Common food allergies in breastfed babies
Is your Baby Reacting to Breastmilk?
Read time: 8 minutes
What should I know about an allergy or intolerance in my breastfed baby?Learn the difference between an allergy and a food intolerance or sensitivity
Know the signs and symptoms of food allergy or intolerance in breastfed infants
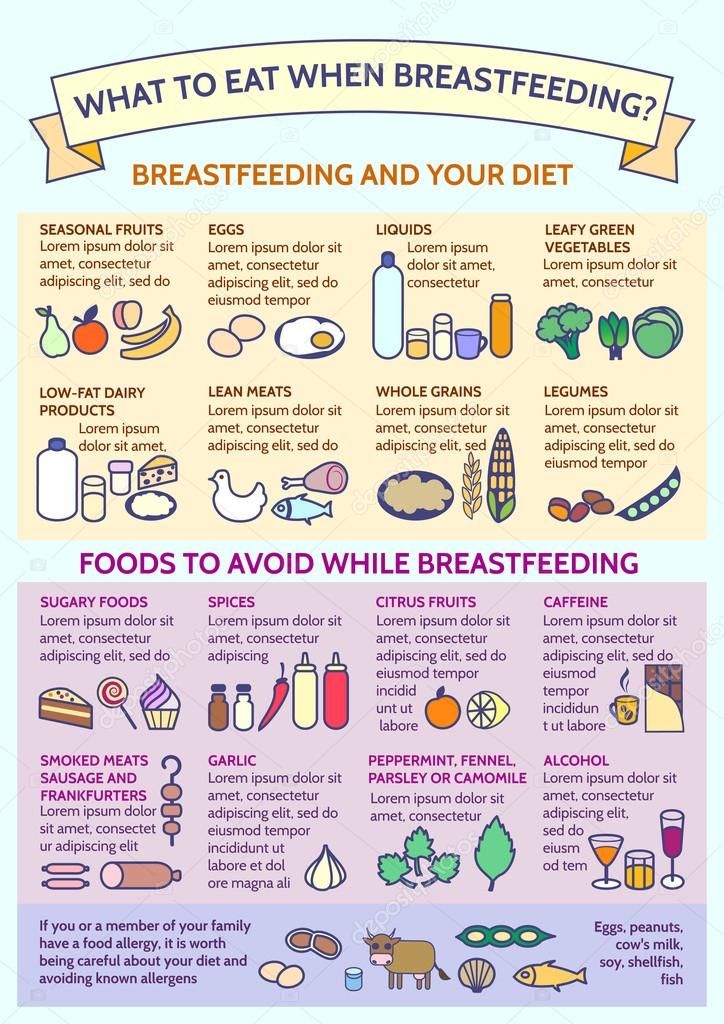
Learn which foods are the most common allergens or culprits in food intolerances
How to manage your food intake to help alleviate your baby’s symptoms
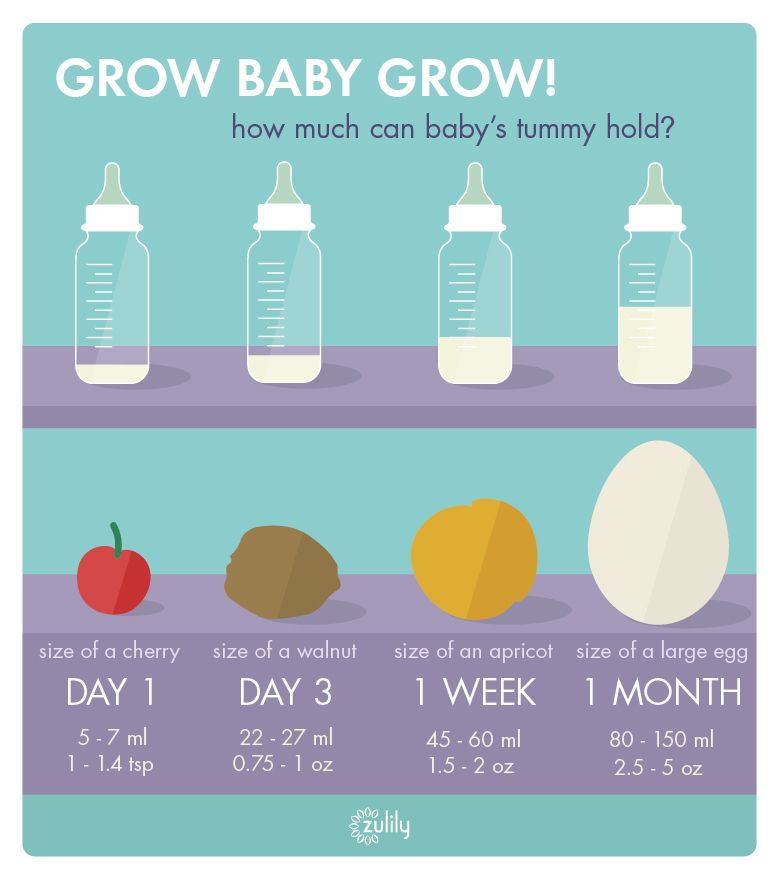
Breastmilk is incredible – it offers a complete form of nutrition for infants, and offers a range of benefits for health, growth, immunity, and development.1 The nutrients in your breastmilk come directly from what’s circulating in your blood, meaning that the nutrients and compounds you absorb from the food you eat are then passed along to your baby.
While being truly allergic or reacting to something in mom’s milk is rare in babies, a small percentage of mothers do notice a difference in their babies’ symptoms or behavior after eating certain foods.
Sometimes these terms are used interchangeably, but an allergy and an intolerance/ sensitivity are very different. According to the American Academy of Allergy Asthma and Immunology (AAAI), an allergy is when the immune system reacts to a food, whereas an intolerance happens during digestion.2
Allergies generally have more severe symptoms, often causing skin reactions or difficulty breathing. Food intolerances occur when we have difficulty digesting a food, which often result in gastro-intestinal symptoms.
With an allergy, the culprit food often needs to be taken out of the diet completely to avoid symptoms.
Food intolerances however may allow for a small amount of the offending food to be eaten without any reactions. This is the ‘threshold’ amount: the lowest amount of the food you can eat without having symptoms.
Read more: Am I Able to Reduce the Risk of Allergies for my Baby while I’m Pregnant and Breastfeeding?
Which foods might cause an allergic reaction?In general, food allergens include cow’s milk, soy, eggs, peanuts, wheat, tree nuts, fish, and shellfish. 3
3
In children, the most common allergens are peanuts, milk, tree nuts, and shellfish.4,5
What are the symptoms of a food allergy in babies?Food allergies affect about 7.6% of children in the United States.4
The most common symptoms of an allergy in breastfed infants are eczema (a scaly, red skin rash) and bloody stool (with no other signs of illness). You might also see hives, wheezing or other breathing problems, nasal congestion, swelling of a body part (tongue, lips, face), throat tightness, pale skin, vomiting or diarrhea.6
If you notice any of these symptoms, be sure to call baby’s pediatrician right away. While you can likely manage most food allergies in your breastfed infant by changing your diet, there are some cases in which using a hypoallergenic formula may be required.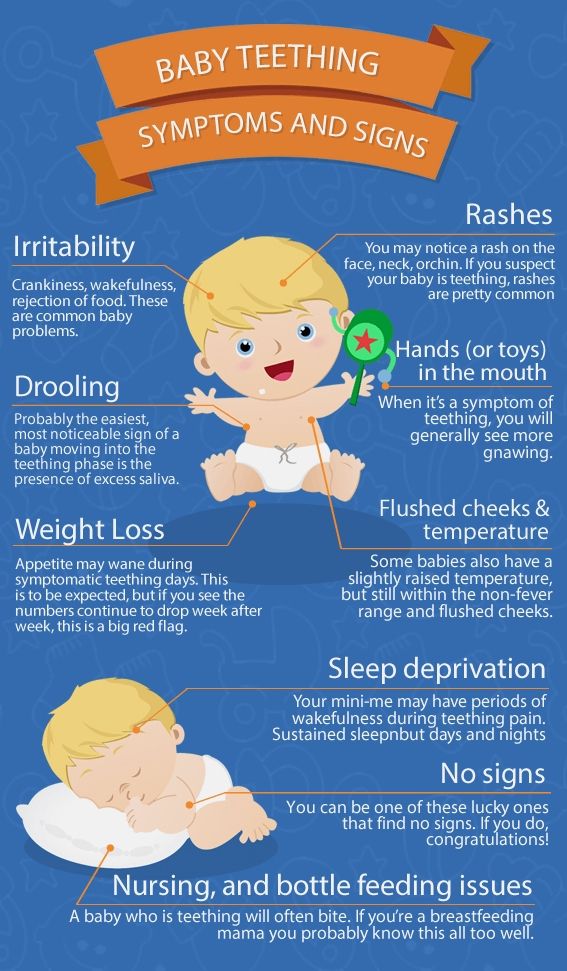
Learn about: How Do I Manage Gas in My Breastfed Baby?
