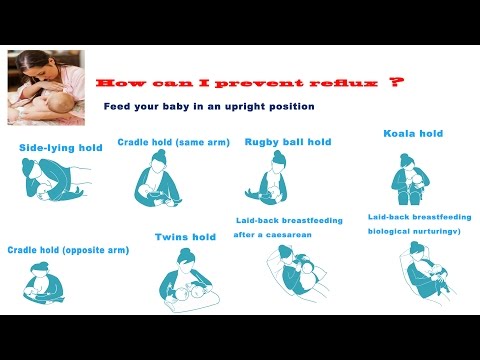
Feeding positions for babies with reflux
Reflux - La Leche League International
A baby spitting up occasionally is usually looked at as “something babies do.” According to the late Dr. Gregory White, husband of the late LLL Founder, Mary White, “In a healthy baby, spitting up is a laundry problem, not a medical problem.”
A baby may spit up for lots of reasons:
- Baby is not be able to swallow quickly enough when milk ejects forcefully during a feeding, resulting in swallowing excess air.
- Mother has an oversupply of milk that can result in baby taking too much too fast for the stomach to handle. Either can result in additional air swallowed with the large volumes of milk. Read our post on oversupply.
- Less common reasons are:
- Immature muscle control
- Allergy to foods and/or dietary supplements mother may consume
- Disease
If the spitting up is frequent and obviously uncomfortable for baby, it may be that your baby is experiencing gastroesophogeal reflux disease, or GERD.
- GERD occurs when the band of voluntary muscle fibers within the esophagus where it enters the stomach fails to keep the stomach contents in the stomach.
- Milk or food, along with acid from the stomach, backs up into the lower esophagus and irritates the tissues there.
- Adults recognize this feeling as heartburn. Read our post on GERD.
If your baby is overall a pleasant and healthy baby with good output and normal growth patterns, be assured that he will likely outgrow this stage by 6-12 months. In the meantime, here are some general tips to keeping spit up episodes to a minimum:
- Use positions for feeding that keep baby’s head higher than her tummy, such as a laid-back position or having baby diagonally across your chest in a cradle hold. Avoid positions that have baby bending at the waist, putting more pressure on her tummy. See Positioning.
- Keep baby upright for 15-20 minutes or so after feedings to allow for digestion to begin.
 This is a nice time to just lean back with baby on your chest to soothe, talk, sing, or hum to him or to just snuggle.
This is a nice time to just lean back with baby on your chest to soothe, talk, sing, or hum to him or to just snuggle. - Burp gently between sides and at the end of the feeding.
- Try shorter, frequent feedings, if baby is agreeable, to reduce the load in her tummy.
- Try nursing at one breast only each feeding to avoid two strong milk ejections and, therefore, reducing overfeeding and excess swallowing of air.
Occasionally, some older babies will start to spit up when they hadn’t typically been spitting up. If your baby doesn’t seem ill, other reasons might include:
- Something new to his diet – solids, adding or changing vitamins for you or baby, medications for either of you.
- Growth spurt – when babies start feeding more frequently with a growth spurt, they can be bringing in larger volumes of milk and/or more air.
- Teething – the discomfort of the gums may cause baby to be less efficient with her sucking and take in more air.
 Teething can also result in increased saliva production and swallowing, adding to the volume of fluid and air in her tummy. See Teething.
Teething can also result in increased saliva production and swallowing, adding to the volume of fluid and air in her tummy. See Teething.
Best feeding positions for babies with reflux gas, colic and fuss
Skip to content
ByStaff Mom
Upright feeding position for babies with Reflux is one of the best-kept secrets to a happy, comfortable baby. According to healthline, “A horizontal position makes it easier for the stomach contents to reflux into the esophagus”. The undeveloped digestive system is the reason why all babies are prone to experience acid reflux symptoms. Furthermore, a pilot clinical study concluded that babies showed an average of 52% reduction of gas, colic and acid reflux symptoms after feeding in an upright position with an air-free device.*
Read 3 Steps for Treating Infant Reflux
Here are 4 of the best upright feeding positions for babies with reflux. Try them out and see the results. Your baby should sleep peacefully and hopefully you will, too. Happy baby, happy mommy! Right?
Try them out and see the results. Your baby should sleep peacefully and hopefully you will, too. Happy baby, happy mommy! Right?
*122 infants in the study were fed with Bare Air-free feeding system, a device that dispenses air-free milk, while in an upright position and lets the babies control the flow and pace.
