unused formula or breast milk after you've finished bottle feeding your baby.
Only make up the feed when needed – one feed at a time.
Help with bottle feeding
Talk to your midwife, health visitor or other mothers who have bottle fed if you need help and support.
You'll find the phone number for your health visitor in your baby's personal health record (red book).
Your questions about bottle feeding
Why if my baby does not settle after feeds?
If your baby swallows air while bottle feeding, they may feel uncomfortable and cry.
After a feed, hold your baby upright against your shoulder or propped forward on your lap. Gently rub their back so any trapped air can find its way out.
Your baby may sometimes only burp up a small amount of air.
Why is my baby sometimes sick after feeds?
It's normal for babies to bring up a little milk during or just after a feed. This is called possetting, regurgitation or reflux.
Keep a muslin square handy just in case.
Check that the hole in your baby's teat is not too big. Drinking milk too quickly can make your baby sick.
Do not force them to take more milk than they want during a feed. This may be distressing for your baby and can lead to overfeeding.
Sitting your baby upright on your lap after a feed may help.
If it happens a lot, or your baby is violently sick, seems to be in pain or you're worried for any other reason, talk to your health visitor or GP.
Can formula make my baby constipated?
When using formula, always use the amount of powder recommended on the packaging.
Do not add extra formula powder. Using too much can make your baby constipated and may cause dehydration.
If your baby is under 8 weeks old and has not done a poo for 2 to 3 days, talk to your midwife, health visitor or GP, particularly if your baby is gaining weight slowly.
Your baby should be gaining weight and have plenty of wet and dirty nappies.
Infant formula and allergies
If you think your baby might be allergic to or intolerant of formula, talk to your GP. If necessary, they can prescribe a special formula feed.
Some formula is labelled as hypoallergenic, but this is not suitable for babies with a diagnosed cows' milk allergy.
Soya formula should only be given to babies under medical supervision.
Always talk to your GP before using hypoallergenic or soya-based formula.
Read more about cows' milk allergy and lactose intolerance.
Get Start4Life pregnancy and baby emails
For information and advice you can trust, sign up for weekly Start4Life pregnancy and baby emails.
The Start4Life website also has more information and advice about expressing and bottle feeding
Everything You Want to Know
Bottle-feeding an infant is not rocket science, but it’s not necessarily easy either. Some babies take to the bottle like champs, while others require a bit more coaxing. In fact, introducing a bottle can be a process of trial and error.
Some babies take to the bottle like champs, while others require a bit more coaxing. In fact, introducing a bottle can be a process of trial and error.
This seemingly simple undertaking is made exponentially more challenging by the staggering plethora of bottle options, varying nipple flows, different formula types, and multiple feeding positions.
Yes, there’s a whole lot more to bottle-feeding than what meets the eye, so don’t be discouraged if your wee one is a bit fussy at first. You’ll soon find the routine — and products — that work for your little one. In the meantime, we’ve got you covered with all the bottle basics.
Once your bottle is prepared and at the ideal temperature (find more details on these below), it’s time to start feeding your baby.
- First, find a position that’s comfortable for you and safe for your baby.
- Hold the bottle at a horizontal angle so that your little one has to gently suck to get the milk.
- Be sure that the milk fills the entire nipple so that your baby isn’t gulping lots of air, which may result in gas and fussiness.

- You’ll want to take breaks every few minutes to gently burp baby. If they seem particularly squirmy during a feeding, they may have a gas bubble; take a pause and gently rub or pat their back.
- Use this opportunity to bond with your baby. Hold them close, look into their wide eyes, sing soft songs, and make feeding time a happy time.
Be sure to pace your feeding. You can’t expect — nor do you want — a new baby to chug a bottle down in 5 minutes flat. It may take a while, and that’s a good thing.
You want a baby to regulate their own hunger, so slow down and allow an infant to go at their own speed. Be sure to follow their cues, pause to burp or reposition them, and put the bottle down if they seem bothered or disinterested. You can try again in a few minutes.
And if they seem to want a top off? Go ahead and offer a free refill if it seems necessary.
There are several positions you can try for bottle-feeding. Make sure you’re both comfortable so it’s a pleasant experience. Find a suitable place to sit comfortably, use pillows to support your arms if needed, and cozy up together during feeds.
Find a suitable place to sit comfortably, use pillows to support your arms if needed, and cozy up together during feeds.
