Dream feed baby with reflux
Dream feeding: How to dream feed your baby
Updated Oct 10, 2022
Maybe you have heard the term “dream feed” from a friend, in one of the many sleep training articles you have read, or in your favorite parenting group. Wherever you were first introduced to the commonly used strategy to encourage fewer night wakings, we bet you still have some questions!
We’re glad you’re curious and are excited to help you better understand dream nursing or bottle feeding and how filling up your baby’s tummy just before their longest sleep can help everyone get a better night’s rest.
IN THIS ARTICLE:
What is a dream feed?
At what age can you dream feed?
Dream feed by age chart
When is the best time to stop the dream feed?
How do I dream feed?
Dream feed schedule (example)
Dream feed FAQs
What is a dream feed?
To put it simply, it’s a sleepy nursing or bottle feeding session given to your baby in the late evening (hours after they’ve already gone to sleep at bedtime), usually just before you go to sleep yourself. This practice of waking your baby to eat can help parents sync the longest stretch of their baby’s night sleep with their own. The idea is to shift your baby’s normal feeding time a bit earlier, and it works best for babies who wake at night due to hunger.
Note that offering breast milk or formula at this time typically won’t help improve sleep if a child is waking due to a sleep onset association rather than hunger. For example, if an infant older than 4 months will only fall asleep while being fed at bedtime, they will more likely need to be fed back to sleep when waking in the night between sleep cycles, even if they aren’t hungry. Offering a twilight feed in a case like this is unlikely to improve your baby’s sleep.
At what age can you dream feed?
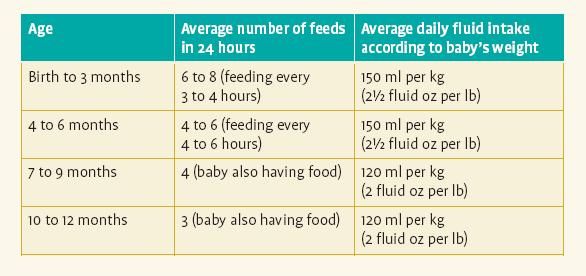
Great question! Parents around the world first introduce this twilight feed at various times. It is never too soon to introduce a sleep feeding into your baby’s schedule, although some prefer to wait until their baby graduates from the newborn phase.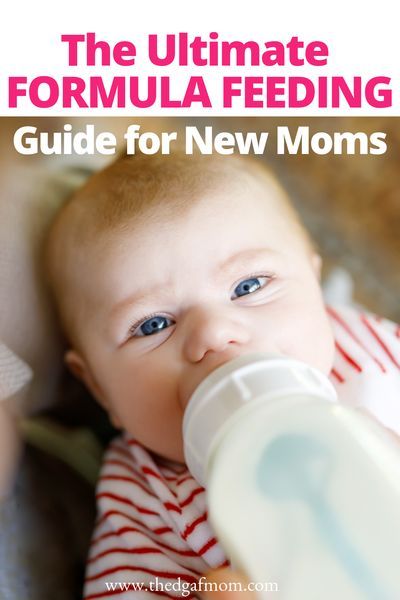 Dream feeding is most used for babies between 6 weeks and 10 months old.
Dream feeding is most used for babies between 6 weeks and 10 months old.
While many older breastfed babies (who are also consuming solids) are capable of going 10 - 12 hours overnight without a feeding, some simply are not. The age at which a baby can go all night without a feeding depends on several factors. While most 10 month olds are ready, or will be ready, to fully wean at night, some babies may continue to need at least 1 feeding overnight until closer to 12 months.
Let’s take a look at the optimal ages to dream nurse or bottle feed.
