Feeding bottle for 1 month baby
Bottle-Feeding (Formula) Questions
Is this your child's symptom?
- Formula and bottle-feeding questions
Topics Covered for Formula Feeding
If your baby is healthy, skip the "What to Do" section. Go directly to the topic number that relates to your question for advice:
- Types of formulas
- Switching formulas and milk allergies
- Powdered versus liquid formulas
- Whole cow's milk, 2%, 1% and skim milk
- Vitamins and iron
- Water to mix with the formula
- Extra water
- Amounts: how much per feeding?
- Schedules or frequency of feedings
- Length of feedings
- Night feedings: how to eliminate?
- Formula temperature
- Formula storage
- Cereals and other solids
- Burping
- Baby bottle tooth decay
- Traveling
- Nipples and bottles
- Normal stools
- Breast discomfort
When to Call for Bottle-Feeding (Formula) Questions
Call 911 Now
- Can't wake up
- Not moving or very weak
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Age less than 1 month old and looks or acts abnormal in any way
- Dehydration suspected.
No urine in more than 8 hours, dark urine, very dry mouth and no tears.
- Will not drink or drinks very little for more than 8 hours
- Fever in baby less than 12 weeks old. Caution: do NOT give your baby any fever medicine before being seen.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- Does not seem to be gaining enough weight
- You think your child needs to be seen, but the problem is not urgent
Contact Doctor During Office Hours
- You have other questions or concerns
Self Care at Home
- Bottle-feeding question about a healthy baby
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
- Virtual Urgent Care
Care Advice for Bottle (Formula) Feeding
- Types of Formulas:
- Milk-protein formulas, soy-protein formulas, and hydrolysate formulas
- Soy formulas don't contain lactose or cow's milk protein.
 Currently, 20% of infants in the U.S. are fed soy formula. Often, switching to soy is not done with a valid reason.
Currently, 20% of infants in the U.S. are fed soy formula. Often, switching to soy is not done with a valid reason. - Hydrolysate formulas mean the protein is broken down. These are advised when children are sensitive to both soy and milk protein.
- Switching Formulas and Milk Allergies:
- Switching from one milk-based formula to another is not helpful for any symptom. It is also not harmful.
- Switching from milk formula to soy formula is sometimes helpful for severe diarrhea. This may occur from temporary low lactase levels. It may also be used for those families who are vegetarian.
- Switching from milk formula to soy is sometimes helpful for cow's milk allergy. A cow's milk allergy occurs in 1-2% of infants. Most often, protein hydrolysate formulas (such as Alimentum) are advised. This is because 15% of these infants are also allergic to soy protein.
- Switching formulas for frequent crying, spitting up or gas is rarely helpful.

- Don't switch formulas without talking with your child's doctor.
- Powdered versus Liquid Formulas:
- Formulas come in 3 forms: powder, concentrated liquid and ready-to-feed liquid.
- Concentrated formulas are mixed 1:1 with water.
- Ready-to-feed formulas do not need any added water.
- Powdered formulas are mixed 2 ounces (60 mL) of water per each level scoop of powder. Never add extra water because dilute formula can cause a seizure.
- Powdered formula costs the least. Ready-to-feed formula costs the most.
- Powdered formula is the easiest to use to supplement breastfeeding.
- Ready-to-feed formula is the easiest to use for traveling.
- Whole Cow's Milk, 1%, 2% and Skim Milk:
- Cow's milk should not be given to babies before 12 months of age. Reason: raises risk of iron deficiency anemia.
- Skim milk (fat free milk), 1% low fat milk or 2% milk should not be used before 2 years.
 Reason: the fat content of whole cow's milk (3.5%) is required. It is needed for rapid brain growth.
Reason: the fat content of whole cow's milk (3.5%) is required. It is needed for rapid brain growth.
- Vitamins and Iron:
- For all infants, use a formula that has iron in it. This helps to prevent iron deficiency anemia.
- The iron amount in iron-fortified formulas is too small to cause any symptoms. Iron in formulas does not cause constipation or diarrhea.
- Iron-fortified formulas contain all the vitamins and minerals needed.
- Extra vitamins are therefore not needed for infants taking formula.
- Fluoride. Babies no longer need to take fluoride drops. Reason: the fluoride in toothpaste works very well. For children at high risk for tooth decay, your dentist may use fluoride varnish.
- Water to Mix With the Formula:
- Most city water supplies are safe for making 1 bottle at a time. Run the cold tap water for 1 minute. Don't use warm tap water. Reason: to avoid potential lead exposure.
 Heat cold water to desired temperature. Add this to powder or formula concentrate.