Here are a few options to try:
Cradle your baby
When you think of holding a newborn baby, you probably envision yourself cradling them in the nook of your arm. This is a great position for feeding your wee one a bottle. Rest their head in your elbow bend, and tilt them up so they’re at a comfortable angle. This position is ideal for some bonus skin-to-skin contact.
Sitting position
Sit down and place baby upright in your lap with their back against your stomach and chest. This position is especially encouraged for infants with reflux. Just be sure that you’re tipping the bottle to completely fill the nipple with milk.
Rest baby on your legs
Sit or lay down, and prop your baby on your legs with their back against your thighs and their head near your bent knees. This position allows for eye contact and interaction.
Use a feeding pillow
Nursing pillows aren’t just for breastfeeding. Some babies enjoy being positioned on a pillow for mealtime. A traditional C-shaped nursing pillow works great for this purpose, allowing baby to relax and be comfortable during a feed.
Some babies enjoy being positioned on a pillow for mealtime. A traditional C-shaped nursing pillow works great for this purpose, allowing baby to relax and be comfortable during a feed.
While this option frees up your arms, you’ll still need to hold the bottle for your baby. Propping or rigging a hands-free situation has potentially dangerous consequences.
Once a baby is old enough and expresses interest in holding the bottle themselves (somewhere around 6–10 months of age), you can let them try. Just be sure to stay close and monitor them carefully.
Whatever position you try, make sure that your little one is angled, with their head raised. You don’t ever want your baby to be lying down flat while eating. This could enable milk to travel into the inner ear, potentially causing an ear infection.
Of course, feeding baby the bottle might be the easy part. Picking the right vessel to hold your breast milk or formula can be a whole other complicated story. The information below can help you master the art of preparing the perfect bottle for your baby.
Choose the right bottle for your baby
If you’ve ever browsed the feeding section of a baby store, you know that bottle options are seemingly endless.
There are bottles designed for colicky babies, gassy babies, and breastfed babies. It’s daunting. The confounding truth is that some babies will take any old bottle you throw at them, while others will be far more discerning.
You might have to try a few different brands to find “the one” for your baby. If you have a gassy guzzler, you could go with one that uses a venting system. If you’ve been exclusively nursing up until now, you can try one that more readily resembles the shape and feel of mama’s breast.
You may also want to pick a bottle that has fewer parts to clean and reassemble. You’ll appreciate the lack of steps during that 2 a.m. feeding session.
Furthermore, start with a slow-flow nipple, and upgrade when your baby seems eager to get more milk, faster.
Prepare your formula or breast milk bottle
Feeding with formula? There are three types to choose from: powder, concentrate, and ready-to-pour.
Ready-to-pour formula is the easiest (and, yes, most expensive) option of the three. It involves no preparation and is as simple as opening and pouring it. You can purchase small, individual bottles that come with nipples, which are especially useful for those early infant feedings, or opt for larger bottles that need to be refrigerated. Either way, it’s fairly foolproof.
When using powder, you’ll need to measure out portions and mix them well with suitable water. It’s important to follow the directions and use the recommend water-to-formula ratio. Using too much water can dilute the nutrients; using not enough can cause dehydration. Both of these possibilities can have dangerous consequences, so use caution and care.
Similarly, concentrate formulas require a safe water source. Once again, measuring appropriately is key.
If you’re breastfeeding, preparing a bottle is pretty straightforward. Just pour pumped fresh or frozen breast milk into a bottle, and warm it up (if refrigerated and desired). Be sure to double-check the pump date, though; thawed and/or refrigerated breast milk has a short shelf life.
Be sure to double-check the pump date, though; thawed and/or refrigerated breast milk has a short shelf life.
Warm your bottle
Some babies will take a bottle straight out of the refrigerator, but many prefer their milk slightly warmed.
The best way to warm up a cold formula or breast milk bottle is by submerging it in a cup of hot water for a few minutes. You can also use a bottle warmer. Test the milk temperature on your wrist before serving it to your baby.
Be sure to never microwave a bottle. This can cause an uneven temperature throughout and create hot spots that could burn baby’s mouth.
How long is a bottle good for?
It may seem painful to throw away precious pumped liquid gold or chuck expensive formula. Yet, at some point or another, you’ll probably watch wistfully as you pour some unused bottle milk down the drain.