4 Best Upright Feeding Positions for Babies with Reflux
Feeding positions for babies with reflux:
- Australian Hold
This is one of the most comfortable feeding positions if you are sore from a C-section:
a. Sit down on the bed or sofa;
b. Sit the baby on your lap, facing you, with his/her torso upright;
c. Hold the back of the baby’s head with your palm fully opened;
e. If you are breastfeeding, bring the baby to the breast and let him/her begin suction to feed;
f. If you are Bare-feeding, hold Bare® right side up (nipple on top, base at the bottom) and offer it to the baby in that same position. Let the baby begin suction to feed.
Let the baby begin suction to feed. - Knees up:
Best bonding position as you can face and make eye-level contact with your little one at all times while feeding:
a. Sit comfortably in your bed, lay back, and put your knees up on the bed;
b. Sit your baby on your belly and let her rest her back on your legs;
c. Hold Bare right side up and offer it to the baby. You don’t need to turn Bare® upside down to feed. - Cradle Hold:
This a great picture-perfect position!
a. Sit down on a couch and support your back;
b. Sit your baby on your lap with her back resting on your forearm, then keep the baby as upright as you can;
c. Offer Bare® to the baby while holding it right side up. - Sit Up:
This is when your baby faces you, as in a cooing conversation.
a. Wrap your fingers and thumb around the lower side of the baby’s head;
b.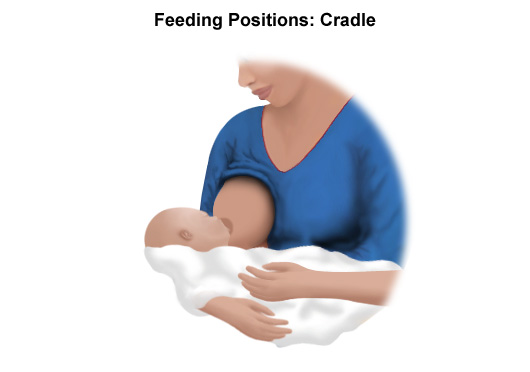 Or sit and strap your baby in a high chair. Be sure to adjust the belt to fit snugly;
Or sit and strap your baby in a high chair. Be sure to adjust the belt to fit snugly;
c. Offer your baby a Bare® Air-free feeding system right side up and let her begin suction to feed.
- Sale! $20.99Add to cartContinueLoadingDone
- $39.99Add to cartContinueLoadingDone
- $39.99Add to cartContinueLoadingDone
Information presented on this website does not replace physician in-person evaluation and treatment. These products have not been evaluated by the Food and Drug Administration.
Various breastfeeding positions
Try different breastfeeding positions to find the one that works best for you and your baby. You can see the options in our selection of photos
Share this information
There is no right or wrong way to hold the baby while
feeding, and mom and baby are sure to find their favorite position.
It is important that both you and your child feel comfortable. 1.2 It's good to learn a few different breastfeeding positions and techniques because life's circumstances often require us to be flexible, especially as your baby gets older and you start to leave the house more often.
Whatever position you choose to breastfeed your baby, remember a few simple rules.
- Prepare everything you need before feeding, including drinks, food, mobile phone, TV remote control, book or magazine. And do not forget to go to the toilet - the feeding process can take a long time!
- Make sure your baby is comfortable. Whichever position you choose, it's important to keep your baby strong, level, and provide good support for their head, neck, and spine.
- You should also be comfortable. Don't stress. If necessary, use pillows of different sizes or rolls of towels to support your back or arms.
- Make sure your baby is latching on correctly.
 Proper grip is the key to comfort when breastfeeding.
Proper grip is the key to comfort when breastfeeding. - If your baby does not latch on well or you experience pain while feeding, contact a lactation consultant for help. The specialist will also be able to show you how to hold your baby more comfortably.
1. Relaxed feeding or reclining position
The relaxed feeding position, also known as biological feeding, 1 is often the first position for most mothers. If, immediately after birth, the baby is placed on the mother’s chest or stomach, normally, he instinctively reaches for the breast and tries to grab the nipple. This phenomenon is known as the breast seeking reflex. Skin-to-skin contact stimulates the infant's feeding instinct, and gravity helps him to latch onto the breast and maintain balance.
But it's not just newborns that can be fed in the reclining position - this position is great for babies of all ages. It can be especially helpful if your baby does not latch well in other positions or does not like to be touched during feeding, and also if you have too much milk flow or too large breasts. Isabelle, a mother from the UK, shares her experience: “I had large breasts, and the baby was born small - 2.7 kg, so it was not easy to find a comfortable position at first. After a few weeks, it became clear that there was no “correct” posture for me. As a result, I most often fed lying down, putting the baby on my chest. ”
Isabelle, a mother from the UK, shares her experience: “I had large breasts, and the baby was born small - 2.7 kg, so it was not easy to find a comfortable position at first. After a few weeks, it became clear that there was no “correct” posture for me. As a result, I most often fed lying down, putting the baby on my chest. ”
It is more convenient to feed not lying flat on your back, but half-sitting, leaning on pillows. So you will have a back support and you will be able to watch the baby during feeding.