Heat cold water to desired temperature. Add this to powder or formula concentrate. - Exceptions:
- Untested well water or
- City water with recent contamination or
- Developing countries with unsafe water supply or
- Your child has decreased immunity.
- For these conditions, use distilled water, bottled water, or filtered tap water.
- Another option is to use city water or well water that has been boiled. Boil for 10 minutes. Add 1 extra minute per each 1,000 feet (305 meters) of elevation.
- Bottled water costs more than distilled water.
- If making a batch of formula, distilled, bottled or boiled water is needed.
- Most city water supplies are safe for making 1 bottle at a time. Run the cold tap water for 1 minute. Don't use warm tap water. Reason: to avoid potential lead exposure.
- Extra Water:
- Babies less than 6 months of age should not be given any extra water. Reason: regular formula is 85% water. Also, water can cause harm at this age.
- Infants older than 6 months of age can have some extra water. Reason: water may be needed after starting solid foods or if weather is very hot.
 Safe at this age.
Safe at this age. - Limit water for infants age 6 to 12 months: don't give more than 4 ounces (120 mL) of extra water per day. On hot days, can give up to 8 ounces (240 mL) per day (AAP).
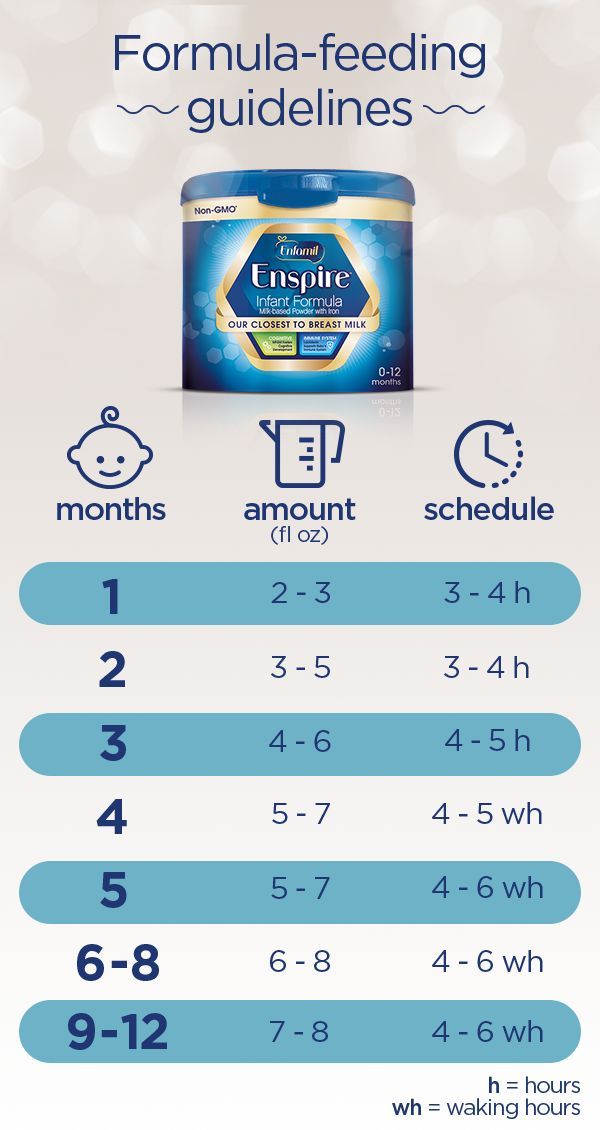
- Amounts - How Much Per Feeding: Newborn to 6 Months Old
- The average amount of formula that babies take per feeding is:
- Newborn: 1-2 ounces (30-60 mL) per feeding
- 1 month old: 3-4 ounces (90-120 mL) per feeding
- 2 months old: 5 ounces (150 mL) per feeding
- 4 months old: 6 ounces (180 mL) per feeding
- 6 months old: 7-8 ounces (210-240 mL) per feeding
- The amount can vary depending on the baby's weight and if the baby is going through a growth spurt.
- A baby's appetite varies throughout the day. If the infant stops feeding or loses interest, the feeding should be stopped.
- If healthy babies are not hungry at several feedings, increase the feeding interval.
- The most amount of formula advised per day is 32 ounces (1 liter).

- Over-feeding can cause vomiting, diarrhea or too much weight gain.
- If your baby needs over 32 ounces (1 liter), talk to your doctor about starting solids.
- Get rid of any formula left in bottle at end of each feeding. Do not reuse this leftover formula. Reason: contains germs that can grow.
- Frequency of Feedings (Schedules): Babies mainly need to be fed when they are hungry. If your baby is fussy and it's been more than 2 hours, feed him. Some guidelines are listed below:
- From birth to 3 months of age, feed every 2 to 3 hours.