Which foods might cause a food intolerance or sensitivity reaction?You may have heard that eating foods that make you gassy will also cause gastrointestinal distress for your baby, or that eating foods like onion, garlic and cruciferous vegetables will cause colic. While there is no significant data to support such an association, there are some mothers who do notice certain foods make their babies fussier than usual. This may be a food intolerance or sensitivity.
There is a much wider variety of foods that may trigger a reaction when it comes to food intolerances; but it’s important to note that food sensitivities in babies are much less common than food allergies.
Foods that may cause reactions include: Fructose, lactose and other FODMAPs (easily fermented carbohydrates found in a variety of foods), wheat, histamine (often found in processed meats, cheeses, and some produce), and food additives.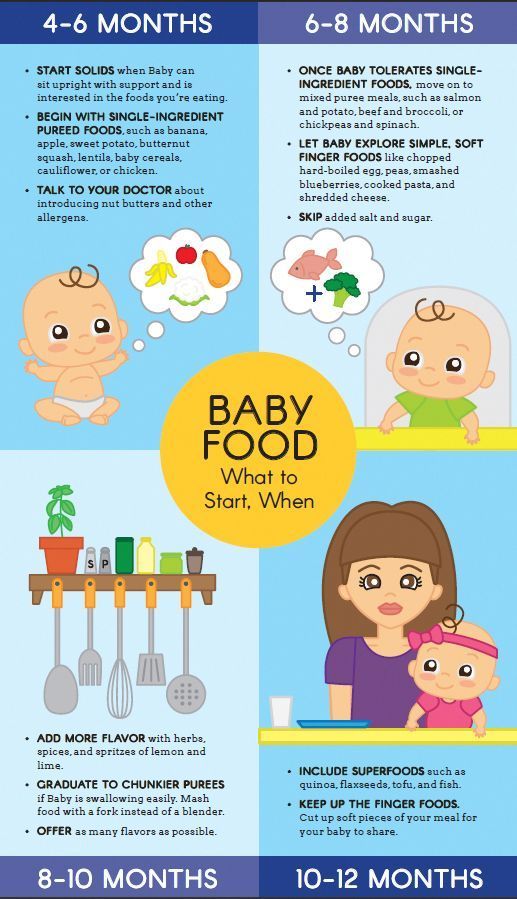 7
7
The most common symptom of a food sensitivity in babies is a change in their bowel habits. Extra gas, bloating, diarrhea or constipation, fussy after eating, mucous in the stool, or crying excessively may indicated baby is not doing well with a food you’re eating.
Note that if your little one has excessive crying that continues on a daily basis and lasts for long periods, that may indicate colic rather than food sensitivity.8 Talk with your pediatrician about this possibility.
Read more: How Can I Manage My Baby's Colic?
What can I do if my baby is reacting to something in my diet?The ultimate goal is figuring out which food is affecting your baby. An elimination diet can help identify which food may be causing the allergy or food sensitivity.9 This means removing possible allergens from your diet for 2 to 3 weeks each while you continue breastfeeding.
If you plan on trying an elimination diet, especially a multi-food elimination, be sure to work with a registered dietitian nutritionist. This will help ensure you are still getting all the nutrition you and your baby need as well as help navigate hidden sources of allergens. Foods like milk, soy, and corn can hide in all sorts of pesky places.
It’s important to add a food back into your diet if no symptoms in your baby improve within a few weeks of eliminating it. If your baby’s symptoms has not improved, it is likely that the food is not the culprit.
Our Happy Baby Experts are registered dietitian nutritionists and infant feeding specialists, they can help you meet your breastfeeding goals while keeping both you and baby happy and healthy. Chat with them now!
Trying to figure out what to eat while also taking out all allergens? Here are some ideas: Meal Plan for Allergen Free Eating while Breastfeeding
Does breastfeeding help protect against allergies?While more research is needed, some studies have indicated that breastfeeding exclusively for at least four months may help to reduce the risk and severity of food allergies, even in families with a history of them. 11,12
11,12
So if your little one does show an intolerance or allergy early, know that it may resolve on its own before they turn one and that continued breastfeeding may help to safeguard against allergies later on.
What should I do if baby is reacting to my breastmilk?Contact your infant's pediatricianBring your baby in for a checkup. You’ll want to rule out any other causes for her symptoms, check baby’s growth and weight gain, and make sure baby is not losing excessive blood if your little one experiencing bloody stool. Your doctor can also discuss the possibility of confirming the presence of an allergy with a skin prick test.
If your child is diagnosed with a food allergy, remember to ask about reintroducing the food later. Most kids will grow out of food allergies, sometimes by their first birthday.
Keep a food and symptom journalWe know it’s hard to find time to eat in those first few months, let alone write down what made it into your mouth, but tracking your intake alongside your baby’s symptoms is a good way to shed light on any possible reactions.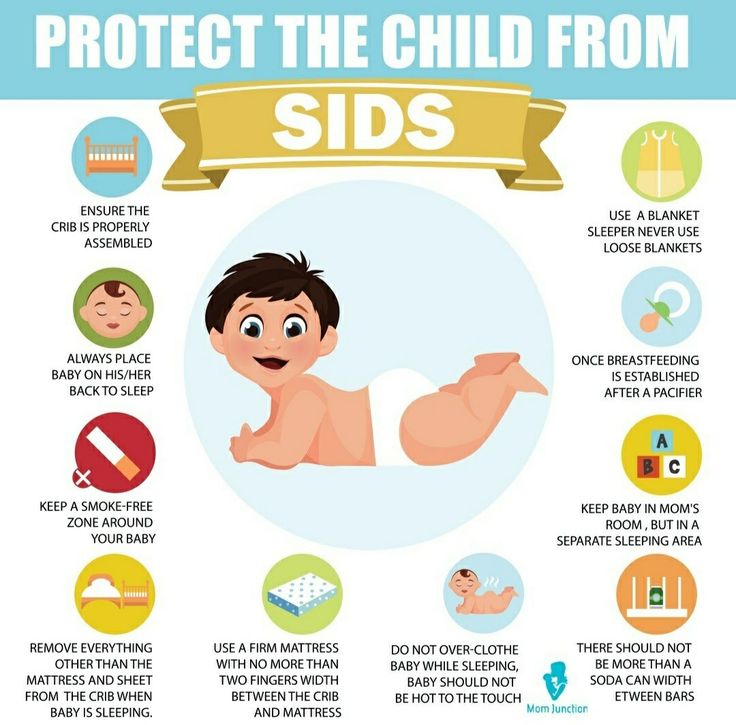
Just remember that foods we eat may remain in our bodies for long periods of time. So while a journal can be helpful to pinpoint the onset of symptoms when you first eat the offending food, know that your baby’s symptoms can persist for several days, even if you don’t eat that particular food again.
Consider eliminating specific foodsIf you notice an adverse reaction in your baby after you eat certain foods, try removing that food from your diet and watch for improvement.
You may want to start with cow’s milk, as the most frequent allergic reaction in breastfed babies is a milk protein allergy.5 Remember, it takes time for your body to be completely free of the offending food, so make sure you’ve removed all sources of the food for at least two weeks.
Always speak with your health care provider before attempting to eliminate foods from your diet. Work closely with a registered dietitian nutritionists during this process to ensure you maintain a balanced diet and are getting all the nutrients you and your baby need.