2. Cradle position
This is the classic
first thought of breastfeeding. Mom sits straight
, and the baby lies on her side on her arm, pressing his stomach against her stomach. 3 Although this is a very popular position, it is not always easy to master with newborns because it gives the baby less support. Try putting a pillow under your back, and put a special breastfeeding pillow on your knees and lean on it with your hands. So you can more reliably support the child, without overstraining your back and shoulders. Just make sure that the baby does not lie too high on the pillow for feeding. The breast should remain at a natural level so that the baby can grab it without effort, otherwise sore nipples cannot be avoided.
Just make sure that the baby does not lie too high on the pillow for feeding. The breast should remain at a natural level so that the baby can grab it without effort, otherwise sore nipples cannot be avoided.
“I breastfed in the cradle position because it suited me perfectly! It was comfortable and I loved just sitting and looking at my little one,” recalls Rachel, a mother of two from Italy.
3. Cross Cradle
This breastfeeding position looks almost the same as Cradle, but the baby is on the other arm. 3 This gives your baby support around the neck and shoulders so he can tilt his head to latch on. This position is great for breastfeeding newborns and small babies, as well as for babies who do not latch well. Since the baby lies completely on the other hand, it becomes easier to control his position and you can adjust the chest with your free hand.
Julie, a UK mother of two, finds this position very practical: “I usually breastfeed my youngest in the cross cradle position. So I have a free second hand, and I can take care of an older baby at the same time. ”
So I have a free second hand, and I can take care of an older baby at the same time. ”
Do not hold the baby's head at first, otherwise you may inadvertently press his chin against his chest. Because of this, the child will not be able to take the breast deeply, because the nipple will rest against the base of the tongue, and not against the palate, which will lead to inflammation of the nipples. As the child grows, this position becomes more comfortable, and he can rest his head on your palm (as shown in the photo above).
4. Underarm breastfeeding
In this position, also known as the “ball grip”, the mother sits with the baby lying along her arm at the side, legs towards the back of the chair (or any other seat). 3 Another comfortable position for newborn breastfeeding, you can give your baby good support, full control of his position and a good view of his face. And the baby feels safe in close contact with the mother's body. This position is especially good for those who have had a caesarean section or a premature birth, as well as mothers of twins and women with large breasts.
“When I breastfed my first daughter, I had very large K-sized breasts—twice the size of her head,” recalls Amy, an Australian mother of two. - I put rolls of towels under each breast, because they were very heavy, and fed my daughter in a pose from under the arm, but only sitting straighter so as not to crush her. This position was also convenient because I had a caesarean section and could not put the baby on my stomach.”
5. Side-lying position
The side-lying position is ideal for a relaxed
nighttime feeding in bed or on the couch. If you had a
caesarean section or ruptures during childbirth, this position may be more comfortable than sitting down. 3 In this position, mother and baby lie side by side, tummy to tummy.
“It was difficult for me to sit during endless night feedings, firstly because of the caesarean section, and secondly because of lack of sleep,” recalls Francesca, a mother from the UK. “And then I discovered that you can feed your baby lying on your side and rest at the same time. ”
”
“Because of the short tongue frenulum, Maisie could only properly latch on to her breasts while lying on her side. The lactation consultant showed me how it's done. In this position, the flow of milk was optimal for my daughter, and it was easier for her to keep the nipple in her mouth. As she got older, she became much better at grabbing her breasts in normal positions,” says Sarah, mother of two from Australia.
6. Relaxed breastfeeding after caesarean section
If you can't find a comfortable position for breastfeeding after caesarean section, 3 try holding the baby on your shoulder in a reclining position – this does not stress the postoperative suture and allows you to breastfeed your baby comfortably. You can also try side feeding.
7. Sitting upright breastfeeding or “koala pose”
When breastfeeding in an upright position or “koala pose”, the baby sits with a straight back and a raised head on the mother's hip. 4 This position can be tried even with a newborn if it is well supported, but it is especially convenient for feeding a grown child who can already sit up by himself. The upright sitting position, or “koala pose,” is great for toddlers who suffer from reflux or ear infections and feel better sitting. In addition, this pose may be suitable for children with a shortened frenulum of the tongue or reduced muscle tone.