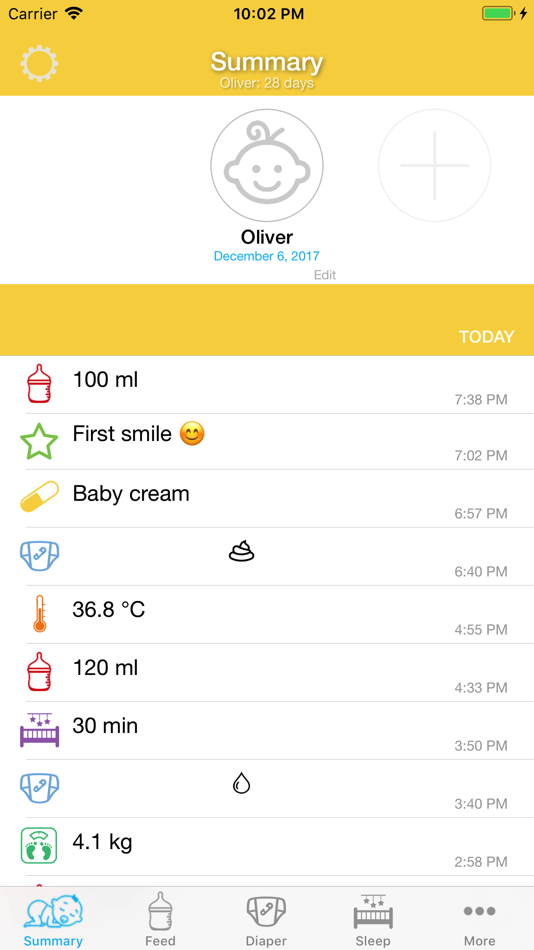
If you’re using expressed breast milk, there are some important time frames to remember. Breast milk can be frozen for up to 6 to 12 months and refrigerated for 4 days. (If it has been thawed, though, you should use it within 24 hours.) Once you begin feeding a breast milk bottle, it’s safe for up to 2 hours.
(If it has been thawed, though, you should use it within 24 hours.) Once you begin feeding a breast milk bottle, it’s safe for up to 2 hours.
A prepared bottle of formula can be refrigerated for 24 hours. Once baby has taken a sip from a bottle of formula, it must be used within 1 hour. Bacteria multiply quickly on milk-based products, so be sure to check the clock.
It may feel like you’re constantly preparing bottles, but don’t worry, this feeding frenzy phase will soon pass.
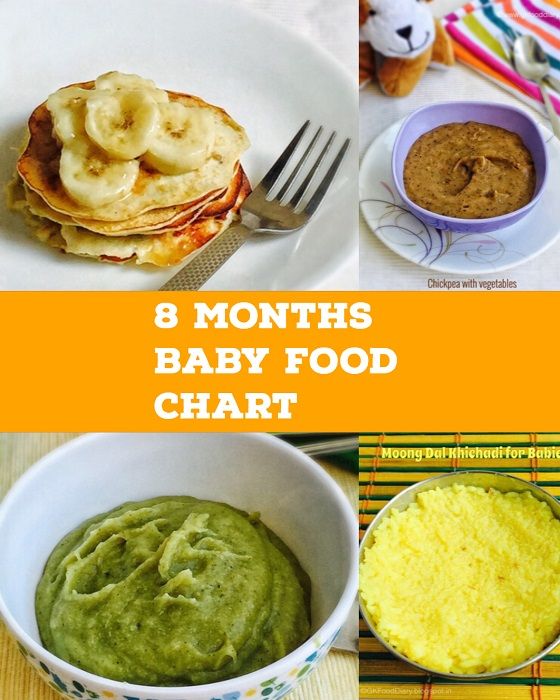
Yes, in the early days of parenthood, you’ll be feeding your little one every 2 to 4 hours. As a newborn, your baby will likely consume around 2 ounces per feed.
As they get older, the feedings may become spaced out, and the amount in each bottle will increase. Around the 2-month mark, your baby may start drinking 4 to 6 ounces each feeding. By 6 months, they’ll probably take in about 8 ounces.
Don’t feel tethered to a strict feeding schedule. It’s best to feed a baby when they seem hungry. Babies go through rapid growth spurts and may need to feed more frequently. Look for hunger cues to determine whether your little one is hankering for a bottle.
Babies go through rapid growth spurts and may need to feed more frequently. Look for hunger cues to determine whether your little one is hankering for a bottle.