Be sure to add foods back in when their elimination does not seem to impact your baby’s symptoms.
Seek supportChanging your diet can be hard. Finding a registered dietitian nutritionist who can help make adjustments to your diet will help take some stress out of this process. Additionally, may lactation consultants are familiar with helping make these adjustments as well and also ensuring baby is getting what they need.
Let’s Chat!We know parenting often means sleepless nights, stressful days, and countless questions and confusion, and we want to support you in your feeding journey and beyond.
Our Happy Baby Experts are a team of lactation consultants and registered dietitian nutritionist certified in infant and maternal nutrition – and they’re all moms, too, which means they’ve been there and seen that. They’re here to help on our free, live chat platform Monday through Friday, from 8am–6pm (ET). Chat Now!
Read more about the experts that help write our content!
For more on this topic, check out the following articles:How to Deal with Nursing Strikes while Breastfeeding
How much Should I Eat while Breastfeeding?
How do I Manage Gas in my Breastfeed Baby?
Which Foods Should You Avoid While Breastfeeding?
Allergies & Food Intolerances - La Leche League GB
Babies can be unsettled for many reasons and it can sometimes take time and effort to work out the cause. Our page The Unhappy Breastfed Baby can help you determine whether your baby’s behaviour is due to something other than an allergy.
Our page The Unhappy Breastfed Baby can help you determine whether your baby’s behaviour is due to something other than an allergy.
But when you have ruled out most of the obvious causes and your baby is still, unhappy, colicky, experiencing dry and itchy skin or passing mucousy stools you may wonder whether they could be reacting to something in their diet or environment, or something in your own diet.
Certain medical conditions can have symptoms similar to those of an allergic reaction. It may be wise to rule these out before deciding whether a baby’s symptoms are due to an allergy or food intolerance.
A baby’s immune system is immature at birth.
Colostrum, or early milk, is rich in antibodies, particularly secretory IgA (SIgA), which provide a protective coating inside a baby’s intestines1. Mature breastmilk continues to provide protection, helping to prevent potential allergens from reaching a baby’s blood.
Exclusive breastfeeding generally helps to protect against allergy but it may still occur.
If any immediate family member ( siblings or parents) has an allergy eczema, hay fever or asthma, it makes it more likely that the baby could develop allergies2.
Food intolerance
A food intolerance does not involve an allergic reaction but can cause similar symptoms. It occurs when a baby has difficulty digesting a particular food. You may not need to stop giving your baby a food to which he is intolerant—reducing the amount may be enough.
Food allergy
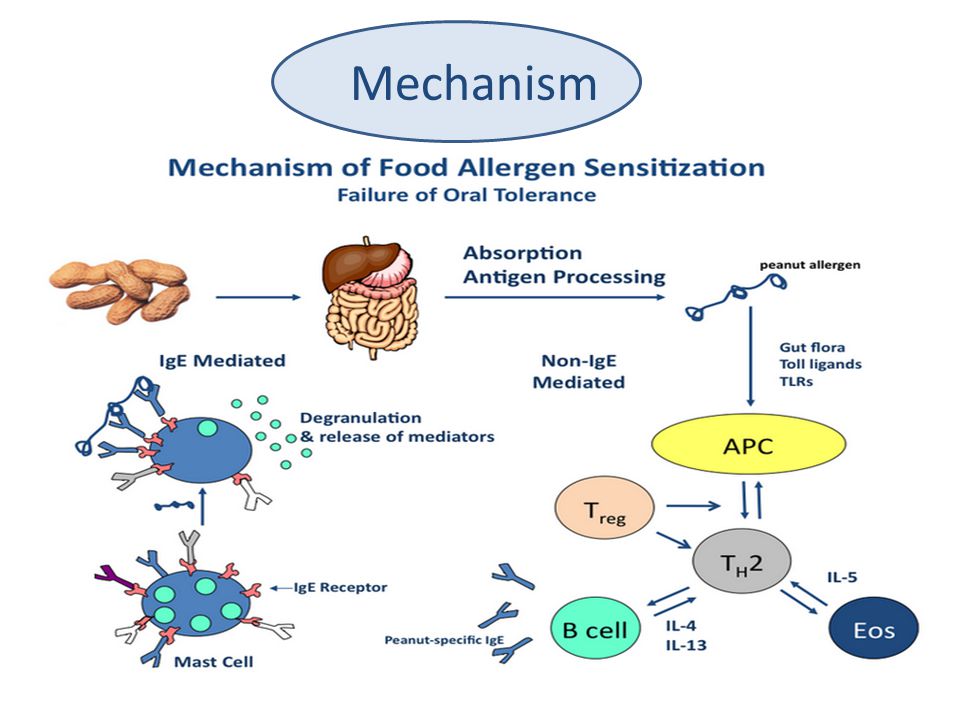
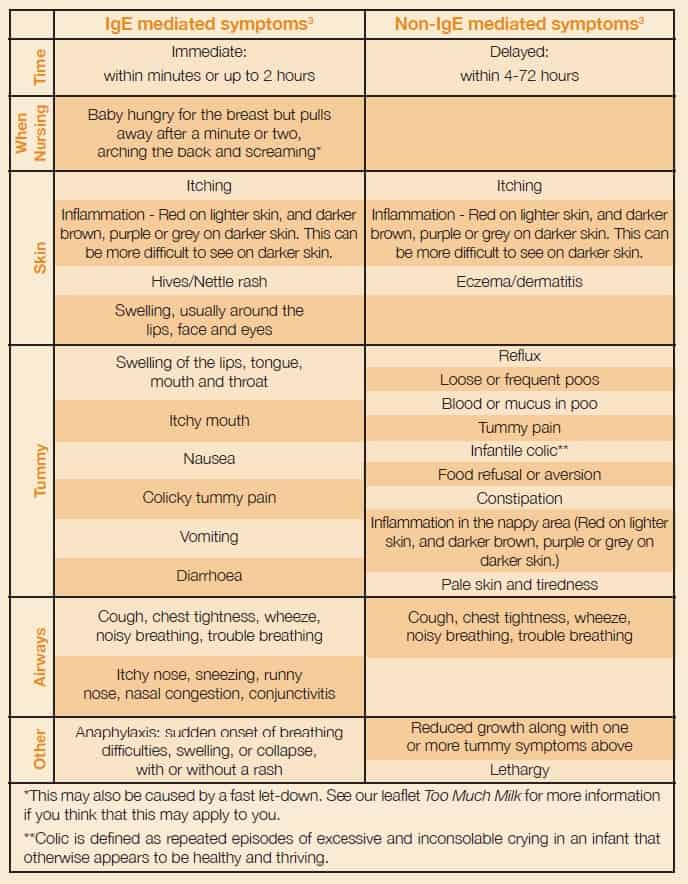
A food allergy occurs when a baby has an immune response to specific foods. There are two types of food allergy reactions; immediate and delayed. A baby can have either or both3.
Immediate reactions are also called IgE-mediated alllergies. This is because the baby’s immune system creates specific IgE antibodies to a certain food. If a baby is given the specific food they are allergic to, the IgE antibodies will recognise it and cause the rapid release of chemicals, including histamine, that trigger inflammation and allergic symptoms.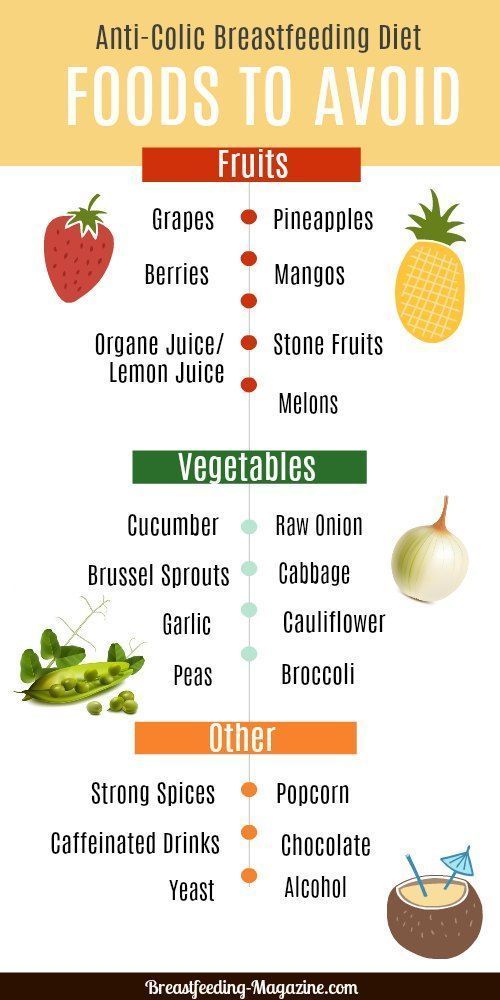 Symptoms appear within minutes, or up to 2 hours after eating the food responsible3.
