Early allergen introduction baby food
How Ready, Set, Food! Early Allergen Introduction Works
Ready, Set, Food! is the only early allergen introduction system that delivers the right food allergen to your baby at the right time starting at 4 months of age.
TEAR
Each day empty one packet into bottle of breast milk or formula with at least 2 ounces of liquid. Can also mix with food.
MIX
Shake bottle or stir food for 10 seconds. Works best in size 1+ nipples.
EAT
Your baby should drink most of the bottle, but does not need to finish it. If you miss a day simply resume the next day.
Scoop & Pour
Scoop the amount of baby oatmeal your child eats into a bowl. Add breast milk, formula or water.
Stir & Warm
Stir to desired consistency. Serve as is or heat until warm.
FEED & ENJOY
It’s mealtime – Yummy!
What is early allergen introduction and why do it?
Early allergen introduction is the process of frequently feeding common allergenic foods, such as peanut or egg, to your baby. The 2020 USDA Dietary Guidelines for Americans and other prominent medical associations (NIH, AAP, AAAAI) recommend introducing peanut and egg in the first year of life (after age 4 months), otherwise known as early allergen introduction. This is especially important for babies with eczema who have a 1 in 3 chance of developing food allergies. With Ready, Set, Food!, we make it easy to introduce allergens early and often.
Why is Ready, Set, Food! the best way to introduce allergens?
Ready, Set, Food! is the best option for introducing allergens because we make the process simple. It is important to note that for early allergen introduction parents need to frequently feed allergenic foods such as peanut, egg, and milk to their babies. Parents have found that trying to do this on their own is difficult and time-consuming, which is why we've created Ready, Set, Food! to help make early allergen introduction easy.
When should I start my baby on Ready, Set, Food! and for how long?
The 2020 USDA Dietary Guidelines for Americans and other prominent medical associations (NIH, AAP, AAAAI) recommend starting babies as early as 4 months of age with food allergen introduction.
We recommend starting the Stage 1 introduction, and Stage 2 for continued exposure together anytime between 4 - 12 months of age. You should sustain exposure to Stage 2 for at least 6 months.
Stage 3 is designed as the next step from Stage 2, and expands allergen exposure from 3 to 9 allergens including tree nuts, sesame, wheat and soy. However, if your baby hasn't started allergen introduction, but is already eating solid foods, feel free to start with Stage 3. Continue on Stage 3 for at least 6 months.
Feeding foods like peanut, egg, and milk only once or twice is NOT enough. We recommend using Ready, Set, Food!, for at least 6 months, or until your baby is regularly eating the allergens at least 3 times a week. We designed Ready, Set, Food!, to make it safe and easy for parents to not only introduce the allergens, but to sustain exposure as well.
What is Ready, Set, Food! Baby Oatmeal?
Guidelines from the leading medical organizations recommend to feed your baby allergens on a daily basis. Our Baby Oatmeal, now available in a variety of flavors, is a safe and easy solution to help follow the new leading medical guidelines that recommend introducing allergens early and often while giving your child a nutritious and healthy meal. Ready, Set, Food! Baby Oatmeal contains 100% organic milled whole grain oats and includes all of the 9 allergens also found in our Stage 3 Mix-ins:
Our Baby Oatmeal, now available in a variety of flavors, is a safe and easy solution to help follow the new leading medical guidelines that recommend introducing allergens early and often while giving your child a nutritious and healthy meal. Ready, Set, Food! Baby Oatmeal contains 100% organic milled whole grain oats and includes all of the 9 allergens also found in our Stage 3 Mix-ins:
Peanut, Egg, Milk, Cashew (tree nut), Almond (tree nut), Walnut (tree nut), Sesame, Soy, Wheat
These top allergens account for ~90% of all childhood food allergies and follow recommendations from the USDA Guidelines to "introduce infants to potentially allergenic foods." As parents ourselves, our goal is to make early allergen introduction as simple, mess-free and convenient as possible; our Baby Oatmeal is the perfect solution for busy families.
How do I use Ready, Set, Food!?
Ready, Set, Food! is a guided system to make early allergen introduction safe, easy and convenient. Each daily pre-measured packet mixes easily in a bottle or food.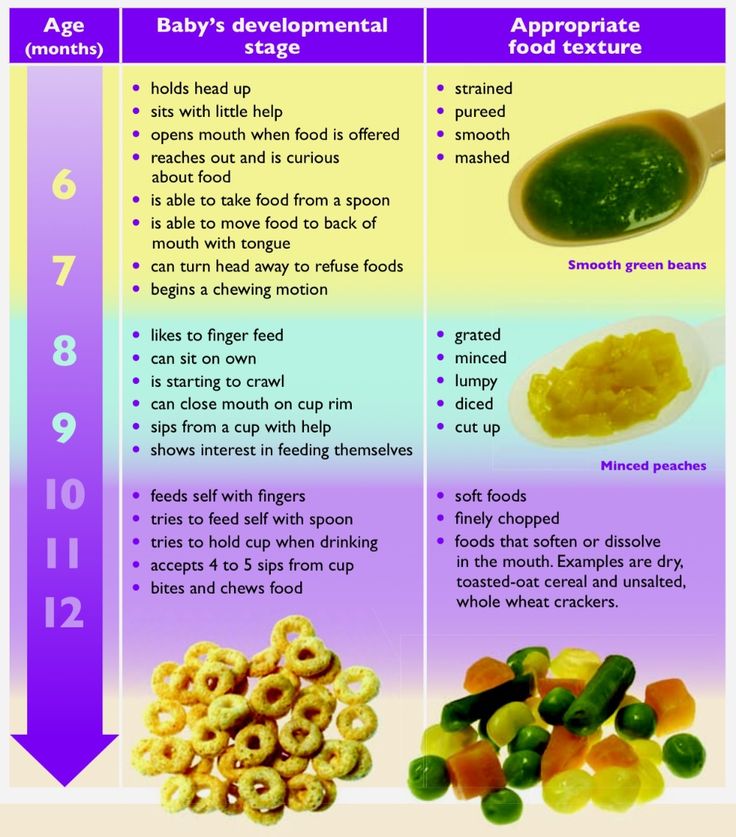 Just shake or stir until dissolved and feed one packet daily.