The upright sitting position, or “koala pose,” is great for toddlers who suffer from reflux or ear infections and feel better sitting. In addition, this pose may be suitable for children with a shortened frenulum of the tongue or reduced muscle tone.
“When my daughter got a little older, I would often feed her in an upright position, which was more comfortable for both of us, and I could still hold her close,” recalls Peggy, a mother from Switzerland. “Besides, it was possible to discreetly breastfeed her in public places.”
8. Overhanging position
In this position, the baby lies on his back, and the mother bends over him
on all fours so that the nipple falls directly into his mouth. 4 Some moms say this breastfeeding position is good to use occasionally for mastitis, when touching the breasts is especially unpleasant. Some say that this breastfeeding position helps with blockage of the milk ducts, although there is no scientific evidence for this yet. You can also feed in the “overhanging” position while sitting, kneeling over the baby on a bed or sofa, as well as reclining on your stomach with support on your elbows. Pillows of various sizes that you can lean on will help you avoid back and shoulder strain.
You can also feed in the “overhanging” position while sitting, kneeling over the baby on a bed or sofa, as well as reclining on your stomach with support on your elbows. Pillows of various sizes that you can lean on will help you avoid back and shoulder strain.
“I have breastfed several times in the 'overhang' position for clogged milk ducts when no other means of dissolving the blockage worked. And this pose seems to have helped. I think it's because of gravity, and also because the breasts were at a completely different angle than with normal feeding, and my daughter sucked her differently, ”says Ellie, a mother of two from the UK.
Feeding in the "overhanging" position is unlikely to be practiced regularly, but in some cases this position may be useful.
“I used to breastfeed in the overhang position when my baby was having trouble latch-on,” says Lorna, mother of two in the UK. - This, of course, is not the most convenient way, but then I was ready for anything, if only he could capture the chest. We succeeded and have been breastfeeding for eight months now!”
We succeeded and have been breastfeeding for eight months now!”
9. Breastfeeding in a sling or in a sling
Breastfeeding in a sling takes some practice, but it can be used to go out, look after older children, or even do a little household chores.
The sling is also useful if the baby does not like to lie down or is often attached to the breast. Lindsey, a mother of two in the US, notes: “I used the carrier frequently for both of my children. When we were out, I tied the sarong around my neck and covered the carrier with it. Under such a cape, the baby can eat as much as he wants until he falls asleep.
This breastfeeding position is best when the baby is already good at breastfeeding and can hold his head up by himself. Any slings are suitable for breastfeeding, including elastic and rings, as well as carrying bags. Whatever option you choose, the main thing is that you can always see the face of the child, and his chin does not rest against his chest.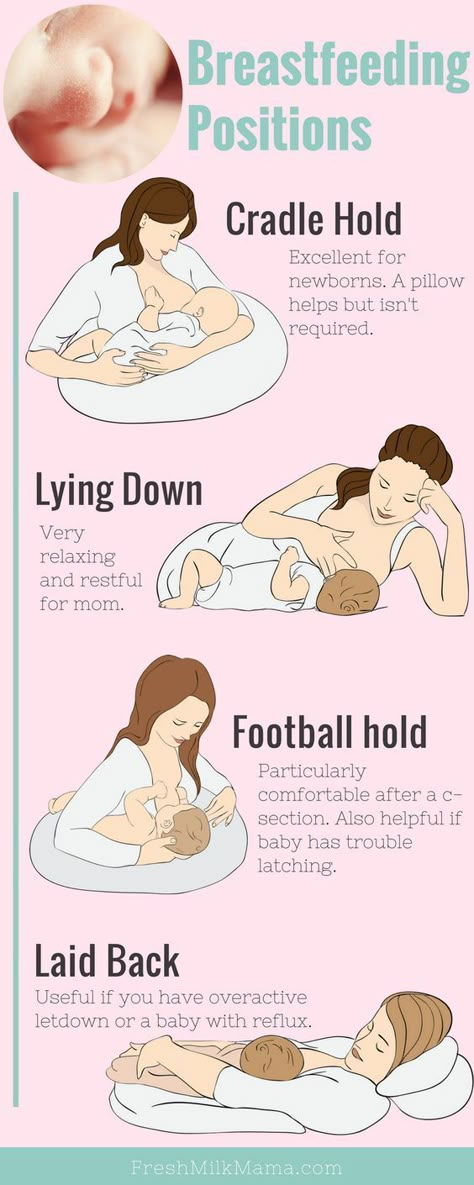
10. Double hand-held breastfeeding
Double hand-held breastfeeding (or “double-ball grab”) is great for mothers of twins—you can breastfeed both at the same time and keep your arms relatively free. 4 When feeding in this position, it is advisable to use a special pillow for breastfeeding twins, especially at first. It will provide extra support and help keep both babies in the correct position, as well as reduce the burden on the abdomen if you had a caesarean section. In addition, the hands are freer, and if necessary, you can deal with one child without interfering with the second.