Symptoms appear within minutes, or up to 2 hours after eating the food responsible3.
Delayed reactions are called non-IgE mediated allergies because they are not controlled by IgE. Instead it is believed such reactions are regulated by immune cells. Symptoms appear 4-72 hours after eating the food3.
It is wise to see your GP or health visitor if your baby is showing signs of allergy, but some symptoms are more worrying than others. Seek immediate medical help if your baby has signs of an anaphylactic reaction: sudden onset of breathing difficulties, swelling, or collapse, with or without a rash, after physical contact or eating a particular food.
Allergy symptoms
Food allergy symptoms occur in several different body systems; the tummy, airways and skin. An Allergic baby will usually have symptoms in more than one body system, but need not experience all the symptoms to indicate allergy. Many of the following allergy symptoms can also occur in normally developing children for other reasons.
| IgE mediated symptoms3 | Non-IgE mediated symptoms3 | |
|---|---|---|
| Time | Immediate: within minutes or up to 2 hours | Delayed: within 4–72 hours |
| When nursing | Baby hungry for the breast but pulls away after a minute or two, arching the back and screaming* | |
| Skin | Itching Inflammation** Hives/nettle rash Swelling, usually around the lips, face and eyes | Itching Inflammation** Eczema (dermatitis) |
| Tummy | Itchy mouth Nausea Colicky tummy pain*** Vomiting Diarrhoea | Reflux Loose or frequent poos Blood or mucus in poo Tummy pain Infantile colic*** Food refusal or aversion Constipation Inflammation in the nappy area** |
| Airways | Cough, chest tightness, wheeze, noisy breathing, trouble breathing Itchy nose, sneezing, runny nose, nasal congestion, conjunctivitis | Cough, chest tightness, wheeze, noisy breathing, trouble breathing |
| Other | Anaphylaxis: sudden onset of breathing difficulties, swelling, or collapse with or without a rash | Reduced growth, along with one or more tummy symptoms above Lethargy |
*This may also be caused by a fast let-down. See Too Much Milk and Oversupply for See Too Much Milk and Oversupply formore information if you think that this may apply to you. **Inflammation appears red on lighter skin, and darker brown, purple or grey on darker skin. ***Colic is defined as repeated episodes of excessive and inconsolable crying in an infant that otherwise appears to be healthy and thriving. | ||
Environmental triggers
An irritant is something that causes damage to the skin. Eczema (also known as dermatitis) and dry skin rashes can be caused by mild irritants such as bubble bath, baby wipes, skin cream, fabric conditioner or laundry detergent4. Many mothers find avoiding unnecessary products or using a different product improves things. Reading packaging can help avoid problems with common irritants such as lanolin and perfumes. Use fragrance-free products whenever possible. Be aware that herbals can also be allergenic and irritant – being natural does not necessarily mean a product is any less irritating.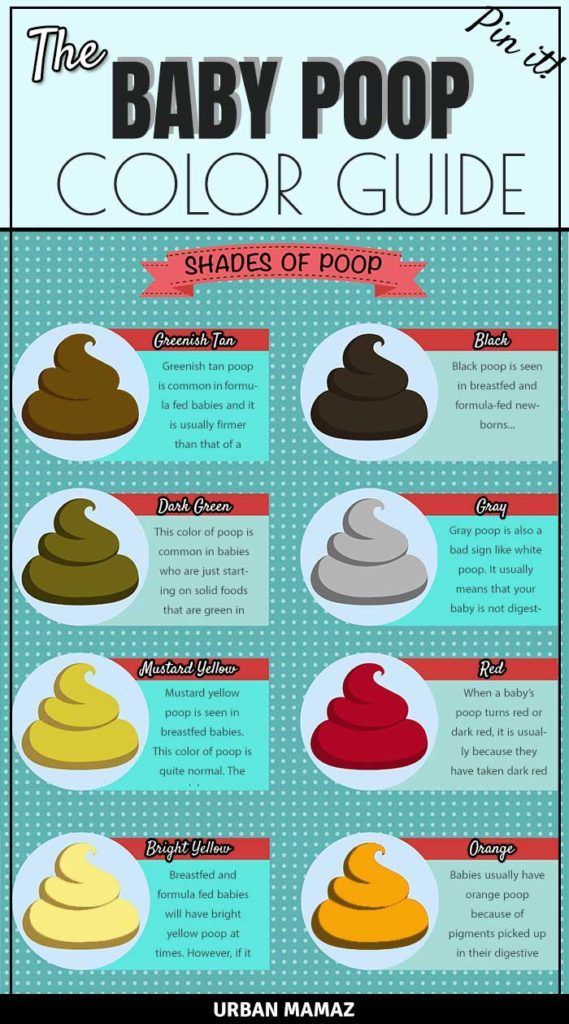 Hay fever symptoms and other ear, nose and throat symptoms can be caused by spring and summer pollens and other airborne allergens such as dust.
Hay fever symptoms and other ear, nose and throat symptoms can be caused by spring and summer pollens and other airborne allergens such as dust.
Identifying the problem food
If your baby is having only your milk
Food allergens in the mother’s diet can pass through into the breastmilk so a breastfed baby can have an allergic response or intolerance to something in the mother’s diet.
Consider:
- Are you taking any laxatives, medicines, vitamins, iron tablets or other supplements?
- Do you drink lots of caffeinated drinks? Coffee, cola, tea and some pain relievers, cold remedies, weight control aids and diuretics contain caffeine. Chocolate contains a substance called theobromine that can have a similar effect to caffeine if you eat a lot.
- Have you recently eaten a new food or any particular food in large amounts?
- Are there any foods that you don’t like but have decided to eat during pregnancy or breastfeeding because you think they will be good for you and your baby?
- Are there foods that you crave? What foods do you snack on when you have a bad day?
Depending on how sensitive your baby is, removing or cutting down on the offending items in your diet may well solve the problem.
If your baby is also having infant formula or solids
The majority of babies don’t need anything other than mother’s milk before about six months — no infant formula, drinks or solids. Babies who have started solids can be sensitive to certain common foods until they are a little older.
Consider:
- Could your baby be reacting to the drinks or solid foods he is having?
- Is he on any medication or vitamin supplements?
- Could he be receiving other drinks such as infant formula or juice, or solid food, from anyone else without your knowledge?
- Infant formula or follow-on formula is usually cow’s milk-based and a common, avoidable cause of allergy. Babies do not need follow-on formula at all.
Removing the offending food from your baby’s diet for now should solve the problem; they may be able to tolerate it in a few months time. If you think your baby may be reacting to a prescribed medication that they have to take, speak to your doctor, who may be able to prescribe an alternative.
Common problem foods
5Common problem foods which may be eaten by a baby or a breastfeeding mother include:
- Milk and other dairy products such as butter, yoghurt, cheese, whey, casein, caseinate, lactose
- Egg
- Peanut
- Soy
- Wheat
- Fish
- Sesame seeds (in tahini and hummus)
- Lupin/lentils (including chickpeas which are in hummus)
- Shellfish; crustaceans (e.g. crab, lobster, crayfish, shrimp, prawn), molluscs (e.g. mussels, oysters, squid)
- Fenugreek is closely related to peanuts
- Tree nuts (almonds, hazelnuts, walnuts, cashews, etc.)
