Breastfeeding and formula feeding baby
Breastfeeding vs. Formula Feeding (for Parents)
Choosing whether to breastfeed or formula feed their baby is one of the biggest decisions expectant and new parents will make.
Healt experts believe breast milk is the best nutritional choice for infants. But breastfeeding may not be possible for all women. For many, the decision to breastfeed or formula feed is based on their comfort level, lifestyle, and specific medical situations.
For moms who can't breastfeed or who decide not to, infant formula is a healthy alternative. Formula provides babies with the nutrients they need to grow and thrive.
Some mothers worry that if they don't breastfeed, they won't bond with their baby. But the truth is, loving mothers will always create a special bond with their children. And feeding — no matter how — is a great time to strengthen that bond.
The decision to breastfeed or formula feed your baby is a personal one. Weighing the pros and cons of each method can help you decide what is best for you and your baby.
All About Breastfeeding
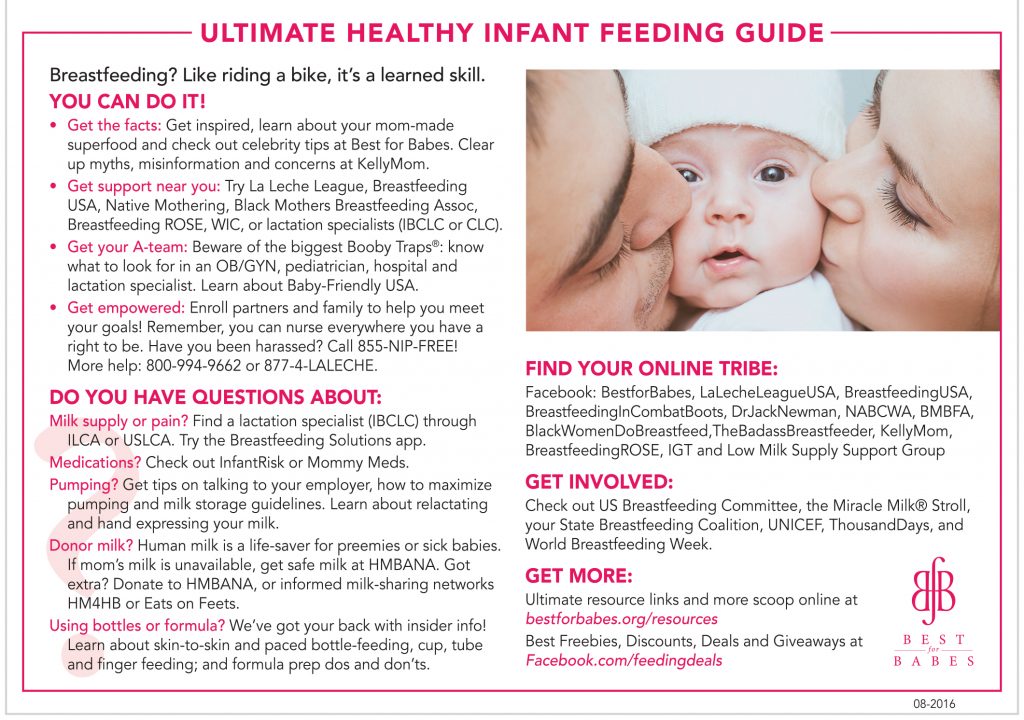
Nursing can be a wonderful experience for both mother and baby. It provides ideal nourishment and a special bonding experience that many mothers cherish.
A number of health organizations — including the American Academy of Pediatrics (AAP), the American Medical Association (AMA), and the World Health Organization (WHO) — recommend breastfeeding as the best choice for babies. Breastfeeding helps defend against infections, prevent allergies, and protect against a number of chronic conditions.
The AAP recommends that babies be breastfed exclusively for the first 6 months. Beyond that, breastfeeding is encouraged until at least 12 months, and longer if both the mother and baby are willing.