Just shake or stir until dissolved and feed one packet daily.
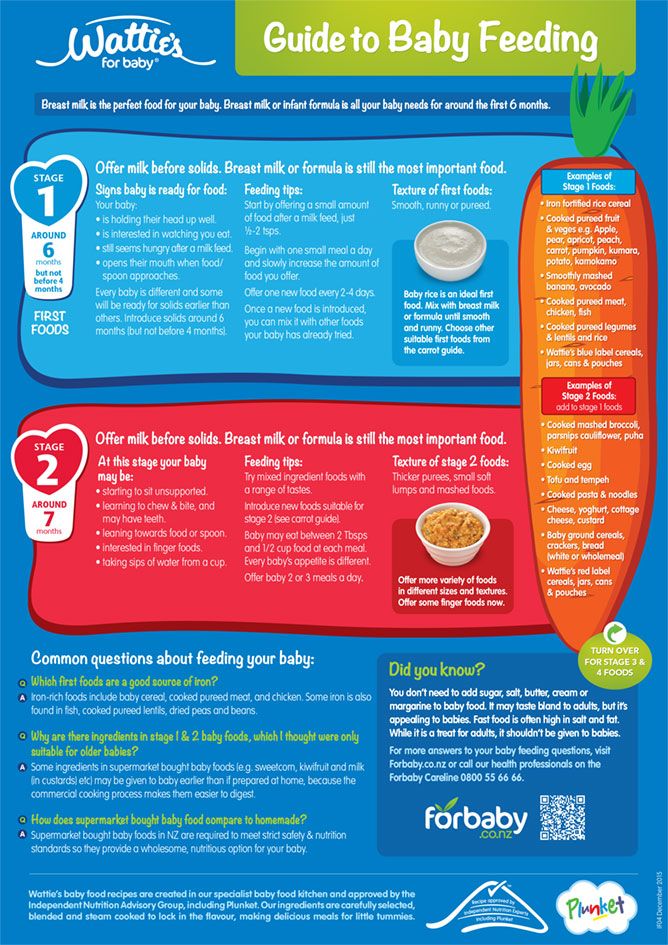
Stage 1
Stage 1 is the introduction to the top 3 allergens - peanut, egg, milk. Start your baby on Stage 1 as early as 4 months of age. Gradually introduce peanut, egg and milk one at a time for the first 30 days. Mix Stage 1 with breast milk, formula, or food.
Stage 2
Stage 2 - Maintains “early and often” exposure to peanut, egg and milk. Start your baby with Stage 2 if you've already introduced these allergens. It is recommended to sustain exposure for at least 3 - 6 months.
Stage 3
Stage 3 is recommended after finishing Stage 2, and if your little one is consistently eating solids such as applesauce, or cheesy mashed potatoes. Once your baby is consistently eating solids, safely expand from peanut, egg and milk to an additional top 6 allergens for at least another 3 - 6 months. If your baby has never started allergen introduction, and is eating solids already, it is okay to start with Stage 3. Mix Stage 3 with food only.
Mix Stage 3 with food only.
Stage 1 + 2 Mix-Ins
Introduce the top 3 allergens safely and easily, one at a time. The only allergen introduction system for babies to start in the bottle. Pre-measured ...
Stage 2 Mix-Ins
Maintain daily exposure to peanut, egg, and milk (top 3 allergens) for at least 6 months. Pre-measured daily packets. 100% organic real food. No added...
Organic Baby Oatmeal
Our Organic Baby Oatmeal provides your baby with a taste they’ll love while introducing the allergens they need right inside every bite. Our 9 top ...
Here is the best way to do it
As a paediatric allergist I am constantly answering questions from friends, relatives, patients and colleagues about introducing allergens to babies. Many people have heard that it’s important to introduce them early, but aren’t clear on exactly why or how to do so.
I strongly encourage early introduction of the major allergens, including milk, eggs, peanuts, tree nuts, wheat, soy, fish, shellfish and sesame into your baby’s diet, as this is the best way to decrease their risk for developing food allergies. As a mom, I know this can feel overwhelming, but it doesn’t have to be. Here are some tips for how to safely introduce allergens to babies.
As a mom, I know this can feel overwhelming, but it doesn’t have to be. Here are some tips for how to safely introduce allergens to babies.
When should you introduce allergens to babies?
The Canadian Paediatric Society (CPS) and Canadian Society for Allergy and Clinical Immunology (CSACI) recommend introducing allergens to all infants at around six months but not before four months. This recommendation especially applies to peanut butter and egg, since evidence supports introducing these allergens early in life to help prevent the development of allergies.
Since there are nine major categories of allergens, it poses quite a challenge to introduce all of them around six months, therefore, practically, many allergists recommend starting allergen introduction between four to six months of age. Personally, I introduced solids for both my daughters at four months, allowing ample time to introduce allergens alongside complementary foods, such as iron-rich foods, fruits and vegetables. I was breastfeeding at the time and continued to do so; introducing solids did not interfere with this.
I was breastfeeding at the time and continued to do so; introducing solids did not interfere with this.
Is introducing allergens important for all babies?
In my clinical experience, many families don’t feel the need to introduce allergens early because they feel that their child is at low risk for developing food allergies. I often hear that “food allergies don’t run in our family”. While I wish it could be that simple, unfortunately, it’s not. According to the Canadian Paediatric Society, an infant is considered to be at high risk for developing food allergies if the infant himself has allergies or eczema, or if there is an immediate family member with an allergic condition. For example, an infant whose sister has asthma is high risk; an infant whose parent has seasonal allergies is also high risk. Bottom line—your baby’s risk may be higher than you think. Food allergy can also develop even in babies with no risk factors.
How to introduce the top allergens
First, let me be clear: Introducing allergens means that your baby needs to be eating the allergenic food—not rubbed on the cheek or lip. It is not recommended (and potentially harmful) to apply foods onto your baby’s skin before feeding them.