- Celery and celeriac
- Mustard
Common foods that can be involved in intolerance or irritation but not usually allergy:
- Sulphur dioxide and sulphites, benzoates, glutamate, salicylates, dietary amines
- Citrus fruits, strawberries, tomatoes
- Certain additives, artificial colourings, flavourings and preservatives
These can turn up in the most unexpected places so do check everything consumed including drinks and medicines. For example, some juice drinks contain milk, and wine can contain milk, egg or sulphites.
For example, some juice drinks contain milk, and wine can contain milk, egg or sulphites.
Cutting out suspected foods
If your baby is exclusively breastfed, you may need to follow an elimination – reintroduction diet. It can help to keep a food and symptom diary.
When eliminating major food groups take care to ensure you continue to eat a healthy and balanced diet. Your GP may be able to refer you to a dietician if you wish.
Only cut out one food at a time and allow 2–4 weeks to see if your baby’s symptoms improve. If there is no improvement in this time, then the food is unlikely to be the culprit and can be reintroduced3. Consider cutting out a different food.
If symptoms do improve, reintroduce the food slowly to confirm the food allergy. However, if your baby has previously experienced a severe or immediate reaction, ask your GP for specialist support before reintroducing the food.
Note: Usually a cow’s milk protein allergy (CMPA) predicts an allergy to other animal milks (e. g. goat or sheep milk), and in some cases soya. If you plan to cut out dairy you may wish to cut out other animal milks and soya at the same time, then reintroduce them each individually.
g. goat or sheep milk), and in some cases soya. If you plan to cut out dairy you may wish to cut out other animal milks and soya at the same time, then reintroduce them each individually.
Seek immediate medical help if your baby has shown anaphylactic signs, such as a rapidly developing rash, breathing difficulties, or swelling.
A note on eczema
Elimination – reintroduction diets should not be done due to the presence of eczema alone.
Some children who have a food allergy do have eczema, but most children who have eczema do not have a food allergy. If the only symptom is eczema it is unlikely to be caused by a food allergy. It is worth noting that frequently eating a particular food may mean a baby learns to tolerate it. If the food is stopped, for example during an elimination diet, there is a risk that tolerance may stop and an IgE mediated allergy (including possible anaphylaxis) can form. If you think your baby’s eczema is due to a food allergy it is best to speak with your GP about allergy testing or to get referred to an allergy specialist6.
Introducing solid foods
Human milk contains tiny traces of whatever foods a mother herself has been eating. This is the ideal way to prepare a baby gently for the eventual introduction of solids. The best foods for your baby are usually healthy foods selected from your diet. Solids can be introduced when your baby can sit up (with or without support) and starts reaching out for the food on your plate. For more information, see Starting Solid Food.
If your baby is under the care of a paediatrician for allergies, talk to your specialist team about how to introduce specific allergenic foods.
Body tolerance levels can change
Being allergic or intolerant to something means that your body is sensitised to it, but the symptoms you display may vary in each particular instance; sometimes you may not display any symptoms. Your body’s allergen tolerance level changes based on many factors including stress and your general health, so its ability to react to immune threats also varies.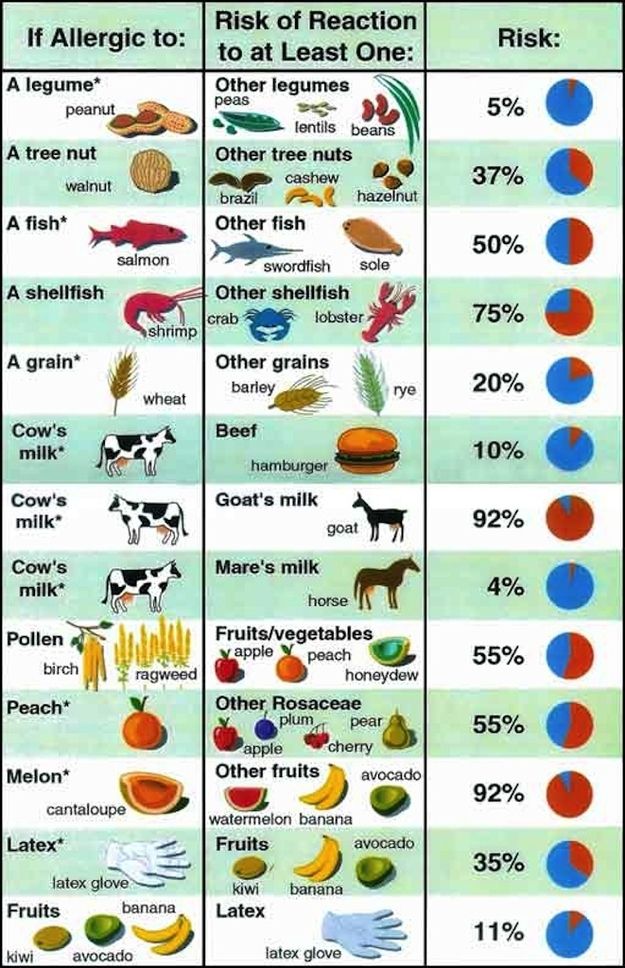 If your immune system is affected by more stressors than usual, you may show symptoms of an allergy/intolerance more readily.
If your immune system is affected by more stressors than usual, you may show symptoms of an allergy/intolerance more readily.
Seek support
It can be quite an effort to be an allergy detective with a fussy baby on your hands, so seek information and support. The good news is that small changes to your diet could make a big difference to a baby with a food allergy or intolerance.
An LLL Leader can help you determine the most likely cause of your baby’s symptoms. Local LLL groups are great for practical and moral support and you may find others there who have had similar experiences. Your GP or health visitor can help diagnose food allergy and refer you to specialist services for testing and advice.
Did you know?
- If a baby reacts when their mother drinks milk or has dairy products, this is a sensitivity to cow’s milk protein, not lactose intolerance.
- Most infant formulas contain cow’s milk, often referred to as whey based or casein based.
- Soya, the basis of some infant formulas, is also a common allergen.

- Infant formula may contain fish oils and vegetable oils (e.g. palm, rapeseed, coconut, sunflower).
- Medicines and supplements can contain other ingredients that are potentially allergenic.
- If you or a member of your immediate family has an allergy or intolerance, your baby is more likely to have one too1.
FAQs
Q. Do I have to give up breastfeeding if my baby is allergic to something in my milk?
A. No; eliminating the offending food from your diet will remove the allergen from your breast milk enabling you to continue breastfeeding if you wish to. See section Cutting out suspected food.
Q. Will my baby outgrow his food allergy?
A. Possibly; some children do, some do not. Children are most likely to grow out of cows’ milk, egg and soy allergies.
Q. I thought I was not meant to feed my baby egg/peanut/etc. until they were over 1 year old?
A. This was old advice.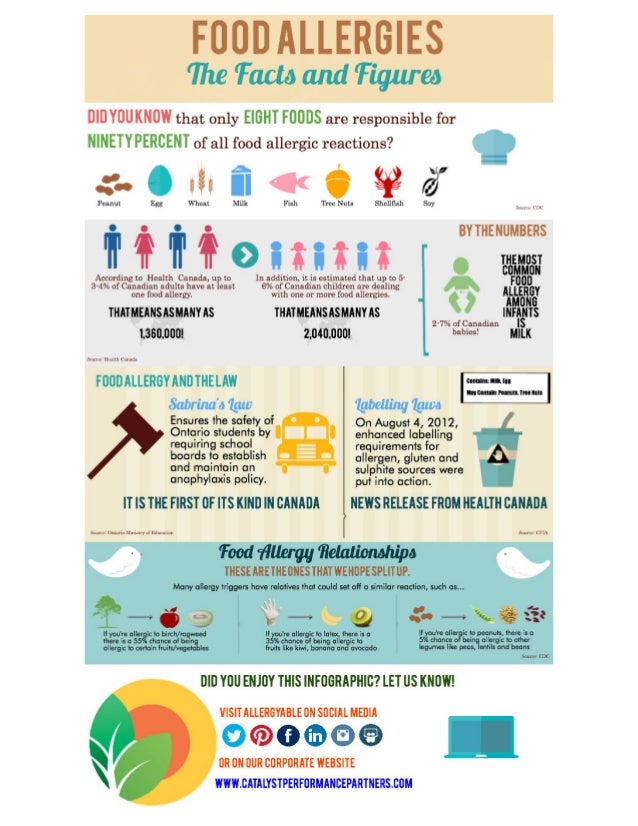 Recent research shows introducing allergenic foods from around 6 months old may help the baby to learn to tolerate the food. Introducing the food later can make it more likely that the baby will develop an allergy to the food.