Here are some of the many benefits of breastfeeding:
Fighting infections and other conditions. Breastfed babies have fewer infections and hospitalizations than formula-fed infants. During breastfeeding, antibodies and other germ-fighting factors pass from a mother to her baby and strengthen the immune system. This helps lower a baby's chances of getting many infections, including:
This helps lower a baby's chances of getting many infections, including:
- ear infections
- diarrhea
- respiratory infections
- meningitis
Breastfeeding also may protect babies against:
- allergies
- asthma
- diabetes
- obesity
- sudden infant death syndrome (SIDS)
Breastfeeding is particularly beneficial for premature babies.
Nutrition and ease of digestion. Often called the "perfect food" for a human baby's digestive system, breast milk's components — lactose, protein (whey and casein), and fat — are easily digested by a newborn.
As a group, breastfed infants have less difficulty with digestion than do formula-fed infants. Breast milk tends to be more easily digested so that breastfed babies have fewer bouts of diarrhea or constipation.
Breast milk also naturally contains many of the vitamins and minerals that a newborn requires. One exception is vitamin D — the AAP recommends that all breastfed babies begin receiving vitamin D supplements during the first 2 months and continuing until a baby consumes enough vitamin D-fortified formula or milk (after 1 year of age).
The U.S. Food and Drug Administration (FDA) regulates formula companies to ensure they provide all the necessary nutrients (including vitamin D) in their formulas. Still, commercial formulas can't completely match breast milk's exact composition. Why? Because milk is a living substance made by each mother for her individual infant, a process that can't be duplicated in a factory.
Free. Breast milk doesn't cost a cent, while the cost of formula quickly adds up. And unless you're pumping breast milk and giving it to your baby, there's no need for bottles, nipples, and other supplies that can be costly. Since breastfed babies are less likely to be sick, that may mean they make fewer trips to the doctor's office, so fewer co-pays and less money are paid for prescriptions and over-the-counter medicines.
Different tastes. Nursing mothers usually need 300 to 500 extra calories per day, which should come from a wide variety of well-balanced foods. This introduces breastfed babies to different tastes through their mothers' breast milk, which has different flavors depending on what their mothers have eaten. By tasting the foods of their "culture," breastfed infants more easily accept solid foods.
This introduces breastfed babies to different tastes through their mothers' breast milk, which has different flavors depending on what their mothers have eaten. By tasting the foods of their "culture," breastfed infants more easily accept solid foods.
Convenience. With no last-minute runs to the store for more formula, breast milk is always fresh and available whether you're home or out and about. And when women breastfeed, there's no need to wash bottles and nipples or warm up bottles in the middle of the night.
Smarter babies. Some studies suggest that children who were exclusively breastfed have slightly higher IQs than children who were formula fed.
"Skin-to-skin" contact. Many nursing mothers really enjoy the experience of bonding so closely with their babies. And the skin-to-skin contact can enhance the emotional connection between mother and infant.
Beneficial for mom, too. The ability to totally nourish a baby can help a new mother feel confident in her ability to care for her baby. Breastfeeding also burns calories and helps shrink the uterus, so nursing moms may be able to return to their pre-pregnancy shape and weight quicker. Also, studies show that breastfeeding helps lower the risk of breast cancer, high blood pressure, diabetes, and cardiovascular disease, and also may help decrease the risk of uterine and ovarian cancer.
Breastfeeding also burns calories and helps shrink the uterus, so nursing moms may be able to return to their pre-pregnancy shape and weight quicker. Also, studies show that breastfeeding helps lower the risk of breast cancer, high blood pressure, diabetes, and cardiovascular disease, and also may help decrease the risk of uterine and ovarian cancer.
p
Breastfeeding Challenges
Breastfeeding can be easy from the get-go for some mothers, but take a while to get used to for others. Moms and babies need plenty of patience to get used to the routine of breastfeeding.
Common concerns of new moms, especially during the first few weeks and months, may include:
Personal comfort. Initially, many moms feel uncomfortable with breastfeeding. But with proper education, support, and practice, most moms overcome this.
Latch-on pain is normal for the first week to 10 days, and should last less than a minute with each feeding. But if breastfeeding hurts throughout feedings, or if their nipples and/or breasts are sore, it's a good idea for breastfeeding mothers to get help from a lactation consultant or their doctor. Many times, it's just a matter of using the proper technique, but sometimes pain can mean that something else is going on, like an infection.