“My twins were born very tiny and had to be fed every two hours at any time of the day or night. Very soon it became clear: if I want to do anything besides feeding, I need to feed them both at the same time, - says Emma, mother of two children from the UK. “I breastfed them two by hand using a breastfeeding pillow.”
Other good positions for breastfeeding twins are two criss-cross cradles, one baby in the cradle and the other close at hand, reclining feeding, or sitting upright (one baby on one side, the other on the other).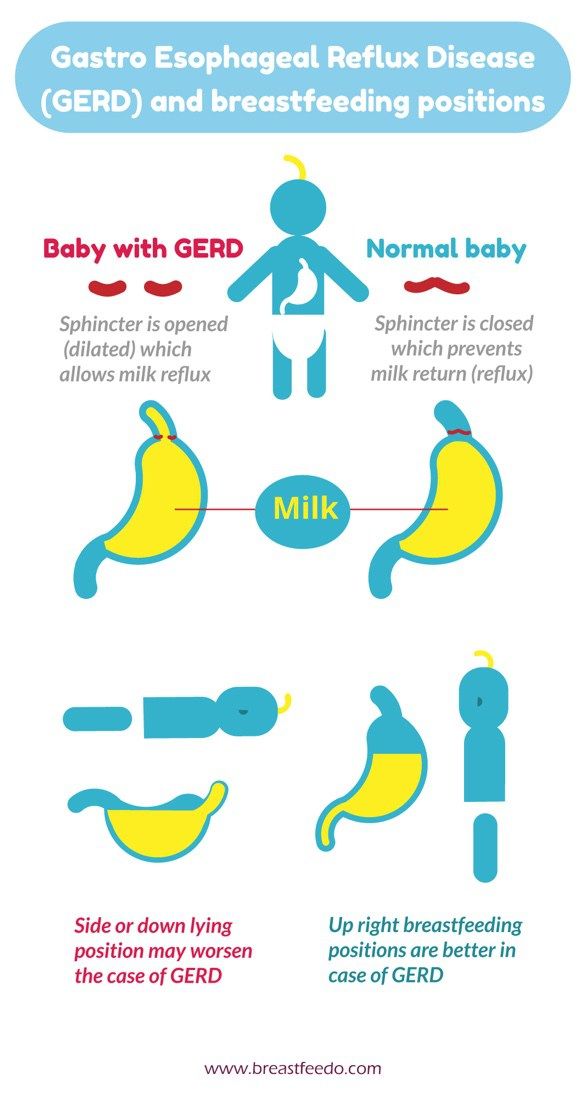
11. Breastfeeding in the "hand-supported" or "dancer's hand" position
muscle tone (which is typical for premature babies, children suffering from various diseases or Down syndrome), try supporting his head and your chest at the same time. 4 Grasp your chest with your palm underneath so that your thumb is on one side and all the others are on the other. Move your hand slightly forward so that your thumb and forefinger form a "U" just in front of your chest. With the other three fingers, continue to support the chest. With your thumb and forefinger, hold the baby's head while feeding so that his chin rests on the part of the palm between them, your thumb gently holds the baby on one cheek, and your index finger on the other. So the baby gets excellent support, and you can control his position and see if he is holding his breast.
Literature
1 Colson SD et al. Optimal positions for the release of primitive neonatal reflexes stimulating breastfeeding. Early Hum Dev . 2008;84(7):441-449. - Colson S.D. et al., "Optimal Positions for Provoking Primitive Innate Reflexes to Induce Breastfeeding." Early Hume Dev. 2008;84(7):441-449.
Early Hum Dev . 2008;84(7):441-449. - Colson S.D. et al., "Optimal Positions for Provoking Primitive Innate Reflexes to Induce Breastfeeding." Early Hume Dev. 2008;84(7):441-449.
2 UNICEF UK BFHI [ Internet ]. Off to the best start ; 2015 [ cited 2018 Feb ]. - UNICEF UK, Baby-Friendly Hospital Initiative, Start the Best You Can [Internet]. 2015 [cited February 2018].