Recent research shows introducing allergenic foods from around 6 months old may help the baby to learn to tolerate the food. Introducing the food later can make it more likely that the baby will develop an allergy to the food.
Q. What’s the difference between cow’s milk protein allergy (CMPA) and lactose intolerance?
A. True lactose intolerance (reduced capacity to digest lactose) is very rare in babies and is diagnosed within days of birth. Temporary lactose intolerance or lactose overload (too much lactose for the baby to digest) can cause tummy symptoms similar to an allergy. Lactose is produced in the breast, regardless of the mother’s diet. Seek support if you suspect your baby has symptoms of lactose overload. CMPA is an immune reaction and can cause symptoms in many body systems. Breastfeeding mothers of children with CMPA generally need to exclude all cow’s milk protein from their diet – including milk, cheese, yogurt etc. See section Cutting out suspected food.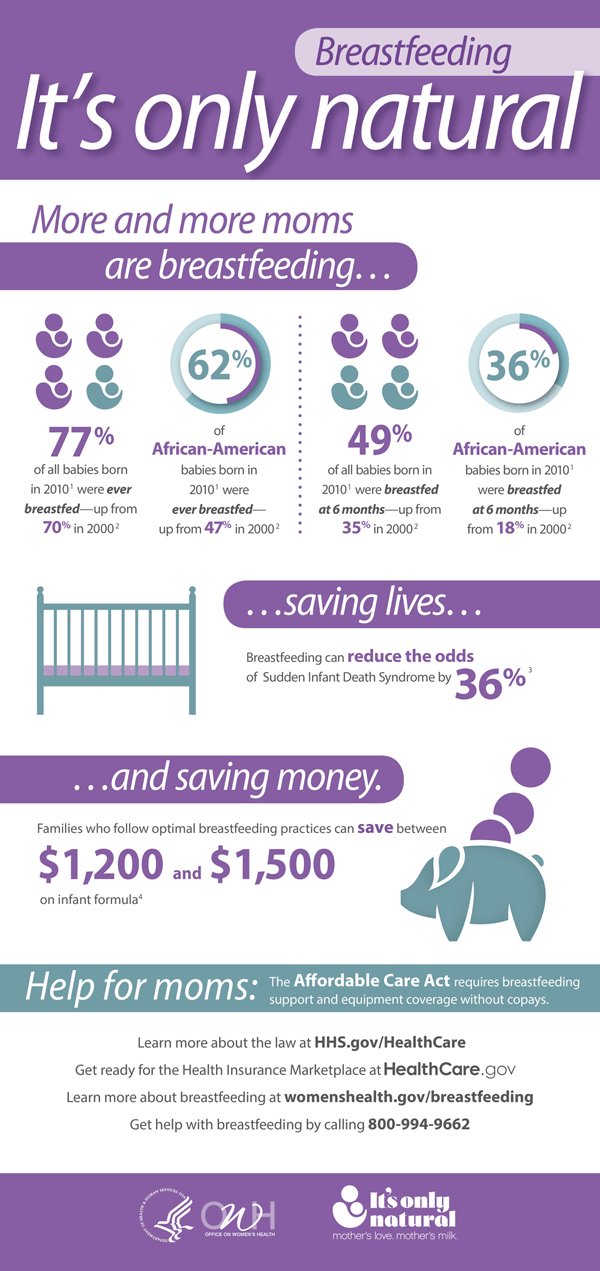
Q. Should I avoid eating a food my baby is allergic to if I become pregnant again?
A. No; as long as you are not allergic to it and it is not one the foods you usually need to avoid in pregnancy (such as undercooked meat) eating a particular food in pregnancy has no effect on the development of allergy.
Q. Is my baby allergic to a food because I ate it whilst pregnant?
A. No; eating a particular food in pregnancy has no effect on the development of allergy.
Q. If I have another baby will it develop allergies too?
A. Possibly; if you have a sibling with allergies you are more likely to be genetically predisposed to develop allergies. However, having an older sibling decreases the risk of developing allergy.
Written by Sue Cardus, Robyn Halliday and mothers of La Leche League Great Britain
Endnotes
- Andreas, N., Kampmann, B., Le-Doare, K. Human Breast Milk: A review on its composition and bioactivity.
 Early Human Development, 2015; 91 (11): 629-635.
Early Human Development, 2015; 91 (11): 629-635. - Muraro, A et al. EACCI Food Allergy and Anaphylaxis Guidelines. Primary prevention of food allergy. Allergy, 2014;69(5):590-601.
- NICE Guideline [CG116]. Food allergy in under 19s: assessment and diagnosis, 23rd February 2011, https://www.nice.org.uk/guidance/cg116 (accessed 26th Jul 2020).
- NHS. Contact dermatitis, https://www.nhs.uk/conditions/contact-dermatitis/causes/ (accessed 26th Jul 2020).
- Muraro, A et al. EAACI Food Allergy and Anaphylaxis Guidelines. Diagnosis and management of food allergy. Allergy, 2014; 69 (8): 1008-25.
- Young, M. Editorial: Elimination Diets in Eczema—A Cautionary Tale. JACI: In Practice, 2016; https://www.jaci-inpractice.org/article/S2213-2198(15)00573-5/pdf
Further Reading
The Womanly Art of Breastfeeding. LLLI. London: Pinter & Martin, 2010.
BREASTFEEDING ANSWERS – A GUIDE
FOR HELPING FAMILIES: SECOND EDITION.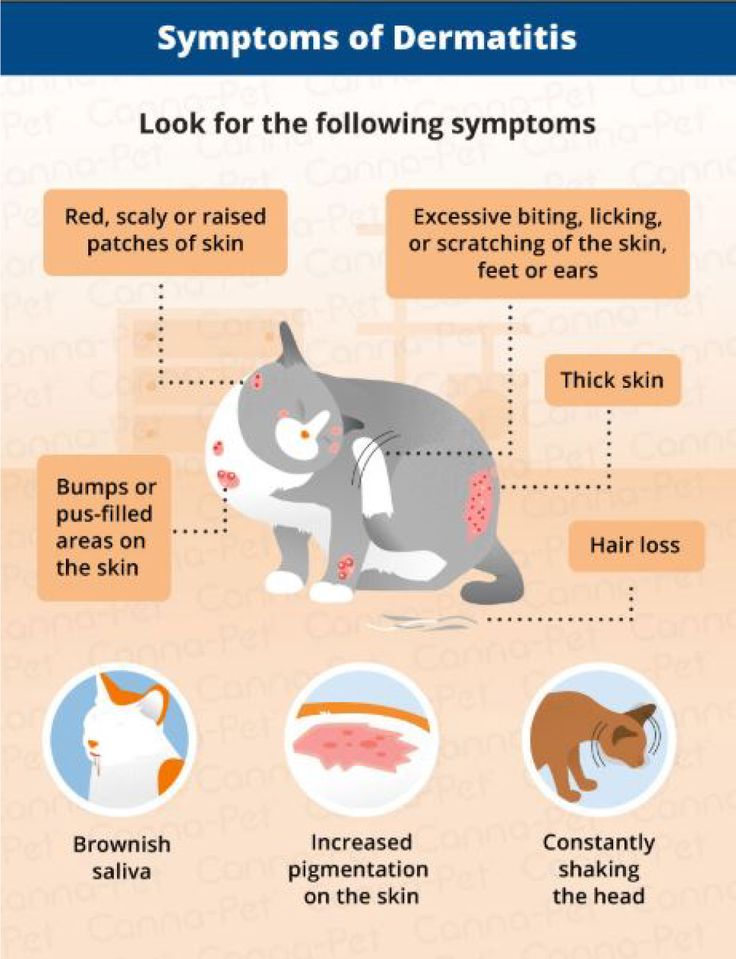 . Mohrbacher, N. Nancy Mohrbacher Solutions inc., 2020.