Many times, it's just a matter of using the proper technique, but sometimes pain can mean that something else is going on, like an infection.
Time and frequency of feedings. Breastfeeding requires a big time commitment from mothers, especially in the beginning, when babies feed often. A breastfeeding schedule or the need to pump breast milk during the day can make it harder for some moms to work, run errands, or travel.
And breastfed babies do need to eat more often than babies who take formula, because breast milk digests faster than formula. This means mom may find herself in demand every 2 or 3 hours (maybe more, maybe less) in the first few weeks.
Diet. Women who are breastfeeding need to be aware of what they eat and drink, since these can be passed to the baby through the breast milk. Just like during pregnancy, breastfeeding women should not eat fish that are high in mercury and should limit consumption of lower mercury fish.
If a mom drinks alcohol, a small amount can pass to the baby through breast milk. She should wait at least 2 hours after a single alcoholic drink to breastfeed to avoid passing any alcohol to the baby. Caffeine intake should be kept to no more than 300 milligrams (about one to three cups of regular coffee) or less per day because it can cause problems like restlessness and irritability in some babies.
She should wait at least 2 hours after a single alcoholic drink to breastfeed to avoid passing any alcohol to the baby. Caffeine intake should be kept to no more than 300 milligrams (about one to three cups of regular coffee) or less per day because it can cause problems like restlessness and irritability in some babies.
Maternal medical conditions, medicines, and breast surgery. Medical conditions such as HIV or AIDS or those that involve chemotherapy or treatment with certain medicines can make breastfeeding unsafe. A woman should check with her doctor or a lactation consultant if she's unsure if she should breastfeed with a specific condition. Women should always check with the doctor about the safety of taking medicines while breastfeeding, including over-the-counter and herbal medicines.
Mothers who've had breast surgery, such as a reduction, may have difficulty with their milk supply if their milk ducts have been severed. In this situation, a woman should to talk to her doctor about her concerns and work with a lactation specialist.
p
All About Formula Feeding
Commercially prepared infant formulas are a nutritious alternative to breast milk, and even contain some vitamins and nutrients that breastfed babies need to get from supplements.
Manufactured under sterile conditions, commercial formulas attempt to duplicate mother's milk using a complex combination of proteins, sugars, fats, and vitamins that aren't possible to create at home. So if you don't breastfeed your baby, it's important to use only commercially prepared formula and not try to make your own.
Besides medical concerns that may prevent breastfeeding, for some women, breastfeeding may be too difficult or stressful. Here are other reasons women may choose to formula feed:
Convenience. Either parent (or another caregiver) can feed the baby a bottle at any time (although this is also true for women who pump their breast milk). This allows mom to share the feeding duties and helps her partner to feel more involved in the crucial feeding process and the bonding that often comes with it.
Flexibility. Once the bottles are made, a formula-feeding mother can leave her baby with a partner or caregiver and know that her little one's feedings are taken care of. There's no need to pump or to schedule work or other obligations and activities around the baby's feeding schedule. And formula-feeding moms don't need to find a private place to nurse in public.
Time and frequency of feedings. Because formula is less digestible than breast milk, formula-fed babies usually need to eat less often than breastfed babies.
Diet. Women who opt to formula feed don't have to worry about the things they eat or drink that could affect their babies.
page 7
Formula Feeding Challenges
As with breastfeeding, there are some challenges to consider when deciding whether to formula feed.
Lack of antibodies. None of the antibodies found in breast milk are in manufactured formula. So formula can't provide a baby with the added protection against infection and illness that breast milk does.
Can't match the complexity of breast milk. Manufactured formulas have yet to duplicate the complexity of breast milk, which changes as the baby's needs change.
Planning and organization. Unlike breast milk — which is always available, unlimited, and served at the right temperature — formula feeding your baby requires planning and organization to make sure that you have what you need when you need it. Parents must buy formula and make sure it's always on hand to avoid late-night runs to the store.
And it's important to always have the necessary supplies (like bottles and nipples) clean, easily accessible, and ready to go — otherwise, you will have a very hungry, very fussy baby to answer to. With 8-10 feedings in a 24-hour period, parents can quickly get overwhelmed if they're not prepared and organized.