- From 3 to 9 months of age, feed every 3 to 4 hours.
- Infants often set their own schedule by 1 to 2 months of age.
- Length of Feedings:
- Feedings shouldn't take more than 20 minutes.
- If the feeding is prolonged, check the nipple to be sure it isn't clogged.
- A clean nipple should drip about 1 drop per second. Check this when the bottle of formula is turned upside down.

- Night Feedings - How to Get Rid of Them:
- Most newborns need to be fed at least twice each night.
- Most formula-fed babies give up night feedings by 4 months of age. The tips below can help your baby sleep for longer stretches during the night:
- Keep daytime feeding intervals to at least 2 hours. Slowly stretch them to 3 hours.
- During daytime, your baby shouldn't sleep for more than 3 hours at a time. If your baby naps longer than that, wake him for a feeding.
- Place your baby in the crib drowsy but awake. Don't bottle-feed or rock until asleep.
- Make middle-of-the-night feedings brief and boring compared to daytime feedings. Don't turn on the lights or talk to your child. Feed him rather quickly.
- Formula Temperature:
- Most babies like formula at body temperature.
- In the summertime, some infants prefer formula that's cooler.
- In the wintertime, some prefer warm formula.

- The best temperature is the one your infant prefers. Either way, there's no health risk involved.
- Just make sure the formula is not too hot. Reason: it can burn your baby's mouth.
- Formula Storage:
- If you can, make your child's formula fresh for each feed. However, if formula needs to be made ahead of time:
- Prepared formula should be stored in the refrigerator. It must be used within 24 hours.
- Open cans of formula should also be kept in the refrigerator. They should be covered and used within 24 hours.
- Prepared formula left at room temperature for more than 1 hour should be discarded.
- Leftover used formula should always be tossed. Reason: contains germs that can grow.
- Cereals and Other Solids:
- Bottle-fed infants should be started on baby foods around 6 months of age. First baby foods can be cereals and/or fruit.
- Starting before 6 months is not needed.
 Starting before 6 months makes feedings messier and longer. Early use of solids can also cause gagging.
Starting before 6 months makes feedings messier and longer. Early use of solids can also cause gagging. - Solids don't increase sleeping through the night for bottle-fed infants.
- Delaying solids past 9 months of age is not advised. The delay runs the risk that your infant will refuse solids.
- Burping:
- It is not harmful if a baby doesn't burp.
- Burping is an option, but not required.
- It can decrease spitting up, but it doesn't lessen crying.
- Burping can be done twice per feeding, once midway and once at the end.
- If your baby does not burp after 1 minute of patting, it can be stopped.
- Baby Bottle Tooth Decay:
- Some older infants and toddlers are used to a bottle before sleeping.
- Falling asleep with a bottle of milk or juice can cause severe tooth decay.
- Prevent this bad habit by not using the bottle as a pacifier. Also, do not use the bottle as a security object.

- If you cannot stop the bottles, fill it with water. Use water instead of formula or milk at bedtime.
- Traveling:
- Use bottles of ready-to-feed formula (most expensive).
- Or mix formula ahead of travel and carry in a cold insulated container.
- Or use powered formula. Put the required number of scoops in a bottle. Carry clean water in a separate bottle. Mix before each feeding.
- Nipples and Bottles:
- Any nipple/bottle products are fine.
- It is not necessary to sterilize bottles or nipples. Wash them with soap and water. Rinse them thoroughly.
- It is also safe to wash bottles and nipples in the dishwasher.
- Formula-fed Stools, Normal:
- Meconium Stools are dark greenish-black, thick and sticky. They normally are passed during the first 3 days of life.
- Transitional Stools are a mix of meconium and milk stools.
 They are greenish-brown and looser. They are passed day 4 to 5 of life.
They are greenish-brown and looser. They are passed day 4 to 5 of life. - Normal Milk Stools without any meconium are seen from day 6 on.
- Formula-fed babies pass 1 to 8 stools per day during the first week. Then it starts to slow down to 1 to 4 per day. This lasts until 2 months of age.
- The stools are yellow in color and thick like peanut butter. Green stools are also normal (usually caused by bile).
- After 2 months of age, most babies pass 1 or 2 stools per day. They can also pass 1 every other day. They are soft and solid.
- Breast Discomfort in Bottle-feeding Mothers:
- Even though you chose not to breastfeed, your breasts will make milk. Breast milk comes in on day 2 or 3. Swollen breasts can be painful for a few days. Here is what to do:
- Ibuprofen. Take 400 mg of ibuprofen (such as Advil) 3 times per day. This will help to lessen pain and swelling. There's no special prescription medicine for this.

