Best position to feed baby after c section
Breastfeeding After Cesarean Birth - La Leche League International
Breastfeeding after cesarean birth is an important way for you and baby to get to know each other. It can also help heal any feelings of sadness or disappointment if birth did not go as planned. Breastfeeding can give you the satisfaction of knowing that you are giving your newborn the very best—something no one else can do—even though you are recovering from major surgery.
Whether you give birth vaginally or by cesarean surgery, family, friends, or a La Leche League Leader can be of great assistance and support when you are beginning the breastfeeding experience.
Choosing a HospitalMake every attempt to choose a health care facility with current, evidence-based policies on breastfeeding. Maternity hospitals that have achieved designation as Baby-Friendly Hospitals™ (BFHI) are especially understanding and supportive of breastfeeding. Any barriers to early contact and exclusive breastfeeding will have a greater negative effect if you have a cesarean birth, because your hospital stay is usually longer after surgery.
Current research strongly supports placing your baby on your chest, skin-to-skin, immediately after birth[i], even after Cesarean surgery – right in the operating room or in the recovery area. In most cases, your baby will move toward your breast and begin breastfeeding within the first hour or so after birth by himself[ii]. There should be no clothing or blankets between your baby’s body and your body because immediate and uninterrupted direct skin-to-skin contact is important for both of you. The baby will be dried and kept warm with a blanket over her back during this skin-to-skin time.
Talk to your care providers during pregnancy about keeping baby skin-to-skin until after the first nursing. If you have complications during after the surgery, a family member can hold the baby skin to skin until you feel more stable, then the baby can begin or resume skin-to-skin contact with you. The maternity staff should offer help as needed.
Most babies can move to the breast and begin nursing all by themselves within the first hour or so after birth. If the baby is ill or unstable, she can be returned to you for skin-skin-contact and breastfeeding as soon as medically feasible. If the facility does not support immediate skin-to-skin policies, talk to your care providers and request that a medical order be written for immediate and uninterrupted skin-to-skin contact for at least an hour, or until after the baby’s first nursing.[iii]
If the baby is ill or unstable, she can be returned to you for skin-skin-contact and breastfeeding as soon as medically feasible. If the facility does not support immediate skin-to-skin policies, talk to your care providers and request that a medical order be written for immediate and uninterrupted skin-to-skin contact for at least an hour, or until after the baby’s first nursing.[iii]
If the birth facility is BFHI-designated, the staff will be trained and able to help you achieve your goal of early and exclusive breast feeding. All routine procedures including the baby’s first bath can be postponed until after the baby’s first nursing, or sometimes longer. The baby’s health will be checked thoroughly by the medical or nursing staff, which can often be done while the baby is resting on your body or in your arms.
Rooming InRooming-in, or the baby staying in your room around the clock, is now standard procedure in BFHI-designated hospitals and in most maternity facilities worldwide. If the hospital still has a central nursery, ask to have your baby remain with you as continually as possible, and ask the reasons for any routine separation. You and your baby will both rest, sleep and recover better if you are in the same room most of the time. Many hospitals now have ‘side-car’ devices, or little cribs that attach to the side of the adult bed. Side-car devices allow easy breastfeeding, yet provide a safe place for the baby to rest if the mother needs to move away for a while.
If the hospital still has a central nursery, ask to have your baby remain with you as continually as possible, and ask the reasons for any routine separation. You and your baby will both rest, sleep and recover better if you are in the same room most of the time. Many hospitals now have ‘side-car’ devices, or little cribs that attach to the side of the adult bed. Side-car devices allow easy breastfeeding, yet provide a safe place for the baby to rest if the mother needs to move away for a while.
- You and your baby will be more relaxed and comfortable when you stay together.
- Early and free access to nursing on your baby’s cues (BFHI Step 8) helps prevent breast and nipple problems, including engorgement and nipple pain.
- Often a baby born by cesarean is groggy from medications used during the surgery (although babies born vaginally are sometimes groggy, too). A groggy baby especially needs lots of skin-to-skin contact and gentle massage. Try to make sure he nurses at least every two hours.
- You are more aware of your baby’s sleeping and waking cycles, and can take advantage of his early feeding cues (eyes moving under his eyelids, hands coming to his face, alert and looking for you).
- Holding baby skin to skin is often all that’s needed for him to begin nursing well. A baby sleeping on your chest or close to you lets you respond to his cues quickly.
- When the baby is with you most of the time, you have more control over what happens to your baby and what the baby might be given. BFHI-designated hospitals have policies that prevent your baby being given a supplemental feed without a medical reason.
The early use of bottles with artificial nipples (teats) can interfere with baby’s ability to nurse effectively. Liquid tends to flow rapidly through a bottle nipple, whether baby sucks or not, which forces him to thrust his tongue forward to stop the flow of liquid to breathe. That’s the opposite motion of what happens in the baby’s mouth during breastfeeding. During nursing, the baby draws your nipple far back into his mouth and uses his tongue and jaw to wrap around your nipple and breast, and gather and swallow the milk. If supplemental fluids must be given, request use of a small cup instead of a bottle-and-teat system. None of the artificial nipples work like your breast.
During nursing, the baby draws your nipple far back into his mouth and uses his tongue and jaw to wrap around your nipple and breast, and gather and swallow the milk. If supplemental fluids must be given, request use of a small cup instead of a bottle-and-teat system. None of the artificial nipples work like your breast.
Pacifiers used in the early days also interfere with baby’s ability to learn how to breastfeed. There is no food in a pacifier – your baby’s need to suck is actually a need for food. In the early days, if your baby seems to ‘need to suck,’ it’s time to nurse again.