Your baby may be hungry if they begin gumming on their hands, sucking on their tongue, or rooting. Rub your finger or a bottle nipple at the side of their cheek or mouth, if they turn toward it, they’re probably ready for a feeding. Give that bottle a go!
If you’re a nursing mama, you may feel especially nervous about introducing a bottle. Rest assured that with a little patience and time, your baby will eventually get the hang of it.
Still, before you offer a bottle, you’ll want to feel confident that nursing has been well established. As such, you should consider waiting 2 to 3 weeks after your baby is born to introduce the bottle to avoid potential nipple confusion and ensure that your milk supply is adequate.
If you need to transition your baby to the bottle before returning to work, cushion in some extra time to normalize this routine. While your breastfed baby may happily accept the first bottle you offer, they may also turn their tiny nose up at it. Spare yourself and your baby unnecessary pressure, and give yourselves some wiggle room to adjust.
While your breastfed baby may happily accept the first bottle you offer, they may also turn their tiny nose up at it. Spare yourself and your baby unnecessary pressure, and give yourselves some wiggle room to adjust.
And if your baby does resist the bottle? Walk out of the room and have a partner or caregiver try. Your baby knows that you have the real deal under your shirt, and they may respond more readily to someone else.
Furthermore, don’t try to introduce the bottle when your little one is impatiently ravenous. Wait until they’re in a pleasant mood, and offer a bit when their tummies aren’t entirely empty. You may get a better reaction.
Even if you plan to be home and available to nurse around the clock, you should still try to introduce the occasional bottle. It’s good to know that your baby will accept it in a pinch.
Bottle-feeding has its challenges and rewards. There are a few other tips to keep in mind to help set you and your baby up for success.
Washing and sterilizing bottles
You may want to sterilize your bottles before their first use. You can do this with a steam sterilizer or in the dishwasher.
Sanitizing them between uses is probably unnecessary, but you do want to ensure that you always have a clean supply on hand — lest you have to wash one in the middle of the night while a crying baby impatiently awaits their bottle.
That said, a bottle requires a thorough scrubbing between uses, especially if it has pieces and parts with nooks and crannies. You can, of course, also use your trusty dishwasher. Either way, it’s smart to at least pour out any unused formula or breastmilk right away and give the bottle a quick rinse after a feeding session.
Mixing breast milk and formula
Want to slowly introduce formula to your breastfed baby? You can mix breast milk and formula in the same bottle. This can get baby more readily adjusted to the unique flavor of formula.
Just be sure to prepare the formula separately. If you’re using powder or concentrate formula, you’ll still need to add water first; don’t use breast milk as a liquid substitute. Once the formula is prepared, pour in the breast milk.
If you’re using powder or concentrate formula, you’ll still need to add water first; don’t use breast milk as a liquid substitute. Once the formula is prepared, pour in the breast milk.
Finally, heed the time restrictions. While breast milk on its own can be used for up to 2 hours, the addition of formula means the bottle is only good for 60 minutes.
Adding cereal to a bottle
Has a well-meaning grandparent suggested adding cereal to your baby’s bottle?
Generally speaking, doctors advise against this practice. While many people assume it will keep their baby fuller for longer — and even help them sleep for a longer chunk of time — it can have a few negative consequences, including excessive weight gain and constipation.
Occasionally, doctors will recommend adding a bit of oatmeal cereal to a bottle to help a baby with gastroesophageal reflux disease (GERD). Talk to your pediatrician before making this decision on your own.
No doubt, the idea of bottle service takes on a whole new meaning these days, but you’re going to love this new adventure.
And while it may seem like a lot to take in, bottle-feeding your baby will soon become second nature. You may encounter some hurdles or missteps along the way, but you’ll quickly discover what works for you and your baby.
Good luck, you’ve got this!
Best Positions for Bottle Feeding
Bottle feeding is not really a complicated process. However, you must remember a few rules. If you feed your baby incorrectly, he may cry, spill formula, suffer from colic, or slowly gain weight. Therefore, in order to properly bottle feed your baby, you must choose the correct upright feeding position. It should remind the baby of a natural position for feeding. Also remember that your baby's head should rest in the crook of your arm, in line with the spine. The longitudinal part of the nipple that enters the baby's mouth must always be full of milk - otherwise the baby swallows air, which can cause colic. Bubbles inside the bottle mean your baby is suckling properly.
Here are some examples of comfortable bottle feeding positions.