Dream feed by age chart
| Dream feed by Age | Why it is the optimal age |
|---|---|
| Dream feed at 6 weeks old | 6 weeks is a great time to add a sleepy feed to your baby’s feeding schedule. Around 6 weeks, many babies have just come out of their 4- to 6-week growth spurt and begin showing signs that they are ready to sleep for longer periods overnight. Around 6 weeks, many babies have just come out of their 4- to 6-week growth spurt and begin showing signs that they are ready to sleep for longer periods overnight. |
| Dream feed at 3 months old | 3 months is a very popular age to add a last feed before midnight. By 12 weeks, many babies can go one stretch of about 3 - 4 hours (or longer) without a feeding. Adding a dream nursing or bottle feeding a couple hours before midnight may help your baby sleep until 1 or 2 AM. |
| Dream feed at 4 months old | 4 months may be the most popular age to begin dream feeding. Between 4 and 6 months, babies will often experience another growth spurt and naturally show signs of needing an extra night feeding (even if they previously dropped an overnight feed). If this sounds like your baby, sleep feeding may be the answer! |
| Dream feed at 6 months old | 6 months is another ideal time to resume or begin. At around 6 months, babies’ bedtimes typically get earlier, leaving more time for nighttime sleep. Feeding your baby again a few hours after they have gone to sleep for the night can be the “magic trick” that gives you and your baby peaceful sleep until the early morning hours. At around 6 months, babies’ bedtimes typically get earlier, leaving more time for nighttime sleep. Feeding your baby again a few hours after they have gone to sleep for the night can be the “magic trick” that gives you and your baby peaceful sleep until the early morning hours. |
| Dream feed at 10 months old | Some 10 month old babies, who are still waking to feed at night, can also benefit from a last feed around 9 or 10 PM. A well-timed dream feeding at this age helps some babies sleep until it is time to wake up for the day. However, do note that a dream feed can interrupt a baby’s natural sleep cycle, and they may continue to wake in the early morning hours. Older babies may sleep better with one feeding between 3:00 and 5:00 AM rather than a dream feed. |
When is the best time to stop the dream feed?
Babies will not need a dream feed forever. The best time to stop or drop it depends on a few things. At Huckleberry, we take into consideration:
The best time to stop or drop it depends on a few things. At Huckleberry, we take into consideration:
Your baby’s primary feeding method (i.e., breastfeeding, bottle feeding, combination feeding, and if solids have been introduced)
Calorie intake during the day
How ready you are to stop the feeding
Whether your baby is waking from true hunger or a sleep onset association
How helpful the feeding is to your baby’s sleep schedule and ability to sleep longer as a result of a late-night last feed
How do I dream feed?
Now that you know what this sleepy feed is, what age you can offer this feed, and the best time to stop, let’s help you learn how to dream feed your baby.
Step 1. Rouse the baby.
After your baby has been sleeping for 1 - 3 hours, you will want to gently wake up your baby. Many families ask us, “How awake should my baby be for the dream feeding?” Ideally, you want your baby to remain drowsy and awake just enough to take a full feeding.
Pro Tips:
Keep the lights off or very dim.
Be boring! Try not to talk, move around, or make a lot of noise.
Be mindful as you pick up your baby from the crib or bassinet. Slow and steady movements help keep you and your baby safe and reduce the chances of waking them fully.
Step 2. Get ready to feed.
How long or how much to feed your baby at this final feed of the night varies.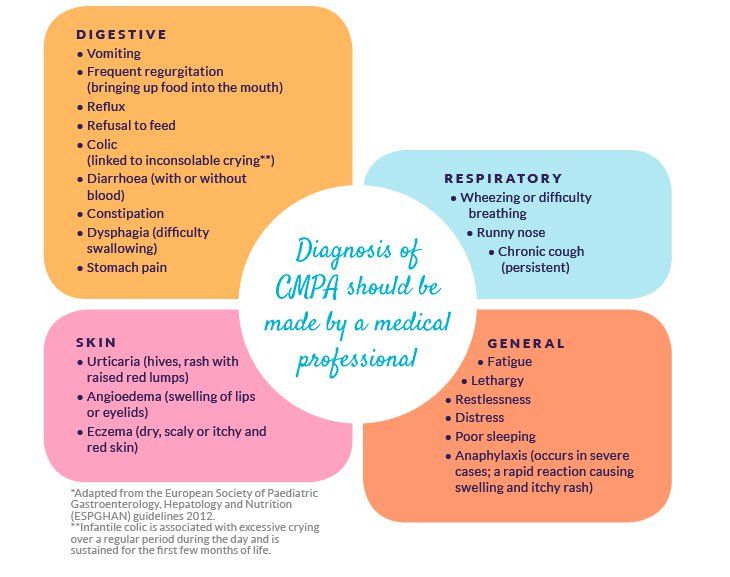 Breastfed babies may need to nurse for just a few minutes (e.g., 5 - 10 minutes) or half an hour. There is no magic twilight feed duration that applies to every breastfeeding mom and baby. Bottle-fed babies, like breastfed babies, will require differing amounts, depending on their age, size, and how recently they last ate.