- Cold Pack. Use a cold pack or ice bag wrapped in a wet cloth. Put it on your breasts for 20 minutes. Do this as often as needed. This will decrease milk production. Do not use heat. Heat will increase milk production.
- Pumping. For moderate pain, hand express or pump off a little breast milk. This will help to reduce your pain. Pumping breast milk can increase milk production. But, doing this to take the edge off your discomfort is not harmful.
- Bra. Wear a bra that offers good breast support or a sports bra. Wear it 24 hours a day.
- Binding. Binding the breasts by wearing a tight bra is no longer advised. Binding by using an elastic wrap is also not advised. Binding can increase the risk of breast infections (mastitis).
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 03/28/2023
Last Revised: 12/30/2022
Copyright 2000-2023. Schmitt Pediatric Guidelines LLC.
Stopping the Bottle (for Parents)
en español: Dejar el biberón
Reviewed by: Madhu Desiraju, MD
Primary Care Pediatrics at Nemours Children's Health
Many toddlers become attached to their bottles. Besides providing nourishment, bottles also mean comfort and security.
It's important for parents to start weaning babies from bottles around the end of the first year and start getting them comfortable drinking from cups. The longer parents wait to start the transition, the more attached kids become to their bottles and the harder it can be to break the bottle habit. Longer bottle use may lead to cavities or cause a child to drink more milk than they need.
Switching from bottle to cup can be challenging, but these tips can make the change easier for parents and kids.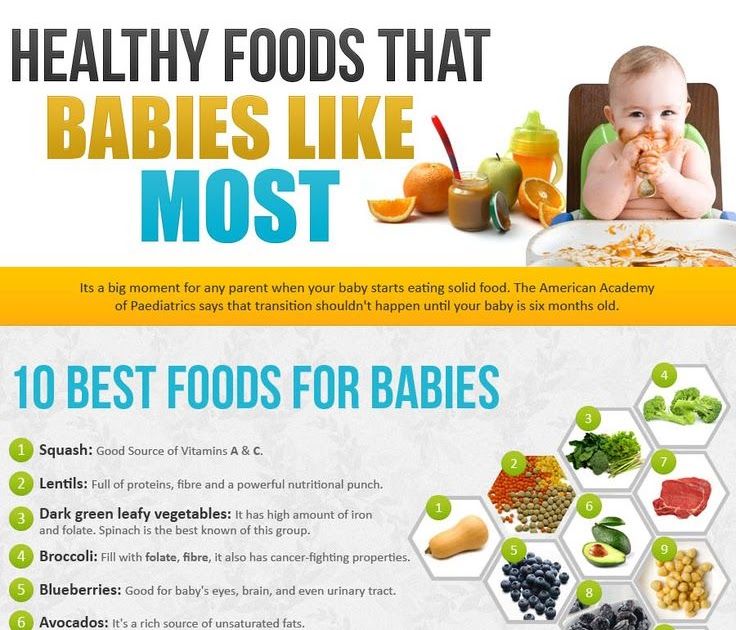
How Should I Start the Switch?
Most doctors recommend introducing a cup around the time a baby is 6 months old. In the beginning, much of what you serve in a cup will end up on the floor or on your baby. But by 12 months of age, most babies have the coordination and hand skills needed to hold a cup and drink from it.
Age 1 is also when doctors recommend switching from formula to cow's milk. It can be a natural change to offer milk in a cup rather than a bottle.
If you're still breastfeeding, you can continue feeding your baby breast milk, but you may want to offer it in a cup.
Tips to Try
Instead of cutting out bottles all at once, try dropping them from the feeding schedule over time.
For example, if your baby usually drinks 3 bottles each day, begin by stopping the morning bottle. Instead of giving a bottle right away, bring your baby to the table and after the feeding has started, offer milk from a cup. You might encourage your baby by saying something like "You're getting so big now and can use a cup like mommy. "
"
As you try to stop the morning bottle, keep offering the afternoon and evening bottles for about a week. That way, if your child asks for the bottle you can say that one is coming later.
The next week, stop another bottle feeding and provide milk in a cup instead. Try to do this when your baby is sitting at the table in a high chair.
Generally, the last bottle to stop should be the nighttime bottle. That bottle tends to be a part of the bedtime routine and is the one that most provides comfort to babies. Instead of the bottle, try offering a cup of milk with your child's dinner and continue with the rest of your nighttime tasks, like a bath, bedtime story, or teeth brushing.
Other tips to keep in mind:
- Spill-proof cups that have spouts designed just for babies ("sippy cups") can help ease the move from the bottle. Dentists recommend sippy cups with a hard spout or a straw, rather than ones with soft spouts.