Types of AnestheticThe type of anesthetic used during cesarean surgery can directly affect breastfeeding. Except in the case when cesarean surgery in a true emergency, most mothers are given a regional anesthetic so that she is awake and aware during the birth. If there is any time to discuss your options, ask that your hospital gown, the IV tubing, blood pressure cuff and any other monitoring equipment be arranged so that your baby can be placed on your bare chest immediately after birth.
During the surgery, you will be lying on your back, and a drape is placed above your belly so that your hands (and nothing else) touches your abdomen. Some hospitals will agree to lower the drape briefly as your baby is lifted out of your body, so you can see most of the birth. After the baby’s umbilical cord is cut and he is dried gently, he can be brought around the drape and placed directly on your bare chest. The nurses will be monitoring you and your baby closely for safety. Your partner is usually allowed to be near you, and can also help watch your baby’s natural instincts emerge.
Newborns go through nine distinct stages [iv]after birth within the first hour or so:
- Birth cry: Intense crying just after birth
- Relaxation phase: Infant resting and recovering. No activity of mouth, head, arms, legs or body
- Awakening phase: Infant begins to show signs of activity. Small thrusts of head: up, down, from side-to-side. Small movements of limbs and shoulders
- Active phase: Infant moves limbs and head, is more determined in movements.
 Rooting activity, ‘pushing’ with limbs without shifting body
Rooting activity, ‘pushing’ with limbs without shifting body - Crawling phase: ‘Pushing’ which results in shifting body
- Resting phase: Infant rests, with some activity, such as mouth activity, sucks on hand
- Familiarization: Infant has reached areola ⁄nipple with mouth positioned to brush and lick areola ⁄nipple
- Suckling phase: Infant has taken nipple in mouth and commences suckling
- Sleeping phase: The baby has closed its eyes. Mother may also fall asleep.
If you are too shaky or ill to start skin-to-skin in the operating room, your partner may be able to hold your baby skin-to-skin until you feel better or in the recovery area. If a general anesthetic is used, you can start skin-to-skin when you are awake and responding normally. If your baby is premature or ill, she may be taken to an intensive care area (NICU) for advanced care. Your partner should be able to stay with your baby. Once you have recovered enough, you can reconnect with your baby.
Immediate and uninterrupted skin-to-skin contact allows your baby’s instinctive behavior to emerge. You can help and support your baby through the 9 stages, but don’t try to force the baby to the breast before she begins nursing on her own. When babies are allowed to move to the breast and self-attach, the chances of poor feeding on your baby’s part, and breast or nipple pain on your part, are drastically reduced. The first few nursing sessions are as important for immune protection and sensory stimulation as they are for nutrition. Your baby’s stomach is small at first, and your colostrum is made in just the right amount. Your baby doesn’t need any other fluids or supplements, as long as he is nursing well and often (8-12 times a day).
B
reastfeed early and often- Early and frequent skin-to-skin contact and breastfeeding t brings you and your baby emotionally closer.
- Early and frequent skin-to-skin and nursing releases hormones to contract the uterus to prevent or limit blood loss.
 You may find the contractions to be painful at first. If you need pain relief for incision pain or uterine cramping, those medications are compatible with breastfeeding. (see below)
You may find the contractions to be painful at first. If you need pain relief for incision pain or uterine cramping, those medications are compatible with breastfeeding. (see below)
- Ask the hospital staff for help in hand-expressing your milk, and ask for electric breast pump. If the baby can’t nurse right away, start hand-expressing within an hour or two after you give birth. Hand-expressing is better than pumping in the first 2 days. If the baby hasn’t nursed by about 6 hours, also ask for an electric breastpump.
- Pumping soon after birth and every couple of hours thereafter will normalize your milk production, prevent engorgement, and collect valuable colostrum and milk which can be given to your baby when he’s able to eat.
Medications used for pain relief after cesarean birth are usually compatible with breastfeeding. So are antibiotics and other medications which may be prescribed. If there is any question about a particular medication, a doctor can almost always prescribe a substitute that has been found safe to use while breastfeeding. Less than 1% of most medications passed into a mother’s milk, although there are variations to this. Most medications are compatible with breastfeeding, even during the newborn period.[v]
If there is any question about a particular medication, a doctor can almost always prescribe a substitute that has been found safe to use while breastfeeding. Less than 1% of most medications passed into a mother’s milk, although there are variations to this. Most medications are compatible with breastfeeding, even during the newborn period.[v]
At first, it may be difficult to find a comfortable position that allows baby to breastfeed without hurting your incision. Have your partner or other helper stay nearby to help move and position your baby during the early days.
Many mothers find breastfeeding while lying on their side the most comfortable during the first day or so. It’s also an easy way to nurse and rest at the same time.
- You and baby lie on your sides facing each other. Use pillows under your head, behind your back, and behind or between your knees to help get comfortable.
- Baby’s feet should be close to your body with your nipple mouth clear of the surface you’re lying on and at the height of baby’s mouth.

- Guide baby onto the breast using the hand of your upper arm on the baby’s upper back. Avoid pushing on the back of his head.
Another position that mothers find comfortable to use after a cesarean birth is called the underarm, football or clutch hold.
- Tuck baby’s body along your side under your arm.
- Support the breast with the other hand. If you’re nursing on the right breast, your left hand will be supporting the breast with the thumb above and well back from the nipple and the fingers below.