Breastfed babies may need to nurse for just a few minutes (e.g., 5 - 10 minutes) or half an hour. There is no magic twilight feed duration that applies to every breastfeeding mom and baby. Bottle-fed babies, like breastfed babies, will require differing amounts, depending on their age, size, and how recently they last ate.
Step 3. Put the baby back to sleep.
After the feed, your goal is to put your sweet one back in their sleep space without them waking up fully. This can be tricky, but with practice and patience, it can be done!
Use slow/steady movements to gently lay your baby back down to sleep. If your baby wakes fully, ideally, they will fall back to sleep in the same way that they fell asleep at the beginning of the night. Follow safer sleep guidelines by laying your baby down on their back.
Let’s not forget burping!
Not every baby is a “big burper” or needs to burp following every feed. You know your baby best; if your baby tends to need a burp after finishing a feed, be sure to get one before laying your baby back in the crib or bassinet.
You know your baby best; if your baby tends to need a burp after finishing a feed, be sure to get one before laying your baby back in the crib or bassinet.
Bonus round! The double dream feed…
You read that right. Some parents double down on the dream nursing or bottle. The double feed is when you purposefully offer your baby two sleepy feedings in the evening, roughly 2 hours apart, with the final feed occurring close to midnight.
Dream feed weaning
Once a family is ready, they can stop waking their baby for the feedings and let them wake naturally when they need to eat. Another option is to offer a little less milk or formula each night. For example, parents can gradually lessen the time spent nursing by a few minutes or reduce the formula in the bottle by 1 - 2 ounces.
Dream feed schedule
Here is an example of a dream nursing or bottle schedule.
6:30 PM Bedtime feeding
7:30 PM Bedtime
9:30 PM Parent rouses baby for dream feeding
10:00 PM Baby is back to sleep
1:30 AM Baby wakes for night feeding
4:30 AM Baby wakes for night feeding
7:30 AM Wake up
Pros and cons of dream feeds
| Pros of dream feed | Cons of dream feed |
|---|---|
| Encourages longer stretch of sleep overnight | Family may prefer a more organic feeding schedule |
| Helps parents feel more rested | Baby may be difficult to wake for feed |
| Protective of milk supply | Baby may wake up fully and need help going back to sleep. Babies helped back to sleep may develop (or maintain) a helped-to-sleep association which can lead to increased night waking. Babies helped back to sleep may develop (or maintain) a helped-to-sleep association which can lead to increased night waking. |
| Helps baby receive adequate calories | Parents may prefer an earlier bedtime for themselves |
| Promotes a more predictable schedule | Requires planning and forethought |
Dream Feed FAQs
Q: Is a dream feed right for us?
A:
For babies 10 months or younger who are waking from hunger (which can also manifest as early risings), you might consider offering a dream feed to lengthen their stretches of nighttime sleep.
Q: Is a dream feed guaranteed to work?
A:
Dream feeds help some families get more sleep, while others don’t find them very useful. We find that dream feeds won’t help babies sleep better if they are waking for reasons unrelated to hunger, such as a sleep onset association or schedule issues. You can always give it a try for a few nights to see if it will work for your family.
Q: When is the ideal time to offer a dream feed?
A:
The ideal time to offer a dream feed is before the parent’s bedtime, typically between 10 PM and midnight.
Q: Will offering a dream feed lower my milk supply?
A:
Feeding your baby again in the late-night hours sends the signal to your body to produce more breast milk and can promote an increase in milk production.
Q: My baby has reflux, can I still dream feed?
A:
Babies with reflux may need to be held upright for 10 - 30 minutes after a feeding. If your baby requires upright time after feedings, be sure to factor in this extra time when planning your night feeding schedule with a dream feed.
Q: Can I dream feed with formula?
A:
A sleep feeding can be done with breast milk or formula.
Q: Should I wake my baby to feed at night?
A:
Waking a baby for a dream nursing or bottle feeding right before the parent’s bedtime can sometimes lengthen night sleep for the entire family. This can be particularly helpful if a baby is waking at night from hunger. However, waking a baby to feed at night won’t typically help extend sleep if a child is waking for other reasons (such as a sleep onset association).
This can be particularly helpful if a baby is waking at night from hunger. However, waking a baby to feed at night won’t typically help extend sleep if a child is waking for other reasons (such as a sleep onset association).