Expense. Formula can be costly. Powdered formula is the least expensive, followed by concentrated, with ready-to-feed being the most expensive. And specialty formulas (such as soy and hypoallergenic) cost more — sometimes far more — than the basic formulas. During the first year of life, the cost of basic formula can run about $1,500.
And specialty formulas (such as soy and hypoallergenic) cost more — sometimes far more — than the basic formulas. During the first year of life, the cost of basic formula can run about $1,500.
Possibility of producing gas and constipation. Formula-fed babies may have more gas and firmer bowel movements than breastfed babies.
Making a Choice
Deciding how you will feed your baby can be a hard decision. You'll really only know the right choice for your family when your baby comes.
Many women decide on one method before the birth and then change their minds after their baby is born. And many women decide to breastfeed and supplement with formula because they find that is the best choice for their family and their lifestyle.
While you're weighing the pros and cons, talk to your doctor or lactation consultant. These health care providers can give you more information about your options and help you make the best decision for your family.
How to combine breast and bottle feeding
It can take several weeks for you and your baby to feel happy and confident with breastfeeding.
Once you've both got the hang of it, it's usually possible to offer your baby bottles of expressed milk or formula alongside breastfeeding.
This is sometimes called mixed or combination feeding.
Why combine breast and bottle?
You may want to combine breastfeeding with bottle feeding if you:
- are breastfeeding and want to use a bottle to offer your baby some expressed breast milk
- want to breastfeed for some of your baby's feeds, but give bottles of formula for 1 or more feeds
- are bottle feeding your baby and want to start breastfeeding
- need to leave your baby and want to make sure they have some milk while you're away
Introducing formula feeds can affect the amount of breast milk you produce. There is also a small amount of evidence to show babies may not breastfeed as well because they learn to use a different kind of sucking action at the bottle than at the breast.
These things can make breastfeeding more difficult, especially in the first few weeks when you and your baby are still getting comfortable with breastfeeding.
Your breastmilk supply will usually not be affected if you start bottle feeding your baby when they are a bit older, you are both comfortable with breastbeeding, and you breastfeed every day.
Introducing formula feeds
If you're combining breastfeeding with formula feeds both you and your baby can carry on enjoying the benefits of breastfeeding.
If you choose to introduce infant formula:
- it's best to do it gradually to give your body time to reduce the amount of milk it makes – this helps lower your chance of getting uncomfortable, swollen breasts, or mastitis
- if you're going back to work, start a few weeks beforehand to give both of you time to readjust
- if your baby is 6 months old or more and can drink milk from a cup, you may not need to introduce a bottle at all
For more information, see drinks and cups for babies.
Giving your baby their first bottle
It may take a while for a breastfed baby to get the hang of bottle feeding, because they need to use a different sucking action.
- it usually helps to give the first few bottles when your baby is happy and relaxed – not when they're very hungry
- it may help if someone else gives the first bottle feeds, so that your baby is not near you and smelling your breast milk
- you might want to try using a different position for bottle and breastfeeding
See more advice on how to bottle feed.
Restarting breastfeeding
If you want to start breastfeeding more and give your baby fewer bottles, it's a good idea to ask your midwife, health visitor or breastfeeding supporter for support.
These tips may help too:
- Hold and cuddle your baby as much as possible, ideally skin to skin. This will encourage your body to make milk and your baby to feed.
- Express your breast milk regularly. Expressing releases the hormone prolactin, which stimulates your breasts to make milk. About 8 times a day, including once at night is ideal. It may be easier to express by hand to begin with – your midwife, health visitor or breastfeeding supporter can show you how.
- Try bottlefeeding while holding your baby skin to skin and close to your breasts.
- If your baby is latching on, feed little and often. Do not worry if your baby does not feed for long to begin with. See tips on how to get your baby properly positioned and attached.
- Choose times when your baby is relaxed, alert and not too hungry, and do not force your baby to stay at the breast.
- Decrease the number of bottles gradually, as your milk supply increases.