- Support baby’s head with your palm on baby’s upper back (not head), thumb behind one ear and index and other fingers behind the other ear.
- Baby’s body should be supported so that he is high enough and his nose is aligned with your nipple. He shouldn’t have to bend his neck forward to latch on—his head, neck, and hips should be in a straight line.
Let the baby ‘finish the first breast first.” Sometimes she will want the second side right away, or a bit later, or may only nurse on one breast at a time. It’s good to offer both breasts at each feeding, realizing some babies only take one breast per nursing. Let the baby finish at her own pace and do not limit baby’s time at the breast. Many babies nurse for about 10-30 minutes for a feed. Breastfed babies cannot overfeed. She will let go of the breast or fall asleep when satisfied. If you hold the baby after a nursing for about as long as the nursing session, she may move into a deeper sleep state. If you need to move away from the baby for a while, make sure she’s lying face-up on a firm, flat surface in a safe place within sight and sound of a responsible adult.
It’s good to offer both breasts at each feeding, realizing some babies only take one breast per nursing. Let the baby finish at her own pace and do not limit baby’s time at the breast. Many babies nurse for about 10-30 minutes for a feed. Breastfed babies cannot overfeed. She will let go of the breast or fall asleep when satisfied. If you hold the baby after a nursing for about as long as the nursing session, she may move into a deeper sleep state. If you need to move away from the baby for a while, make sure she’s lying face-up on a firm, flat surface in a safe place within sight and sound of a responsible adult.
It is important for your loved ones to realize that you need time to recover from childbirth and surgery, and to learn to breastfeed your baby.
While in the hospital, ask the nurse for a sign to put on your door several times a day to tell visitors that you are resting so that you do not have to entertain guests in your room all day long.
In the early weeks after arriving home, feel free to ask for and accept help from family and friends. They want to help, so ask them to do some of the usual household chores or bring prepared, healthy food. You don’t need a special diet to recover from surgery and birth. Continue to drink to thirst and eat nutritious foods to help regain your strength.
Breastfeeding should be comfortable. Learning a new skill often takes time, no matter how your baby arrived! If for any reason breastfeeding is not going smoothly or you find it painful to breastfeed, ask a La Leche League Leader for help.
[i] BFHI Step 4: “Help mothers initiate breastfeeding within one hour of birth.” World Health Organization, & United Nations Childrens Fund. (2009). Baby-Friendly Hospital Initiative: Revised, Updated and Expanded for Integrated Care. Geneva: World Health Organization.
[ii] Male and female pronouns referring to the baby are used randomly in this document.
[iii] Feldman-Winter, L. , & Goldsmith, J. P. (2016). Safe Sleep and Skin-to-Skin Care in the Neonatal Period for Healthy Term Newborns. Pediatrics, 138(3). doi: 10.1542/peds.2016-1889
, & Goldsmith, J. P. (2016). Safe Sleep and Skin-to-Skin Care in the Neonatal Period for Healthy Term Newborns. Pediatrics, 138(3). doi: 10.1542/peds.2016-1889
[iv] Widstrom, A. M., Lilja, G., Aaltomaa-Michalias, P., Dahllof, A., Lintula, M., & Nissen, E. (2011). Newborn behaviour to locate the breast when skin-to-skin: a possible method for enabling early self-regulation. Acta Paediatr, 100(1), 79-85.
[v] Sachs, H. C., & DRUGS, C. O. (2013). The Transfer of Drugs and Therapeutics Into Human Breast Milk: An Update on Selected Topics. Pediatrics. doi: 10.1542/peds.2013-1985
Published November 2017.
Breastfeeding After a C-Section: What Positions to Know
Icon of phone 1-844-867-9890
Check Your Insurance Eligibility
Toggle Nav
Search
Menu
Account
- By Aeroflow Breastpumps
- Sep 22, 2021
Everyone's breastfeeding experience is different. And there is no “one size fits all” guide, especially after having a cesarean section! But trying out different positions is essential to finding what's most comfortable for you and your baby and setting you up for breastfeeding success. Here are six IBCLC approved breastfeeding positions we recommend for mamas who have had a cesarean section.
And there is no “one size fits all” guide, especially after having a cesarean section! But trying out different positions is essential to finding what's most comfortable for you and your baby and setting you up for breastfeeding success. Here are six IBCLC approved breastfeeding positions we recommend for mamas who have had a cesarean section.
Football Hold:
An upright position to use while sitting with the baby off to the side where they are less likely to kick or rub against your incision. This one can only be used for a short period of time because your baby will physically outgrow it.
Cradle Hold:
A classic breastfeeding position where you sit upright with baby positioned on their side, with their head and neck laying along your forearm and their body against your stomach.
Cross-Cradle Hold:
Very similar to the cradle hold but your arms switch so that your baby’s body lies along your opposite forearm.
Side-Lying:
The side-lying position is the most critical position for any new c-section mama to learn as it allows for rest and recovery! C-section mothers should recline in a comfortable position to rest when possible, especially in the early days and weeks of c-section recovery, so reclining as you nurse is key.
Reverse Crawl:
Laying back and relaxing with your baby's body across your shoulder can be especially useful just after a cesarean birth (get help from your partner or family member) or during recovery if you can't find another position that you and your baby are comfortable in. This position can allow moms to have their baby skin-to-skin and breastfeed even while mom is still in the operating room.
Laid Back:
This is another well-known, popular breastfeeding position and can be great for c-section mamas as you try to recline, rest, and recover! Be sure to avoid weight and pressure on your wound site.