Q: Can dream feeding cause early waking?
A:
A feeding before the parent’s bedtime won’t typically be the cause of an early morning waking habit. However, some babies will continue to wake during the early morning hours to feed, even if they are offered a twilight feed.
Q: Can a dream feed reduce night wakings?
A:
Yes, in some cases, offering an additional night feeding before the parent’s bedtime can extend sleep. Offering breast milk or formula at this time tends to be most helpful if the child would otherwise wake from hunger in the middle of the night.
How to Properly Dream Feed Your Baby
Skip to contentLearning how to dream feed baby is quite simple. Yay! Yet dream feeding is one of those terms that gets tossed around so much that everyone assumes that everyone else knows the exact meaning of the term. When you dig a little deeper, you see that people have WILDLY different definitions of the same exact term!
Last Updated Jan 27, 2021.
Photo Credit: Zach Lucero
So What Is a Dream Feed?
Just so everyone is on the same page…
A dream feed is when:
- a parent goes to their sleeping infant,
- picks them up to breastfeed
- or props them up either in their crib, or in a caregiver’s arms, to offer a bottle,
- feeds the child,
- and then puts them back down *asleep* without the baby ever having woken up.
A dream feed is NOT a dream feed if a child:
- opens their eyes at any point in the process,
- or if the feeding is in response to the baby waking up.
Generally speaking, a dream feed is done between the hours of about 9:30pm and 12:00am. Technically, if all other terms are met, but the feed is done outside of these hours, the feeding is still a dream feed.
The Right Age for Dream Feeding
Dream feeds are a great tool from birth (or a few weeks after, when babies are not quite so sleepy), through to when a baby is done being swaddled. It is very challenging to dream feed a baby, even a very young one, without waking them up if they are not swaddled. Generally speaking, it’s wise to stop dream feeding around 14–16 weeks of age. After this age, babies become a lot more awake and aware, and dream feeds tend to disrupt the rest of their overnight sleep.
Check out my Newborn Sleep Program!
Benefits of Dream Feeding
Let me first dispel a myth. A dream feed does not necessarily prevent a baby from waking up to eat at night. Although, sometimes it does work. I like dream feeds for young babies because I appreciate the “insurance policy” of extra calories at night. As long as a baby is young enough that the dream feed itself does not wake them, and fracture their remaining nighttime sleep, a dream feed can insure as many calories as possible during each 24-hour period.
As long as a baby is young enough that the dream feed itself does not wake them, and fracture their remaining nighttime sleep, a dream feed can insure as many calories as possible during each 24-hour period.
A gift to reflux-y babies!
Some babies respond beautifully to a dream feed. Especially those with reflux! From about 7pm on through to about 2 or 3am, the body is flooded with the hormone melatonin. Melatonin is responsible for many things. Chief amongst them is making the body feel drowsy, and relaxing the long muscles (abs, legs, and arms). Since the abdominal muscles are relaxed, it’s common for babies with a lot of reflux to tolerate a dream feed without spitting up. And even possibly negate the need to be burped, or held upright afterwards. I can speak to this from personal experience with my own extremely reflux-y, wholly unmedicated daughter. Since the concern for calorie intake is so high with reflux babies, dream feeds can be especially useful for them.
Burping After a Dream Feed
If you feel your sleeping baby needs to be burped, go ahead and attempt to burp them as you normally would during the day. Check in with your pediatrician to ask how long to attempt a burp before giving up and putting baby back to sleep.
Check in with your pediatrician to ask how long to attempt a burp before giving up and putting baby back to sleep.
The bottom line is that a dream feed done correctly can benefit baby AND parents by offering an extra dose of nutrition, while also possibly helping baby sleep! (Which means YOU can get more sleep too! Win!)
If you like staying in the know with the most up-to-date information, and learning everything you can about your little one’s sleep, please sign up for my newsletter using the button below!
Sign up for my newsletter!
So remember, to properly dream feed your baby…
- Enter their room (keeping it dark!), and prop baby up either in their crib, or your arms, and immediately start feeding them the breast or bottle.
- Dream feed between 9:30pm-12:30am (or whenever you are heading to bed yourself!)
- Baby should NOT wake up AT ALL during the entire feeding. (Baby should be put back down in bed just as asleep as they were when you starting the feeding.