It is not recommended (and potentially harmful) to apply foods onto your baby’s skin before feeding them.
When it comes to introducing the major allergens, there is no particular order that needs to be followed. However, because most of the evidence for early introduction stems from studies conducted with peanut butter and egg, I tend to recommend introducing these first.
While I recommend only introducing one major allergen at a time, the traditional advice of waiting three days between introducing new foods is not evidence-based and may unnecessarily prolong the introduction of new foods. It’s important to note that oils (eg. peanut oil, almond oil, sesame oil) do not contain enough protein and therefore, do not count as sufficient allergen exposure. When introducing allergens (and solid food in general) avoid hard or chunky foods, as they are choking hazards. Also, avoid any raw or undercooked foods (e.g. raw eggs, fish or shellfish) and unpasteurized dairy.
Once an allergen is introduced, it is important to maintain it in your baby’s diet on a regular basis. How often? The truth is, we don’t know the precise answer to this, although giving less often than once per week may be ineffective. Ideally, I recommend two to three times per week to start, though this can be more challenging once you have introduced multiple allergens. In that case, I suggest aiming for at least once per week.
Peanut
- Do not feed whole peanuts as they are a choking hazard
- Peanut butter from the jar is too thick for babies, so you can dilute smooth peanut butter with hot water (then cool before feeding it on a spoon), breast milk, formula, or fruit purees and feed it on a spoon. (If you have peanut flour or peanut butter powder on hand, this works too.)
- Peanut puffs (eg. Bamba Peanut Snack) are also an easy way to introduce peanuts to a baby, although they should be softened if your baby is under 7 months.

Egg
- Egg white and yolk can be introduced together. There is no advantage to introducing these separately
- Offer your infant tiny, soft pieces of scrambled egg. It can sometimes take babies a few tries to get used to the texture of the egg so if they don’t like it the first time, keep trying.
- Cooked scrambled egg can also be pureed with breast milk, formula, water, or even a fruit or vegetable puree.
- Another great option is a hard boiled egg, either mashed or blended with water, breastmilk or a puree and fed on a spoon.
Milk
- If your baby is being fed with a cow’s milk-based formula, then they are already being exposed to cow’s milk. If used in early infancy, continuing cow’s milk formula in small amounts daily was shown in recent research to prevent cow’s milk allergy, whereas stopping it increased the risk of developing cow’s milk allergy.
- Many common baby cereals will list ‘skim milk powder’ as an ingredient and can be used to introduce milk. However, if you have not introduced wheat yet, choose an oat or rice cereal that does not contain wheat.
- Yogurt or cottage cheese are also great (if a bit messy!) ways to introduce milk.
- Note that up until 9 months of age, babies should drink either breast milk or formula. Around 9 to 12 months of age, it is okay to introduce homo milk.
Soy
- Many families use soy sauce in cooking, but it does not contain enough soy protein to be considered an introduction and it’s also high in salt
- You may see soy lecithin on an ingredient list for things like baby cereals and formula, but it also does not count as a soy exposure
- Serve extra soft tofu – on its own, or blended with other fruit/vegetable purees.
- Steam and puree edamame and feed on a spoon.

- Serve soy yogurt, mixed with a fruit puree if you’d like.
Wheat
- You can introduce wheat by feeding baby cereals containing ‘wheat flour’—however, avoid those with skim milk powder in the ingredients unless your baby is already tolerating dairy.
- Your baby can eat cooked soft pasta but keep in mind some sauces, particularly tomato sauce, can sometimes cause redness/irritation of the skin (this is not an allergy and isn’t a concern)
- Pancakes (if the other ingredients such as egg and/or dairy have already been successfully introduced).
Tree nuts
- Tree nuts are the most daunting allergen to introduce because there are so many of them, and introducing one doesn’t count as an introduction to all. The main tree nuts that allergists recommend to introduce include almond, cashew, pistachio, hazelnut, walnut, and pecan.
- Other tree nuts that you can consider introducing early are: Brazil nut, Macadamia nut and pine nut (which is technically a seed).
 However, allergy to these specific tree nuts is relatively rare, so some allergists feel that they do not need to be prioritized.
However, allergy to these specific tree nuts is relatively rare, so some allergists feel that they do not need to be prioritized. - There is no particular order that tree nuts need to be introduced. However, when my patients ask for more specific guidance, I usually recommend prioritizing (in no particular order) cashew, hazelnut and walnut, as allergy to these is more common. Fun fact: cashew is closely related to pistachio, so by eating cashew regularly, your child will also gain protection against developing a pistachio allergy. Similarly, walnut is closely related to pecan, so by eating walnut regularly, your child will also gain protection against developing a pecan allergy.
- Introduce them using smooth nut butters (eg. almond butter, cashew butter, hazelnut butter) – these need to be diluted similar to peanut butter, above.
- You can also grind the tree nuts into a fine flour-like consistency – be careful to check for any chunks, which would be a choking hazard.
 This can be mixed with cereals, yogurts (if dairy has already been introduced), smoothies, fruit purees, etc.
This can be mixed with cereals, yogurts (if dairy has already been introduced), smoothies, fruit purees, etc. - Once you’ve had a chance to introduce the tree nuts individually, the best way to maintain them in your baby’s diet is by using a mixed nut butter or ground tree nuts combined with yogurt, cereal, fruit/vegetable purees, smoothies, baked goods and in sandwiches (for older children).
Fish
- It is impossible to introduce every type of fish, so I encourage families to introduce a variety of fish, specifically ones that the family enjoys to eat. For those seeking an easy ‘rule’ on what to prioritize, I tend to recommend salmon, canned tuna and a white fish.
- Serve small pieces/flakes of soft, cooked fish
- For younger babies, steamed fish can be blended with other vegetables- for example, I like to steam salmon and potato and then blend them together for my 5 month old daughter.

- Light canned tuna is the preferred form of tuna according to the FDA (due to concern regarding mercury levels in other forms of tuna, such as Albacore tuna). Some experts recommend waiting until your baby is at least six months before serving tuna because of mercury levels. Avoid the highest mercury fish such as shark, swordfish and marlin.
