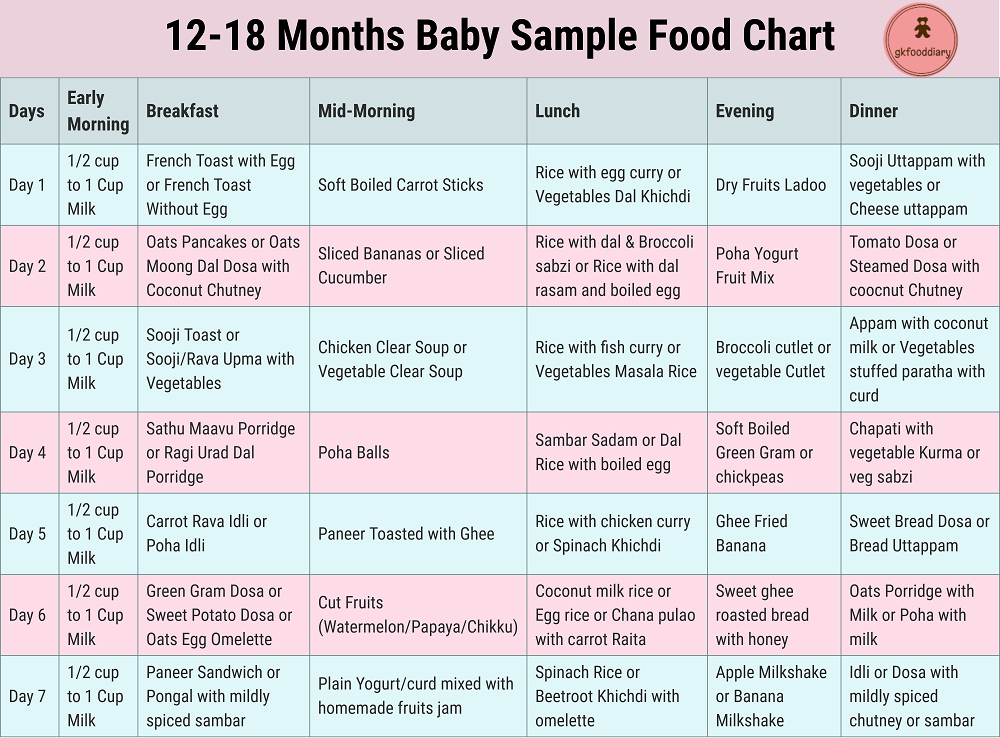
Feeding tube in baby stomach
Gastrostomy Tube (G-Tube) (for Parents)
What Is a G-Tube?
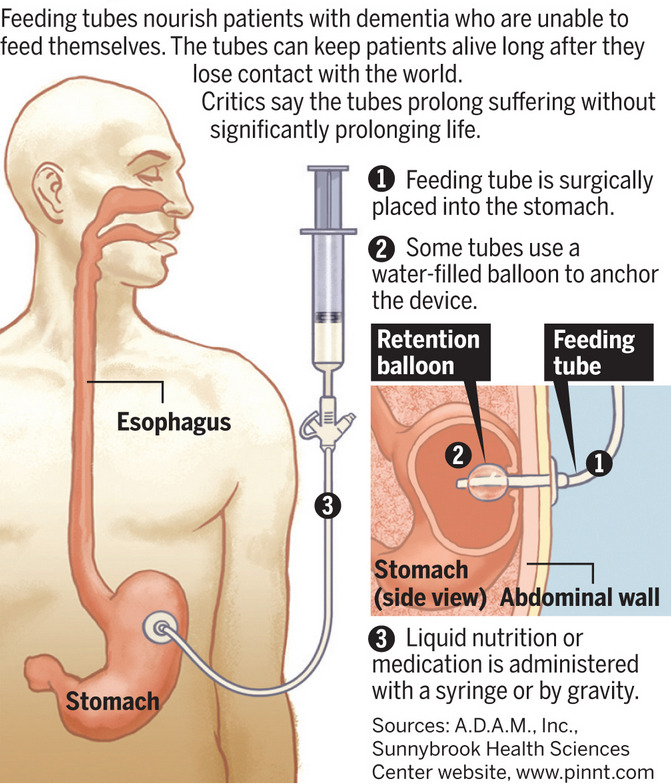
Some kids have medical problems that make it hard for them to get enough nutrition by mouth. A gastrostomy tube (also called a G-tube) is a tube inserted through the belly that brings nutrition directly to the stomach. It's one of the ways doctors can make sure kids who have trouble eating get the fluid and calories they need.
A surgeon puts in a G-tube during a short procedure called a gastrostomy. The G-tube can stay in place for as long as a child needs it.
Kids who have had a gastrostomy (ga-STROSS-teh-mee) can get back to their normal activities fairly quickly after they have healed.
Who Needs a G-Tube?