Whatever position you choose, it is best to always sit on the floor, comfortably leaning back against the wall. Try all positions to find the most comfortable one:
Sitting position
This is the most classic position. The child sits on one of your thighs with his back against your other thigh. You can hold his head in the crook of your arm or straight with your arm.
Side
If your baby spit up frequently, has gastroesophageal reflux disease, or has a runny nose, it is best to feed him when he lies diagonally on his side (preferably on his left side, but from time to time you need to shift to the other side). Your baby lies on its side, on one of your thighs, with its back and head against your other thigh. His ass rests on your stomach. You can change the angle of your child's body by raising or lowering your knees.
Facing each other
Place the baby on your lap with his bottom pressed against your stomach. This position ensures the correct position of the head and torso (the head is in line with the spine). Remember to keep your child's torso straight, don't let him arch his back.
Remember to keep your child's torso straight, don't let him arch his back.
Almost apart from each other
In this position, you must keep the child's torso in line with the head. This will help your baby breathe properly, suck and swallow more effectively, and be less tired during feedings. If your child wants to, let him hold the bottle in his hand, even if he is still very small. At about 7 months, the baby begins to feel independent and wants to hold the bottle on his own. However, you should still support the bottle with your hand and help your baby with feeding until he finishes eating. When your baby grows up (i.e., sits up on his own), you can feed him in a high chair and replace the bottle with a non-spill cup or a regular cup with a straw. Do not leave your child alone with a bottle. This is strictly prohibited! You also shouldn't let your baby sleep with a bottle during mouth. In both cases, it can choke!
Whether you are breastfeeding or bottle feeding, always remember these rules:
- First of all, always feed your baby in your arms.
Do not feed your baby when he is lying, especially on his back. He may choke on milk. Babies often suffer from reflux, which means the mixture flows back from their stomach into their esophagus.
Also remember that your child feels safest in your arms. Try also to change hands from time to time, ie. support the child first with one hand and then with the other. Thanks to this, your child's muscles will develop evenly.
- Second, remember to always keep your child's head higher than his torso (put him on your arm). This is the best position for a baby while breastfeeding. If you are breastfeeding, make sure your baby cuddles and suckles properly. When bottle feeding, make sure that the part of the nipple that is in the baby's mouth is completely filled with milk. This minimizes the risk of swallowing air (i.e., prevents colic). Make sure your baby doesn't tilt their head back or forward too much. This makes sucking very difficult and can even cause food to enter your baby's airways.
- Third, never feed your baby when you are irritable or stressed. Take a moment for yourself first, take a deep breath and try to relax. When you have calmed down, sit in a comfortable chair, place a pillow under your armpit, place your baby on the pillow, and start feeding while speaking gently to your baby. Your child feels your emotions. If you are tense, he will also feel awkward. Also, never feed a baby if he is excited, crying or screaming. When he is in this condition, his airways are not protected and the mixture can enter his larynx instead of his esophagus.
- Fourth, take breaks after and during each feed by holding the baby in an upright or semi-upright position. Lay his head on your shoulder and support his back with your hand. Keep your baby upright until he releases any air he swallows while feeding. It usually only takes a moment, although sometimes it can take a little longer.
Various breastfeeding positions
Try different breastfeeding positions to find the one that works best for you and your baby. You can see the options in our selection of photos
You can see the options in our selection of photos
Share this information
There is no right or wrong way to hold the baby while
feeding, and mom and baby are sure to find their favorite position.
It is important that both you and your child feel comfortable. 1.2 It's good to learn a few different breastfeeding positions and techniques because life's circumstances often require us to be flexible, especially as your baby gets older and you start to leave the house more often.
Whatever position you choose to breastfeed your baby, remember a few simple rules.
- Prepare everything you need before feeding, including drinks, food, mobile phone, TV remote control, book or magazine. And do not forget to go to the toilet - the feeding process can take a long time!
- Make sure your baby is comfortable. Whichever position you choose, it's important to keep your baby strong, level, and provide good support for their head, neck, and spine.

- You should also be comfortable. Don't stress. If necessary, use pillows of different sizes or rolls of towels to support your back or arms.
- Make sure your baby is latching on correctly. Proper grip is the key to comfort when breastfeeding.
- If your baby does not latch on well or you experience pain while feeding, contact a lactation consultant for help. The specialist will also be able to show you how to hold your baby more comfortably.