- Consider using a lactation aid (supplementer). A tiny tube is taped next to your nipple and passes into your baby's mouth so your baby can get milk via the tube as well as from your breast. This helps to support your baby as they get used to attaching to the breast. Your midwife, health visitor or breastfeeding supporter can give you more information.
See more tips on boosting your milk supply.
Help and support with mixed feeding
If you have any questions or concerns about combining breast and bottle feeding:
- talk to your midwife, health visitor or breastfeeding supporter
- call the National Breastfeeding Helpline on 0300 100 0212 (9.
 30am to 9.30pm, every day)
30am to 9.30pm, every day) - find breastfeeding support near you
Video: why combine breast and bottle feeding?
In this video, 3 mothers discuss ways to combine breast and bottle feeding.
Media last reviewed: 22 March 2020
Media review due: 22 March 2023
Page last reviewed: 8 October 2019
Next review due: 8 October 2022
Breastfeeding and its benefits for the normal development of the infant.
Mother's milk is a natural biological product that provides physiologically adequate nutrition for babies. This is the "gold standard" of early childhood nutrition, and far from all aspects of its multifaceted influence have been studied.
A breastfed mother can follow different dietary patterns for her baby. Free feeding, or "on demand" feeding, is the diet of a child of the first year of life, when the mother puts the child to the breast as many times and at the time as the child requires, including at night. The duration of feeding is also determined by the child. It is more often carried out in the first months of life and with exclusive breastfeeding. Regulated feeding is such a diet of a child when feedings are carried out at more or less fixed hours, the frequency and volume of feedings is recommended by the doctor, taking into account the age, body weight, appetite and individual characteristics of the child. It is more often carried out after 1-2 months of life, especially with the option of mixed feeding. The duration of feeding of newborns ranges from 20 to 30 minutes, and for children older than 1 month - from 10 to 20 minutes. The water requirement of children in the first months of life is satisfied by breast milk with a sufficient level of lactation, so they do not need additional drinking.
The duration of feeding is also determined by the child. It is more often carried out in the first months of life and with exclusive breastfeeding. Regulated feeding is such a diet of a child when feedings are carried out at more or less fixed hours, the frequency and volume of feedings is recommended by the doctor, taking into account the age, body weight, appetite and individual characteristics of the child. It is more often carried out after 1-2 months of life, especially with the option of mixed feeding. The duration of feeding of newborns ranges from 20 to 30 minutes, and for children older than 1 month - from 10 to 20 minutes. The water requirement of children in the first months of life is satisfied by breast milk with a sufficient level of lactation, so they do not need additional drinking.
The criteria for a sufficient level of lactation are normal daily diuresis (600-700 ml), weight gain adequate to the age of the child and psychomotor development. If you suspect a lack of milk, you should determine the daily volume of lactation using control weighing and compare it with the calculated one, take measures to restore lactation or introduce supplementary feeding.
Breast milk is the most complex biologically active substance with unique properties:
- regulation of the processes of growth, development and differentiation of tissues;
- anti-infective protection;
- formation of immunological tolerance to dietary antigens;
- influence on the formation of the maxillofacial skeleton, speech, hearing;
- prevention of obesity, diabetes, atherosclerosis;
- beneficial effect on mental and behavioral responses, intelligence, learning ability and social adaptation;
- reduced risk of cancer in the mother, contraceptive effect in the first months of lactation.
Breast milk provides anti-inflammatory (antioxidants, enzymes that break down pro-inflammatory neurotransmitters, anti-inflammatory cytokines) and immunomodulatory substances (live CD4 and CD8 lymphocytes, nucleotides, IgA, cytokines IL-2, IL-10, IL-12, etc., soluble cytokine receptors). Breastfeeding and the state of the intestinal microflora play a key role in maintaining a balance in the Thh Th3, Th4 cytokine system. Thanks to the bifidogenic properties of human milk, a complete intestinal microbiota of the child is formed, innate immunity and protective mechanisms of the intestinal mucosa are activated, and the immune response matures.
Thanks to the bifidogenic properties of human milk, a complete intestinal microbiota of the child is formed, innate immunity and protective mechanisms of the intestinal mucosa are activated, and the immune response matures.