- Always make sure all bones have been removed from the fish prior to feeding.
Shellfish
- If shellfish is not a part of your family’s diet (for religious, cultural or other reasons), don’t worry about introducing it, especially if you’re only going to feed it once or twice as that will be ineffective. If shellfish is a part of your family’s diet, it still may be difficult and not always practical to give every type of shellfish to your infant. From an allergen standpoint, I recommend that patients focus on at least one crustacean (shrimp, crab, lobster) and one mollusk (eg.
 clam or scallop)
clam or scallop) - Since shellfish can be a bit trickier for a baby to eat, I usually save this allergen for last once my baby has had more practice with eating.
- Options include steamed shrimp, cut into tiny pieces or blended with a vegetable puree or small pieces of soft, cooked lobster tail or scallop
- Your baby might enjoy lobster bisque or clam chowder, assuming other ingredients such as dairy have already been introduced (be sure to avoid large chunks)
- Crab cakes, assuming other allergenic ingredients have been introduced, are another option.
Sesame
- Hummus is a safe, healthy and delicious way to introduce sesame. Note that some children can develop contact/irritant reactions from the lemon juice, salt and garlic, but this is not an allergy
- Tahini can also be given plain although not all babies enjoy the taste, in which case it can be blended with fruits or inside a smoothie.

- Sesame oil and sesame seeds often do not contain sufficient sesame protein to count as a sesame exposure.
What about baby-led weaning?
Unpopular opinion: I am not the biggest fan of baby led weaning (BLW). Since BLW encourages self-feeding with finger foods, it tends to start at age 6 months. It is felt that this approach can have many benefits – including self-feeding skills, fine motor skills, and exposure to different tastes and textures. However, as an allergist, my main issue with BLW is that it is not always conducive with introducing allergens early. Additionally, self-feeding leads to more food being smeared on the skin, which can sometimes cause irritation that is mistaken for food allergy and often confusing. So, for the BLW fans, I’d like to offer a compromise: Consider starting solids (including allergens) between four to six months in a baby-safe format, which may not always include finger foods (and that’s okay!). Especially for the common allergens, strongly consider feeding these foods with a spoon for the first several weeks, so you don’t mistake irritation from smeared food as an allergic reaction. When your baby reaches six months or is more developmentally ready for finger foods, you can transition to Baby Led Weaning. Babies can still learn self-feeding skills from eating purees. My little ones loved to suck their fingers and enjoyed trying to feed themselves with a soft baby spoon.
Especially for the common allergens, strongly consider feeding these foods with a spoon for the first several weeks, so you don’t mistake irritation from smeared food as an allergic reaction. When your baby reaches six months or is more developmentally ready for finger foods, you can transition to Baby Led Weaning. Babies can still learn self-feeding skills from eating purees. My little ones loved to suck their fingers and enjoyed trying to feed themselves with a soft baby spoon.
What are the symptoms of an allergic reaction?
The vast majority of allergic reactions will occur within two hours of consuming the food. Symptoms include hives, swelling (eg. swollen lips, swollen skin around the eyes), vomiting, abdominal pain, coughing, wheezing, hoarse voice or hoarse cry, irritability and lethargy.
The good news: the risk of a severe reaction when infants eat a food for the first time is extremely low. As well, anaphylaxis in infants tends to be milder compared to anaphylaxis in older children. All the more reason to introduce allergens when your kids are infants.
All the more reason to introduce allergens when your kids are infants.
Remember, babies can get rashes for lots of different reasons, most commonly in association with a viral illness. Don’t assume that every rash is a food allergy—especially if the rash lasts for more than a day, if the rash came on randomly (rather than within two hours of eating an allergen), or if your baby has been experiencing infectious symptoms such as fever, runny nose or cough.
Also some rashes are nonallergic contact reactions. If your baby develops flat or dry redness of the skin that is isolated to areas where the food contacts the skin (e.g. around the mouth or chin), this might be what we call a contact or irritant reaction. This is NOT an allergy, but can sometimes be mistaken for one. The difference is that contact reactions are not harmful, and you do not need to avoid these foods. If you are unsure, take photos and check with your physician. If your baby has eczema or sensitive skin, you can consider applying a protective barrier to the skin before feeding new foods. I like to use Vaseline for this purpose and apply it around the lips, cheeks and chin, before and after feeding. Eliminating foods from your baby’s diet for the purpose of treating eczema is strongly discouraged—in the long term, this may increase your baby’s risk for developing anaphylaxis to those same foods.
I like to use Vaseline for this purpose and apply it around the lips, cheeks and chin, before and after feeding. Eliminating foods from your baby’s diet for the purpose of treating eczema is strongly discouraged—in the long term, this may increase your baby’s risk for developing anaphylaxis to those same foods.
What do you do if your kid has an allergic reaction?
If there are any concerns for severe allergic symptoms call 911 and seek immediate medical attention. If your child already has known food allergies and carries an epinephrine autoinjector, this should be administered without delay.
For mild symptoms, it is recommended to monitor your child very closely and have a low threshold to seek medical attention if any further concerns develop. Consider taking photos of any skin reactions. Avoid the specific food that was consumed until you have a chance to speak with your physician.
It is important to note that epinephrine is the only life-saving treatment for a severe allergic reaction. Benadryl (diphenhydramine) is not recommended, because it often causes drowsiness, which is difficult to differentiate from drowsiness associated with a severe allergic reaction.
Benadryl (diphenhydramine) is not recommended, because it often causes drowsiness, which is difficult to differentiate from drowsiness associated with a severe allergic reaction.
Melanie Conway is a paediatrician, paediatric allergist, and a mom with two girls, Rebecca (2.5 years) and Freya (5 months).