1. Relaxed feeding or reclining position
The relaxed feeding position, also known as biological feeding, 1 is often the first position for most mothers. If, immediately after birth, the baby is placed on the mother’s chest or stomach, normally, he instinctively reaches for the breast and tries to grab the nipple. This phenomenon is known as the breast seeking reflex. Skin-to-skin contact stimulates the infant's feeding instinct, and gravity helps him to latch onto the breast and maintain balance.
But it's not just newborns that can be fed in the reclining position - this position is great for babies of all ages. It can be especially helpful if your baby does not latch well in other positions or does not like to be touched during feeding, and also if you have too much milk flow or too large breasts. Isabelle, a mother from the UK, shares her experience: “I had large breasts, and the baby was born small - 2.7 kg, so it was not easy to find a comfortable position at first. After a few weeks, it became clear that there was no “correct” posture for me. As a result, I most often fed lying down, putting the baby on my chest. ”
It is more convenient to feed not lying flat on your back, but half-sitting, leaning on pillows. So you will have a back support and you will be able to watch the baby during feeding.
2. Cradle position
This is the classic position that comes to mind first when we talk about breastfeeding
. Mom sits
straight, and the baby lies on her side on her arm, pressing her stomach against her stomach. 3 Although this is a very popular position, it is not always easy to master with newborns because it gives the baby less support. Try putting a pillow under your back, and put a special breastfeeding pillow on your knees and lean on it with your hands. So you can more reliably support the child, without overstraining your back and shoulders. Just make sure that the baby does not lie too high on the pillow for feeding. The breast should remain at a natural level so that the baby can grab it without effort, otherwise sore nipples cannot be avoided.
3 Although this is a very popular position, it is not always easy to master with newborns because it gives the baby less support. Try putting a pillow under your back, and put a special breastfeeding pillow on your knees and lean on it with your hands. So you can more reliably support the child, without overstraining your back and shoulders. Just make sure that the baby does not lie too high on the pillow for feeding. The breast should remain at a natural level so that the baby can grab it without effort, otherwise sore nipples cannot be avoided.
“I breastfed in the cradle position because it suited me perfectly! It was comfortable and I loved just sitting and looking at my little one,” recalls Rachel, a mother of two from Italy.
3. Cross Cradle
This breastfeeding position looks almost the same as the Cradle, but the baby is on the other arm. 3 This gives your baby support around the neck and shoulders so he can tilt his head to latch on. This position is great for breastfeeding newborns and small babies, as well as for babies who do not latch well. Since the baby lies completely on the other hand, it becomes easier to control his position and you can adjust the chest with your free hand.
This position is great for breastfeeding newborns and small babies, as well as for babies who do not latch well. Since the baby lies completely on the other hand, it becomes easier to control his position and you can adjust the chest with your free hand.
Julie, a UK mother of two, finds this position very practical: “I usually breastfeed my youngest in the cross cradle position. So I have a free second hand, and I can take care of an older baby at the same time. ”
Do not hold the baby's head at first, otherwise you may inadvertently press his chin against his chest. Because of this, the child will not be able to take the breast deeply, because the nipple will rest against the base of the tongue, and not against the palate, which will lead to inflammation of the nipples. As the child grows, this position becomes more comfortable, and he can rest his head on your palm (as shown in the photo above).
4. Underarm breastfeeding
In this position, also known as the "ball grip", the mother is seated and the baby lies along her arm at the side, legs towards the back of a chair (or any other seat). 3 Another comfortable position for newborn breastfeeding, you can give your baby good support, full control of the position and a good view of his face. And the baby feels safe in close contact with the mother's body. This position is especially good for those who have had a caesarean section or a premature birth, as well as mothers of twins and women with large breasts.
3 Another comfortable position for newborn breastfeeding, you can give your baby good support, full control of the position and a good view of his face. And the baby feels safe in close contact with the mother's body. This position is especially good for those who have had a caesarean section or a premature birth, as well as mothers of twins and women with large breasts.
“When I breastfed my first daughter, I had very large K-sized breasts—twice the size of her head,” recalls Amy, an Australian mother of two. - I put rolls of towels under each breast, because they were very heavy, and fed my daughter in a pose from under the arm, but only sitting straighter so as not to crush her. This position was also convenient because I had a caesarean section and could not put the baby on my stomach.”