Digestive system:
- One of the main advantages of women's milk is the proximity of its proteins in terms of qualitative composition to blood serum proteins. Breast milk contains mainly finely dispersed, that is, consisting of the smallest particles, albumin proteins, which are easily absorbed in the child's digestive tract.
Digestibility, completeness of absorption of women's milk proteins reaches 98-99%, for cow's milk proteins this figure is much less. The main protein component of cow's milk is casein, the content of which is up to ten times higher than that in human breast milk. Casein, being a large and aggressive soluble protein, is able to penetrate the intestinal walls, forcing the child's body to produce an endogenous inflammatory mediator - histamine. What can cause both intestinal bleeding, which is fraught with the subsequent development of anemia, and various kinds of allergic reactions.
What can cause both intestinal bleeding, which is fraught with the subsequent development of anemia, and various kinds of allergic reactions.
- The residence time of food in the gastrointestinal tract of the baby with natural and artificial feeding is also different. The child's stomach is freed from food after 2-3 hours with breastfeeding, and with artificial feeding - after 3-4 hours. Thus, artificial feeding puts a lot of stress on the digestive tract and on the baby's body as a whole.
- The activity of the enzyme lipase, which is responsible for the breakdown of fat in the gastrointestinal tract of the child, is much higher in human breast milk. Due to the activity of maternal lipase, a high degree of fat dispersion is achieved, which facilitates their further absorption and assimilation. As a result of the action of breast milk lipase, there is a significantly lower load on the pancreas and liver of the baby, the organs responsible for the digestion of fat
- Women's milk contains 5-6 times more linoleic acid. With a lack of this polyunsaturated fatty acid, a child may experience a delay in physical development, metabolism is disturbed, and adverse changes in the condition of the skin are possible.
With a lack of this polyunsaturated fatty acid, a child may experience a delay in physical development, metabolism is disturbed, and adverse changes in the condition of the skin are possible.
Immune system:
- The most important advantage of mother's milk in comparison with its artificial substitutes is the presence in it of a large group of substances that protect the child's body from infections. These are secretory immunoglobulin A - sIgA, interferon, lysozyme, lactoferrin, bifidus factor, cells of the immune system.
- Immunoglobulin A is contained in secrets (fluids) on the surface of mucous membranes in contact with the external environment - lungs, nasal cavity, gastrointestinal tract, urinary tract. Maternal secretory immunoglobulin A provides protection against infection of the vital organs and systems of the child.
- Human milk lactoferrin plays an exceptional role in protecting the baby from viral infections, preventing the penetration of viral particles through the cell membrane, thus preventing infection from entering the baby's body. In addition to the antiviral action, lactoferrin also has antibacterial properties. Many microorganisms contain receptors for lactoferrin on their surface, and the binding of lactoferrin to the corresponding receptor leads to the death of a foreign bacterial cell. Lactoferrin has a bactericidal effect against a large number of gram-positive and gram-negative bacteria.
In addition to the antiviral action, lactoferrin also has antibacterial properties. Many microorganisms contain receptors for lactoferrin on their surface, and the binding of lactoferrin to the corresponding receptor leads to the death of a foreign bacterial cell. Lactoferrin has a bactericidal effect against a large number of gram-positive and gram-negative bacteria.
- the bifidus factor of human milk is represented by a whole complex of various sugars (oligosaccharides) and their monomers: beta-lactose, galactooligosaccharides, D-glucose, D-galactose, N-acetylglucosamines, L-fucose and sialic acids. The bifidus factor of human milk stimulates the formation of the intestinal microflora, mainly consisting of bifidobacteria (B. Bifidum) and lactobacilli. Normal intestinal microflora lines the intestinal crypts like a blanket, creating a protective layer that prevents foreign bacteria and allergens from entering the baby's circulatory system. Also, bifido- and lactobacilli create a favorable intra-intestinal environment with a shift in the pH of the contents of the colon to the acid side, which inhibits the growth of pathogenic and conditionally pathogenic bacteria and promotes the absorption of iron, calcium, vitamin D and other micro- and macroelements; participates in the synthesis of vitamins B1, B2, B3, PP, B6, B12, folic acid, biotin. In addition, the normal intestinal microflora makes the baby's immunity stronger.