 )
) - You should stop attempting dream feeds when baby starts to sleep unswaddled. (Or around 14-16 weeks old when these feeds can start to become disruptive to their nighttime sleep.)
If you want to learn everything I know about babies under 16 weeks, check out The Newborn Sleep Program. This program can help set up your newborn (and you) for the best possible sleep! And if your baby is older than 16 weeks old, and you’re looking for affordable, hands-on sleep training support, check out my online training series: The Baby Sleep Trainer Program + Support. Use the code DFbaby for 10% off either program.[/fusion_text][/fusion_builder_column][/fusion_builder_row][/fusion_builder_container]
Search for:
Articles by Age
Categories
- Naps
- Newborn
- Opinion
- Sleep FAQs
- Sleep Training
- Getting Started
- How To Be Successful
- Success Stories
- Troubleshooting
Reflux in a child does not sleep at night
What is reflux?
Reflux is an extremely unpleasant phenomenon at any age; And for children under one year old, this is a fairly common problem, due to the underdevelopment of the lower esophageal sphincter.![]() Food mixed with gastric juice, moving in the "wrong" direction, enters the esophagus, pharynx, or even into the oral cavity, irritates them and causes vivid pain. If this happens in adults, we call it heartburn.
Food mixed with gastric juice, moving in the "wrong" direction, enters the esophagus, pharynx, or even into the oral cavity, irritates them and causes vivid pain. If this happens in adults, we call it heartburn.
Babies with reflux often spit up, eat small meals, sleep restlessly, wake up with a sharp cry, experience pain after feeding, and therefore have difficulty falling asleep after eating.
For many children the problem disappears by 12-14 weeks, other babies cope with it closer to the year. But until then, sleep will remain very restless . And it happens that all the mother's efforts aimed at teaching sleep: creating favorable conditions, maintaining a comfortable sleep regime, consciously teaching how to fall asleep on their own, do not lead to a calm, predictable sleep. The child continues to sleep in fits and starts for 20-30-40 minutes, often wakes up crying, behaves restlessly, refuses to go to bed after evening feeding, does not fall asleep after a snack at night.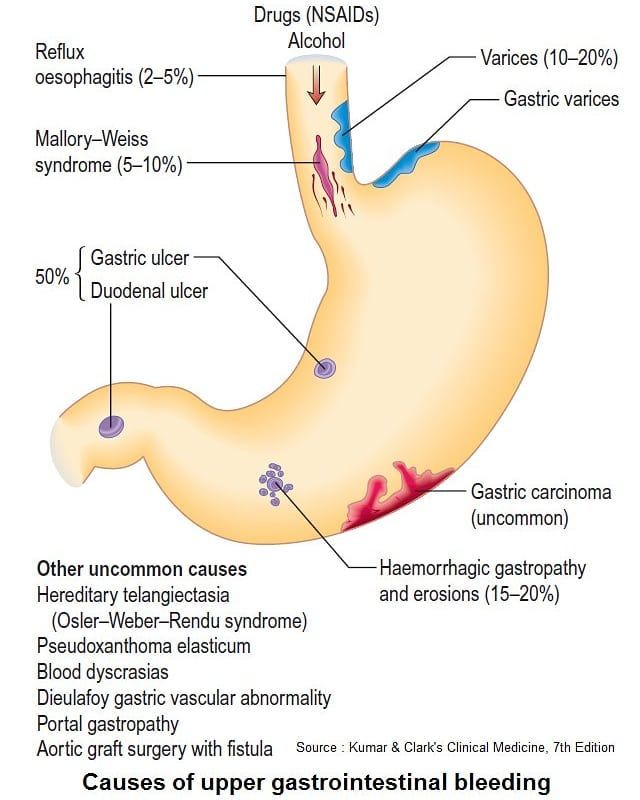
How to recognize reflux?
It is important to know that although the most obvious sign of reflux is frequent spitting up and vomiting, it is also impossible to calm the baby at the time of the attack, because. he cries in pain. Reflux can also be silent. Shorter than peers, thirty-minute sleep cycle can also indicate problems with digestion.
If "behavioral" methods of improving sleep do not lead to the desired result, there may be an occasion to once again talk with a pediatrician or pediatric gastroenterologist.