5. Side-lying position
The side-lying position is ideal for relaxed
feeding at night in bed or on the couch. If you had a
caesarean section or ruptures during childbirth, this position may be more comfortable than sitting down. 3 In this position, mother and baby lie side by side, tummy to tummy.
3 In this position, mother and baby lie side by side, tummy to tummy.
“It was difficult for me to sit during endless night feedings, firstly because of the caesarean section, and secondly because of lack of sleep,” recalls Francesca, a mother from the UK. “And then I discovered that you can feed your baby lying on your side and rest at the same time.”
“Because of the short tongue frenulum, Maisie could only properly latch on to her breasts while lying on her side. The lactation consultant showed me how it's done. In this position, the flow of milk was optimal for my daughter, and it was easier for her to keep the nipple in her mouth. As she got older, she became much better at grabbing her breasts in normal positions,” says Sarah, mother of two from Australia.
6. Relaxed breastfeeding after caesarean section
If you can't find a comfortable position for breastfeeding after caesarean section, 3 try to hold the baby on the shoulder while reclining - this does not put pressure on the postoperative suture and allows you to breastfeed the baby comfortably. You can also try side feeding.
You can also try side feeding.
7. Upright breastfeeding or “koala pose”
When breastfeeding in an upright position or “koala pose”, the baby sits with a straight back and a raised head on the mother's hip. 4 This position can be tried even with a newborn if it is well supported, but it is especially convenient for feeding a grown child who can already sit up by himself. The upright sitting position, or “koala pose,” is great for toddlers who suffer from reflux or ear infections and feel better sitting. In addition, this pose may be suitable for children with a shortened frenulum of the tongue or reduced muscle tone.
“When my daughter got a little older, I would often feed her in an upright position, which was more comfortable for both of us, and I could still hold her close,” recalls Peggy, a mother from Switzerland. “Besides, it was possible to discreetly breastfeed her in public places.”
8. Overhanging position
In this position, the baby lies on his back, and the mother bends over him
on all fours so that the nipple falls directly into his mouth.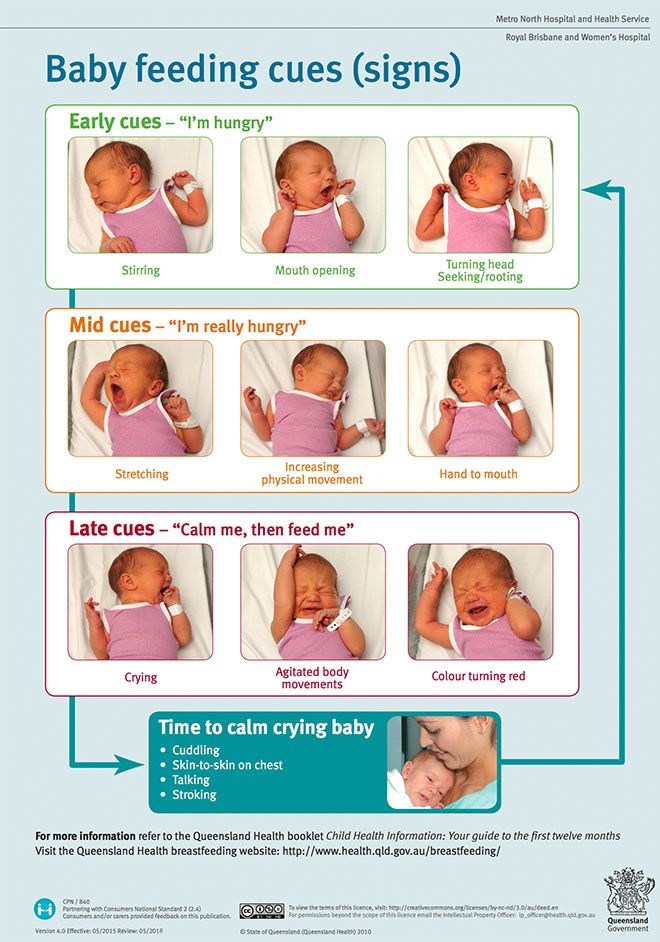 4 According to some mothers, this breastfeeding position is good to use from time to time for mastitis, when touching the breast is especially unpleasant. Some say that this breastfeeding position helps with blockage of the milk ducts, although there is no scientific evidence for this yet. You can also feed in the “overhanging” position while sitting, kneeling over the baby on a bed or sofa, as well as reclining on your stomach with support on your elbows. Pillows of various sizes that you can lean on will help you avoid back and shoulder strain.