In addition, the normal intestinal microflora makes the baby's immunity stronger.
At present, using the latest scientific methods, the existence of oligosaccharides containing up to 32 sugar fragments and up to 15 fructose fragments has been established. This means that the number of different types of oligosaccharides in human breast milk can reach several tens of thousands of units. Naturally, even modern artificial mixtures containing prebiotics (industrial analogues of the bifidus factor) cannot be compared in quality and variety with breast milk.
Urinary system:
- The formation of the child's urinary system and the development of its functions takes place in the first year of life. In an infant at the time of birth, the plasma flow and the process of formation of primary urine by filtering plasma in the renal glomeruli are reduced, osmotic concentration of urine is not effective enough. The main indicators of kidney function come to the level of an adult by the beginning of the second year of life.
 Therefore, it is very important that the load on the kidneys, depending on the content of proteins and mineral salts in the food taken, be adequate to the physiological age of the child.
Therefore, it is very important that the load on the kidneys, depending on the content of proteins and mineral salts in the food taken, be adequate to the physiological age of the child. - The protein level in women's milk averages from 0.8 to 1.2 g / 100 ml, while even in the adapted ready-made milk formula this figure is 40 - 70% higher and is 1.4 - 1, 6 g/100 ml. The increased content of proteins increases the load on the glomerular apparatus of the kidney.
- Another problem with milk mixtures is their normalization by mineral composition. Excess salt can overload the kidneys and cause thirst, which is reflected in the addition of water to formula-fed babies.
- Many pediatricians still recommend giving babies about 100 ml of water daily to avoid dehydration. However, at present, the World Health Organization and UNICEF insist that there is no need for supplementation and the introduction of any foreign liquids and products before the child reaches the age of 6 months.

- What is the basis for these recommendations? If breastfeeding is organized correctly (the mother feeds the baby on demand, approximately every 1.5 - 2 hours, keeping night feedings), then the baby receives enough water from milk in the first six months of life.
This section describes only the main advantages of breastfeeding.
Is there any benefit from breastfeeding for the mother and does this process affect the “usual” way of life?
The benefits for the mother can be divided into three groups:
1. Health benefits
- Breastfeeding within the first hour after birth significantly reduces the risk of postpartum uterine bleeding.
- Breastfeeding maintains a high level of hormones (oxytocin and prolactin) in the blood of the mother, which contributes to the formation of strong maternal feelings.
- If a woman breastfeeds her baby exclusively, then in the first 4-6 months after birth, the probability of pregnancy is reduced by 95%.
- Long-term breastfeeding reduces the risk of breast cancer by 50%, and if a mother breastfeeds multiple children, breastfeeding each child reduces the risk of ovarian cancer by 25%. Also, women who breastfeed for a long time are less likely to suffer from osteoporosis.\
2. Economic benefits
- You don't need to buy breast milk, you don't need additional accessories - nipples, sterilizers, heaters, breast pumps, which you still need to run around and choose exactly those that fit the size and shape of your breasts.
- Savings on artificial mixtures, which are not cheap at all.