3 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women's Health. 2007;52(6):638-642. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
4 Wambach K, Riordan J, editors.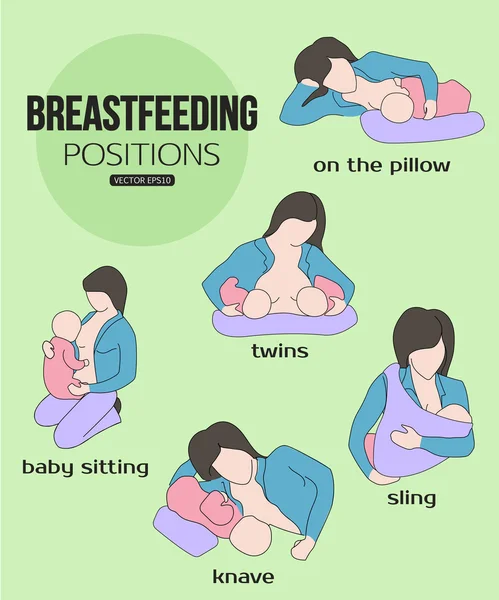 Breastfeeding and human lactation. Jones & Bartlett Learning ; 2014. 966 p . - Wambach K., Riordan J., "Breastfeeding and female lactation". Burlington, MA: Publishing House Jones & Bartlett Learning ; 2014. Pp. 966.
Breastfeeding and human lactation. Jones & Bartlett Learning ; 2014. 966 p . - Wambach K., Riordan J., "Breastfeeding and female lactation". Burlington, MA: Publishing House Jones & Bartlett Learning ; 2014. Pp. 966.
Looks like my baby has reflux!
Diseases and special conditions of the baby05/25/2020
It is normal for your baby to spit up in the first couple of months of life. About half of all newborns do this at least once a day. As the baby's digestive system matures, regurgitation occurs less frequently, so for most mothers it is only a short-term inconvenience [1].
However, in some children, the valve between the stomach and esophagus does not close properly. Because of this, the contents of the stomach periodically back up into the esophagus and can cause vomiting. Since a child vomits for a variety of reasons, it is important that the doctor rule out other options.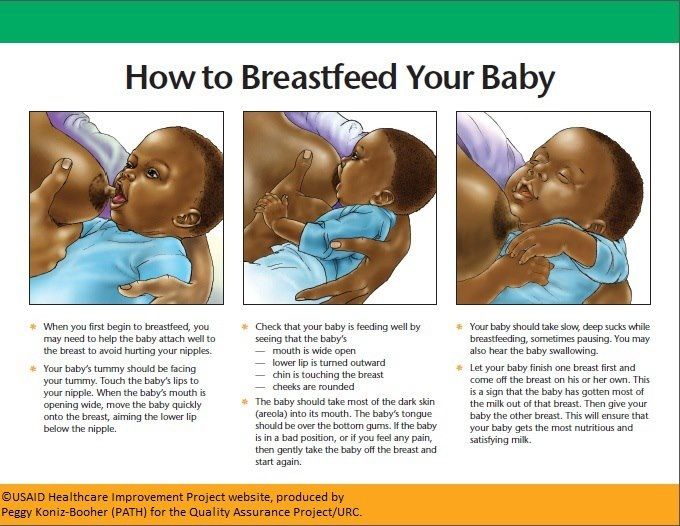 But it is quite possible that the baby has gastroesophageal reflux disease (GERD, it is also called gastroesophageal reflux). Reflux is not always noticeable, and it does not always cause discomfort to the child. However, severe symptoms of reflux can be painful and distressing for mother and baby [2].
But it is quite possible that the baby has gastroesophageal reflux disease (GERD, it is also called gastroesophageal reflux). Reflux is not always noticeable, and it does not always cause discomfort to the child. However, severe symptoms of reflux can be painful and distressing for mother and baby [2].
What signs to look out for?
The child may choke and cough, and may have a sore throat. Some children experience bad breath.
The mother may notice that the baby arches its back and turns its head. Instead of cuddling up to the mother, the baby tries to stretch his body, as this reduces the pain.
The baby may cry for a long time and be irritable during and after feeding. Sometimes his screams sound hoarse. This sometimes leads to misdiagnosis: it is mistakenly assumed that the baby has colic.
The child may resist feeding and even refuse to eat, and as a result, gain weight poorly.
What can help?
- First of all, your baby will most likely be more comfortable if his head is higher than his feet during feeding.
 For example, you can hold the baby at an angle of 30-40 degrees, placing the lower part of his body on the mother's lap. This is one way to make feeding more comfortable.
For example, you can hold the baby at an angle of 30-40 degrees, placing the lower part of his body on the mother's lap. This is one way to make feeding more comfortable. - Secondly, if the baby is breastfeeding while lying on its side, it is likely that things will go better on the left side. When you need to give the baby a different breast, it makes sense to change the position, and not turn the baby on the right side. It is also desirable to move the baby to a more upright position as soon as possible after feeding [3].