We encourage all breastfeeding mothers, regardless of if they had a cesarean delivery or vaginal birth, to try out different positions to figure out which ones are the most comfortable breastfeeding positions for them. The positions listed here are recommended by lactation consultants specifically for moms who need to be mindful of their incision site while recovering from major surgery. Breastfeeding can be tricky, but remember that there is a lot of breastfeeding support available! A lactation consultant can be a game-changer in helping you troubleshoot any breastfeeding issues you're having, and they can answer any questions you may have about colostrum during early breastfeeding, milk supply, how much breast milk your baby needs, engorgement, and anything else that may come up.
In addition to resting, postpartum compression garments can also help moms recovering from a c-section. They provide stability and support to the abdomen and can help with postpartum swelling. To speed up the healing process and protect the incision site, you may want to consider getting c-section bandages.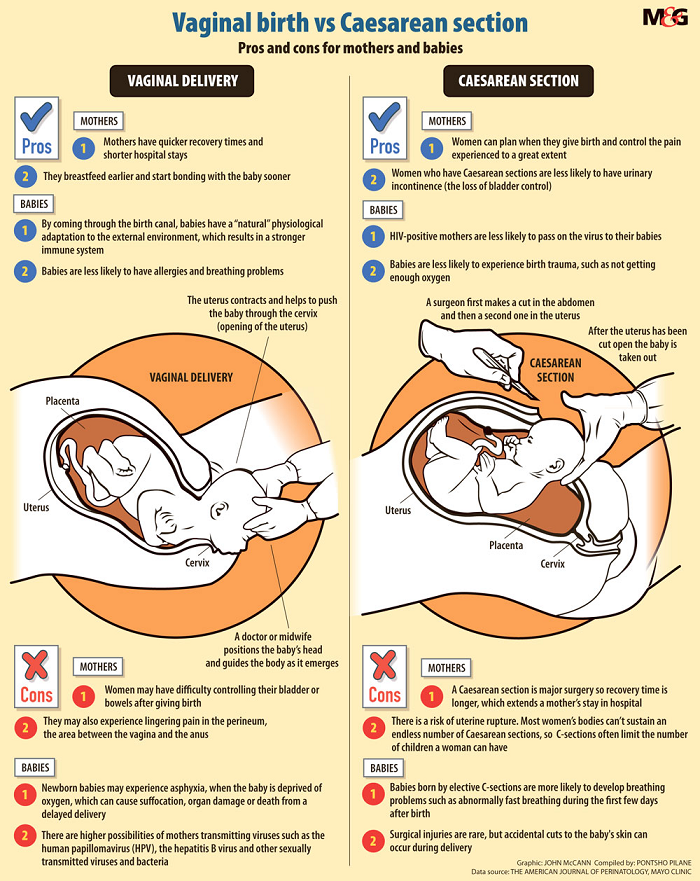 Aeroflow Breastpumps carries both of these items, and they may be covered by your insurance. These medical-grade items often require a prescription from your doctor to obtain through insurance. If maternity or postpartum compression could help you throughout your motherhood journey, be sure to fill out our quick and easy Qualify Through Insurance Form.
Aeroflow Breastpumps carries both of these items, and they may be covered by your insurance. These medical-grade items often require a prescription from your doctor to obtain through insurance. If maternity or postpartum compression could help you throughout your motherhood journey, be sure to fill out our quick and easy Qualify Through Insurance Form.
Remember that there are no right or wrong breastfeeding positions. Do what works best for you and your little one, and don't forget to rest!
Information provided in blogs should not be used as a substitute for medical care or consultation.
Postpartum Recovery How To's
Share:
Posted in Breastfeeding and Postpartum
Related Posts
Recent Posts
How to improve lactation after caesarean section
06/11/2021 Reading time: 5 min 62842
Less than half of babies in Russia up to six months of age are breastfed. Only a third of children receive it per year. These are the data of the Federal State Statistics Service.
Only a third of children receive it per year. These are the data of the Federal State Statistics Service.
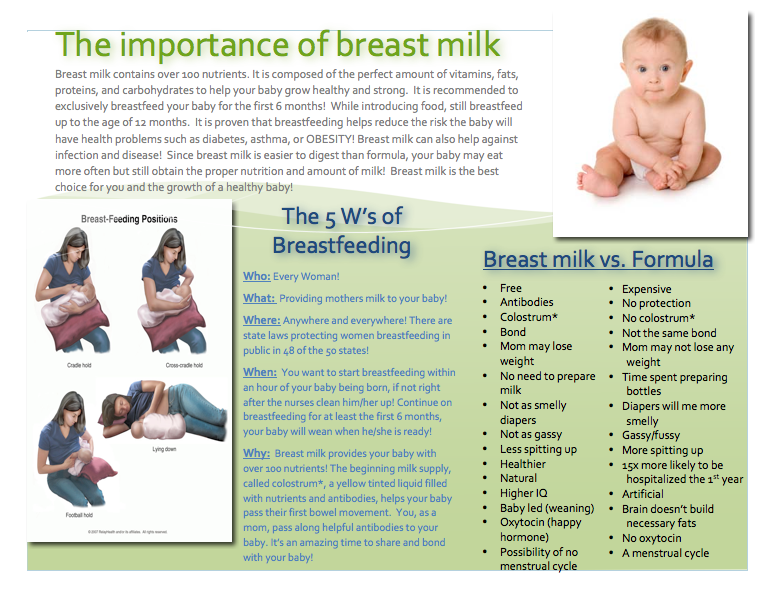
Meanwhile, a full-fledged replacement for breast milk has not yet been invented, and it is almost always possible to establish lactation if the mother and the newborn do not have serious illnesses.