Kids need G-tubes for different kinds of health problems, including:
- congenital (present at birth) problems of the mouth, esophagus, stomach, or intestines
- sucking and swallowing disorders (due to premature birth, injury, a developmental delay, or another condition)
- failure to thrive (when a child can't gain weight and grow normally)
- extreme problems with taking medicines
What Happens Before G-Tube Placement?
Doctors often order several tests before a child can get a G-tube. The most common test is an X-ray of the upper gastrointestinal (GI) system. This lets the doctor see the upper part of the digestive system.
Sometimes the surgeon asks the family to meet with specialists, such as a gastroenterologist, dietitian, or social worker. This is to prepare a care plan so everything will be set up when the child goes home with the G-tube.
To get ready for the procedure, you will need to carefully follow instructions about when your child must stop eating and drinking. When you get to the hospital, the doctor will describe what will happen and answer any questions. The anesthesiology team will ask about your child's
medical historyand when your child last ate and drank.
Before the procedure begins, the care team sets up monitors to keep track of your child's vital signs (like blood pressure and oxygen level) and puts in an intravenous line (IV) to give medicines and anesthesia.
Your child will go to the operating room, and you'll go to a waiting area. A hospital staff member will tell you when the procedure is over.
A hospital staff member will tell you when the procedure is over.
What Happens During G-Tube Placement?
There are three ways doctors can insert a G-tube. Sometimes a combination of methods is used.
- The laparoscopic technique is done by making two small incisions (cuts) in the belly. One is for inserting the G-tube, and the other is where the surgeon inserts a tiny telescope called a laparoscope. The laparoscope helps the surgeon see the stomach and other organs and guide the G-tube into place.
- Open surgery is done with larger incisions. Surgeons choose this method to guide the G-tube into place when other methods are not a good choice — for example, if there is scar tissue from a past surgery or if the child needs another surgery done at the same time.
- The PEG procedure stands for percutaneous (through the skin) endoscopic gastrostomy. The surgeon inserts an endoscope (a thin, flexible tube with a tiny camera and light at the tip) through the mouth and into the stomach to guide the G-tube into place.

How Long Does G-Tube Placement Take?
Putting in a G-tube takes only about 30 to 45 minutes.
What Happens After G-Tube Placement?
Kids usually stay in the hospital for 1 or 2 days. Most hospitals let a parent stay with their child. While in the hospital, your child will get pain medicine as needed.
The nurses will teach you how to:
- Care for the tube and the skin around it to keep it clean and infection-free.
- Handle potential problems, such as the tube accidentally falling out.
- Give a feeding through the tube. You will also learn what to feed.
- Help your child eat independently, if the doctor says it's OK.
By the time your child is ready to go home, you should have:
- detailed instructions on home care, including bathing, dressing, physical activity, giving medicines through the tube, and venting (releasing gas from) the tube
- a visit scheduled with a home health care nurse to make sure things are going smoothly
- follow-up visits scheduled with your doctor to check the tube and your child's weight
Are There Any Risks From G-Tube Placement?
All surgeries come with some risks. The surgical team will discuss them with you before the procedure and do everything possible to minimize them. If you have any concerns, be sure to bring them up before the procedure.
The surgical team will discuss them with you before the procedure and do everything possible to minimize them. If you have any concerns, be sure to bring them up before the procedure.
Complications of surgery can include:
- extra tissue (granulation tissue) forming at the tube site
- leaking
- problems from anesthesia
- bleeding
- an allergic reaction
- infection
Granulation tissue or leaking can usually be fixed by caring for the wound as instructed or changing the feeding schedule. Sometimes surgery is needed to fix a problem at the surgery site.
How Can Parents Help After G-Tube Placement?
It's normal to feel a little bit nervous about the G-tube at first, but it's important that you feel comfortable taking care of it. Here are some tips:
- Always wash your hands well before caring for the G-tube.
- Always keep the feeding set tubing out of the way of infants and children. There is a risk that the feeding set tubing can get wrapped around a child’s neck, which could lead to strangulation or death.
- Know what to expect as the G-tube heals. Talk to your child's care team if you have questions.
- Get support from other parents. It can help to connect with other parents whose kids have G-tubes. Ask your child's doctor about a support group, or look online.
- Talk with a social worker. Some kids with a G-tube worry about how the tube looks and how others might react. If your child is concerned, ask your care team to recommend a social worker who can help.
When Should I Call the Doctor?