3. Breastfeeding is convenient
From a practical point of view, breastfeeding makes life easier for mothers. Breast milk is always sterile, at the ideal temperature and composition, requires no preparation, and is always fresh and ready to drink. It is convenient that a mother can feed a child in any conditions: in transport, at a party, in nature - in those places where preparing baby food is difficult and dangerous due to infection.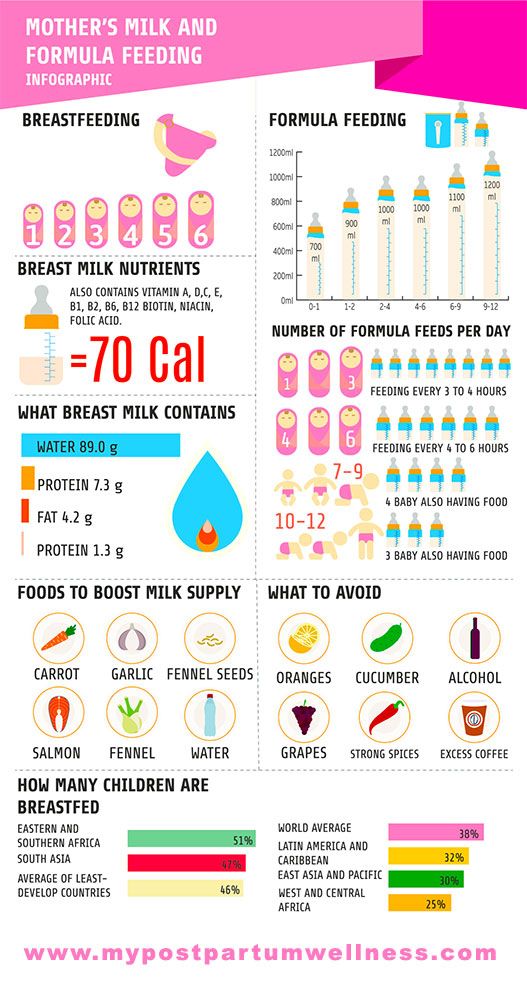
Undoubtedly, breastfeeding has its own difficulties, however, it depends only on you whether your child will receive the benefits necessary for life: good health, an adequate level of physical and mental development, social adaptation in society.
Doctor -pediatrician of the highest category
Motina Irina Vyacheslavovna
Breastfeeding is the key to future health. Articles
Home \ Articles \ Breastfeeding is the key to future health.
| « Back The annual World Breastfeeding Support Week was held in our city in the first week of August. The slogan for World Breastfeeding Week 2016 is " Breastfeeding is more than just nutrition ". Rational feeding of infants is the key to their adequate growth and development, as well as a high quality of life both in early childhood and in subsequent years. The optimal food product for a child in the first months of life is mother's milk, which corresponds to the characteristics of its digestive system and metabolism, ensuring adequate development of the child's body with a rational diet of a nursing woman. Due to the presence of antibodies, immune complexes, active leukocytes, lysozyme, macrophages, secretory immunoglobulin A, lactoferrin and other biologically active substances, breast milk increases the protective functions of the child's body. Therefore, breastfed children are much less likely to suffer from infectious diseases and develop more stable post-vaccination immunity. Breastfeeding reduces the risk of developing diseases such as atherosclerosis, hypertension, diabetes mellitus, obesity, leukemia, etc. in subsequent years. Cases of sudden death are less frequently recorded in breastfed children. Natural feeding has a beneficial effect on the development of the central nervous system of the child and his mental status. There are several factors that contribute to lactation. The most important of them is the early attachment of the child to the mother's breast, which ensures the rapid activation of the mechanisms of milk secretion and more stable subsequent lactation. Evaluation of the adequacy of lactation requires a thorough analysis of the child's behavior, the nature of the stool, the frequency of urination. Possible signs of insufficient lactation are:
Significant signs of malnutrition are low weight gain and infrequent urination (less than 6 times a day). |

 All nutrients in human milk are easily digestible, as their composition and ratio correspond to the functionality of the gastrointestinal tract of the infant. Breast milk is a source of hormones and various growth factors that play an important role in the regulation of appetite, metabolism, growth and differentiation of tissues and organs of the child.
All nutrients in human milk are easily digestible, as their composition and ratio correspond to the functionality of the gastrointestinal tract of the infant. Breast milk is a source of hormones and various growth factors that play an important role in the regulation of appetite, metabolism, growth and differentiation of tissues and organs of the child.  The bonding between mother and child during breastfeeding has a profound mutual emotional impact. It is noted that children who were fed with mother's milk are distinguished by harmonious physical development, they are more calm, balanced, friendly and benevolent compared to children who were bottle-fed, and later they themselves become attentive and caring parents. According to some data, children who are breastfed have a higher IQ.
The bonding between mother and child during breastfeeding has a profound mutual emotional impact. It is noted that children who were fed with mother's milk are distinguished by harmonious physical development, they are more calm, balanced, friendly and benevolent compared to children who were bottle-fed, and later they themselves become attentive and caring parents. According to some data, children who are breastfed have a higher IQ.