- It is useful to always remember the rule “head over legs”. A sling may come in handy for this purpose. A baby with reflux is often uncomfortable on a flat surface and may cry or spit up when in bed. Some parents prefer to hold their baby in their arms or in a sling during daytime naps. For others, it helps to bring the baby upright for a while after feeding.
- To change your baby, you can put him on the side: in this case, the baby will not press his legs on the tummy.
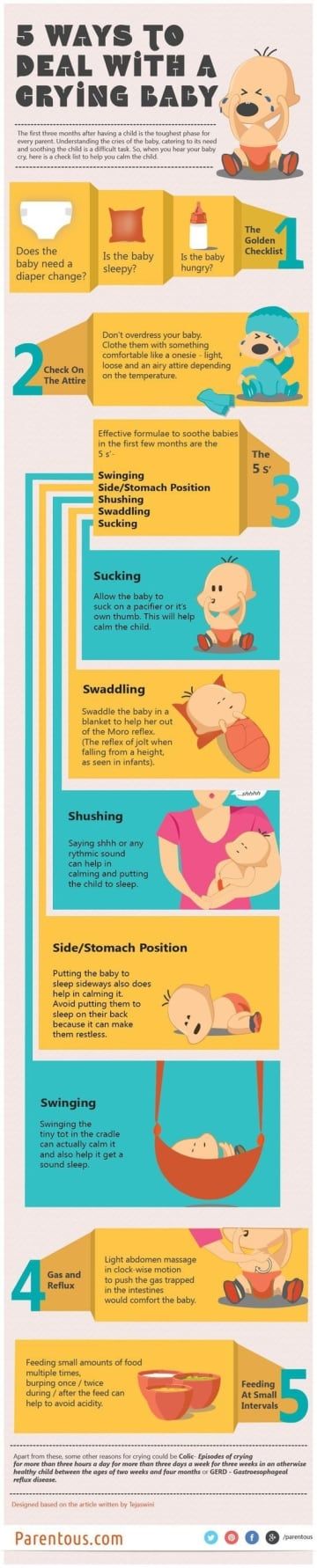 Some children like sun loungers in which they lie slightly elevated. Infants with reflux are often uncomfortable traveling in a car seat due to the pressure on their abdomen. Therefore, some mothers prefer to use the car as little as possible as long as the reflux bothers the baby. Instead, they ride public transport and carry their baby in a sling.
Some children like sun loungers in which they lie slightly elevated. Infants with reflux are often uncomfortable traveling in a car seat due to the pressure on their abdomen. Therefore, some mothers prefer to use the car as little as possible as long as the reflux bothers the baby. Instead, they ride public transport and carry their baby in a sling. - Since the opening between the stomach and esophagus is usually on the right side, it may be helpful to hold the right side of the child's body higher than the left.
- Short, frequent feedings reduce the frequency and discomfort of reflux [4]. If the mother has plenty of milk, the one-feed-one-breast approach can provide relief. However, it is worth evaluating whether it helps your baby.
What causes reflux?
There are several theories as to why reflux occurs. Some sources write that it is caused by the immaturity of the sphincter muscle [5], which becomes stronger as the child grows.
Other studies show an association between reflux and allergy or intolerance to cow's milk protein [6].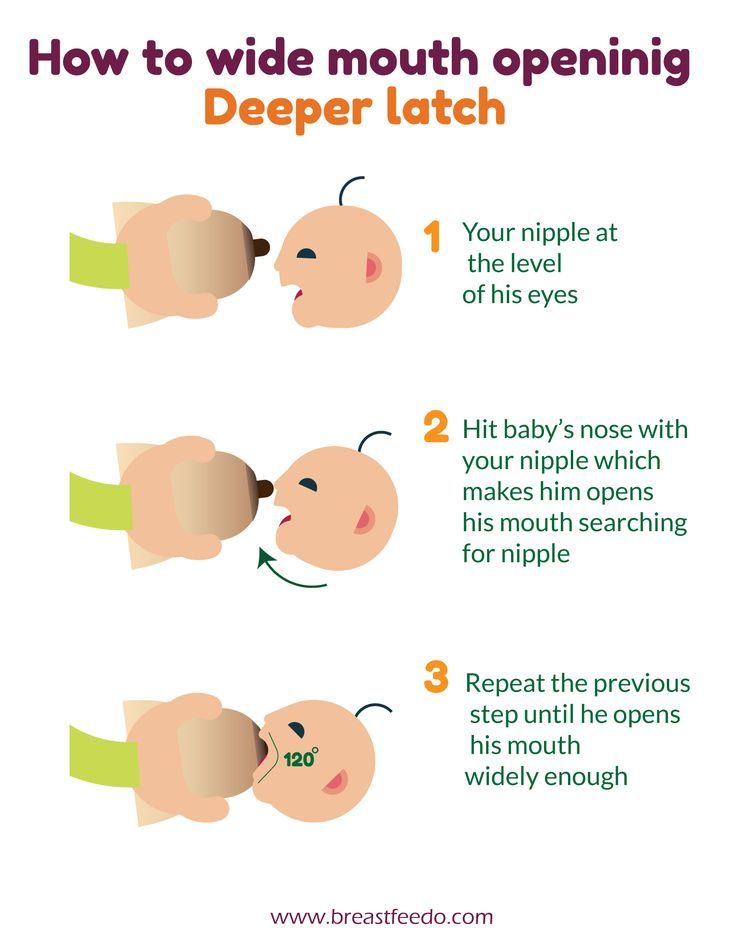 You can try eliminating dairy products from your diet by talking to your doctor to see if this can improve the situation.