VIDEO LESSON
Baby sleep from 0 to 3 months
More
Signs of reflux can be:
1. Very short sleep cycle - no more than 35 minutes (especially if the baby is over 6 months old).
2. Frequent regurgitation, vomiting.
3. Frequent awakenings with sharp crying.
4. The child eats restlessly, with pauses, sometimes lets go of the breast or the bottle crying, refuses to take it again.
5. Dislikes lying on his back, especially after eating. Likes vertical position.
6. The kid mastered the skill of turning over from back to stomach and from stomach to back quite late, much later than peers, after about 5-6 months.
7. Crying after eating, especially in a horizontal position
8. Sometimes a child in a lying position may shake his head or, turning over, hit his head on the mattress (in this way he helps himself to burp).
9. Frequent mouth breathing, as stuffy nose (especially after waking up in the morning or after naps).
10. In general, reflux often causes breathing problems, which can be said:
a. Sweating during sleep.
b. Noisy breathing, deep voice.
11. Reflux can be associated with allergies, especially cow's milk protein allergy.
12. In general, children with reflux are often more moody, whiny, and always look overtired.
How can I help my child with reflux sleep?
If reflux is diagnosed, how can mom help:
1. Do not feed directly at bedtime . Eating at least 30 minutes before bedtime.
Do not feed directly at bedtime . Eating at least 30 minutes before bedtime.
2. Be sure to hold your baby upright after eating for 15-20 minutes.
3. If you are breastfeeding, avoid dairy products in your diet. Eliminate other foods and factors causing your allergic reaction. It will take at least a few days for the mucous membrane of the stomach and esophagus to “heal”, and the baby will feel better.
4. Your baby will be more comfortable sleeping in a head-to-toe position. Raise one part of the mattress (put something on it) to form a slight angle (15-20 degrees). To prevent the baby from sliding down, you can put a thin blanket rolled into a tube in the form of a horseshoe (or the letter U) under the stretch sheet, and lay the child with his legs inside the formed horseshoe.
5. If the baby freely rolls over from back to stomach and from stomach to sleep, put the baby to sleep on the LEFT side or on the stomach (again, not immediately after eating).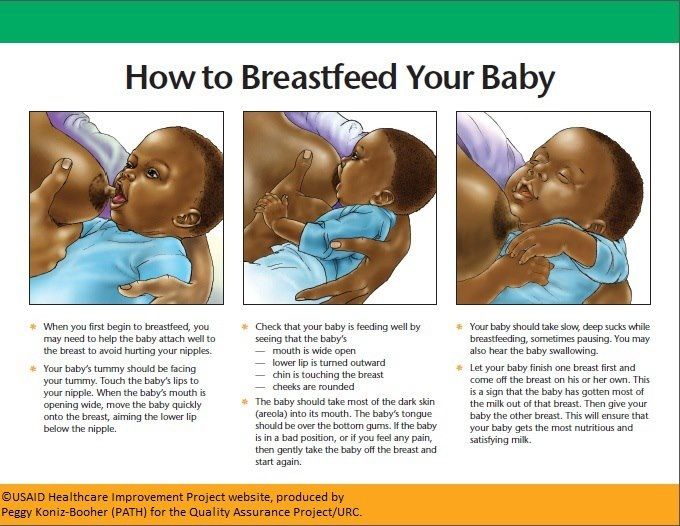
6. Do not wear clothes with tight elastic bands around the stomach and do not tighten the diaper too tightly.
7.On the first awakening (30-40 minutes after the start of sleep), immediately lift the child vertically and simply hold. Then put back to sleep in the crib or help to fall asleep in your arms.
8. Be sure to ask your doctor to prescribe acid-reducing medicines indicated for children with reflux. These medicines relieve pain for at least a few hours - this will help you sleep more peacefully.
9. Start learning how to fall asleep on your own after you get your reflux under control.
Medical Problems and Sleep Physiology Sleep
Reflux in Infants: Symptoms and Treatment
Search Support IconSearch Keywords
Home ›› What is Reflux in Infants?
Home ›› What is reflux in babies?
↑ Top
Signs and what to do
Post-feed regurgitation is common in the first few months of life. This is usually harmless and completely normal, but parents should read about gastroesophageal reflux (GER) and laryngopharyngeal reflux (LPR) in infants and how long it lasts to give them peace of mind.
This is usually harmless and completely normal, but parents should read about gastroesophageal reflux (GER) and laryngopharyngeal reflux (LPR) in infants and how long it lasts to give them peace of mind.