This is important!
Even after a caesarean section, which in practice in 70% of cases leads to the introduction of formula supplementation already in the hospital, breastfeeding can be successfully started and continued for as long as the young mother and her baby need.
Why does caesarean section negatively affect lactation?
A caesarean section is not a reason to refuse breastfeeding, but it is objectively more difficult for mothers to establish lactation after this operation than for women who have given birth naturally.
- The organism of the expectant mother prepares for feeding the baby from the first days of pregnancy: the structure and size of the breast changes, in the second trimester the production of colostrum begins.
 Childbirth is the logical conclusion of this preparation. When a baby is born by caesarean section, the mechanism of lactation starts late, as its natural hormonal setting gets off.
Childbirth is the logical conclusion of this preparation. When a baby is born by caesarean section, the mechanism of lactation starts late, as its natural hormonal setting gets off. - In a newborn after a caesarean section, the sucking reflex may be weak at first, because the child did not pass through the birth canal and did not have time to adapt to the new conditions that suddenly appeared.
- The first application to the breast is possible in the first minutes after caesarean section, only if the operation was elective and was performed under epidural anesthesia. If a woman in labor needs an emergency CS, then it can be under general anesthesia. In this case, the first feeding can take place only a day after the operation. During this time, the child will already be fed with a mixture and it will be much more difficult to successfully establish lactation.
- After a caesarean section, a woman may be given antibiotics. Doctors usually prescribe medications that are compatible with breastfeeding, but complications sometimes require stronger medications.
 Then the mother will have to express milk regularly to maintain lactation until the end of the course of treatment. However, it is not a fact that the baby will prefer the breast to the familiar bottle with the mixture.
Then the mother will have to express milk regularly to maintain lactation until the end of the course of treatment. However, it is not a fact that the baby will prefer the breast to the familiar bottle with the mixture. - After the operation, a young mother may have difficulty recovering from anesthesia, experience weakness if there was a large blood loss. A painful stitch will make it difficult to find a comfortable feeding position. In this state, it takes a lot of determination to feed on demand, against all odds.
Despite the fact that a caesarean section creates additional difficulties in organizing breastfeeding, the mother can and should try to cope with them. This will help her save her own health and protect her baby.
Why fight to breastfeed?
- Breastfeeding reduces the risk of sudden infant death syndrome and strengthens the baby's immunity not only while he is breastfeeding, but for many years after.
- When breastfeeding, a correct bite is formed in a child, intelligence develops better, and the risk of obesity decreases.

- Long-term breastfeeding protects a mother from ovarian cancer, breast cancer, reduces the risk of developing type 2 diabetes in her.
- Breast milk is unique in composition: it changes during the day and the first year of life, adjusting to the needs of a particular child.
Tips on how to establish breastfeeding after caesarean section
- If you are having an elective caesarean section, talk to your doctor ahead of time and let them know that you would like to breastfeed. Discuss any points that make you anxious. Your mental attitude is just as important as your physical condition, so work on it and get support.
- Before the operation, ask that the baby be placed immediately on your breast, if possible, while still on the operating table.
- Insist on sharing the room with the newborn, even if you are offered to rest alone and bring the baby to feeds. The baby will feel protected next to you, and you can feed him on demand - then the milk will come faster and there will be more of it.

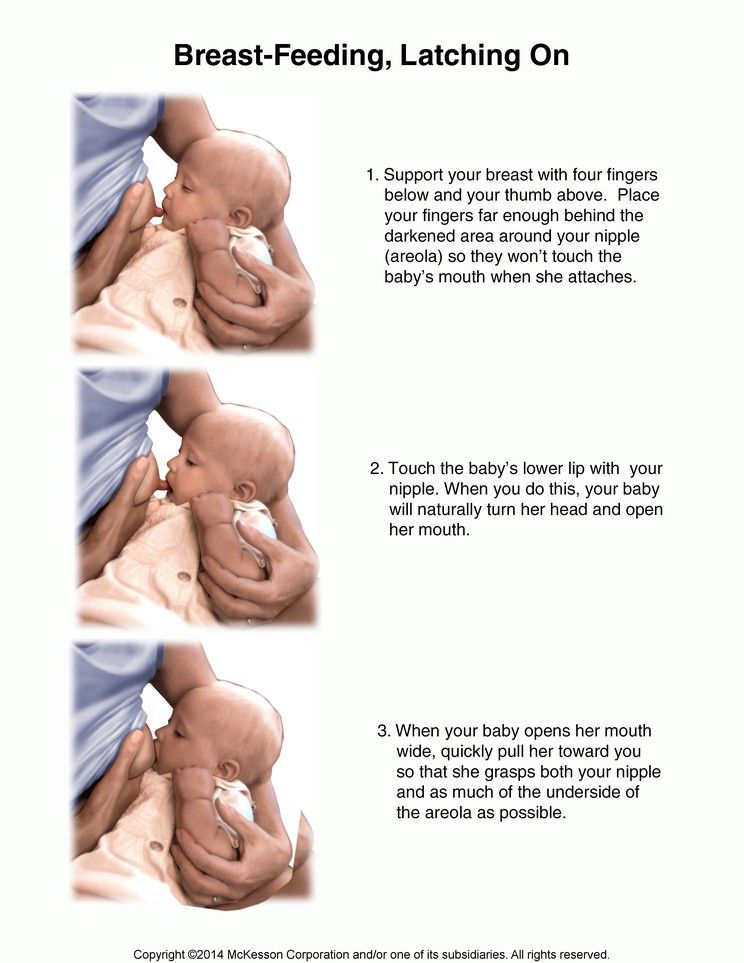
- Ask your midwife or pediatric nurse to show you how to properly latch on to your baby. The baby's mouth should be wide open, the lower lip turned inside out, the areola can be visible only above the upper lip, and completely hidden from below in the baby's mouth. If the baby does not take the breast correctly, he may remain hungry, and it will be painful for you to feed, cracked nipples may appear.