- When your child does use the cup, offer plenty of praise.
 If grandma is around, for example, you might say, "See, Emma is such a big girl she drinks milk in a cup!"
If grandma is around, for example, you might say, "See, Emma is such a big girl she drinks milk in a cup!" - If you keep getting asked for a bottle, find out what your child really needs or wants and offer that instead. If your baby is thirsty or hungry, provide nourishment in a cup or on a plate. If it's comfort, offer hugs, and if your little one is bored, sit down and play!
- As you wean your baby from the bottle, try mixing the milk in the bottle with water. For the first few days, fill half of it with water and half of it with milk. Then slowly add more water until the entire bottle is water. By that time, it's likely that your child will lose interest and be asking for the yummy milk that comes in a cup!
- Get rid of the bottles or put them out of sight.
If you have problems or concerns about stopping the bottle, talk with your child's doctor.
Reviewed by: Madhu Desiraju, MD
Date reviewed: June 2022
Share:
/content/kidshealth/misc/medicalcodes/parents/articles/no-bottles
Feeding with expressed milk | breastfeeding
When can I start breastfeeding my baby with expressed breast milk? How to do it right? Is it worth worrying that the child will confuse the pacifier with the breast? In this article we will answer your questions.
Share this information
When can I start breastfeeding my baby?
If your baby is healthy and breastfeeding well, there is no need to give him expressed milk. For the first four weeks, you work together to start and increase milk production, and your baby also learns to suckle properly at the breast. There is not enough scientific data on this yet, 1 but there is an opinion that bottle feeding in the first month may adversely affect the process of establishing breastfeeding.
However, if the newborn is unable to latch on or suckle for some reason, start expressing milk as soon as possible after delivery. Read more about this in our articles on coping with problems in the first week, breastfeeding premature babies and babies with special needs, and seeking help from your healthcare provider.
How can I feed my baby with expressed breast milk?
There are many expert feeding solutions that allow you to give your baby expressed milk in a variety of ways, depending on your and your baby's needs.
For example, the innovative Calma smart pacifier only lets milk through when the baby creates a vacuum by suckling. This means that when feeding from a bottle, he will make the same movements with his tongue and jaws as when sucking at the breast. 2.3 Calma was developed with the help of breastfeeding experts from the University of Western Australia. When using this pacifier, the baby can suck, swallow, pause and breathe in the same way as when breastfeeding. 4 Preserving natural sucking habits allows baby to transition easily from breast to bottle and back.
In addition, Medela also offers regular bottle teats* in two versions that produce milk at different rates. All Medela* nipples can be placed directly on bottles used for expressing milk, minimizing the risk of spillage.
If you need to feed your baby with expressed milk, but you do not want to bottle feed him until he is learning to breastfeed, you can use a sippy cup* for temporary feeding. The baby will be able to drink milk from such a mug, but you should be careful not to spill the milk. For the first time, it is advisable to feed the child from a drinking cup under the supervision of the attending physician in order to learn how to do it correctly.
The baby will be able to drink milk from such a mug, but you should be careful not to spill the milk. For the first time, it is advisable to feed the child from a drinking cup under the supervision of the attending physician in order to learn how to do it correctly.
If your baby needs to be supplemented with expressed milk in addition to regular breastfeeding, the Supplementary Feeding System (SNS)* can be used. It is equipped with a thin, flexible capillary that can be clipped close to the nipple to give your baby expressed milk while breastfeeding. Thanks to this, the baby suckles the breast for longer, thereby developing sucking skills and stimulating the production of milk from the mother. This can be helpful when there is a shortage of breast milk, as well as when feeding adopted or surrogate children.
If the baby is unable to breastfeed because he is too weak or has a congenital disease, you can use the Special Needs Cup*, which releases milk with gentle pressure, making it suitable for feeding these babies.
How to teach a child to bottle feed?
If breastfeeding is going well and you decide to start bottle feeding your baby with expressed breast milk, follow these guidelines.
Start early and take your time
Don't wait until the first day of work or the first time you leave the house to start bottle feeding your baby. Start accustoming your baby to small portions of expressed milk a couple of weeks before the desired date, calmly and without haste. Gradually build up to one full serving of pumped milk from a bottle.
Choose a time
Ideally, at the first bottle feeding, the baby should be hungry, but not too hungry - in this state, he is as relaxed as possible.
Let others feed
Your baby is used to feeding from your breast, so when you offer him a bottle it can be confusing. The process can go faster if the first time the baby is bottle-fed by someone else while you are not in the room, so that your sight and smell do not embarrass the baby.