We look at signs of reflux in babies, symptoms of different types of reflux, and how to help a child with signs of reflux. If you require further information, always contact your healthcare provider.
What is reflux in babies?
So we know reflux is common, but what causes reflux in babies? Because young children have not yet fully developed the lower esophageal sphincter (LES), that is, the muscle at the bottom of the esophagus that opens and closes to let food into the stomach and keep it there, food can easily pass back up the esophagus.
Acid reflux, also known as gastroesophageal reflux (GER), is a normal reflux that occurs in babies. This type of reflux is considered normal and occurs in 40-65% of babies.
How do I know if my child has acid (gastroesophageal) reflux?
If a baby is spitting up milk after a feed, it is most likely acid reflux. As babies get older, GER usually goes away on its own without any intervention. If a baby has complications beyond just spitting up a small amount of milk (such as feeding difficulties and discomfort), they may have gastroesophageal reflux disease (GERD).
As babies get older, GER usually goes away on its own without any intervention. If a baby has complications beyond just spitting up a small amount of milk (such as feeding difficulties and discomfort), they may have gastroesophageal reflux disease (GERD).
Symptoms of GERD include:
- baby arching during or after feeding;
- crying more than three hours a day for no apparent reason;
- cough;
- gag reflex or difficulty swallowing;
- irritability, restlessness after eating;
- eating little or not eating;
- poor weight gain or loss;
- difficult breathing;
- severe or frequent vomiting.
GERD usually occurs when LES muscles are not toned in time, causing stomach contents to back up into the esophagus.
How do I know if my child has Laryngopharyngeal Reflux?
Another type of reflux, laryngopharyngeal reflux (LPR), also called silent reflux, is when the contents of the baby's stomach leak back into the larynx, the back of the nasopharynx. This type of reflux does not always cause external symptoms, which is why it is called "silent". Babies can have GERD and silent reflux at the same time, but their symptoms are somewhat different.
This type of reflux does not always cause external symptoms, which is why it is called "silent". Babies can have GERD and silent reflux at the same time, but their symptoms are somewhat different.
Some of the symptoms of laryngopharyngeal reflux are listed below:
- trouble breathing;
- gag reflex;
- chronic cough;
- trouble swallowing;
- hoarseness;
- regurgitation;
- poor weight gain or weight loss.
We have looked at the signs of reflux in infants, now we will move on to the treatment and duration of silent reflux in children, as well as the treatment of GERD.
How to deal with laryngopharyngeal reflux in infants while breastfeeding?
Breastfeeding mothers may need to review their diet if their babies show signs of reflux. The American Academy of Pediatrics (AAP) recommends breastfeeding mothers cut eggs and milk from their diet for two to four weeks to see if their baby's reflux symptoms improve or disappear. It may be worth eliminating acidic foods from your diet.
It may be worth eliminating acidic foods from your diet.
In most cases, GER and laryngopharyngeal reflux go away on their own. Typically, children outgrow reflux in the first year of life. If a child has persistent symptoms of laryngopharyngeal reflux, parents should consult a doctor. If your baby has severe vomiting, blood in the stool, or any of the symptoms of GERD listed above, parents should contact their pediatrician as soon as possible.
How can I help my child with reflux or GERD?
Reflux symptoms in infants usually go away on their own, but the following tips may help relieve symptoms:
- Thicken food with rice or a special milk thickener.
- Hold the bottle at an angle that fills the nipple completely with milk to reduce the amount of air your baby swallows. This can help prevent colic, gas, and reflux.
- Try the AirFree anti-colic bottle, designed to reduce air swallowing during feeding.

4. Let your baby burp during and after feeding. If the baby is bottle fed, parents can let him burp after every 30-60 ml. If the mother is breastfeeding, she may let the baby burp when changing breasts.
5. Hold baby upright after feeding. As a rule, in order for the milk to remain in the stomach, after feeding the baby, it is necessary to hold it in an upright position for 10-15 minutes. But, if the child has reflux, parents should keep him upright a little longer.
These tips may help relieve symptoms, but they do not replace a doctor's advice.
Parents should not change their infant formula formula without first talking to their healthcare provider.
Don't panic! Reflux is very common in babies during the first three months of life, and most babies outgrow it without any consequences. Although GERD is a slightly more serious condition, there are many treatments, ways to manage it, and help newborns. Feel free to contact your doctor with any questions or concerns you may have.