- Learn how to express by hand and, if necessary, with a breast pump. It will help to maintain lactation if, while taking medication, you will not be able to breastfeed for the first time.
- Do not give your baby a pacifier and a bottle with a nipple for at least the first month after birth, until lactation is fully established. Drink the mixture or medicine, if necessary, from a spoon or syringe.
So, a caesarean section is not a hindrance to breastfeeding, although it will be a little more difficult to establish lactation. Considering how beneficial breastfeeding is for the mother, and breast milk for the baby, you need to tune in to overcome difficulties. Successful breastfeeding after cesarean will be helped by the joint stay of mother and baby in the postpartum ward, on-demand feeding, the correct application technique and psychological support from both medical staff and loved ones.
Considering how beneficial breastfeeding is for the mother, and breast milk for the baby, you need to tune in to overcome difficulties. Successful breastfeeding after cesarean will be helped by the joint stay of mother and baby in the postpartum ward, on-demand feeding, the correct application technique and psychological support from both medical staff and loved ones.
(1 ratings; article rating 5.0)
Various breastfeeding positions
Try different breastfeeding positions to find the one that works best for you and your baby. You can see options in our selection of photos
Share this information
There is no right or wrong way to hold the baby while feeding
, and mom and baby are sure to find their favorite position.
It is important that both you and your child feel comfortable. 1.2 It's good to learn a few different breastfeeding positions and techniques because life's circumstances often require us to be flexible, especially as your baby gets older and you start to leave the house more often.
Whatever position you choose to breastfeed your baby, remember a few simple rules.
- Prepare everything you need before feeding, including drinks, food, mobile phone, TV remote control, book or magazine. And do not forget to go to the toilet - the feeding process can take a long time!
- Make sure your baby is comfortable. Whichever position you choose, it's important to keep your baby strong, level, and provide good support for their head, neck, and spine.
- You should also be comfortable. Don't stress. If necessary, use pillows of different sizes or rolls of towels to support your back or arms.
- Make sure your baby is latching on correctly. Proper grip is the key to comfort when breastfeeding.
- If your baby does not latch on well or you experience pain while feeding, contact a lactation consultant for help. The specialist will also be able to show you how to hold your baby more comfortably.
1. Relaxed feeding or reclining position
The relaxed feeding position, also known as biological feeding, 1 is often the first position for most mothers.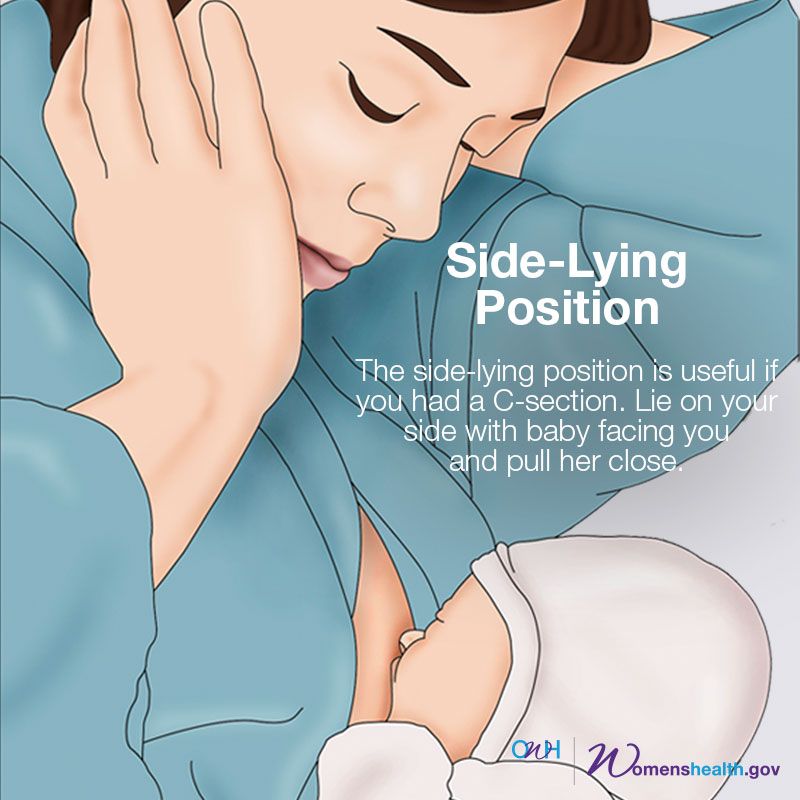 If, immediately after birth, the baby is placed on the mother’s chest or stomach, normally, he instinctively reaches for the breast and tries to grab the nipple. This phenomenon is known as the breast seeking reflex. Skin-to-skin contact stimulates the infant's feeding instinct, and gravity helps him to latch onto the breast and maintain balance.
If, immediately after birth, the baby is placed on the mother’s chest or stomach, normally, he instinctively reaches for the breast and tries to grab the nipple. This phenomenon is known as the breast seeking reflex. Skin-to-skin contact stimulates the infant's feeding instinct, and gravity helps him to latch onto the breast and maintain balance.
