Food for baby with gastro
Gastroenteritis in children - Better Health Channel
Gastroenteritis (or gastro) is a bowel infection that causes diarrhoea and sometimes vomiting. Diarrhoea is runny, watery bowel motions.
Vomiting may settle quickly, but diarrhoea may last up to 10 days. Bouts of gastro can cause dehydration, which can be dangerous for very young babies.
Causes of gastroenteritis in children
Gastroenteritis is caused by different things – including viruses, bacteria, bacterial toxins, parasites, particular chemicals and some drugs.
If your child gets gastro more than once the cause may be different each time.
Infectious gastroenteritis in children
Gastroenteritis can spread quickly. Infectious gastroenteritis is caused by viruses, bacteria or parasites. It is usually ingested through food or drink. Some of the common types of infectious gastroenteritis include:
- Escherichia coli infection
- Campylobacter infection
- Cryptosporidium infection
- Giardiasis
- Salmonellosis
- Shigellosis
- Viral gastroenteritis.
Symptoms of gastroenteritis
Children may not have all symptoms, but in general, gastroenteritis symptoms can include:
- loss of appetite
- bloating
- nausea
- vomiting
- abdominal cramps
- abdominal pain
- diarrhoea
- bloody stools (poo) – in some cases
- pus in stools – in some cases
- generally feeling unwell – including lethargy and body aches.
Children with gastroenteritis must keep drinking
If your child has gastroenteritis, make sure they drink clear fluids (or breastmilk if your baby is breastfeeding).
Babies under 6 months old can become ill quickly with gastro – they need extra fluids to replace fluids lost by diarrhoea and vomiting.
If you are breastfeeding, continue to do this. If bottle feeding, give clear fluids for the first 12 hours, then give the normal formula in smaller, more frequent amounts.
It is important for the fluids to be taken even if the diarrhoea seems to get worse. It will help if you:
It will help if you:
- Offer babies a drink every time they vomit.
- Give older children a drink (150–200ml) after every big vomit or bout of diarrhoea.
- Give small amounts of fluids often if your child is vomiting a lot (a mouthful every 15 minutes).
Go to the doctor if your child is very sick
Take your child to the doctor if they:
- Vomit often.
- Are not drinking
- Show any signs of dehydration.
- Have blood in their bowel motion (poo)
- Have significant abdominal pain.
Babies under 6 months who have gastroenteritis may need extra visits to the doctor – they need to be checked again after 6 to 12 hours. Your doctor can advise what other steps to take.
Do not give medicines to reduce the vomiting or diarrhoea.
Go to your doctor if you notice that your child:
- Has a dry mouth and tongue.
- Is not passing urine (dry nappies).
- Has sunken eyes.
- Has cold hands and feet.
- Is more sleepy than usual.
How to prevent dehydration in children with gastroenteritis
To prevent your child becoming dehydrated give clear fluids like:
- Water.
- Oral rehydration products available from a pharmacist – follow instructions to make it up.
- Diluted fruit juice (natural) – 1 tablespoon of juice to 4 tablespoons of water.
Children with gastroenteritis can eat their usual foods
Your child may refuse food at first. This is not a problem as long as they drink clear fluids.
Doctors now suggest there is no need to restrict food if your child has gastroenteritis. Generally, if your child is hungry at any time, give them the food they normally eat.
How to prevent the spread of gastroenteritis
Good old-fashioned handwashing with soap and water is still the best defence against spreading gastroenteritis.
You can prevent the spread of gastroenteritis to other people if you:
- Make sure everyone in the family washes their hands regularly, especially after they use the toilet and before they eat.

- Wash your child’s hands with warm water and soap after they use the toilet and before and after they eat.
- Wash your hands before you feed and after you change your child’s nappies.
- Clean kitchen tops, toys, toilet seats, nappy change tables and taps to ensure you don’t spread the infection to others at home.
- Keep your child away from others until 48 hours after their symptoms have stopped. If symptoms persist, visit your GP.
- Don't allow your child to attend child care or school until 48 hours after their symptoms have stopped.
- Teach your child good hand hygiene by showing them how to become a Soapy Hero!
Remember, washing hands with soap and water is the best way to prevent gastroenteritis infection. Alcohol-based hand sanitisers while effective against some viruses (such as coronavirus), are not effective against gastroenteritis.
Where to get help
- Your GP (doctor)
- NURSE-ON-CALL Tel. 1300 606 024 – for expert health information and advice (24 hours, 7 days)
- Your local council health department
- Communicable Disease Epidemiology and Surveillance Unit, Department of Health, Victorian Government Tel.
 1300 651 160
1300 651 160 - Maternal and child health nurse
- Maternal and Child Health Line Tel. 13 22 29 (for the cost of a local call throughout Victoria).
- Local school nurse
Gastroenteritis in children - Better Health Channel
Gastroenteritis (or gastro) is a bowel infection that causes diarrhoea and sometimes vomiting. Diarrhoea is runny, watery bowel motions.
Vomiting may settle quickly, but diarrhoea may last up to 10 days. Bouts of gastro can cause dehydration, which can be dangerous for very young babies.
Causes of gastroenteritis in children
Gastroenteritis is caused by different things – including viruses, bacteria, bacterial toxins, parasites, particular chemicals and some drugs.
If your child gets gastro more than once the cause may be different each time.
Infectious gastroenteritis in children
Gastroenteritis can spread quickly. Infectious gastroenteritis is caused by viruses, bacteria or parasites. It is usually ingested through food or drink.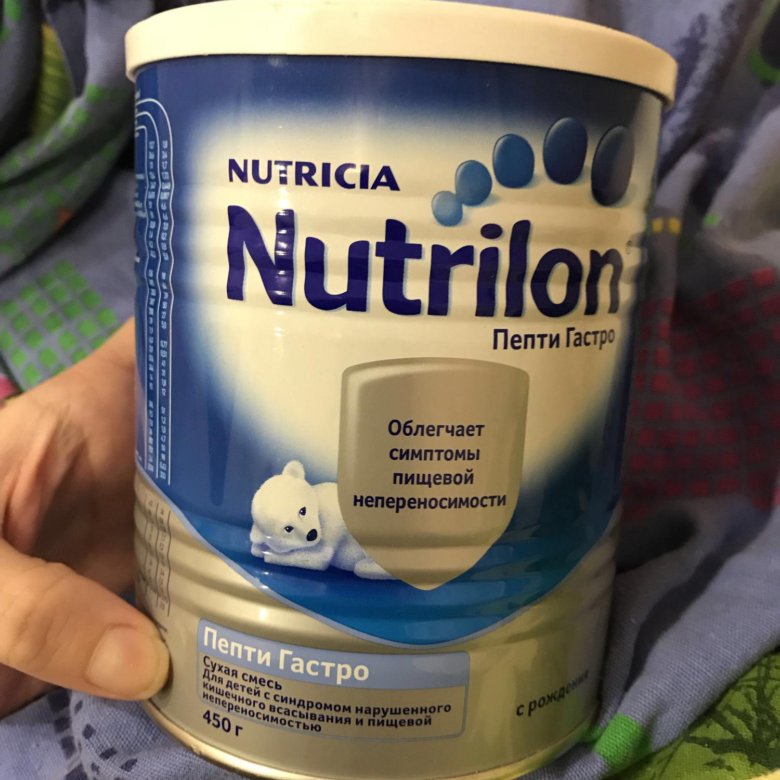 Some of the common types of infectious gastroenteritis include:
Some of the common types of infectious gastroenteritis include:
- Escherichia coli infection
- Campylobacter infection
- Cryptosporidium infection
- Giardiasis
- Salmonellosis
- Shigellosis
- Viral gastroenteritis.
Symptoms of gastroenteritis
Children may not have all symptoms, but in general, gastroenteritis symptoms can include:
- loss of appetite
- bloating
- nausea
- vomiting
- abdominal cramps
- abdominal pain
- diarrhoea
- bloody stools (poo) – in some cases
- pus in stools – in some cases
- generally feeling unwell – including lethargy and body aches.
Children with gastroenteritis must keep drinking
If your child has gastroenteritis, make sure they drink clear fluids (or breastmilk if your baby is breastfeeding).
Babies under 6 months old can become ill quickly with gastro – they need extra fluids to replace fluids lost by diarrhoea and vomiting.
If you are breastfeeding, continue to do this. If bottle feeding, give clear fluids for the first 12 hours, then give the normal formula in smaller, more frequent amounts.
It is important for the fluids to be taken even if the diarrhoea seems to get worse. It will help if you:
- Offer babies a drink every time they vomit.
- Give older children a drink (150–200ml) after every big vomit or bout of diarrhoea.
- Give small amounts of fluids often if your child is vomiting a lot (a mouthful every 15 minutes).
Go to the doctor if your child is very sick
Take your child to the doctor if they:
- Vomit often.
- Are not drinking
- Show any signs of dehydration.
- Have blood in their bowel motion (poo)
- Have significant abdominal pain.
Babies under 6 months who have gastroenteritis may need extra visits to the doctor – they need to be checked again after 6 to 12 hours. Your doctor can advise what other steps to take.
Do not give medicines to reduce the vomiting or diarrhoea.
Go to your doctor if you notice that your child:
- Has a dry mouth and tongue.
- Is not passing urine (dry nappies).
- Has sunken eyes.
- Has cold hands and feet.
- Is more sleepy than usual.
How to prevent dehydration in children with gastroenteritis
To prevent your child becoming dehydrated give clear fluids like:
- Water.
- Oral rehydration products available from a pharmacist – follow instructions to make it up.
- Diluted fruit juice (natural) – 1 tablespoon of juice to 4 tablespoons of water.
Children with gastroenteritis can eat their usual foods
Your child may refuse food at first. This is not a problem as long as they drink clear fluids.
Doctors now suggest there is no need to restrict food if your child has gastroenteritis. Generally, if your child is hungry at any time, give them the food they normally eat.
How to prevent the spread of gastroenteritis
Good old-fashioned handwashing with soap and water is still the best defence against spreading gastroenteritis.
You can prevent the spread of gastroenteritis to other people if you:
- Make sure everyone in the family washes their hands regularly, especially after they use the toilet and before they eat.
- Wash your child’s hands with warm water and soap after they use the toilet and before and after they eat.
- Wash your hands before you feed and after you change your child’s nappies.
- Clean kitchen tops, toys, toilet seats, nappy change tables and taps to ensure you don’t spread the infection to others at home.
- Keep your child away from others until 48 hours after their symptoms have stopped. If symptoms persist, visit your GP.

- Don't allow your child to attend child care or school until 48 hours after their symptoms have stopped.
- Teach your child good hand hygiene by showing them how to become a Soapy Hero!
Remember, washing hands with soap and water is the best way to prevent gastroenteritis infection. Alcohol-based hand sanitisers while effective against some viruses (such as coronavirus), are not effective against gastroenteritis.
Where to get help
- Your GP (doctor)
- NURSE-ON-CALL Tel. 1300 606 024 – for expert health information and advice (24 hours, 7 days)
- Your local council health department
- Communicable Disease Epidemiology and Surveillance Unit, Department of Health, Victorian Government Tel. 1300 651 160
- Maternal and child health nurse
- Maternal and Child Health Line Tel. 13 22 29 (for the cost of a local call throughout Victoria).
- Local school nurse
Nutrition for intestinal infections in children
Parents of small children are especially afraid of intestinal infections. After all, it is important for a mother that her baby is full and healthy. And the presence of an intestinal infection in the body does not even allow to feed the child properly. Any meal is accompanied by vomiting, diarrhea, and in severe forms of the disease, children cannot eat at all.
After all, it is important for a mother that her baby is full and healthy. And the presence of an intestinal infection in the body does not even allow to feed the child properly. Any meal is accompanied by vomiting, diarrhea, and in severe forms of the disease, children cannot eat at all.
Experienced grandmothers advise to keep the child on dry rations (ie, to eat crackers, dryers, biscuit cookies), others offer to treat immediately with herbal decoctions. Feeding children with an intestinal infection is a very important and delicate issue, so you should know not only how and what to feed a child, but also other important principles, for example, combating dehydration, drinking regimen, and so on. You can read about all this in the materials of this article.
What is an intestinal infection
Intestinal infections are the second most common childhood disease and are more common in young children (under 3 years of age). In the morning, the child was healthy and cheerful, as after a couple of hours the baby abruptly begins to vomit, the stool is upset and the temperature rises. All these symptoms indicate the presence of an intestinal infection in the body.
All these symptoms indicate the presence of an intestinal infection in the body.
Intestinal infection can be either viral or bacterial. From the names themselves it becomes clear what the difference between their pathogens is. In childhood, it is the rotovirus causative agent of intestinal infection that is more common.
As a type of intestinal infection, one can name:
- dysentery;
- salmonellosis;
- enterovirus.
At the first signs of an intestinal infection in a child, parents should not despair and become depressed. Doctors say that in 90% of cases, medical care is not needed and parents can cope with the disease on their own at home, you just need to follow the rules that will prevent dehydration.
But, in the remaining 10%, the situation is more complicated and at home you can only aggravate the situation. This requires urgent medical intervention and qualified assistance. It is worth remembering that in acute forms of intestinal infection, rapid dehydration of the body occurs and if slowed down with treatment, it can be fatal.
An ambulance should be called if:
- Bloody manifestations have been noticed in the child's vomit or stool.
- If the child cannot get water to drink (the child cannot swallow liquid or the water comes out immediately with vomit).
- The first signs of dehydration begin to appear, such as: dry skin, "dry" tongue, lack of sweat, tears, urination (the child has not gone to the toilet in the last few hours).
- In case of upset stool or vomiting, symptoms such as a sharp increase in temperature (in severe forms more than 38.5 C), lethargy, drowsiness, complete or partial refusal to eat, vomiting or diarrhea can be observed.
How can you get an intestinal infection?
The very moment of infection with an intestinal infection occurs when a bacterium or virus enters the body, namely, it settles in the gastrointestinal tract.
There are several ways to become infected with an intestinal infection:
- Through food - when eating poor-quality, contaminated food.

- By water - by bathing in contaminated water, swallowing water, or using poor-quality water at home.
- Contact-household - dirty hands and non-compliance with the rules of personal hygiene.
Treatment of intestinal infection
In the treatment of acute intestinal infection, special attention is paid to replenishing fluid in the body, as well as the use of a number of antibiotics. There is an opinion that antibiotics should be used in moderate and severe forms of the disease. Indeed, against the background of inhibition of the viability of microbes, antibiotics weaken the body's immunity, which leads to the development of dysbacteriosis, and hence the removal of all useful substances.
Prescribe antibiotics strictly after passing a series of tests, identifying the causes of the disease and monitoring by medical personnel.
Indications for prescribing therapeutic nutrition
One of the important factors in the treatment of children who have had an intestinal infection is proper nutrition or diet therapy. With improper nutrition, prolonged diarrhea, a sharp weight loss and lactose intolerance (milk is not absorbed by the body) can be seen.
With improper nutrition, prolonged diarrhea, a sharp weight loss and lactose intolerance (milk is not absorbed by the body) can be seen.
The main function of diet therapy is the ability to adjust the diet, nutrition of the child and make timely adjustments based on the form of the disease, the state of the body and the rate of recovery. Scientists have proven that even in severe forms of the disease, the gastrointestinal tract retains the function of eating and absorbing nutrients, but if food does not enter the child’s body for a long time (water-tea diets), then the body loses its recovery function, which and leads to dramatic weight loss.
Principles of nutrition in intestinal infections
The main principle of the modern approach to the nutrition of children who have had acute intestinal infections is the rejection of water-tea diets and the correct selection of products that contributed to an increase in the level of body resistance.
The type of food, the amount of servings and the amount of food consumed per day will be determined by a number of factors:
- the age of the child;
- form of the disease;
- the presence of other diseases;
- feeding form.
There are several principles that should be applied to all forms of the disease. There must be a break at night, there should not be overfeeding and force-feeding. We should not forget that in feeding you must always adhere to the regimen. In older children, the urge to vomit is associated with overeating. It is necessary to adhere to the generally accepted principle: it is better to eat more often, but in smaller portions.
If the child has a mild form of intestinal infection, without severe intoxication of the body, doctors advise to reduce the amount of food consumed in the first days, the lack of food can be filled with liquid. It can be unsweetened teas, compotes, decoctions of chamomile, purified non-carbonated water. P
P
I'm looking for a better use in pureed form (soup-puree, porridge and scrambled eggs), so it will be easier for the body to perceive it. All cooked food should be boiled or steamed. And already for 5-6 days it will be possible to return to normal life. In mild forms of diarrhea, it is recommended to reduce the volume of food by 15-20% and increase the number of meals by 1-2. By the fourth day after the onset of the disease state, the volume of food becomes the same and the diet is restored. With medium forms, it is necessary to divide meals into 5-6 approaches, the amount of food received per day is reduced by 30%. On the 6-7th day, there is a complete restoration of the volume of portions, and the number of meals.
In severe forms of intestinal infections, the patient is transferred to fractional food intake, and the daily volume is reduced by half - 45-50%. On the fourth day, the volume is gradually increased and only on the 8th day the diet is resumed.
Drinking regimen
First of all, in case of an intestinal infection, doctors try to restore the body's water balance. The patient is recommended to drink 1 teaspoon of pure water every 5 minutes. Water allows you to remove all toxins from the body. You can also drink decoctions of chamomile, compotes, teas. It is important to take liquid in small portions. Too much fluid taken at one time can cause repeated vomiting and severe dehydration. Instead of water, it is mono to give the child a solution of rehydron, a slightly sweet compote of dried fruits, non-carbonated mineral water.
The patient is recommended to drink 1 teaspoon of pure water every 5 minutes. Water allows you to remove all toxins from the body. You can also drink decoctions of chamomile, compotes, teas. It is important to take liquid in small portions. Too much fluid taken at one time can cause repeated vomiting and severe dehydration. Instead of water, it is mono to give the child a solution of rehydron, a slightly sweet compote of dried fruits, non-carbonated mineral water.
With diarrhea and vomiting, the water-salt balance of the body is disturbed. To restore it, it is recommended to drink Regidron. This drug can be purchased at a pharmacy or prepared at home. For a liter of water, you need to take 2 tbsp. spoons of sugar, 1 tbsp. a spoonful of coarse salt (fine you need to take 0.5 tablespoons) and 0.5 teaspoons of soda. It is not worth drinking such a drink in large doses, it is necessary to alternate. A teenager will need 50 ml 1 time in 1.5-2 hours, a child no more than 1 spoon at the same intervals. If there is a shortage of food, it must be supplemented with liquid.
If there is a shortage of food, it must be supplemented with liquid.
Do's and don'ts for children with intestinal infection
In case of intestinal infection, remember that all food should be steamed or boiled, in the form of puree, rarely soup, soufflé or scrambled eggs. The less often and lighter the food used, the faster it is absorbed by the body. If, after eating one portion, the patient did not eat and wants more, this is a sure sign that he is on the mend. But do not rush, but rather take care of the body. In this case, try to maintain an interval of at least 30 minutes and then offer the child another meal.
If an intestinal infection is transferred to the diet, you can use:
- Kissels from natural berries, preferably blueberries and dried fruits.
- Kashi on the water.
- Baked apples.
- Mashed potatoes.
- Vegetable puree.
Do not eat if you have an intestinal infection:
- Whole milk.

- Milk porridge.
- Dairy products: fermented baked milk, cream.
- Rye crackers and bread.
- Vegetables, fruits rich in fiber: radish, cabbage, beets, cucumbers, radishes, lettuce, grapes, apricots and plums.
- Nuts, mushrooms and legumes.
- Bakery and confectionery products.
- Salted, smoked and pickled foodstuffs.
- Carbonated drinks and water.
- Fatty varieties of poultry and meat.
- Fatty fish.
- Rich broths and soups.
The first few days the child's diet will be as scarce as possible, but on the 4th day you can gradually introduce meatballs, steam cutlets, low-fat soups, boiled or steamed fish, eggs, bananas and peeled apples. On the recommendation of a doctor, you can enter milk porridge in a ratio of 1: 1.
Later you can add bakery products: dry biscuits, biscuits, rusks from dark bread varieties, prepared by yourself. By the end of the third week, you can gradually drive rich pastries.
Peculiarities of breastfeeding in case of intestinal infection
If the child is infancy, then you should not refuse breastfeeding, but you can increase the number of attachments, if the baby needs it, switch to feeding on demand.
The only food at this age is mother's milk. After all, it is believed that children with severe diarrhea tolerate lactose in human milk more easily, so there is no need to refuse it at all. In addition, lactose retains a large amount of useful substances and those that promote growth. All of them affect the speedy recovery of the intestine.
But it should be remembered that for children who are bottle-fed, on the contrary, doctors recommend reducing the dose of the resulting mixture and increasing the number of meals (more often, but in smaller portions). But more detailed recommendations on nutrition can only be obtained from the attending pediatrician. For children who have already been introduced to complementary foods, pediatricians recommend replacing milk porridges with water ones./imgs/2020/05/20/11/3918012/61cc6c8a22744a70e207fcbe71a26590c69b0a93.jpg) May be allowed to add baked apples and dairy products to the diet. To increase the amount of pectin in the body, you can eat bananas, carrots and applesauce. You can also eat vegetable puree and mashed potatoes.
May be allowed to add baked apples and dairy products to the diet. To increase the amount of pectin in the body, you can eat bananas, carrots and applesauce. You can also eat vegetable puree and mashed potatoes.
To restore the body's water balance, rehydration is used (re-introduction of fluid into a dehydrated body).
Instead of conclusion
If you follow all the principles and recommendations for proper nutrition after suffering an intestinal infection in a short time, you can safely restore the normal functioning of the gastrointestinal tract of the child and his body as a whole. The main thing is to seek help in time and trust your doctor.
Source: ChildAge.ru Online magazine about children's health, development, psychology, upbringing and education of children
Therapeutic nutrition for acute intestinal infections in children | #02/09
Acute intestinal infections (AII) are a large group of human infectious diseases with an enteral (fecal-oral) mechanism of infection caused by pathogenic (Shigella, Salmonella, etc. ) and opportunistic bacteria (Proteus, Klebsiella, Clostridia, etc.), viruses (rota-, astro-, adeno-, caliciviruses) or protozoa (amoeba dysenteric, cryptosporidium, balantidia coli, etc.).
) and opportunistic bacteria (Proteus, Klebsiella, Clostridia, etc.), viruses (rota-, astro-, adeno-, caliciviruses) or protozoa (amoeba dysenteric, cryptosporidium, balantidia coli, etc.).
Up to now, acute intestinal infections occupy a leading place in the infectious pathology of childhood, second only to influenza and acute respiratory infections in terms of incidence. According to WHO data, up to 1-1.2 billion "diarrheal" diseases are registered annually in the world, and about 5 million children die annually from intestinal infections and their complications.
The leading component of AII therapy is a rational therapeutic diet adapted to the age of the child, the nature of the previous disease and feeding.
The goal of diet therapy is to reduce inflammatory changes in the gastrointestinal tract, normalize functional activity and digestion processes, and maximize sparing of the intestinal mucosa.
Of fundamental importance is the refusal to conduct "hungry" or "water-tea" pauses, since even with severe forms of acute intestinal infections, the digestive function of the intestine is preserved, and "hungry diets" significantly weaken the body's defenses and slow down the processes of mucosal recovery.
Basic dietary requirements for AII:
-
food should be mechanically and chemically gentle, easily digestible, varied in taste;
-
culinary processing: food is steamed, boiled, rubbed, mashed;
-
restriction in the diet of fats, carbohydrates, salt and calories;
-
the introduction of a sufficient amount of protein;
-
inclusion in diets of low- and lactose-free products and fermented milk products enriched with bifidus and lactobacilli;
-
a decrease in the volume of food in the first days of the disease by 15–20% (in severe forms up to 50%) of the physiological need;
-
eating food in a warm form (33–38 ° C) in 5–6 doses.
Stimulants of intestinal motility, foods and dishes that enhance the processes of fermentation and decay in the intestine are excluded from the diet: raw, sour berries and fruits, juices, raw vegetables, butter and vegetable oils (in pure form), sweets, fresh pastries. You should not give legumes, beets, cucumbers, sauerkraut, radishes, oranges, pears, tangerines, plums, grapes. Oatmeal is not recommended, as it enhances fermentation processes. Fatty varieties of meat and fish products (pork, lamb, goose, duck, salmon, etc.) should be excluded from the diet.
You should not give legumes, beets, cucumbers, sauerkraut, radishes, oranges, pears, tangerines, plums, grapes. Oatmeal is not recommended, as it enhances fermentation processes. Fatty varieties of meat and fish products (pork, lamb, goose, duck, salmon, etc.) should be excluded from the diet.
Whole milk in the acute period of intestinal infections should not be prescribed, as it increases intestinal motility and fermentation processes as a result of a violation of the breakdown of milk sugar (lactose), which is accompanied by increased watery diarrhea and bloating.
In the first days of the disease, black bread is also excluded, which contributes to increased intestinal motility and increased stool.
With a decrease in the manifestations of intoxication, the cessation of vomiting and an improvement in appetite, cottage cheese, meat (beef, veal, turkey, rabbit in the form of cutlets, meatballs, dumplings), low-fat fish, egg yolk and steam omelet are introduced. Thinly sliced crackers from white bread, porridges on the water (except for millet and barley), slimy soups, cereals with boiled noodles in a weak meat broth are allowed.
Thinly sliced crackers from white bread, porridges on the water (except for millet and barley), slimy soups, cereals with boiled noodles in a weak meat broth are allowed.
In the acute period of the disease, it is recommended to use lactic acid products (kefir, acidophilic mixtures, etc.). Due to the active action of lactobacilli, bifidobacteria, end products of casein proteolysis (amino acids and peptides, glutamic acid, threonine, etc.), an increased amount of vitamins B, C, etc. influence on the secretory and motor functions of the intestine, improve the absorption of nitrogen, calcium salts and fat. In addition, kefir has an antitoxic and bactericidal effect on pathogenic and opportunistic flora due to the presence of lactic acid and lactobacilli. However, long-term use of only kefir or other lactic acid mixtures is impractical, since these products are poor in proteins and fats. The curative fermented milk product is Laktofidus, a low-lactose product enriched with bifidobacteria.
When treating children with acute intestinal infections during the recovery period, it is necessary to widely use fruit and vegetable products (apples, carrots, potatoes, etc.), since they contain a large amount of pectin. Pectin is a colloid that has the ability to bind water and swell, forming a foamy mass, which, passing through the intestinal tract, adsorbs the remains of nutrients, bacteria, and toxic products. In an acidic environment, calcium is easily split off from pectin, providing an anti-inflammatory effect on the intestinal mucosa. Fruits and vegetables contain organic acids that have a bactericidal effect, as well as a large amount of vitamins, glucose, fructose, carotene, etc. The use of boiled vegetables and baked fruits already in the acute period of intestinal infections contributes to the faster disappearance of intoxication, normalization of stool and recovery.
Infant nutrition
The optimal type of nutrition for infants is mother's milk, which is prescribed fractionally up to 10 times a day (every 2 hours, 50. 0 ml). It is possible to apply the principle of "free feeding".
0 ml). It is possible to apply the principle of "free feeding".
Recently, in the clinic of intestinal infections, preference has been given to prescribing formula-fed children with low- and lactose-free mixtures (Low-lactose Nutrilon, Frisopep, Humana LP + MCT, soy mixtures). In severe forms of acute intestinal infections and the development of malnutrition, hydrolyzed mixtures (Nutrilon Pepti TSC, Nutrimigen, Alfare, Pregestimil, etc.) are widely used, which contribute to the rapid restoration of secretion and absorption processes in the intestine and the absorption of proteins, fats and carbohydrates, which prevents the development of fermentopathy in the outcome of intestinal infections (table).
According to our data, as a result of a clinical and laboratory assessment of the effect of low-lactose mixtures on the clinical picture and the state of intestinal microbiocenosis in viral diarrhea in young children, a positive effect was obtained by stimulating the functional activity of normal and, first of all, saccharolytic microflora (by stabilizing indicators of acetic, oil and propionic acids), as well as a regulatory effect on the metabolism of carbohydrates and fats in the acute period of the disease.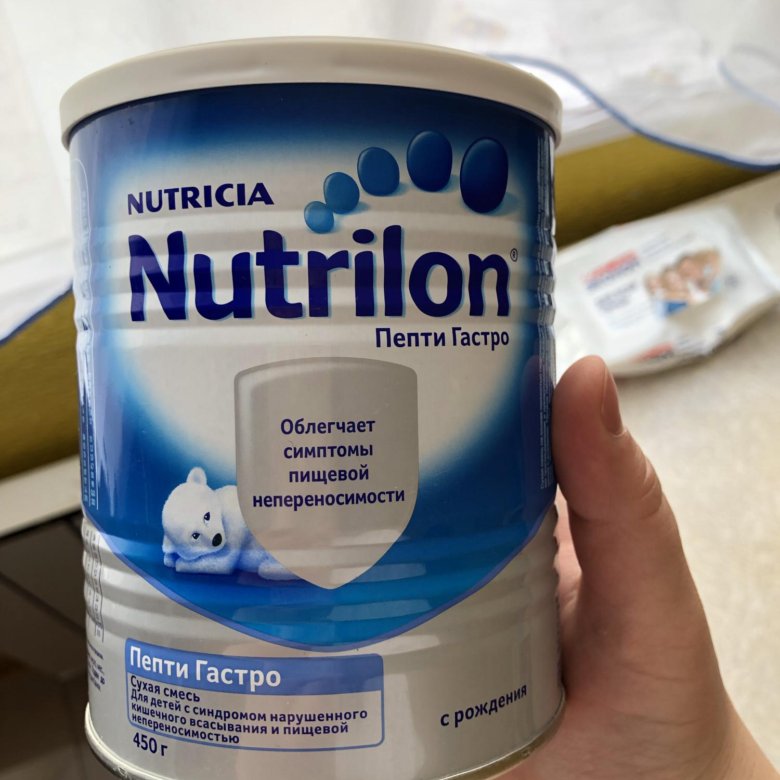 The clinical effect consisted in the rapid and persistent relief of the main manifestations of the disease: vomiting, diarrhea, abdominal syndrome and exsicosis, which, along with good tolerance, made it possible to recommend low-lactose mixtures for use as therapeutic nutrition in young children during the acute period of intestinal infections of viral etiology.
The clinical effect consisted in the rapid and persistent relief of the main manifestations of the disease: vomiting, diarrhea, abdominal syndrome and exsicosis, which, along with good tolerance, made it possible to recommend low-lactose mixtures for use as therapeutic nutrition in young children during the acute period of intestinal infections of viral etiology.
The tactics of feeding and introducing complementary foods in patients with acute intestinal infections is individual. The frequency of feeding and the amount of food per meal are determined by the age of the child, the severity of the disease, the presence and frequency of vomiting and regurgitation. It is important to consider that with 8–10 feedings (after 2 hours) with a mandatory night break of 6 hours, the child should receive 10–50 ml of food per feeding, with 8 feedings (after 2.5 hours) - 60– 80 ml, with 7-fold (after 3 hours) - 90-110 ml, with 6-fold (after 3.5 hours) - 120-160 ml, with 5-fold (after 4 hours) - 170-200 ml. The missing amount of nutrition to the physiological need for children of the first year of life should be compensated by liquid (glucose-salt solutions - Regidron, Glucosolan, etc.).
The missing amount of nutrition to the physiological need for children of the first year of life should be compensated by liquid (glucose-salt solutions - Regidron, Glucosolan, etc.).
When unloading food daily, the volume of food increases by 20-30 ml per feeding and, accordingly, the frequency of feedings changes, that is, the interval between feedings increases. With a positive dynamics of diseases and an improvement in appetite, it is necessary to bring the daily amount of food to the physiological need no later than 3-5 days from the start of treatment.
Children aged 5-6 months, with an improvement in the condition and positive dynamics from the gastrointestinal tract, are given complementary foods with porridge made from rice, semolina, buckwheat in half milk (or water in case of rotavirus infection). Porridge is prescribed in the amount of 50-100-150 g, depending on the age of the child and the method of feeding before the disease. A few days later, 10-20 g of cottage cheese made from boiled milk is added to this complementary food, and then vegetable purees, berry or fruit jelly in the amount of 50-100-150 ml, juices.
A few days later, 10-20 g of cottage cheese made from boiled milk is added to this complementary food, and then vegetable purees, berry or fruit jelly in the amount of 50-100-150 ml, juices.
The nutrition of children 7–8 months old should be more varied. When their condition improves, they are prescribed not only cereals, cottage cheese and kissels, but also vegetable purees, chicken egg yolk for 1/2 or 1/4 parts, then broths, vegetable soup and minced meat. It is allowed to add butter to cereals and vegetable puree. The yolk (the egg must be hard-boiled) can be given separately or added to porridge, vegetable puree, soup.
Nutrition for children older than a year is built on the same principle as for infants. Only a single amount of food is increased and foods recommended for healthy children of this age are included in the diet faster. In the acute period of the disease, especially in the presence of frequent vomiting, unloading in the diet should be carried out. On the first day, the child is prescribed kefir 100-150-200 ml (depending on age) after 3-3.5 hours. Then they switch to age-appropriate food, but with the exception of prohibited foods. In the acute period of the disease, all food is given in a pureed form, steam cooking of second courses is used. Cereals for cooking porridge and side dishes, vegetables are boiled until soft. The set of products should be varied and contain fermented milk mixtures, kefir, cottage cheese, cream, butter, soups, meat, fish, eggs, potatoes, fresh vegetables and fruits. You can use vegetable and fruit canned food for baby food. Foods rich in fiber and causing flatulence (legumes, beets, turnips, rye bread, cucumbers, etc.) are excluded from the diet. Watermelons, blueberries, lemons, jelly from various berries, jelly, compotes, mousses are recommended, in which it is desirable to add freshly extracted juice from cranberries, lemons.
On the first day, the child is prescribed kefir 100-150-200 ml (depending on age) after 3-3.5 hours. Then they switch to age-appropriate food, but with the exception of prohibited foods. In the acute period of the disease, all food is given in a pureed form, steam cooking of second courses is used. Cereals for cooking porridge and side dishes, vegetables are boiled until soft. The set of products should be varied and contain fermented milk mixtures, kefir, cottage cheese, cream, butter, soups, meat, fish, eggs, potatoes, fresh vegetables and fruits. You can use vegetable and fruit canned food for baby food. Foods rich in fiber and causing flatulence (legumes, beets, turnips, rye bread, cucumbers, etc.) are excluded from the diet. Watermelons, blueberries, lemons, jelly from various berries, jelly, compotes, mousses are recommended, in which it is desirable to add freshly extracted juice from cranberries, lemons.
Properly organized nutrition of a child with an intestinal infection from the first days of the disease is one of the main conditions for a smooth course of the disease and a quick recovery. Inadequate nutrition and dietary errors can worsen a child's condition, as can long-term dietary restrictions. It is important to remember that at all stages of the treatment of acute intestinal infections, it is necessary to strive for a complete physiological nutrition, taking into account the age and functional state of the child's gastrointestinal tract.
Inadequate nutrition and dietary errors can worsen a child's condition, as can long-term dietary restrictions. It is important to remember that at all stages of the treatment of acute intestinal infections, it is necessary to strive for a complete physiological nutrition, taking into account the age and functional state of the child's gastrointestinal tract.
Significant difficulties in diet therapy arise in children with the development of post-infectious fermentopathy, which develops at different stages of the disease and is characterized by impaired digestion and absorption of food due to a lack of enzymes.
With AII, especially with salmonellosis, campylobacteriosis, occurring with reactive pancreatitis, there is a violation of the absorption of fat and the appearance of steatorrhea - stools are plentiful with shine, light gray with an unpleasant odor. Diet therapy for steatorrhea is carried out with a restriction of fat in the diet, but not more than 3–4 mg / kg of body weight per day for children of the first year of life. This is achieved by replacing some of the dairy products with specialized low-fat products (Acidolact) and mixtures of foreign production, which include medium-chain triglycerides as a fat component, which practically do not need pancreatic lipase for absorption (Nutrilon Pepti TCT, Humana LP + MCT, Alfare, Pregestimil , Frisopep and others). When signs of acute pancreatitis appear, fresh fruits, berries, vegetables, concentrated fruit juices are excluded from the diet for up to 1 month.
This is achieved by replacing some of the dairy products with specialized low-fat products (Acidolact) and mixtures of foreign production, which include medium-chain triglycerides as a fat component, which practically do not need pancreatic lipase for absorption (Nutrilon Pepti TCT, Humana LP + MCT, Alfare, Pregestimil , Frisopep and others). When signs of acute pancreatitis appear, fresh fruits, berries, vegetables, concentrated fruit juices are excluded from the diet for up to 1 month.
The most common form of enzymatic deficiency in acute intestinal infections, especially with rotavirus infection, escherichiosis, cryptosporidiasis, is disaccharidase deficiency (impaired digestion of carbohydrates, primarily milk sugar - lactose). In this case, there is frequent "splashing" stools, watery with a sour smell, bloating, regurgitation and restlessness after feeding.
In case of lactase deficiency, it is recommended to use adapted low-lactose mixtures (Low-lactose Nutrilon, Frisopep, Humana LP + MCT, etc. ) or soy mixtures (Nutrilon Soya, Frisosoy, Humana SL, Similak Izomil, Enfamil Soya, etc.). In their absence - 3-day kefir; children of the first three months of life can be given a mixture of the B-kefir type, consisting of 1/3 of rice broth and 2/3 of 3-day kefir with the addition of 5% sugar (glucose, fructose), 10% porridge in water, vegetable broths.
) or soy mixtures (Nutrilon Soya, Frisosoy, Humana SL, Similak Izomil, Enfamil Soya, etc.). In their absence - 3-day kefir; children of the first three months of life can be given a mixture of the B-kefir type, consisting of 1/3 of rice broth and 2/3 of 3-day kefir with the addition of 5% sugar (glucose, fructose), 10% porridge in water, vegetable broths.
As complementary foods, these patients are given dairy-free cereals and vegetable purees in water with vegetable or butter, cottage cheese washed from whey, meat puree, and a baked apple. Schemes for the introduction of complementary foods can be individualized, attention should be paid to the early appointment of meat (daily dose of 3-4 doses). Avoid the use of sweet fruit juices, products that increase gas formation in the intestines and increase peristalsis (rye bread, white cabbage, beets and other vegetables with coarse fiber, fruit peel, prunes, dried fruits). The duration of a low-lactose diet is individual - from 1. 5–2 to 6 months.
5–2 to 6 months.
After severe intestinal infections, intolerance not only to lactose, but also to other disaccharides may occur, less often - complete carbohydrate intolerance (glucose-galactose malabsorption), in which patients have severe diarrhea, which is aggravated by the use of mixtures and products containing disaccharides, monosaccharides and starch ( dairy and soy formulas, cereals and almost all fruits and vegetables). This extremely debilitating condition, leading to dehydration and progressive malnutrition, requires a strict carbohydrate-free diet and parenteral glucose or total parenteral nutrition. In some cases, oral administration of fructose is possible. With individual tolerance, protein and fat-containing foods are preserved in the diet: lean meat - turkey, horse meat, beef, rabbit, vegetable oil, a limited range of vegetables with a low content of sucrose and glucose - cauliflower and Brussels sprouts, spinach, green beans, lettuce.
Protein deficiency occurs due to impaired utilization, absorption, or due to the loss of endogenous protein, especially in children with initial malnutrition. Correction of protein losses is carried out by prescribing hydrolyzed mixtures (Nutrilon Pepti TSC, Nutrimigen, Alfare, Pregestimil, Frisopep, etc.).
Correction of protein losses is carried out by prescribing hydrolyzed mixtures (Nutrilon Pepti TSC, Nutrimigen, Alfare, Pregestimil, Frisopep, etc.).
With prolonged post-infectious diarrhea, especially in children who received repeated courses of antibacterial drugs, a secondary food allergy may develop, accompanied by sensitization to cow's milk proteins, less often to egg protein, cereal proteins. Such disorders can occur not only in children with allergic diathesis, but also in patients without aggravated premorbid background. Clinically, post-infectious food allergy is manifested by hypersensitivity to previously well-tolerated products - milk mixtures, milk porridge, cottage cheese, etc. Children have abdominal pain, bloating after feeding, regurgitation, loose stools with cloudy vitreous mucus, sometimes with streaks of blood, during a coprological examination eosinophils are found in the feces. It is characteristic to stop weight gain, up to the development of malnutrition.
When an allergy to cow's milk proteins is detected in the nutrition of children of the first year of life, soy-based mixtures are used (Nutrilak Soya, Nutrilon Soya, Frisosoy, Humana SL, Enfamil Soya, etc.) and based on protein hydrolysates (Nutrilon Pepti TSC, Nutrimigen, Pregestimil, Frisopep and others).
The lack of specialized products is not an insurmountable obstacle to the organization of a dairy-free diet. The elimination diet in this case is based on dairy-free pureed cereals (rice, buckwheat, corn), fruit and vegetable purees, potatoes, zucchini, cauliflower, pumpkin, baked apple, banana, vegetable and butter, meat puree. In this case, it is necessary to take into account the physiological needs of the child for basic nutrients and energy. Meat puree, as the main source of protein, in the absence of specialized mixtures, can be prescribed from 2–3 months of age. It is preferable to use horse meat, rabbit meat, poultry, lean pork, as well as dietary canned meat - the Little Humpbacked Horse, Cheburashka, Petushok, Pork Puree, etc.