. Mohrbacher, N. Nancy Mohrbacher Solutions inc., 2020.
MILK MATTERS: INFANT FEEDING AND IMMUNE DISORDER. Minchin, M. Geelong: Alma Publications, 2015.
BREASTFEEDING WORKS! EVEN WITH ALLERGIES. Noble, R. Brisbane: Complete Publishing, 2017.
Amazing milk
Is My Baby Getting Enough Milk?
My Baby Won’t Breastfeed
Rhythms and Routines
Safer Sleep & the Breastfed Baby
Starting Solid Food
Toddlers and Food
The Unhappy Breastfed Baby
Too Much milk
Thrush and Breastfeeding
Online information:
LLLGB website
Unicef Research on Allergies
NICE Guideline [CG116]. Food allergy in under
19s: Assessment and Diagnosis
GP Infant Feeding Network: Cow’s Milk Allergy
National Eczema Society
Anaphylaxis Campaign
CMPA Support
You can buy this information in printed form from our shop.
Copyright LLLGB 2022
90,000 signs, causes, prevention, how to cure? Any ailment in a small child causes serious anxiety in his parents. But if, for example, with colds, everything is relatively simple (it is easy to suspect, the treatment regimen is clear, only strict adherence to doctor's prescriptions is required), then food allergies can confuse a young mother.
But if, for example, with colds, everything is relatively simple (it is easy to suspect, the treatment regimen is clear, only strict adherence to doctor's prescriptions is required), then food allergies can confuse a young mother.
Allergy is a kind of false alarm: the immune system reacts in this way to a harmless substance that it mistakenly considered a threat. This condition often occurs in children, since their defenses are not fully formed and “not trained” to recognize who is a “stranger” in the body and who is their own. The most common type is food allergy. In babies, fortunately, it lends itself well to correction. Moreover, timely treatment and exclusion of the allergen from the diet will most likely lead to the fact that someday the product will cease to be an irritant. This means that an adult child will be able to include it in his diet without fear of unwanted reactions of the body.
The predisposition to an allergy to a particular product can be hereditary .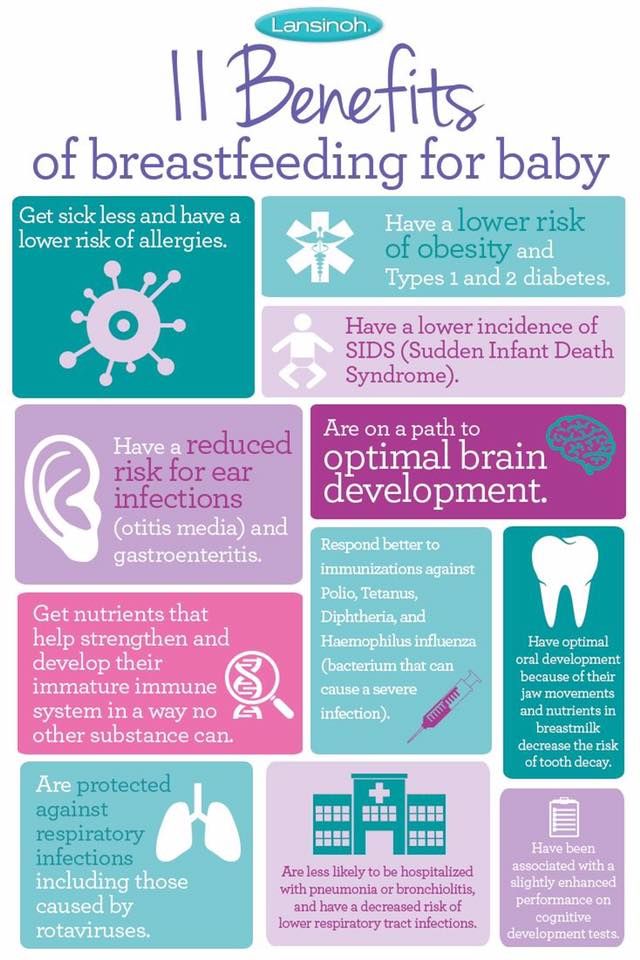 This does not mean that a mother with fish intolerance will necessarily have a child with the same feature. According to statistics, heredity manifests itself in 25% of cases, but if both parents are allergic, then the probability doubles [1] .
This does not mean that a mother with fish intolerance will necessarily have a child with the same feature. According to statistics, heredity manifests itself in 25% of cases, but if both parents are allergic, then the probability doubles [1] .
A food allergy in an infant may be caused by the infant's use of formula for artificial feeding. Despite the fact that manufacturers are trying to bring the composition of this product as close as possible to breast milk, the body can still reject some components. For example, milk formulas contain cow or goat milk, and animal protein often acts as an allergen. Some babies are allergic to soy, a common ingredient in dairy-free formulas. Therefore, nutrition is selected individually, under the supervision of a neonatologist.
Even when breastfeeding, a child can develop severe food allergies if the mother does not monitor her diet. The main products that irritate the immune system are known to most. But let's refresh the list:
- fruits and vegetables with red or orange pigment: tomatoes, peppers, peaches, strawberries, raspberries, cherries, cranberries, apples, oranges, tangerines, watermelon, dried apricots;
- exotic fruits: mango, dragon fruit, rambutan, etc.
 ;
; - fish and seafood;
- cow's milk;
- chicken eggs;
- nuts;
- honey;
- coffee, cocoa;
- chocolate.
The list is not complete, it may vary depending on the individual characteristics of the organism.
The introduction of complementary foods is another test for children's immunity. All the same rules work here as with the diet of a nursing mother. When adding new foods to your baby's diet, you need to carefully monitor his reaction to each meal. Below we will tell you how food allergies manifest in infants.
Food allergy symptoms in children
Food allergy symptoms in a child can be very diverse. This fact often leads to difficulties during the diagnosis of such conditions. Here are the main symptoms of food allergies in children:
- Changes in the skin : rash, peeling and itching on the cheeks, neck, in the folds of the skin, crusts and scales on the scalp, sweating and diaper rash.
- Edema . Of course, this is also a skin manifestation, but we decided to single out edema as a separate item. This is a very dangerous sign of allergy, warning of the possible development of Quincke's edema, which leads to respiratory failure, and without timely emergency assistance, even to death.
Attention!
If you notice that the baby is not breathing well, his eyes are swollen, the nose and lips are swollen, immediately remove all potential allergens from the child and call an ambulance!
- Change in the child's behavior. If the baby cries often, sleeps poorly, becomes restless or, on the contrary, lethargic, this may signal an allergic reaction.
- Gastrointestinal disorders . Vomiting, intestinal colic, frequent constipation and flatulence may be the body's reaction to an allergen. In addition, the listed symptoms are possible signs of serious problems in the digestive system.
 And regardless of the reasons, such violations of the digestive tract can have serious consequences. For example, frequent vomiting and diarrhea in young children leads to dehydration, which in turn can lead to more serious conditions and even death. Therefore, it is impossible to postpone the visit to the doctor in any case.
And regardless of the reasons, such violations of the digestive tract can have serious consequences. For example, frequent vomiting and diarrhea in young children leads to dehydration, which in turn can lead to more serious conditions and even death. Therefore, it is impossible to postpone the visit to the doctor in any case.
Frequent allergic reactions lead to the destruction and excretion of a large number of beneficial bifidus and lactobacilli from the intestines. These microorganisms colonize the human intestine in the first hours after birth. They do not allow pathogenic bacteria and viruses to multiply, participate in the process of digestion of food, and promote the absorption of vitamins and nutrients. The imbalance between beneficial and harmful bacteria is called dysbiosis. Food allergies can be both a cause and a consequence of microflora imbalance.
It should be said that dysbiosis occurs in almost every baby, only 10% of babies do not experience such a condition. So in most cases, the treatment of food allergies in young children includes correcting the balance of microflora.
So in most cases, the treatment of food allergies in young children includes correcting the balance of microflora.