Call your doctor if your child has any of these problems:
- a dislodged tube
- a blocked tube
- any signs of infection (including redness, swelling, or warmth at the tube site; discharge that's yellow, green, or foul-smelling; fever)
- excessive bleeding or drainage from the tube site
- severe belly pain
- vomiting or diarrhea that keeps happening
- trouble passing gas or having a bowel movement
- pink-red tissue coming out from around the tube
Most problems can be treated quickly when they're found early.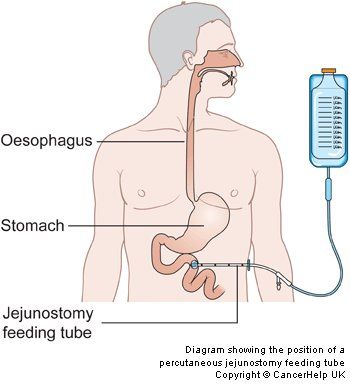
Reviewed by: Loren Berman, MD and Kate M. Cronan, MD
Date reviewed: February 2022
Tube feeding | Bliss
Your baby may be fed using tube feeding while on the neonatal unit. Find out why this might be and information about caring for your baby while they are being tube fed.
What is tube feeding?
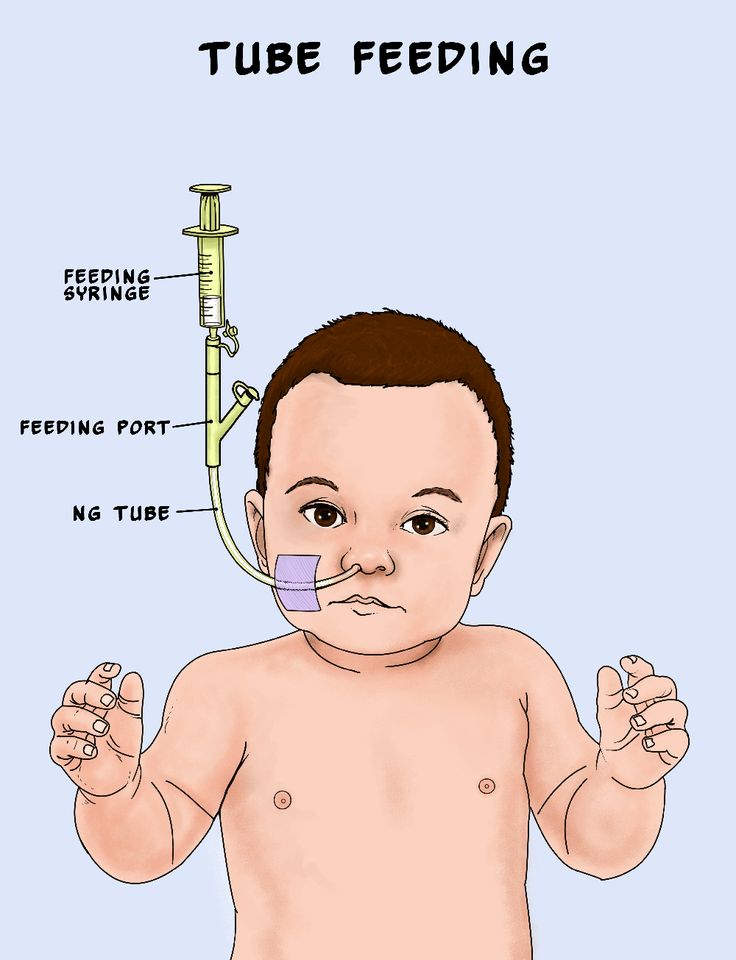
During tube feeding, breast milk or formula is given through a tube passed into your baby’s nose or mouth to their stomach. Types of tube feeding include the following:
- Nasogastric tube feeding (also called an NG tube) - This is when a baby is fed through a small soft tube, which is placed in the nose and runs down the back of the throat, through the food pipe (oesophagus) and into the stomach.
- Orogastric tube feeding - This is when a baby is fed through a small soft tube, which is placed in the mouth and runs down the back of the throat, through the food pipe (oesophagus) and into the stomach.

Babies who are very premature or sick may need to be fed using parenteral nutrition (PN) at first.
Why does my baby need to be fed using tube feeding?
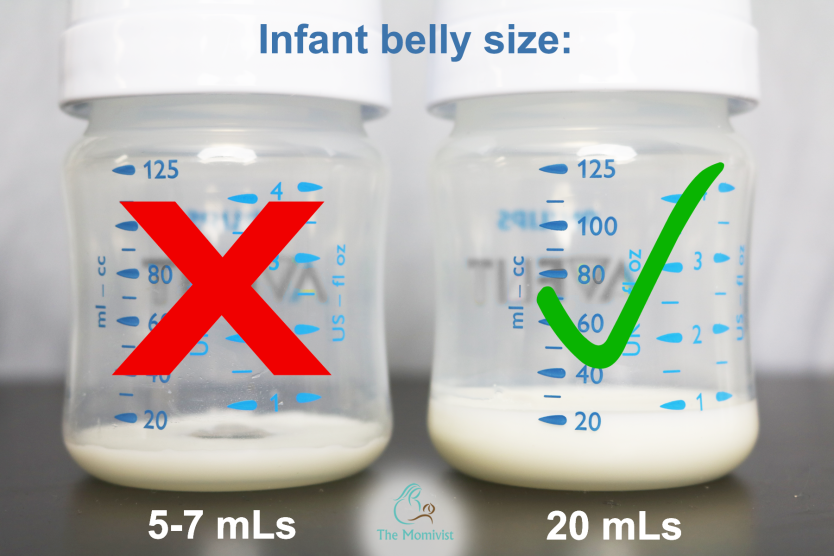
Tube feeding is often used to feed premature and sick babies as they can be too small and sick to breastfeed or bottle feed at first. Babies born premature or sick have a low supply of energy and nutrients, so it is important that they are able to have small nutritional feeds often, without lowering their energy levels.
In babies born premature, the coordination of sucking, swallowing and breathing needed for effective feeding is usually not fully established until about 32 to 34 weeks’ gestation (although this is different for different babies). Babies born at term and sick may also take longer to co-ordinate feeding. Tube feeding will help your baby receive enough nutrition to grow and develop.
Can I be involved in caring for my baby if they are being tube fed?
Yes, you can. Staff on the neonatal unit will encourage you to be as involved as possible in the care of your baby on the neonatal unit.![]() If you feel comfortable doing so, they should show you and your partner how to give tube feeds. Staff on the neonatal unit will explain how tube feeding works and will teach you how to:
If you feel comfortable doing so, they should show you and your partner how to give tube feeds. Staff on the neonatal unit will explain how tube feeding works and will teach you how to:
- Check the tube is in the correct position before feeding
- Prepare the milk and fill the syringe that is connected to the feeding tube
- Position your baby correctly for tube feeds
- Give the milk slowly to support comfortable digestion
- Know what to look for during a feed.
This can feel quite scary at first, but with practice you should gain confidence. You will have the time to give the milk very slowly which helps your baby to digest more comfortably.
If your baby is well enough to come out of the incubator, you and your partner can also practice skin-to-skin contact with your baby while they are tube feeding. Skin-to-skin contact has lots of benefits for you and your baby, and helps parents to feel closer to their baby and more confident in caring for them.
When can my baby stop tube feeding?
In time, you may notice your baby demonstrating feeding cues during a tube feed. For example, they may open and close their mouth, put out their tongue or suck their fingers during a tube feed. This shows that they might be ready to practise breastfeeding or bottle feeding.
If you are planning to breastfeed and your baby is well enough to come out of the incubator, giving them lots of opportunities to be close to the breast may help them to learn to breastfeed. During a tube feed may be a good time to do this. When they are more mature and interested enough, some babies will start licking milk and in time practice sucking. As your baby starts to take more breast and bottle feeds, they will not need as many top-ups of milk from the feeding tube. This will depend on your baby’s energy levels and their ability to coordinate sucking, swallowing and breathing.
Some parents have concerns about their baby changing from tube feeding to breastfeeding, as it is more difficult to measure how much milk their baby is having. Your baby will show signs that they are receiving enough milk, such as feeding cues and wet and dirty nappies. The healthcare team supporting you will monitor your baby’s feeding and will manage any top-ups that might be needed. Talk to a member of staff on your unit if you have any concerns.
Your baby will show signs that they are receiving enough milk, such as feeding cues and wet and dirty nappies. The healthcare team supporting you will monitor your baby’s feeding and will manage any top-ups that might be needed. Talk to a member of staff on your unit if you have any concerns.
What will happen if my baby needs to go home from the neonatal unit with a feeding tube?
If your baby is going home with a feeding tube, a member of unit staff will show you how to feed and care for the tube yourself. It may be you or your community neonatal nurse who will replace the tube when you go home. This will depend on your baby’s needs, your preferences, and the support the unit provides.
Support will always be available if you do not feel comfortable with replacing the tube yourself. If you have any questions or concerns, talk to the unit staff.
Related content
Bolus Feeding Using a Syringe)
Your child is discharged from the hospital with a nasogastric (NG) feeding tube in place. The tube is a thin, soft tube that is inserted into the baby's stomach through the nose. This tube delivers liquid food directly to the stomach. Before your baby was released from the hospital, you were shown how to feed with a nasogastric tube. This memo will help you remember the necessary procedure for feeding at home. You can also get help from a district nurse at your home. nine0005
The tube is a thin, soft tube that is inserted into the baby's stomach through the nose. This tube delivers liquid food directly to the stomach. Before your baby was released from the hospital, you were shown how to feed with a nasogastric tube. This memo will help you remember the necessary procedure for feeding at home. You can also get help from a district nurse at your home. nine0005
NOTE: There are many different types of nasogastric tubes, feeding syringes, and pumps. The appearance and function of the nasogastric tube and accessories prescribed for your child may differ from those shown and described below. Always follow the advice of your child's primary care physician or district nurse. Write down their phone numbers in case you need help. Also write down the phone number of the facility that supplies medical equipment for your child. In the future, you will need to order additional accessories that your child may need.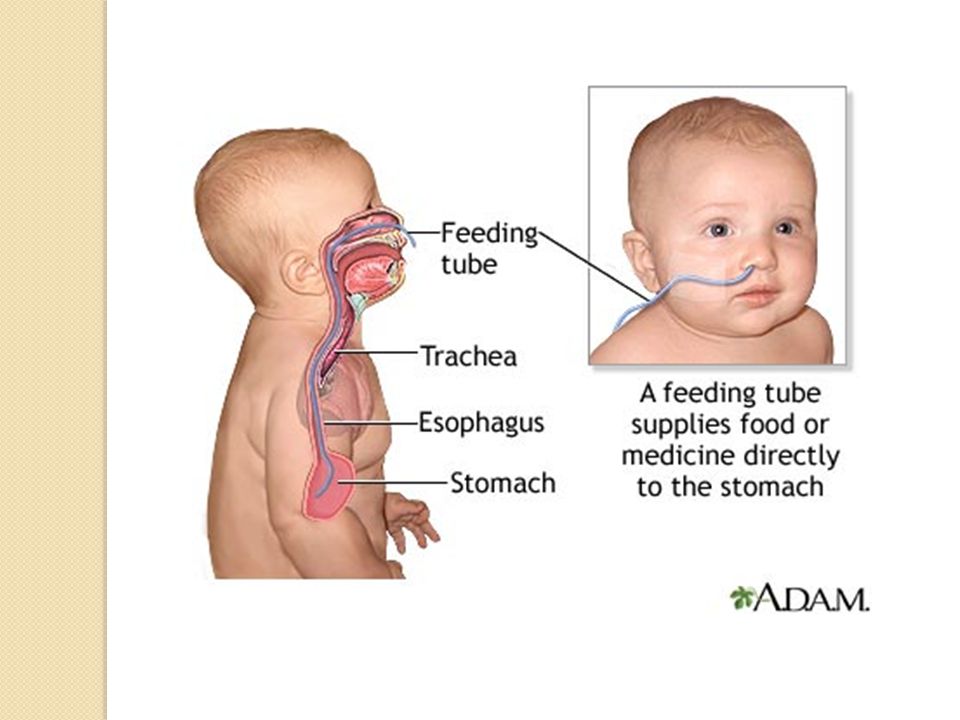 Write down all the phone numbers you need in the spaces below. nine0005
Write down all the phone numbers you need in the spaces below. nine0005
Healthcare provider phone number: _________________________________________________________
Home health nurse phone number: _________________________________________________
Medical supply company phone number: ______________________
Types of feeding
nine0019Two types of feeding can be performed with a nasogastric tube:
-
bolus feeding. Several times a day, an amount of liquid food, commensurate with one meal, is fed through the tube. Bolus feeding is done with a syringe or pump;
- nine0002 continuous feeding. Liquid food drips slowly through the tube. Continuous power is supplied by a pump.
Your child may be prescribed one or both types of food. Detailed instructions for each type of food are given below.
Detailed instructions for each type of food are given below.
Syringe Bolus
Your child's doctor or district nurse will tell you how much liquid food to use with each bolus. You will also be told how many times a day to feed your baby. Record this information below.
How much to give at each feeding: _____________
Number of feedings per day (How often to feed): __________________________
nine0017 AccessoriesActions
-
Wash your hands with soap and water.
-
Make sure the tube is in the stomach (as you were shown in the hospital). Be sure to perform this step BEFORE feeding begins.
-
Check liquid food label and expiration date. Never use jars (or bags) with food that have already expired.
 In this case, you must use a new jar (or bag) with food. nine0005
In this case, you must use a new jar (or bag) with food. nine0005 -
Open the hole plug at the end of the food probe.
-
Remove the plunger of the feeding syringe.
-
Connect the feeding syringe to the feeding port of the probe.
-
Gently bend or squeeze the probe with one hand. While holding the tube bent or pinched, slowly draw the liquid food into the feeding syringe with your free hand. In this case, the food will not flow through the probe, which will allow you to measure its amount. nine0005
-
Fill the feeding syringe to the level prescribed by the child's healthcare provider.
-
The probe can now be released.
-
Hold the feeding syringe straight.
 In this case, the food will pass through the probe by gravity without additional pressure. Adjust the angle of the feeding syringe to control the rate of fluid flow. nine0005
In this case, the food will pass through the probe by gravity without additional pressure. Adjust the angle of the feeding syringe to control the rate of fluid flow. nine0005 -
If the food flows too slowly or does not flow at all, insert the plunger into the syringe. Gently, lightly press the piston. This will remove any particles blocking or clogging the probe. Do not push the syringe plunger all the way or with force.
-
Refill the feeding syringe with food if necessary. Repeat the above steps until the child receives the prescribed amount of food. nine0005
-
After feeding, rinse the tube with water (as you were shown in the hospital).
-
Disconnect the feeding syringe.
-
Close the cap on the food inlet of the probe.
| nine0002 AddiAdditional instructions:_________________________________________________________________________________ ________________________________________________________________________________________________ ________________________________________________________________________________________________ ________________________________________________________________________________________________ |
Call your doctor right away if you experience any of the following.
-
The child has trouble breathing.
-
Formation of redness, swelling (swelling), leakage (leakage), ulcers (sores) or suppuration (pus) on the skin in the area of the probe.
nine0029
-
Presence of blood (blood) around the probe, in the child's stool or stomach contents.
-
Baby coughing (cough), shortness of breath (choke) or vomiting (vomit) while feeding.
-
Urebenka swollen (bloated abdomen) or hard abdomen (rigid abdomen) (abdomen hard with light pressure).
nine0029 -
Child diarrhea (diarrhea) or constipation (constipation).
-
Child temperature (fever) 38˚C ( 100.4° F) or higher.
© 2000-2022 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions. nine0005
Was this helpful?
Yes no
Tell us more.

Check all that apply.
Wrong topic—not what I was looking for.
It was hard to understand. nine0005
It didn't answer any of my questions.
I still don't know what to do next.
other.
NEXT ▶
nine0017 Last question: How confident are you filling out medical forms by yourself? Not at all A little Somewhat Quite a bit Extremely
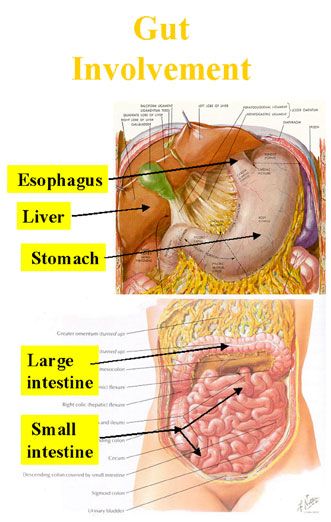
Enteral nutrition (tube feeding)
What is enteral nutrition?
Sometimes during treatment and recovery, children with cancer cannot get the calories and nutrients they need orally. Tube feeding, or enteral nutrition, provides nutrition in the form of a liquid or mixture given through a tube that is inserted into the stomach or intestines. Some medications may also be delivered through such a tube (probe).
Tube feeding, or enteral nutrition, provides nutrition in the form of a liquid or mixture given through a tube that is inserted into the stomach or intestines. Some medications may also be delivered through such a tube (probe).
Typically, the tube is inserted in two ways:
- Nasal (non-surgical)
- Through a small incision in the abdomen (surgical method)
Most commonly used are nasogastric tubes and gastrostomy tubes. But there are several types of enteral feeding tubes that differ in the method of insertion and location in the digestive tract.
Sometimes the patient is simply not able to eat enough calories or protein. There is no fault in this. It is important to help your child understand that nutritional support is not a punishment. Most children get used to the enteral feeding tube quickly. It is important that the child does not touch or pull the phone. Follow skin care instructions at the insertion site to avoid irritation or infection. nine0005
nine0005
A nasogastric tube is inserted into the stomach or small intestine through the nose and throat.
Enteral feeding tube types
Enteral feeding tube connects to the stomach or small intestine. The location depends on how the patient tolerates the formula and how well their body is able to digest the nutrients. If possible, they try to place the probe in the stomach so that digestion occurs naturally.
There are 5 types of enteral feeding tubes:
Nasogastric Tube . A nasogastric tube is inserted into the stomach through the nose. It passes through the throat, esophagus and into the stomach.
Nasojejunal Probe . A nasojejunal tube is similar to a nasogastric tube but passes through the entire stomach into the small intestine.
Gastrostomy Tube (Gastrostomy Probe) . A gastrostomy tube is inserted through a small incision in the skin. The probe in this case passes through the wall of the abdominal cavity directly into the stomach. nine0005
nine0005
Gastrojejunostomy tube (gastrojejunostomy probe) . The gastrojejunostomy tube is inserted into the stomach like a gastrostomy tube, but passes through the stomach into the small intestine.
Jejunostomy Probe . A jejunostomy tube is inserted through a small incision in the skin and passed through the abdominal wall into the small intestine.
Nasal tubes, including nasogastric and nasojejunal tubes, are generally used for short-term enteral feeding, usually not more than 6 weeks. The probe comes out of the nostril and is attached to the skin with adhesive tape. Nasogastric and nasojejunal tubes have a number of advantages, such as a low risk of infection and a simple insertion procedure. However, the probe must be attached to the face, and this worries some children. Other children may have problems with the nasogastric tube due to chemotherapy, which irritates the skin and mucous membranes. nine0250
Surgical insertion tubes - gastrostomy tube, gastrojejunostomy tube and jejunostomy tube - are used for longer periods of time or if a nasal tube cannot be placed in the child.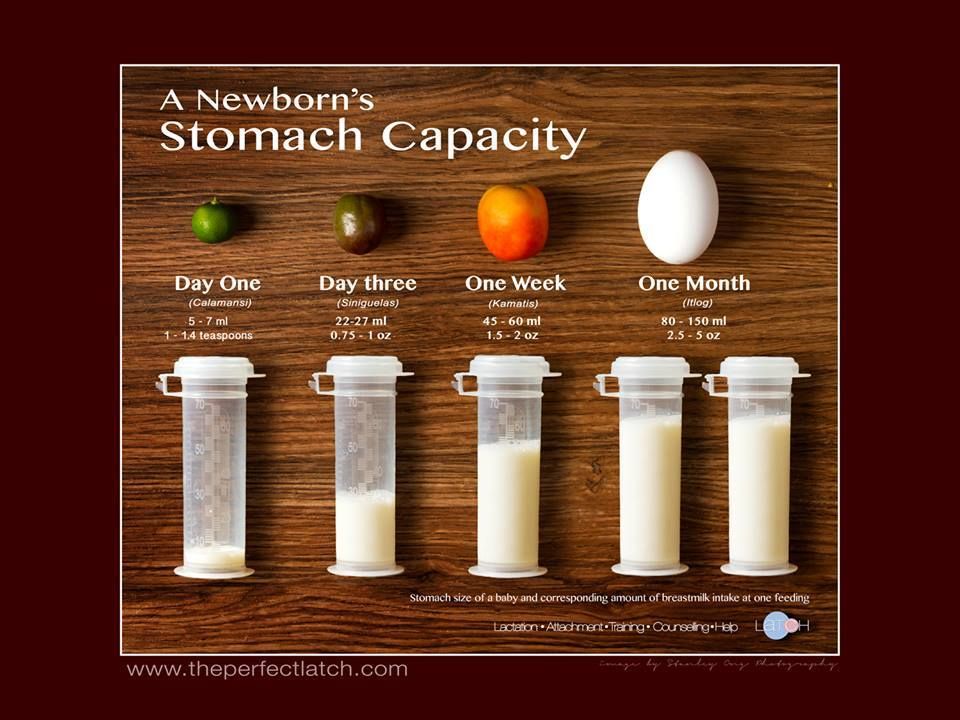 The opening in the abdominal wall through which the probe is inserted is called the stoma. A long tube or a "button" (low profile) probe may be visible on the patient's body. After healing, the stoma is usually pain free and the child can perform most daily activities. nine0005
The opening in the abdominal wall through which the probe is inserted is called the stoma. A long tube or a "button" (low profile) probe may be visible on the patient's body. After healing, the stoma is usually pain free and the child can perform most daily activities. nine0005
-
Insertion of nasogastric and nasojejunal tubes
-
Gastrostomy, gastrojejunostomy and jejunostomy insertion
After healing, the stoma usually does not hurt. The child can perform most daily activities.
Side effects of enteral nutrition
The most common side effects of enteral nutrition are nausea, vomiting, stomach cramps, diarrhoea, constipation and bloating. nine0005
There may be other side effects:
- Infection and irritation at the insertion site
- Probe misaligned or falling out
- Lung feeding formula
Most side effects can be avoided by following the care and nutrition instructions.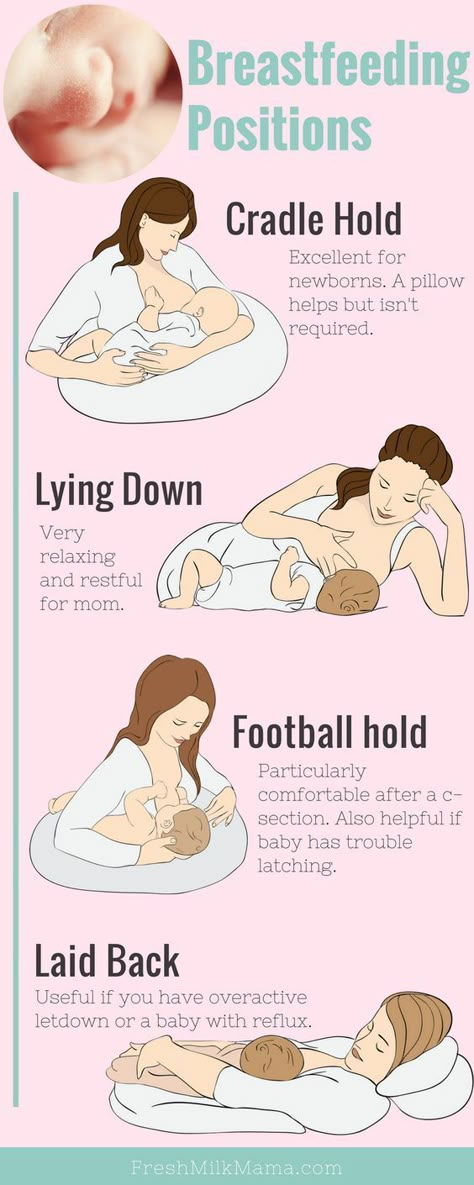
Feeding babies with tubes in place
The nutritionist is responsible for providing the baby with all the necessary nutrients. In children with cancer, an enteral feeding tube is often used in addition to what the child can eat normally. However, some patients have to enter all the nutrients through a tube. nine0005
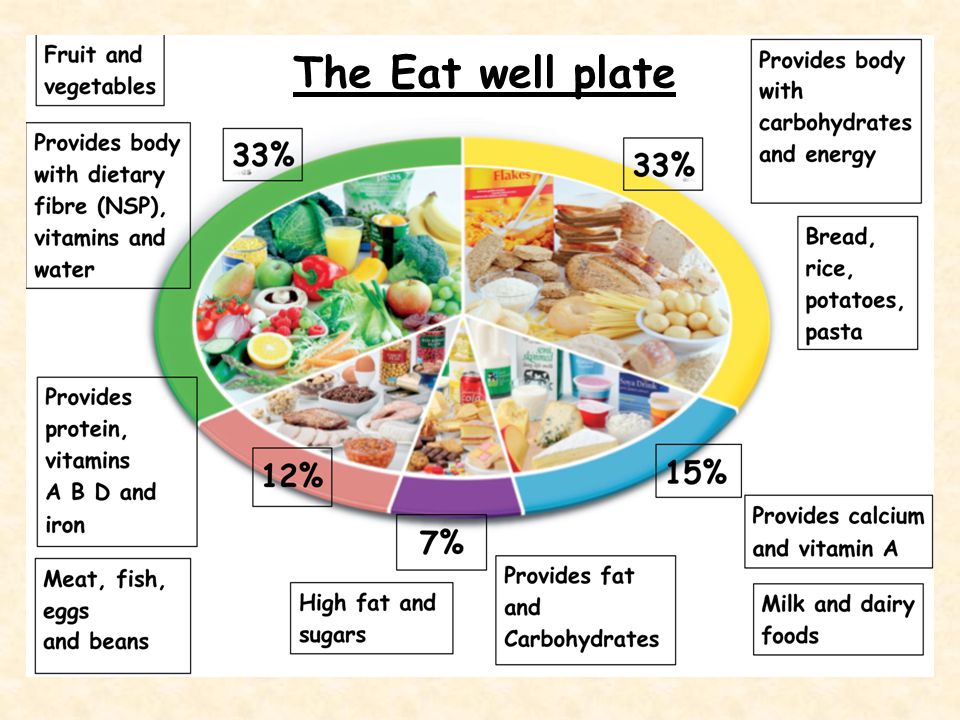
The patient is prescribed a mixture containing:
- Calories
- Fluid
- Carbohydrates
- Fats
- Protein
- Vitamins and minerals
Standard formulas are suitable for many patients. For babies, it is preferable to use breast milk. Some children need special formulas that take into account their characteristics: the presence of allergies, diabetes or digestive problems.
It is very important for family members to work closely with a nutritionist. Nutritional needs may change due to changes in the child's health or side effects such as vomiting or diarrhea. nine0005
Types of enteral feeding
There are three types of enteral feeding - bolus, continuous and gravity.
Bolus feeding - large doses of the mixture are given to the patient by tube several times a day. This species is closest to the usual diet.
Continuous Power - Electronic pump delivers small doses of formula over several hours. Some children may need continuous feeding to reduce nausea and vomiting. nine0005
Gravity Feeding - A bag of formula is placed on the IV stand and a predetermined amount of formula is dripped through the tube at a slow rate. The duration of such nutrition depends on the needs of the patient.
Enteral feeding at home
Children can go home with a feeding tube. The doctors will ensure that family members know how to feed and care for the probe. Family members need to pay attention to the following issues:
- Weight gain or loss
- Vomiting or diarrhea
- Dehydration
- Infection
Formulas, Consumables, and Equipment Required:
- Formula: Most enteral formulas are sold ready-made.
 Some are available as a powder or liquid to mix with water.
Some are available as a powder or liquid to mix with water. - Syringe
- Adapter tube (if the child has a button tube for long-term enteral nutrition)
- Pump (with continuous power)
- Feeding formula bag with tubing (for continuous feeding)
- IV Stand (Gravity Feed)
General tips for enteral feeding at home:
- Always wash your hands with soap and water before feeding your baby.
- Make sure the baby's head is above the stomach.
- Throw away any ready-made or homemade formulas that have been opened and kept in the refrigerator for 24 hours or more. nine0029
- Store mixed formulations in the refrigerator and discard after 24 hours.
- Ready-to-use formulas do not need to be refrigerated.
- Do not empty the syringe completely during feeding.
- Wash the syringe (and transfer tube, if used) with warm water and dishwashing detergent after each use.
- Watch for signs of nausea, vomiting, bloating or irritability while feeding.