Maintain optimal temperature
Your baby will be more willing to eat expressed milk if the temperature is around 37°C, close to body temperature.
Dip the nipple in milk
Try dipping the nipple in expressed milk before offering it to your baby. This way it will taste and smell like your breast milk. Lightly touch the baby's upper lip with the nipple to open the mouth.
Choose the right position for bottle feeding
Feed your baby on demand and keep him reclining during feeding. Never bottle feed your baby when he is lying or sitting, otherwise he may choke. Listen to the wishes of the child - take as many pauses as he needs. You can even try to shift it from one hand to another during feeding.
Be patient
Don't worry if your baby doesn't take the bottle right away - it may take several tries. If he pushes the bottle away or starts crying, calm him down, wait a few minutes and try again. If he still doesn't want to bottle feed, wait a few more minutes and breastfeed him as usual. Repeat the bottle experiment at a different time of day.
If he still doesn't want to bottle feed, wait a few more minutes and breastfeed him as usual. Repeat the bottle experiment at a different time of day.
How much pumped milk should I give my baby?
All children are different. Research shows that between the ages of one and six months, a baby can consume between 50 and 230 ml of milk per feeding. To start, prepare about 60 ml and observe how much your baby needs - more or less. You will soon realize how much milk he usually eats. Just never force him to finish the cooked portion.
How can I keep my baby safe when bottle feeding?
Always clean and sterilize your pump and bottles according to the manufacturer's instructions. Wash your hands before expressing, pouring milk, and feeding your baby. Follow our instructions for safely storing and thawing your expressed milk.
If breastmilk needs to be warmed, place the bottle or bag in a bowl of warm water or a heater or under running water at a maximum of 37°C. Never heat breast milk in the microwave or on the stove.
Never heat breast milk in the microwave or on the stove.
Will the baby be able to transition from breast to bottle?
Some mothers worry that if they start bottle feeding too early, the baby will get used to the artificial nipple and not want to breastfeed. Others, on the contrary, are worried that if the child is not immediately accustomed to the bottle, then he will no longer eat from it. In general, in these cases, they say that the child confuses the nipple with the breast.
Experts disagree on whether such confusion is a problem. 1 Without a doubt, it is easier for a baby to suckle milk from a regular bottle with a nipple, which does not require a vacuum, than from the breast, since the milk flows faster, also under the influence of gravity. And some babies really have clear preferences: only the breast or only the nipple. However, many babies are comfortable suckling both the breast and the pacifier.
If you are unable to feed your baby with expressed breast milk, seek help from a lactation consultant or specialist.
Literature
1 Zimmerman E, Thompson K. Clarifying nipple confusion. J. Perinatol. 2015;35(11):895-899. - Zimmerman I., Thompson K., "On the issue of breastfeeding." Zh Perinatol (Journal of Perinatology). 2015;35(11):895-899.
2 Geddes DT et al. Tongue movement and intra-oral vacuum of term infants during breastfeeding and feeding from an experimental teat that released milk under vacuum only. Early Hum Dev . 2012;88(6):443-449. - Geddes D.T. et al., "Language Movements and Oral Vacuum Generation in Term Infants During Breastfeeding and Feeding from an Experimental Vacuum-Delivery Teat". Airlie Hume Dev. 2012;88(6):443-449.
3 Segami Y et al. Perioral movements and sucking pattern during bottle feeding with a novel, experimental teat are similar to breastfeeding. J. Perinatol. 2013;33(4):319-323. - Segami I. et al.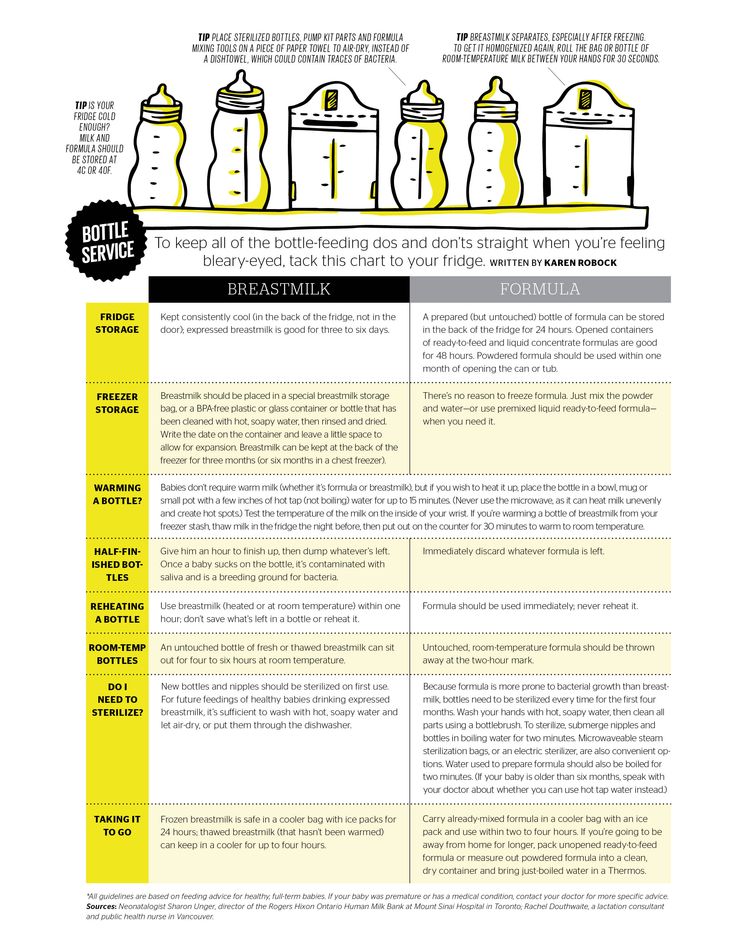 , "Perioral movements and sucking during bottle feeding with a new experimental nipple are very similar to sucking from the breast." Zh Perinatol (Journal of Perinatology). 2013;33(4):319-323.