Stay in touch
Subscribe to Today's Parent's daily newsletter for our best parenting news, tips, essays and recipes.- Email*
- CAPTCHA
- Consent*
Yes, I would like to receive Today's Parent's newsletter. I understand I can unsubscribe at any time.**
FILED UNDER: allergic reaction Allergies baby food feeding health service seo Starting solids
Allergy to baby food in a child: nutrition for infants with allergies
Published: 03/16/2017
Reading time: 4 min.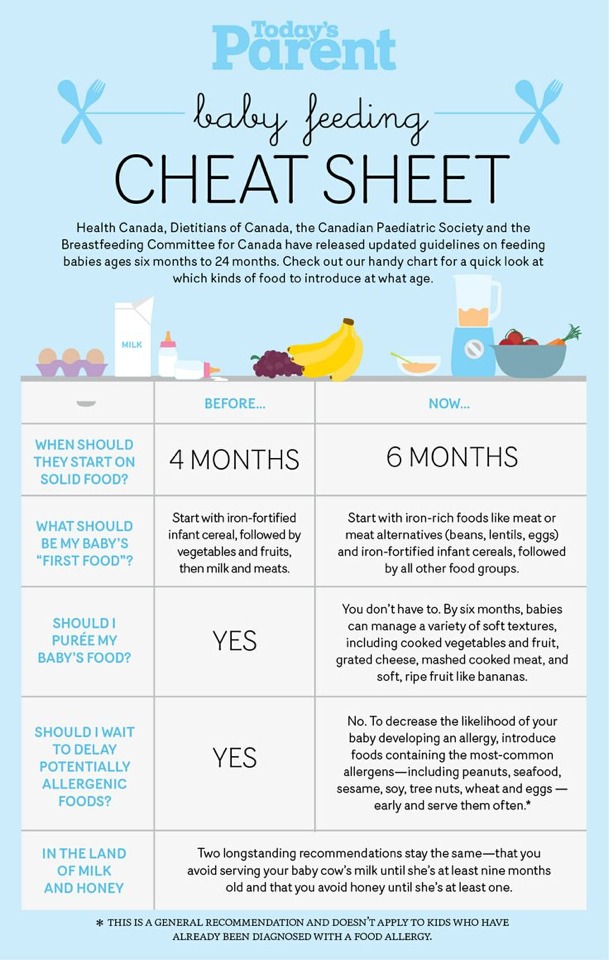
Number of reads: 31455
Author of the article: Ponomareva Yulia Vladimirovna
Pediatrician, Candidate of Medical Sciences, Allergist-Immunologist
Food allergy is one of the most common health problems in a baby in the first year of life. According to statistics, every third child of this age has manifestations of food intolerance. Many parents are concerned about the question of what this condition is connected with and whether it is possible to avoid the development of an allergy to baby food in a baby.
Content: Hide
- State of the art
- Food allergy
- Major allergens
- Prevention is easier than cure
- Transition period
- Where to start?
- Complementary cereals in the diet of allergy sufferers
- Benefits of industrial baby food
Current state of the problem
In developed countries, there is a steady increase in allergic diseases every year, not only among children, but also among adults. There is no definitive answer about the reason for the increase in the incidence rate, but the role of factors such as living in large metropolitan areas, the distance of a person from nature, and a decrease in infectious load at an early age is being discussed. The immune system of the child, not receiving infectious stimuli, begins to respond to factors that normally do not cause any reactions - food, pollen or pet hair. In most babies at an early age, allergy manifestations are associated with food intolerance. Typically onset is in children over 3 months of age, with peak incidence at 5–9months. Often the first symptoms are associated with the start of the introduction of complementary foods.
There is no definitive answer about the reason for the increase in the incidence rate, but the role of factors such as living in large metropolitan areas, the distance of a person from nature, and a decrease in infectious load at an early age is being discussed. The immune system of the child, not receiving infectious stimuli, begins to respond to factors that normally do not cause any reactions - food, pollen or pet hair. In most babies at an early age, allergy manifestations are associated with food intolerance. Typically onset is in children over 3 months of age, with peak incidence at 5–9months. Often the first symptoms are associated with the start of the introduction of complementary foods.
Food allergies
Why do babies have so many food allergies? In addition to hereditary predisposition to allergic diseases, the immaturity of the digestive system, early cessation of breastfeeding, and disturbances in the intestinal microbiota play an important role.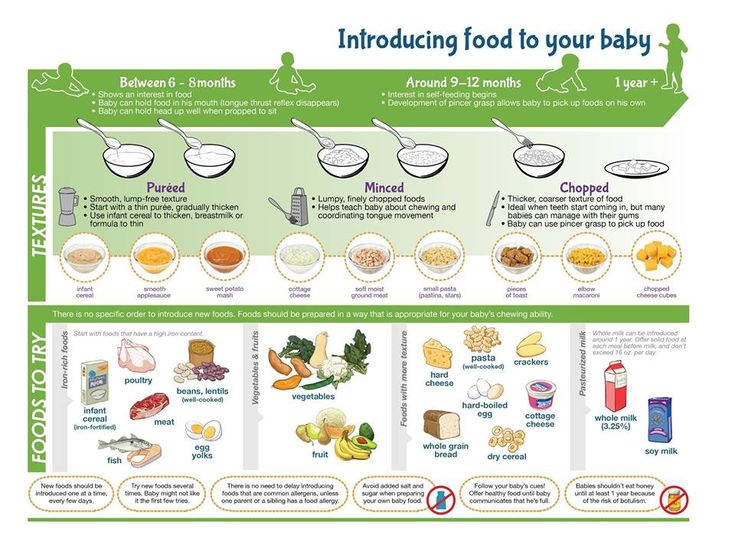 The introduction of foods with a high allergenic potential into the diet, as a rule, gives rise to the first manifestations of allergies. It is not difficult to diagnose this condition, typical manifestations are itchy skin rashes and disorders of the gastrointestinal tract. Often there is a causal relationship between rashes and the use of a particular product. Allergy symptoms cause anxiety to the baby, disrupt his sleep and quality of life. And the lack of adequate timely treatment increases the risk of further development of respiratory diseases such as allergic rhinitis and bronchial asthma.