Treatment of food allergies in infants
Note that "treatment" for allergies is not quite the correct wording. As we said, such a hostile reaction of the body to a common product occurs by mistake. To eliminate this condition, it is necessary, firstly, to review the diet of the baby (and mother, if the child is breastfed) and exclude all potential allergens. A pediatrician will help you choose a diet. If necessary, he can prescribe sorbents, the use of which will remove the allergen from the body.
If the allergy is not a simple redness of the cheeks, but is more severe, the specialist may prescribe antihistamine therapy.
Note
Histamine is a substance that the body begins to actively produce in response to an irritant.
With the help of such drugs, rashes, swelling and other symptoms can be quickly eliminated, however, in pediatrics, histamine is used in rare cases - due to an impressive list of contraindications and side effects.
With a high degree of probability, the pediatrician will also prescribe a remedy containing live beneficial bacteria to correct dysbiosis - probiotics. It is important to note that this is not a drug, which means that it does not give a medicinal load on the baby's body. Contraindications to the use of such drugs are most often only individual intolerance to the components.
Allergy in a baby is not the most pleasant condition for both the baby and his parents. However, it is, as a rule, easily corrected, provided that the mother, having noticed the first signs of a food allergy in a child, did not delay contacting the attending physician.
Amelekhin Leonid Aleksandrovich Managing editor
Editorial opinion
In the first two or three weeks of life, almost every baby has red spots on his face that resemble an allergic reaction. In fact, this is a hormonal rash: the body of a newborn is cleared of the mother's hormones that he received in the womb. This condition is considered normal and does not require treatment.
This condition is considered normal and does not require treatment.
Allergy in an infant: who is to blame and what to do?
Allergic diseases in children are among the top problems of modern pediatrics. Allergic reactions, in addition to unpleasant external manifestations, disrupt the physical and psycho-emotional development of the child. In addition, starting in early childhood, allergies can accompany a person all his life, developing into more serious forms (the so-called "allergic march"). All these facts oblige to treat allergies as a serious problem, not to self-medicate, and if a child has alarming symptoms, immediately contact a pediatrician or an allergist.
What could be the reason?
The direct cause of allergy is the contact of the child's body with the allergen. Among the most common allergens are the following:
Food
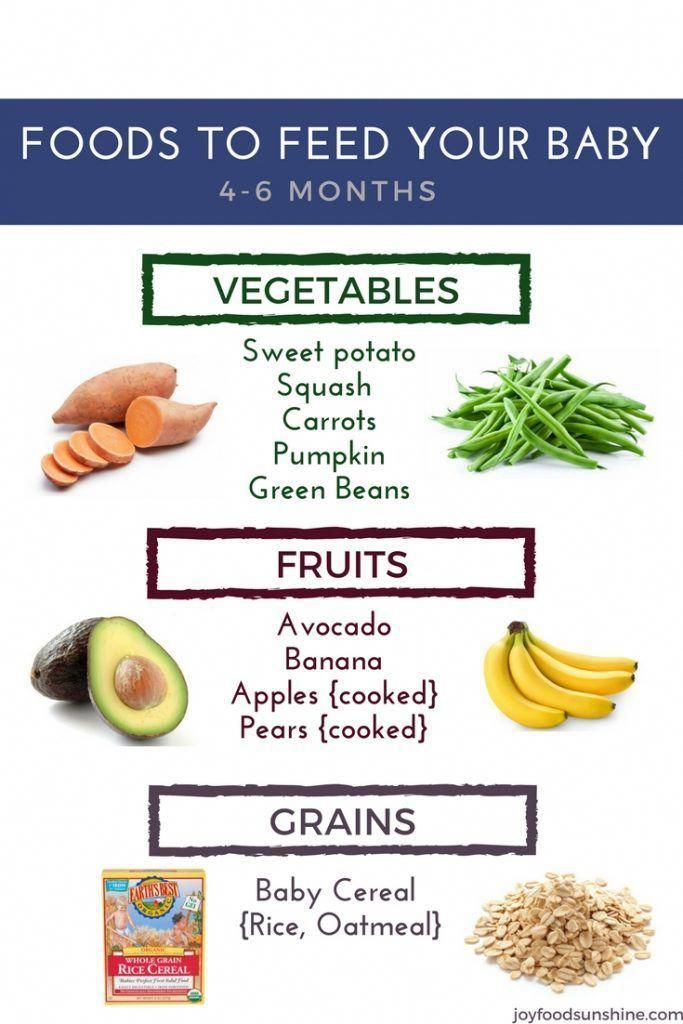
Allergies are more common in formula-fed children. Usually this is a reaction to cow's milk, which is part of an unadapted mixture. As complementary foods are introduced, a reaction to vegetable or animal protein may occur. That is why it is so important to introduce complementary foods gradually, in small portions, starting with the most “non-allergenic” foods.
As complementary foods are introduced, a reaction to vegetable or animal protein may occur. That is why it is so important to introduce complementary foods gradually, in small portions, starting with the most “non-allergenic” foods.
Household
These are dust, animal dander, cleaning products, washing powders and other allergens found in the home.
Contact
These are various cosmetics and dyes that get on the baby's skin or come into contact with it, causing irritation (soap, cream, clothing dyes, diaper impregnations).
Medications
Taking medicines, which inexperienced parents like to practice, can cause an allergy in a child. Thus, a negative reaction of the immune system to a foreign agent is manifested. Therefore, any medicine should be given to the child strictly according to the prescription of the attending physician.
In addition, there are a number of factors that increase the risk of developing allergies in babies.
First of all, this is heredity - parents suffering from certain forms of allergies can "give" this predisposition to their child. Moreover, the probability of inheriting the pathology increases if both parents have allergies.
Intrauterine hypoxia, premature birth, mother's smoking at any stage of pregnancy, and even insufficiently varied diet of a pregnant woman, which does not allow the baby to get acquainted with certain foods in the womb, can become provoking factors.
Unfavorable environmental conditions can also play a negative role in the appearance of allergic reactions in a child.
Oddly enough, an excessive desire of parents to ensure sterile cleanliness in the house can provoke an allergy. It is not necessary to do this - it is important for the child to train his immune system by contacting with various microorganisms.
How does an allergy manifest itself?
Most often, allergies in very young children manifest themselves in the form of a skin rash, itching, redness, dry skin, peeling, crusts on the head. Possible reactions from the gastrointestinal tract - bloating, diarrhea, severe colic, frequent regurgitation, discoloration of the stool. At the same time, the child behaves restlessly, sleeps poorly, refuses to feed, often cries.
Possible reactions from the gastrointestinal tract - bloating, diarrhea, severe colic, frequent regurgitation, discoloration of the stool. At the same time, the child behaves restlessly, sleeps poorly, refuses to feed, often cries.
Respiratory symptoms such as sneezing, coughing, clear nasal discharge, watery eyes and red eyes are also typical of allergies.
Fortunately, severe manifestations such as edema in the face, neck and chest, anaphylactic shock, generalized urticaria in infants are extremely rare.
How to diagnose allergies?
It is worth noting that allergies can have similar manifestations to prickly heat, parasitic or infectious diseases. Therefore, one should not hurry with self-diagnosis, and even more so with treatment.
The first thing to do if you suspect an allergy is to contact a specialist. The doctor will perform an examination, prescribe a blood test for the presence of specific antibodies (skin tests are not taken from infants), and only after that will determine the treatment.
An allergen can also be detected by simple observation - to monitor how the child reacts to potential allergy triggers: dyes, powder, diapers, pets, etc. It is very effective for parents to keep a food diary, which indicates all new foods introduced as complementary foods, and the baby's reaction to them.
What to do if the diagnosis is established
The most important thing in the treatment of allergies is to eliminate provoking factors. It is important to switch to hypoallergenic cosmetics, perhaps change the manufacturer of diapers, limit contact with pets, use only baby powders for washing things.
If an infant has a food allergy and is formula-fed, the use of hypoallergenic milk formulas is recommended. Complementary foods should be introduced according to the scheme approved by WHO, not earlier than the child reaches six months. And such obviously "allergic" products as citrus fruits, eggs, fish, nuts, should be introduced after two years of life.