, "Perioral movements and sucking during bottle feeding with a new experimental nipple are very similar to sucking from the breast." Zh Perinatol (Journal of Perinatology). 2013;33(4):319-323.
4 Sakalidis VS et al. Oxygen saturation and suck-swallow-breathe coordination of term infants during breastfeeding and feeding from a teat releasing milk only with vacuum. Int J Pediatr. 2012;2012:130769. - Sakalidis V.S. et al., "Oxygenation and Coordination of Sucking, Swallowing, and Breathing in the Term Infant During Breastfeeding and Feeding from a Purely Vacuum Teat". Int J Pediatrician 2012;2012:130769.
Read instructions before use. Consult a specialist about possible contraindications.
* RC № ФСЗ 2010/07353 dated 07/19/2010
Bottle for newborns | Nutrilak
Turganova Elena
Published: 03/09/2023
Reading time: 5 minutes
591
Breast milk is natural and therefore the most suitable food for an infant. Breastfeeding does not require any special equipment. But if for some reason it is not possible, the newborn feeding bottle becomes the No. 1 accessory and you will have to choose it carefully and meticulously. Here are some tips to make this choice easier.
Breastfeeding does not require any special equipment. But if for some reason it is not possible, the newborn feeding bottle becomes the No. 1 accessory and you will have to choose it carefully and meticulously. Here are some tips to make this choice easier.
Baby bottles. Which is better to choose?
Don't buy a bottle before going to the hospital unless you have a health problem that makes breastfeeding unavailable. Even if at first not everything works out with breastfeeding and you need to give the newborn expressed milk or formula, you can use a pipette or a teaspoon. Pediatricians generally do not recommend the first month of a baby's life, while breastfeeding is being established, to use nipples and pacifiers so that the child does not prefer them to the still undeveloped breast, from which milk is extracted with effort.
Start choosing feeding aids only when you have made a clear decision to switch to artificial feeding. It is good if there is an opportunity to choose a bottle directly at the pharmacy: you hold it in your hands, make sure that everything is intact, the packaging and completeness are not violated. But if the presented assortment does not suit you, you can order everything you need in the online store. At the same time, carefully read the reviews and do not hesitate to ask questions about the product to the seller. So the likelihood of an unsuccessful online purchase will decrease.
But if the presented assortment does not suit you, you can order everything you need in the online store. At the same time, carefully read the reviews and do not hesitate to ask questions about the product to the seller. So the likelihood of an unsuccessful online purchase will decrease.
When choosing a feeding bottle, consider the following criteria:
-
The material the bottle is made from. It can be glass or plastic. Glass is more hygienic. It is easier to wash and sterilize. It does not stain from drinks, does not deteriorate from time to time. The main disadvantage of glass is brittleness. The glass bottle is easy to break. In addition, it is quite heavy. Plastic is lightweight, bottles made of it are distinguished by a wide variety of shapes and sizes. However, not all types of plastic tolerate heat well. These bottles may have microwave and dishwasher restrictions. Also, scratches, cracks quickly appear on the plastic, it becomes cloudy, stained and needs to be replaced rather quickly.

-
Type of teat. The nipple is perhaps even more important than the bottle itself. It is the nipple that enters the baby's mouth and is responsible for the success of feeding. Nipples can be silicone or latex, classically round or anatomically shaped, with a wide or narrow opening for feeding. In accordance with modern recommendations, you should choose nipples that are closest to the anatomical version, but it is not a fact that the child will appreciate your choice. It can only be verified experimentally.