But it's not just newborns that can be fed in the reclining position - this position is great for babies of all ages. It can be especially helpful if your baby does not latch well in other positions or does not like to be touched during feeding, and also if you have too much milk flow or too large breasts. Isabelle, a mother from the UK, shares her experience: “I had large breasts, and the baby was born small - 2.7 kg, so it was not easy to find a comfortable position at first. After a few weeks, it became clear that there was no “correct” posture for me. As a result, I most often fed lying down, putting the baby on my chest. ”
It is more convenient to feed not lying flat on your back, but half-sitting, leaning on pillows. So you will have a back support and you will be able to watch the baby during feeding.
So you will have a back support and you will be able to watch the baby during feeding.
2. Cradle position
This is the classic
first thought of breastfeeding. Mom sits
straight, and the baby lies on her side on her arm, pressing her stomach against her stomach. 3 Although this is a very popular position, it is not always easy to master with newborns because it gives the baby less support. Try putting a pillow under your back, and put a special breastfeeding pillow on your knees and lean on it with your hands. So you can more reliably support the child, without overstraining your back and shoulders. Just make sure that the baby does not lie too high on the pillow for feeding. The breast should remain at a natural level so that the baby can grab it without effort, otherwise sore nipples cannot be avoided.
“I breastfed in the cradle position because it suited me perfectly! It was comfortable and I loved just sitting and looking at my little one,” recalls Rachel, a mother of two from Italy.
3. Cross Cradle
This breastfeeding position looks almost the same as Cradle, but the baby is on the other arm. 3 This gives your baby support around the neck and shoulders so he can tilt his head to latch on. This position is great for breastfeeding newborns and small babies, as well as for babies who do not latch well. Since the baby lies completely on the other hand, it becomes easier to control his position and you can adjust the chest with your free hand.
Julie, a UK mother of two, finds this position very practical: “I usually breastfeed my youngest in the cross cradle position. So I have a free second hand, and I can take care of an older baby at the same time. ”
Don't hold your baby's head at first, otherwise you might inadvertently press his chin against his chest. Because of this, the child will not be able to take the breast deeply, because the nipple will rest against the base of the tongue, and not against the palate, which will lead to inflammation of the nipples. As the child grows, this position becomes more comfortable, and he can rest his head on your palm (as shown in the photo above).
As the child grows, this position becomes more comfortable, and he can rest his head on your palm (as shown in the photo above).
4. Underarm breastfeeding
In this position, also known as the "ball grip", the mother sits and the baby lies along her arm at the side, legs towards the back of the chair (or any other seat). 3 Another comfortable position for newborn breastfeeding, you can give your baby good support, full control of the position and a good view of his face. And the baby feels safe in close contact with the mother's body. This position is especially good for those who have had a caesarean section or a premature birth, as well as mothers of twins and women with large breasts.
“When I breastfed my first daughter, I had very large K-sized breasts—twice the size of her head,” recalls Amy, an Australian mother of two. - I put rolls of towels under each breast, because they were very heavy, and fed my daughter in a pose from under the arm, but only sitting straighter so as not to crush her. This position was also convenient because I had a caesarean section and could not put the baby on my stomach.”
This position was also convenient because I had a caesarean section and could not put the baby on my stomach.”
5. Side-lying position
The side-lying position is ideal for relaxed
feeding at night in bed or on the couch. If you had a
caesarean section or ruptures during childbirth, this position may be more comfortable than sitting down. 3 In this position, mother and baby lie side by side, tummy to tummy.
“It was difficult for me to sit during endless night feedings, firstly because of the caesarean section, and secondly because of lack of sleep,” recalls Francesca, a mother from the UK. “And then I discovered that you can feed your baby lying on your side and rest at the same time.”
“Because of the short tongue frenulum, Maisie could only properly latch on to her breasts while lying on her side. The lactation consultant showed me how it's done. In this position, the flow of milk was optimal for my daughter, and it was easier for her to keep the nipple in her mouth. As she got older, she became much better at grabbing her breasts in normal positions,” says Sarah, mother of two from Australia.
As she got older, she became much better at grabbing her breasts in normal positions,” says Sarah, mother of two from Australia.
6. Relaxed breastfeeding after caesarean section
If you can't find a comfortable position for breastfeeding after caesarean section, 3 try to hold the baby on the shoulder in a reclining position – this does not put pressure on the postoperative suture and allows you to breastfeed the baby comfortably. You can also try side feeding.
7. Sitting upright breastfeeding or “koala pose”
When breastfeeding in an upright position or “koala pose”, the baby sits with a straight back and a raised head on the mother's hip. 4 This position can be tried even with a newborn if it is well supported, but it is especially convenient for feeding an older child who can already sit up by himself. The upright sitting position, or “koala pose,” is great for toddlers who suffer from reflux or ear infections and feel better sitting.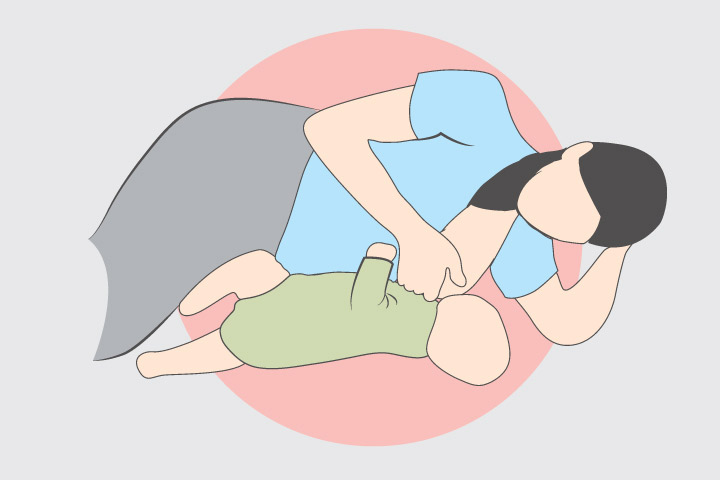 In addition, this pose may be suitable for children with a shortened frenulum of the tongue or reduced muscle tone.