You can try eliminating dairy products from your diet by talking to your doctor to see if this can improve the situation.
One of the main reasons may be the rapid flow of milk or its excess. If the baby appears to be choking or choking due to the rapid flow, you can try taking him off the breast for a few seconds (until the flow slows down) or feeding in a more upright position.
Make sure the baby is attached comfortably to the breast. The efficiency of tongue movements also matters. A short frenulum of the tongue can affect the quality of breast sucking and lead to air swallowing.
related articles:
Adding thickeners to food has significant disadvantages.
The addition of thickeners to expressed breast milk or formula is sometimes thought to help children with reflux. A 2018 study in the British Medical Journal reported that “nutrition thickeners are commonly used to treat children with gastroesophageal reflux despite a lack of conclusive evidence” [7]. Since most of the existing studies evaluating the effectiveness of thickened feeding for reflux symptoms have been conducted in formula-fed infants, information on the possible reduction of regurgitation in breastfed infants is limited [8].
Since most of the existing studies evaluating the effectiveness of thickened feeding for reflux symptoms have been conducted in formula-fed infants, information on the possible reduction of regurgitation in breastfed infants is limited [8].
In addition to the lack of conclusive evidence, this treatment has a number of significant disadvantages. Introducing complementary foods too early replaces breast milk, which is ideal for infant nutrition, with food with a lower energy content. It also reduces the mother's milk production. Spitting up thickened foods can increase distress and discomfort in a baby, and introducing complementary foods too early can also cause allergies in an already sensitive baby.
Switching to a mixture may not solve the problem
Although breastfeeding mothers are sometimes encouraged to switch to formula, this can aggravate symptoms. Reflux occurs in both breastfed and formula-fed infants, but studies have shown that formula-fed infants experience more frequent reflux episodes and last longer than breastfed infants [9].
Why is this so? One cause of reflux may be delayed gastric emptying. The fact that breast milk leaves the stomach twice as fast as formula milk means that breast milk reduces the chance of reflux [10].
If nothing works
If your child continues to suffer, your pediatrician may refer you to a gastroenterologist for medication.
The good news
In his Guide to Breastfeeding [11], Dr. Jack Newman, member of the Professional Advisory Board of the International La Leche League, says that breast milk is full of immune factors that interact with each other and protect the baby from bacteria, viruses and other microorganisms.
They form a protective layer on the baby's mucous membranes that line the intestines, respiratory tract and other areas. This stops microorganisms from entering the body through these mucous membranes. Dr. Newman explains that a baby who spit up gets double protection: both when the milk goes down into the stomach and when the baby spit it up.
If you need additional help and support, look for the nearest LLL group or meeting leader.
More information can be found here: Reflux in Newborns
Materials used:
1. Nancy Mohrbacher, “Breastfeeding Answers Made Simple. A Pocket Guide for Helping Mothers”
2. La Leche League International, “The Womanly Art of Breastfeeding”, 8th Edition, 2010, p. 417.
3. Boekel, S. “Gastro-esophageal reflux disease (GERD) and the breastfeeding baby”, ILCA Independent Study Module. Raleigh, North Carolina: International Lactation Consultant Association, 2000.
4. La Leche League International, “The Womanly Art of Breastfeeding” 8th Edition, 2010, p. 417.
5. NHS Reflux in babies
6. Nancy Mohrbacher, “Breastfeeding Answers Made Simple” 2010, pp. 517-520.
7. T'ng Chang Kwok, Shalini Ojha and Jon Dorling: “Feed thickeners in gastro-oesophageal reflux in infants” BMJ Pediatrics Open 2018
8.
Learn more