-
Easy to use and maintain. Immediately check whether the bottle can be boiled, sterilized in a microwave oven, washed in a dishwasher. Pay attention to whether the neck is wide enough to make the product easy to wash. Evaluate the design itself: is it convenient to assemble and disassemble it.
-
Anti-colic system. Modern feeding bottles have various devices to prevent air swallowing, which can increase discomfort in the tummy.
 This may be a special inclination of the neck, a valve system, and so on. There is no guarantee that with such a bottle the baby's well-being will improve significantly, but if there is a problem, you can try this method.
This may be a special inclination of the neck, a valve system, and so on. There is no guarantee that with such a bottle the baby's well-being will improve significantly, but if there is a problem, you can try this method. -
Replaceable teat. You can buy an expensive, beautiful bottle in every respect, but after a while you will find that it is almost impossible to find a replacement nipple for this model. Check this point before buying.
-
Age marking. For newborns, smaller bottles are made; for older babies, feeding utensils can be equipped with handles so that the child independently holds it while eating. Look for the age designation on the packaging: 0+, 6+, 12+, or other markings indicating age.
And, of course, choose trusted manufacturers, buy baby utensils in a pharmacy or a specialized store, do not use a bottle if you are confused by its appearance, smell, if it has visible defects.
How to bottle feed your newborn
Having decided on how to choose your formula feeding accessories, let's look at how to properly bottle feed your newborn.
The bottle and teat must be sterilized before the first use. The mixture is diluted immediately before feeding. Be sure to wash your hands with soap and water before preparing baby food.
To dilute the mixture correctly, carefully read the instructions on the package. Keep the proportions right so the mixture doesn't get too thick or runny, both of which will harm your digestion.
Before giving the bottle to your baby, check the temperature of the finished formula by putting a couple of drops on the back of the brush.
Sit in a comfortable position for breastfeeding so that both your back and the arm you will hold your baby on are securely supported. The position of the baby when feeding from a bottle is exactly the same as when breastfeeding. Position it so that the baby's head is in the crook of your arm and above his belly. Make sure that the baby does not throw his head back and does not turn it to the side. Bring the bottle to the baby's mouth, lightly touch the nipple to the lips. The child should reflexively open his mouth and begin to suck. Hold the bottle at a slight angle, gradually changing its angle so that the nipple is always completely filled with formula and no air enters it.
After feeding, clean the bottle and teat with special baby dishwashing liquid and sterilize them.
How to sterilize baby bottles
Sterilize baby bottles after every feeding. For babies aged 1-3 months at least 1-2 times a day, up to six months - at least every other day. A warm, humid environment is ideal for the reproduction of pathogenic bacteria, therefore, it is impossible to neglect the regular sterilization of children's feeding utensils, as well as pacifiers, drinkers, and nibblers.
Sterilize by boiling, microwave oven or special sterilizer. If the child is switched to formula in the first months of life, it makes sense to purchase a sterilizer, because you will have to use it a lot and often. Another plus of such an acquisition is that the bottle can be used immediately after sterilization. You will get it from the device disinfected and dry.
If you need to sterilize dishes from time to time, you can do without a sterilizer. Processing dishes in the microwave or on the stove will take a little more time and effort.
Boiling sterilization is an old and proven method. Allocate a separate pan for these purposes and do not use it for cooking. Take a little more than half the capacity of water, dip the bottles and nipples in cold water, turn on the fire. Check from time to time that nothing sticks to the bottom and melts. From the moment of boiling, note an average of 5 minutes. Use silicone tongs [TE1] to remove items from the water and place them on a clean ironed towel to dry. Paper is not suitable for this, since soaked particles can stick to the dishes, and besides, paper cannot be heat-treated, unlike fabric.
Sterilize in the microwave in the same way. A glass bowl is filled with water, a bottle and a nipple are placed in it, put in a microwave oven for 6-8 minutes at maximum power. You can purchase special disposable or reusable sterilization bags or a microwave sterilizer and use them according to the manufacturer's instructions.
Most importantly, before starting sterilization, make sure that the material of the bottle and nipple allows this method of processing.
Conclusions
-
Feeding bottles should be selected based on the convenience and safety of their use.
-
Bottle feed your newborn in the same position as when breastfeeding. Hold the bottle at an angle to prevent air from entering the nipple.
-
Bottles can be sterilized by boiling, in a microwave oven or in a special sterilizer.
Article author
Turganova Elena
Pediatrician
About the author
Share on Vkontakte Share on Odnoklassniki
Contents of the article
- Baby bottles.