In addition, this pose may be suitable for children with a shortened frenulum of the tongue or reduced muscle tone.
“When my daughter got a little older, I often fed her in an upright position, which was more comfortable for both of us, and I could still hold her close to me,” recalls Peggy, a mother from Switzerland. “Besides, it was possible to discreetly breastfeed her in public places.”
8. Overhanging position
In this position, the baby lies on his back, and the mother bends over him
on all fours so that the nipple falls directly into his mouth. 4 Some moms say this breastfeeding position is good to use from time to time for mastitis, when touching the breasts is especially unpleasant. Some say that this breastfeeding position helps with blockage of the milk ducts, although there is no scientific evidence for this yet. You can also feed in the “overhanging” position while sitting, kneeling over the baby on a bed or sofa, as well as reclining on your stomach with support on your elbows. Pillows of various sizes that you can lean on will help you avoid back and shoulder strain.
Pillows of various sizes that you can lean on will help you avoid back and shoulder strain.
“I have breastfed several times in the overhang position for clogged milk ducts when no other means of resolving the blockage worked. And this pose seems to have helped. I think it's because of gravity, and also because the breasts were at a completely different angle than with normal feeding, and my daughter sucked her differently, ”says Ellie, a mother of two from the UK.
Feeding in the "overhanging" position is unlikely to be practiced regularly, but in some cases this position may be useful.
“I used to breastfeed in the overhang position when my baby was having trouble latch-on,” says Lorna, mother of two in the UK. - This, of course, is not the most convenient way, but then I was ready for anything, if only he could capture the chest. We succeeded and have been breastfeeding for eight months now!”
9. Feeding a baby in a sling or "on the fly"
Breastfeeding in a sling takes some practice, but you can go out, look after older children or even do a little household chores.
The sling is also useful if the baby does not like to lie down or is often attached to the breast. Lindsey, a mother of two in the US, notes: “I used the carrier frequently for both of my children. When we were out, I tied the sarong around my neck and covered the carrier with it. Under such a cape, the baby can eat as much as he wants until he falls asleep.
This breastfeeding position is best when the baby is already good at breastfeeding and can hold its head up by itself. Any slings are suitable for breastfeeding, including elastic and rings, as well as carrying bags. Whatever option you choose, the main thing is that you can always see the face of the child, and his chin does not rest against his chest.
10. Double hand-held breastfeeding
Double hand-held breastfeeding (or “double-ball grab”) is great for mothers of twins—you can breastfeed both at the same time and still have relatively free hands. 4 When feeding in this position, it is advisable to use a special pillow for breastfeeding twins, especially at first. It will provide extra support and help keep both babies in the correct position, as well as reduce the burden on the abdomen if you had a caesarean section. In addition, the hands are freer, and if necessary, you can deal with one child without interfering with the second.
It will provide extra support and help keep both babies in the correct position, as well as reduce the burden on the abdomen if you had a caesarean section. In addition, the hands are freer, and if necessary, you can deal with one child without interfering with the second.
“My twins were born very tiny and had to be fed every two hours at any time of the day or night. Very soon it became clear: if I want to do anything besides feeding, I need to feed them both at the same time, - says Emma, mother of two children from the UK. “I breastfed them two by hand using a breastfeeding pillow.”
Other comfortable positions for breastfeeding twins are two criss-cross cradles, one baby in the cradle and the other close at hand, reclining or sitting upright feeding (one baby on one side, the other on the other).
11. Breastfeeding in the “hand-supported” or “dancer's hand” position
muscle tone (which is typical for premature babies, children suffering from various diseases or Down syndrome), try supporting his head and your chest at the same time. 4 Grab your chest with your palm underneath so that your thumb is on one side and all the others are on the other. Move your hand slightly forward so that your thumb and forefinger form a "U" just in front of your chest. With the other three fingers, continue to support the chest. With your thumb and forefinger, hold the baby's head while feeding so that his chin rests on the part of the palm between them, your thumb gently holds the baby on one cheek, and your index finger on the other. So the baby gets excellent support, and you can control his position and see if he is holding his breast.
4 Grab your chest with your palm underneath so that your thumb is on one side and all the others are on the other. Move your hand slightly forward so that your thumb and forefinger form a "U" just in front of your chest. With the other three fingers, continue to support the chest. With your thumb and forefinger, hold the baby's head while feeding so that his chin rests on the part of the palm between them, your thumb gently holds the baby on one cheek, and your index finger on the other. So the baby gets excellent support, and you can control his position and see if he is holding his breast.
Literature
1 Colson SD et al. Optimal positions for the release of primitive neonatal reflexes stimulating breastfeeding. Early Hum Dev . 2008;84(7):441-449. - Colson S.D. et al., "Optimal Positions for Provoking Primitive Innate Reflexes to Induce Breastfeeding." Early Hume Dev. 2008;84(7):441-449.
2 UNICEF UK BFHI [ Internet ].