The introduction of foods with a high allergenic potential into the diet, as a rule, gives rise to the first manifestations of allergies. It is not difficult to diagnose this condition, typical manifestations are itchy skin rashes and disorders of the gastrointestinal tract. Often there is a causal relationship between rashes and the use of a particular product. Allergy symptoms cause anxiety to the baby, disrupt his sleep and quality of life. And the lack of adequate timely treatment increases the risk of further development of respiratory diseases such as allergic rhinitis and bronchial asthma.
Major allergens
Almost any food can cause an allergic reaction, but in 90% of cases only a few allergens are responsible for this condition: cow's milk, chicken eggs, wheat, fish and seafood, soy, tree nuts (peanuts are the most common among them). ). Heat treatment does not lead to a decrease in allergenicity, therefore the most effective method of treatment is to completely eliminate the causative product from the baby's diet. Allergy to several products at once occurs quite rarely, but you need to be aware of the possibility of cross-reactions. So, a baby with an allergy to cow's milk protein has a high risk of reactions to the milk of other mammals and beef, with intolerance to a chicken egg, a reaction to chicken meat is likely, and intolerance to other gluten-containing cereals is possible with a reaction to wheat protein. Cow's milk protein is the most common cause of food allergies, so mothers should follow a strict dairy-free diet if their child develops an intolerance. If the baby is bottle-fed, special therapeutic mixtures are recommended in the diet, which are based on the most split milk protein. In addition to the exclusion of dairy products, the timing of the introduction of other strong food allergens - chicken eggs and fish, is being postponed, these products are used in the menu of children older than a year.
Allergy to several products at once occurs quite rarely, but you need to be aware of the possibility of cross-reactions. So, a baby with an allergy to cow's milk protein has a high risk of reactions to the milk of other mammals and beef, with intolerance to a chicken egg, a reaction to chicken meat is likely, and intolerance to other gluten-containing cereals is possible with a reaction to wheat protein. Cow's milk protein is the most common cause of food allergies, so mothers should follow a strict dairy-free diet if their child develops an intolerance. If the baby is bottle-fed, special therapeutic mixtures are recommended in the diet, which are based on the most split milk protein. In addition to the exclusion of dairy products, the timing of the introduction of other strong food allergens - chicken eggs and fish, is being postponed, these products are used in the menu of children older than a year.
Prevention is easier than cure
Is it possible to avoid developing allergies to baby food? Indeed, this disease is better to prevent than to cure. Of course, the presence of allergic diseases in the immediate family determines the risk of developing allergies in the child. Therefore, parents at the earliest stages should take care of the prevention of this condition. Modern experts do not recommend a special diet for mom during pregnancy. Her diet should be complete and varied as much as possible, in reasonable quantities she can eat various foods, including unconditional allergens. The baby, even in the womb, begins to get acquainted with the whole variety of food. Unnecessary use of antibiotics during pregnancy should be avoided and, when planning a mode of delivery, only cesarean delivery should be considered when absolutely necessary. These factors play an important role in disrupting the development of the gut microbiota, which in turn increases the risk of allergic reactions. Another key factor is early breastfeeding. If there is a need for artificial feeding or supplementary feeding to a baby at risk of developing allergies, nutrition should be organized on the basis of special preventive mixtures that a specialist can recommend.
Of course, the presence of allergic diseases in the immediate family determines the risk of developing allergies in the child. Therefore, parents at the earliest stages should take care of the prevention of this condition. Modern experts do not recommend a special diet for mom during pregnancy. Her diet should be complete and varied as much as possible, in reasonable quantities she can eat various foods, including unconditional allergens. The baby, even in the womb, begins to get acquainted with the whole variety of food. Unnecessary use of antibiotics during pregnancy should be avoided and, when planning a mode of delivery, only cesarean delivery should be considered when absolutely necessary. These factors play an important role in disrupting the development of the gut microbiota, which in turn increases the risk of allergic reactions. Another key factor is early breastfeeding. If there is a need for artificial feeding or supplementary feeding to a baby at risk of developing allergies, nutrition should be organized on the basis of special preventive mixtures that a specialist can recommend.
Transition period
The next most important step in the prevention of food allergies is the correct introduction of complementary foods. This is a crucial moment in the baby's life, since on the one hand it is necessary to introduce each product with caution, carefully monitoring possible reactions, and giving preference to low-allergenic products. On the other hand, it is wrong to delay the expansion of the diet. It is important to introduce all major food groups in as much variety as possible between 5 and 8 months. This is the corridor for the formation of an adequate response of the immune system to food products, when it is ready to recognize and accept food, which allows a person to eat these products in subsequent years without the risk of allergic reactions.
Where to start?
In infants at risk of developing food allergies, the general recommendations for starting food groups follow the standard approach. That is, complementary foods can be started with vegetables or cereals. Vegetable complementary foods would be preferable in a child with functional digestive disorders with a tendency to stool retention. Low-allergenic green and white vegetables such as squash, cauliflower, and broccoli are good choices. The first vegetable complementary foods should not contain salt, sugar and prepared without adding milk. In other cases, in children with food allergies or the risk of their occurrence, cereals are the best option for starting complementary foods. Why cereals? Under the conditions of compliance with a hypoallergenic diet by the mother and forced restrictions on the child's diet, cereals, as a source of essential nutrients, vitamins and minerals, significantly increase the nutritional, biological and energy value of the diet.
Complementary cereals in the diet of allergy sufferers
Can a child with an allergy or a predisposition to develop it have any porridge? Of course, not any. Dairy-free and gluten-free products are introduced as the first cereal food. Whole cow's milk, due to the high risk of food intolerance, is excluded from the diet of this group of children at least until the end of the first year of life. Accordingly, porridge is prepared on the basis of mother's milk, a specialized mixture or baby water without the addition of salt and sugar. Gluten-free cereals include buckwheat, rice and corn. How to cook porridge based on mother's milk in order to preserve all the valuable biological substances? Cooking is certainly detrimental to the protective antibodies, enzymes, hormones, and beneficial bacteria found in breast milk. Therefore, the best solution is to use commercially produced instant cereals for baby food. Mother's milk or a specialized formula can be heated in a water bath to 40 ° C, add the dry part in accordance with the manufacturer's recommendations and quickly get a ready-to-eat meal, preserving all the most valuable for the baby's health.
Benefits of industrial baby food
In addition to being quick and easy to prepare, modern industrial baby food meets high quality and environmental standards. The Bebi Premium product line "Porridges for the first feeding" is a good choice for babies with food allergies or a predisposition to them. It is preferable to start with a subgroup of low-allergenic cereals from this line. They fully comply with all the conditions for introducing cereal complementary foods to babies with food allergies. A distinctive feature of these products is an enriched composition, including prebiotics and the most important vitamins and minerals for this age. Prebiotics support the gut's own microbiota, which play a significant role in causing allergies. By the 6th month of life, vitamins and minerals are already supplied in insufficient quantities with mother's milk, especially in the conditions of the mother's hypoallergenic diet, so their guaranteed intake with complementary foods is a reliable prevention of deficient conditions in the baby.
Rate the article
(Number of votes: 21, average 4.8)
Share with friends:
Major food allergens | Nestle Baby
Baby allergies have many distinctive symptoms, the most common of which are eczema, rashes (scaly patches that are wet or dry, and seborrheic crusts on the baby's head), digestive problems (flatulence, colic, loose stools or constipation) and breathing difficulties (asthmatic bronchitis, bronchial asthma). The risk group for developing allergies includes infants whose parents or siblings suffer from an allergic reaction to any product. If food allergy was observed in one of the parents, then the risk of its development in the child reaches 20-40%, if both, then the probability of the child increases to 60-80%, and not this or that disease is inherited, but the very predisposition to it.
The immune system of baby begins to form in the womb and then, during the first year of life, "matures", encountering various foreign environmental factors, learning to recognize them and defend itself. During 15-16 years there are constant changes that can be considered as the development and formation of "adult" immunity. But the first year of life is the most difficult and responsible.
For a baby, food is the main and main source of foreign proteins, potential allergens. Especially dangerous for an infant is the early introduction of ordinary children's dairy products with whole cow's milk protein, and even more so whole milk, into the diet, since a child's allergy in a newborn to cow's milk protein, developing very quickly, can cause acute and even life-threatening reactions in the child.
The timely appearance of certain beneficial bacteria in the intestines is also very important for the formation of the child's immunity. These are primarily bifidobacteria and a little later lactobacilli. The establishment of a normal microflora helps the cells of the intestinal mucosa to properly process and assimilate food, as well as more effectively prevent the development of an allergic reaction to foreign proteins.
With mother's milk, the child "passively" receives immunoglobulins and other protective factors to avoid infection and the early development of food allergies in the newborn infant, even if there is a family predisposition. Breast milk contains a small amount of proteins from the food eaten by the mother, which prepares the baby for a painless encounter with these foods in the future.
Prevention of food allergies
As you know, it is better to prevent a disease than to treat it later. Mistakes in the diet of babies predisposed to allergies often begin immediately after the birth of a child. Usually, after giving birth, the mother has very little milk, but it has a special composition, “invented” by nature for feeding a newly born little man. This "starter", highly nutritious milk is called colostrum and is gradually replaced by breast milk. The apparent "lack" of colostrum milk in the first 3-4 days of a child's life is normal; it is not necessary to supplement the baby with any special children's dairy products. Immediately after birth, children are often restless and additional artificial nutrition calms them, creating a false effect of well-being. Such a desire to "feed and soothe" the child is contrary to the laws of nature and can be a disservice if the baby has a predisposition to allergies. Feeding such babies with cow's milk protein-based infant formula immediately after birth means several times the risk of developing food allergies.
Therefore, the first rule of : do not supplement a child with a predisposition to allergies with conventional infant milk products, and if necessary, use only special hypoallergenic infant dairy products with a proven preventive effect.
Hypoallergenic means that infant formula helps prevent food allergies in the baby. When creating such children's dairy products, manufacturers of baby food using a special treatment (hydrolysis) break down the protein found in the infant formula. All hypoallergenic baby dairy products are divided into moderately hydrolyzed and highly hydrolyzed, depending on how much protein is broken down in them. Highly hydrolyzed infant formula can be conditionally called non-allergenic, since it does not contain or almost does not contain proteins that can cause or maintain children's allergies, and is used mainly to treat an already developed allergic reaction. Such children's dairy products should not be used alone, without medical supervision. If a food allergy has already developed, then first of all it is necessary to consult a doctor who will select the treatment and help determine the diet.
Moderately hydrolyzed baby milk products break down cow's milk protein into "medium" sized pieces that are less likely to cause an allergic reaction than whole milk protein. In addition, it is the partially cleaved protein that affects the immune cells of the child's intestines, causing the production of immunity and suppressing allergic reactions. This process is called the formation of tolerance (tolerance) to cow's milk protein, i.e. normal tolerance without the development of allergies. Partially digested protein infant formula is designated H. A. (H. A. stands for HypoAllergenic, that is, hypoallergenic). Thus, hypoallergenic infant milk products have a dual effect on the immune system: they prevent the development of infant allergy to infant formula and promote gradual addiction to milk protein.
Second rule: Breastfeed your baby for as long as possible, at least until six months of age . It will be better if a nursing mother limits the consumption of chicken eggs, milk and dairy products, fish and seafood, chicken meat, peas, beans, beans, and millet. These foods should not be completely excluded, but it is better to eat them not every day and in moderation. You should also limit the use of long-term storage products containing dyes, spices, preservatives, stabilizers and food additives.
The most important condition for the prevention of allergies, which, unfortunately, is often violated, is not to introduce complementary foods - cereals, vegetable puree, cottage cheese - for up to four months. In the first six months, feed the baby only with breast milk, and in case of its deficiency, if the child is predisposed to allergies, with a special hypoallergenic infant formula. After the sixth month, the baby's diet gradually expands, however, up to a year, children with a predisposition to allergies should not be given whole milk (both cow's and goat's), kefir and other dairy products; up to one and a half and even up to two years, it is better to exclude eggs, fish, seafood; up to three years - nuts, peanuts, honey. This “delayed” introduction of foods that are more likely to be food allergens helps to reduce the likelihood of childhood allergies.
Introduction of complementary foods to children with food allergies
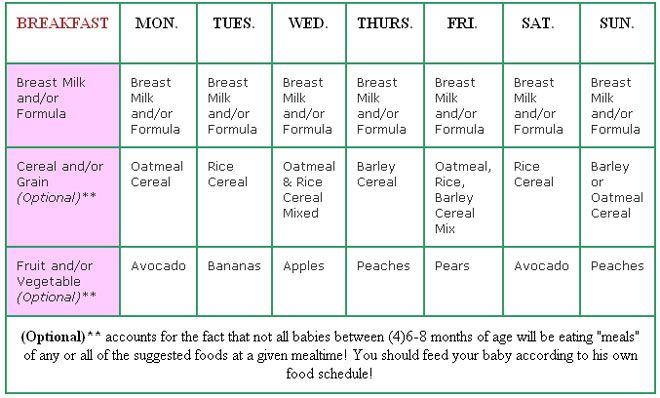
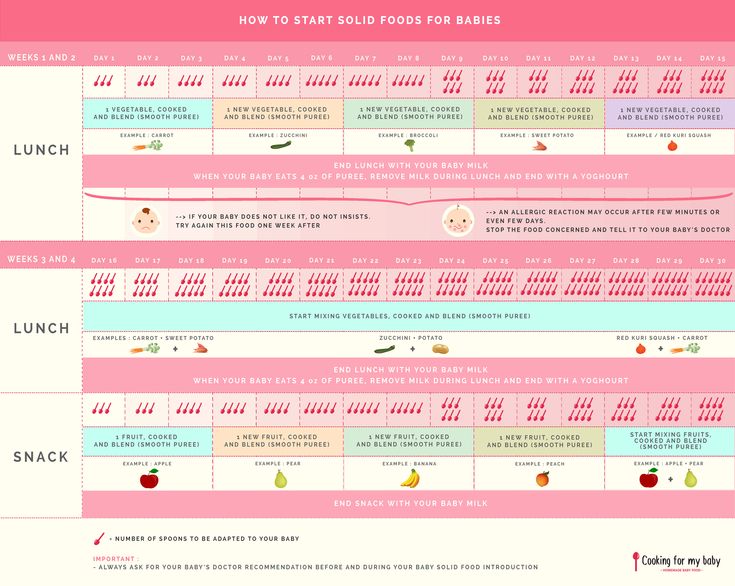
Complementary foods are introduced to infants at risk at a later date than their healthy peers - from 5-6 months of life.
When feeding a child up to a year old, pediatricians recommend starting complementary foods with one-component purees or cereals in order to be able to track the reaction of the baby's body.
If the child has frequent loose or unstable stools and is not gaining weight well, give him porridge as the first food. Children with overweight and constipation are given vegetable puree first.
For children with food allergies in the first year, 1 type of cereal, 1 type of meat, 1-2 types of vegetables and fruits is enough.
Beef has an antigenic affinity for cow's milk proteins and may also cause allergies. It is better to give piglet or turkey meat. Among meat purees, choose those that do not contain broth, spices, or salt.
Introduce whole cow's milk after 1 year of age, whole eggs after 2 years, fish and nuts after 3 years.
Introduce a new product only when the baby is healthy, starting with ½ tsp. and gradually increasing its volume. In case of poor tolerance, temporarily exclude the product and try to give it again after a few days.
Give each new product 5-7 days in a row before introducing another one to track the reaction of the baby's body.
Replenish your child's diet with single-ingredient foods only - reactions to one or another ingredient are difficult to track when using multi-ingredient products.
Give complementary foods from a spoon in the morning and afternoon to track the reaction to the product during the day.
Low allergenic foods: cauliflower, green apple, plum, pear, rice porridge, rabbit, turkey.
The most common food allergens are: cow's milk, eggs, fish, nuts, soy, wheat, citrus fruits, honey, chocolate, strawberries, tomatoes.
If your child is allergic to cow's milk, avoid milk and dairy products (yogurt, cream, etc.) from the diet. The doctor will recommend how you can replace them. To avoid nutritional deficiencies, your doctor will advise you to drink calcium-fortified water or increase your daily intake of fruits and vegetables, and recommend hypoallergenic infant formula. As a rule, over time, children's allergies of this type disappear.
Gluten
Gluten is a vegetable protein found in certain grains (rye, wheat, barley, oats) and products made from them (pasta, biscuits, bread). Gluten allergy occurs in about one in 2,000 children. Among her symptoms is diarrhea, accompanied by a small increase in weight and bloating. If you notice these symptoms, see your doctor. If the baby is allergic to gluten, exclude foods containing it from the diet and feed the baby gluten-free cereals: buckwheat, rice, corn.
Chicken eggs
In eggs, allergens are mainly contained in the protein, but not only. Doctors recommend not to give the child egg whites in the first year of life. It is necessary to be attentive to the composition of products: eggs, like cow's milk and peanuts, are used in the preparation of a wide variety of foods, as well as individual vaccines (for mumps, flu, etc.). Symptoms of an egg allergy can be respiratory (asthma) or skin (eczema or rash) in nature. In order not to leave the child without animal proteins, replace eggs with meat, oily fish or cereals.
Will a child outgrow a food allergy?
Children's food allergies are most common in children under 2 years of age. In most of them, adverse reactions to food allergens decrease as immunity is strengthened and treatment is carried out. However, an allergic reaction to nuts, fish, and seafood can last a lifetime. Give the child this food not earlier than the above terms.
The GERBER ® baby food range includes a large number of one-component fruit, vegetable and meat purees, juices and cereals, on the basis of which you can create an individual hypoallergenic diet for your baby.
Doctor of Medicine, Head of the Department of Nutrition for Children and Adolescents at the Morozov Children's City Clinical Hospital Tatyana Nikolaevna Sorvacheva: "The growth of atopic diseases worldwide in recent years indicates the need to develop effective preventive measures, starting from the earliest age of the child.