4 According to some mothers, this breastfeeding position is good to use from time to time for mastitis, when touching the breast is especially unpleasant. Some say that this breastfeeding position helps with blockage of the milk ducts, although there is no scientific evidence for this yet. You can also feed in the “overhanging” position while sitting, kneeling over the baby on a bed or sofa, as well as reclining on your stomach with support on your elbows. Pillows of various sizes that you can lean on will help you avoid back and shoulder strain.
“I have breastfed several times in the 'overhang' position for clogged milk ducts when no other means of dissolving the blockage worked. And this pose seems to have helped. I think it's because of gravity, and also because the breasts were at a completely different angle than with normal feeding, and my daughter sucked her differently, ”says Ellie, a mother of two from the UK.
Feeding in the "overhanging" position is unlikely to be practiced regularly, but in some cases this position may be useful.
“I used to breastfeed in the overhang position when my baby was having trouble latch-on,” says Lorna, mother of two in the UK. - This, of course, is not the most convenient way, but then I was ready for anything, if only he could capture the chest. We succeeded and have been breastfeeding for eight months now!”
9. Feeding a baby in a sling or “on the fly”
Breastfeeding in a sling takes some practice, but you can go out, look after older children or even do a little household chores.
The sling is also useful if the baby does not like to lie down or is often attached to the breast. Lindsey, a mother of two in the US, notes: “I used the carrier frequently for both of my children. When we were out, I tied the sarong around my neck and covered the carrier with it. Under such a cape, the baby can eat as much as he wants until he falls asleep.
This breastfeeding position is best when the baby is already good at breastfeeding and can hold his head up by himself. Any slings are suitable for breastfeeding, including elastic and rings, as well as carrying bags. Whatever option you choose, the main thing is that you can always see the face of the child, and his chin does not rest against his chest.
Any slings are suitable for breastfeeding, including elastic and rings, as well as carrying bags. Whatever option you choose, the main thing is that you can always see the face of the child, and his chin does not rest against his chest.
10. Double hand-held breastfeeding
Double hand-held breastfeeding (or “double-ball grab”) is great for mothers of twins—you can breastfeed both at the same time, with your arms relatively free. 4 When feeding in this position, it is advisable to use a special pillow for breastfeeding twins, especially at first. It will provide extra support and help keep both babies in the correct position, as well as reduce the burden on the abdomen if you had a caesarean section. In addition, the hands are freer, and if necessary, you can deal with one child without interfering with the second.
“My twins were born very tiny and had to be fed every two hours at any time of the day or night. Very soon it became clear: if I want to do anything besides feeding, I need to feed them both at the same time, - says Emma, mother of two children from the UK. “I breastfed them two by hand using a breastfeeding pillow.”
“I breastfed them two by hand using a breastfeeding pillow.”
Other good positions for breastfeeding twins are two criss-cross cradles, one baby in the cradle and the other close at hand, reclining feeding, or sitting upright (one baby on one side, the other on the other).
11. Feeding in the position “with breast support by hand” or “hand of dancer”
muscle tone (which is typical for premature babies, children suffering from various diseases or Down syndrome), try supporting his head and your chest at the same time. 4 Grab your chest with your palm underneath so that your thumb is on one side and all the others are on the other. Move your hand slightly forward so that your thumb and forefinger form a "U" just in front of your chest. With the other three fingers, continue to support the chest. With your thumb and forefinger, hold the baby's head while feeding so that his chin rests on the part of the palm between them, your thumb gently holds the baby on one cheek, and your index finger on the other. So the baby gets excellent support, and you can control his position and see if he is holding his breast.
So the baby gets excellent support, and you can control his position and see if he is holding his breast.
Literature
1 Colson SD et al. Optimal positions for the release of primitive neonatal reflexes stimulating breastfeeding. Early Hum Dev . 2008;84(7):441-449. - Colson S.D. et al., "Optimal Positions for Provoking Primitive Innate Reflexes to Induce Breastfeeding." Early Hume Dev. 2008;84(7):441-449.
2 UNICEF UK BFHI [ Internet ]. Off to the best start ; 2015 [ cited 2018 Feb ]. - UNICEF UK, Baby-Friendly Hospital Initiative, Start the Best You Can [Internet]. 2015 [cited February 2018].
3 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment.