Formula feeds for preterm babies
A Guide to Premature Baby Feeding and Preemie Nutrition
A Guide to Premature Baby Feeding and Preemie Nutrition
When it comes to premature baby feeding, you may have questions. Whether you're breastfeeding or formula feeding, learn more about preemie baby nutrition and your baby's feeding schedule.
Premature baby feeding
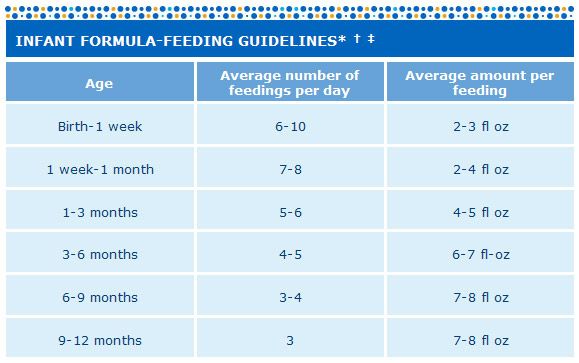
- Premature babies need to eat at least every three hours. Tiny babies have tiny tummies. This means they’ll have to eat a lot of small meals for them to gain weight.
- Your baby will eat at their own pace. While they may be eating every three hours, the premature baby feeding process is often slow. You'll soon recognize their pattern of swallowing and breathing. Babies who eat slowly seem to take more milk at each feeding and may be satisfied and sleep longer between feedings.
- Their mouths are often extra-sensitive. If your baby has spent their first few days with tubes and respirators in their mouth, they may assume that anything that goes into their mouth is painful, which could include a breast or a bottle.
- Premature babies are slow to feed. Feeding them too fast by mouth may result in a feeding aversion or spitting up. They are also likely to have more digestive issues than a full-term baby, since their digestive system may not be as mature as a full-term baby's.
Try these premature baby feeding tips
- Each baby is unique. Follow the advice of your baby's doctor.
- Introduce your baby to a nipple. Even if they are still feeding by tube, this will help them adjust to bottle-feeding when they’re ready. You may need to try different nipples at first.
- Stick to breast milk or one type of formula and nipple to help them adjust.
- Keep a record of your baby's feedings.
- Get growth charts, specially designed for premature babies, from your baby's doctor to help monitor their progress.
- Keep your baby on a fairly regular schedule of awake and nap time, to help them eat better.
- Make sure your baby is fully awake before feeding.

- Don't force your baby to eat. If they’re not sucking as fast, sealing their lips or turning away, they may be full.
- Feed them on demand, not a schedule. Studies have shown that premature babies grew at a faster pace when fed on demand.
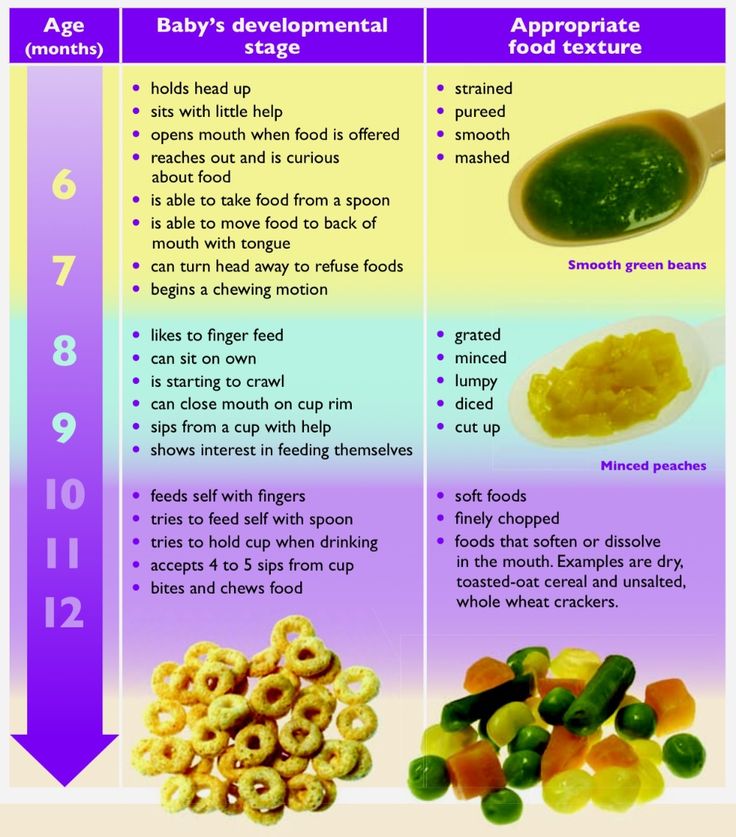
- When your baby is developmentally ready, slowly introduce solid foods while they are still on formula.
- Enlist the help and support of family and friends, to give yourself a break.
Preemie Nutrition
Most premature babies have low birth weight.
If a baby is too premature to breastfeed, moms are encouraged to pump their milk, as breast milk is considered to be best for the baby. Sometimes, doctors will recommend using a breast milk fortifier, to help give your baby the extra protein, vitamins, calcium and other nutrients they need at this early stage.
If you can't pump or breastfeed, or choose not to, ask your baby’s doctor about the specially designed formulas available for premature or low birth weight babies.
Premature babies may have more digestive issues than full-term babies.
Chances are, your baby’s feeding skills haven't fully developed yet. This means they’ll likely be slow to feed, or they may feed too fast and spit up or develop a feeding aversion. But there are some things you can try to help:
- Introduce your baby to a pacifier. This can help get them used to the feeling of bottle-feeding for when they’re ready to switch over from the tube.
- Record their feedings, so you can keep track of spit ups and how much they’re keeping down.
- Monitor your preemie’s progress with growth charts from the doctor.
- Try to keep them on a sleep schedule.
- Make sure they are fully awake before feeding
- Be aware of indicators, so you know when your little one is full or tired.
- Slowly introduce solids when they are developmentally ready.
Babies who are born premature often undergo developmental testing and programs.

If your baby weighs less than 3.5 lbs. at birth, they will most likely be referred for formal developmental testing around their 1st and 2nd birthdays. If your baby is born prematurely, your doctor may recommend an infant stimulation program. This usually involves working with a physical therapist or specialized healthcare professional to learn gentle exercises, positioning and other ways to interact with your premature baby and help them with physical development. Early intervention programs can help with social and functional skills and provide support for the family.
Preterm babies have a harder time maintaining the proper water balance in their bodies. These babies can become dehydrated or over-hydrated. This is especially true for very premature infants. Keep the following preemie nutrition facts in mind as you navigate feeding your baby:
- Premature babies may experience more water loss through the skin or respiratory tract than babies born at full term.
- The kidneys in premature babies have not grown enough to control water levels in the body.
- The NICU team keeps track of how much premature babies urinate (by weighing their diapers) to make sure that their fluid intake and urine output are balanced.
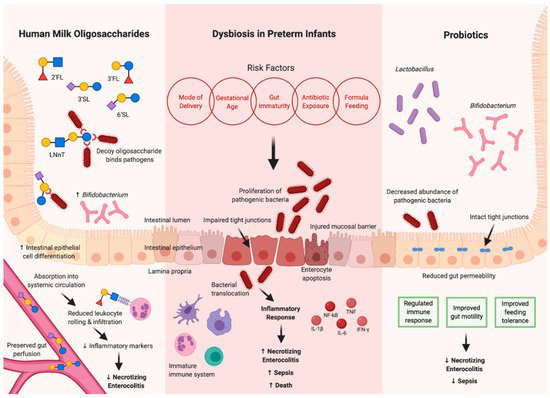
- Human milk from the baby's own mother is the best for babies born early and at very low birth weight.
- Human milk can help babies avoid infections and sudden infant death syndrome (SIDS) as well as necrotizing enterocolitis (NEC).
- Many NICUs will give donor milk from a milk bank to high-risk babies who are not able to get adequate amounts of milk from their own mother.
- Special preemie formulas can also be used. These formulas have more added calcium and protein to meet the special growth needs of premature babies.
- Older premature babies (34 to 36 weeks gestation) may be switched to regular formula or a transitional formula.

- Babies who are given breast milk may need a supplement called human milk fortifier mixed into their feedings. This gives them extra protein, calories, iron, calcium, and vitamins. Babies fed formula may need to take supplements of certain nutrients, such as vitamins A, C, and D, and folic acid.
- Some infants will need to continue taking nutritional supplements after they leave the hospital. For breastfeeding infants, this may mean a bottle or two of fortified breast milk per day as well as iron and vitamin D supplements. Some babies will need more supplementation than others. This may include babies who are not able to consume adequate amounts of milk through breastfeeding to get the calories they need to grow well.
- After each feeding, babies should seem satisfied. They should have 8 to 10 feedings and at least 6 to 8 wet diapers each day. Watery or bloody stools or regular vomiting could indicate an issue and you should discuss them with your doctor.
Preemie Weight Gain
Weight gain is monitored closely for all babies. Research suggests developmental delays could be associated with premature babies who experience slow growth.
- In the NICU, babies are weighed every day.
- It is normal for babies to lose weight in the first few days of life. Most of this loss is water weight.
- Most premature infants should start gaining weight within a few days of birth.
- The desired weight gain depends on the baby's size and gestational age. Sicker babies may need to be given more calories to grow at the desired rate.
- It might be as little as 5 grams a day for a tiny baby at 24 weeks, or 20 to 30 grams a day for a larger baby at 33 or more weeks.
- In general, a baby should gain about a quarter of an ounce each day for every pound (about 1/2 kilogram) they weigh. (This is equal to 15 grams per kilogram per day. It is the average rate at which a fetus grows during the third trimester).
If you are experiencing difficulty affording specialty premature formulas for your baby, financial assistance is available.
Enfamil has developed a program called Helping Hand for Special Kids, to help families who need specialty formulas for their premature baby but have difficulty affording them. Depending on your needs, the Helping Hand program provides either long-term assistance or a free, one-time shipment of products. To us, all babies deserve the very best start in life. Ask your doctor if you qualify for this program.
You may also like
How to Feed Preemie Babies
Feeding Your Premature Baby
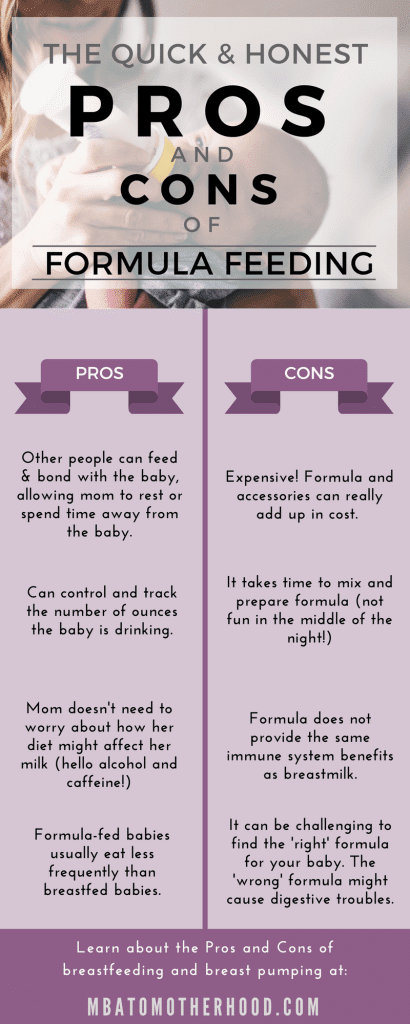
Whether you choose to breastfeed or formula feed, meal time is an important opportunity for bonding with your baby. Here are a few tips to help you both have a successful experience.
If you choose to formula feed, ask your baby's doctor which formula is appropriate for your baby.
If you choose to breastfeed, ask your baby's doctor if supplements and vitamins are appropriate for your baby.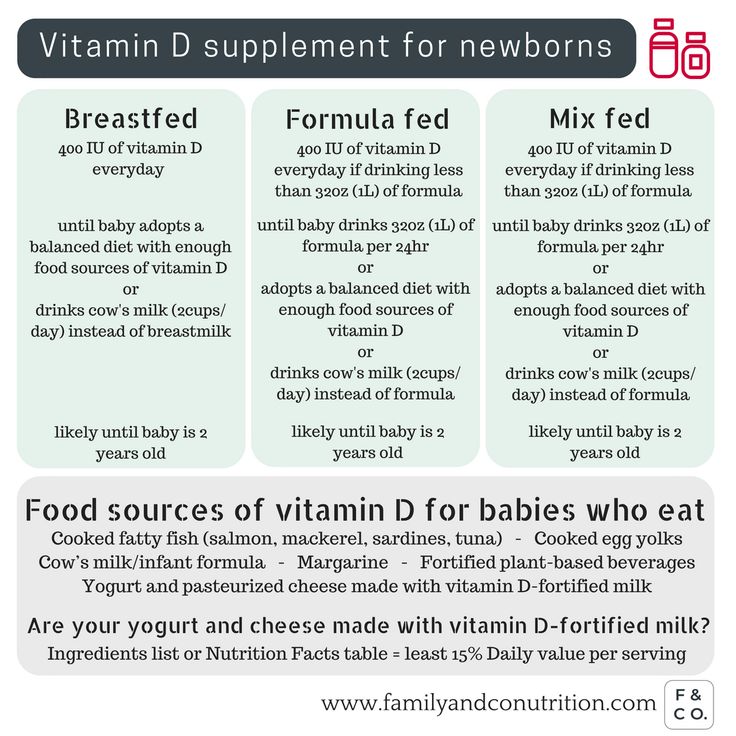
In This Article
About Formula | Preparing Bottles | Feeding Your Baby | How to Tell if Your Baby's Getting Enough to Eat | What You Can Learn From Her Diaper
About Formula
Ready-to-use and Concentrated Liquid infant formulas are commercially sterile in the sealed container.
Powdered infant formulas are not sterile and should not be fed to premature infants or infants who might have immune problems, unless directed and supervised by your baby's doctor.
Remember that improper hygiene, preparation, dilution, use or storage may result in severe harm.
Ask your baby's doctor which formula is appropriate for your baby.
» Return to top
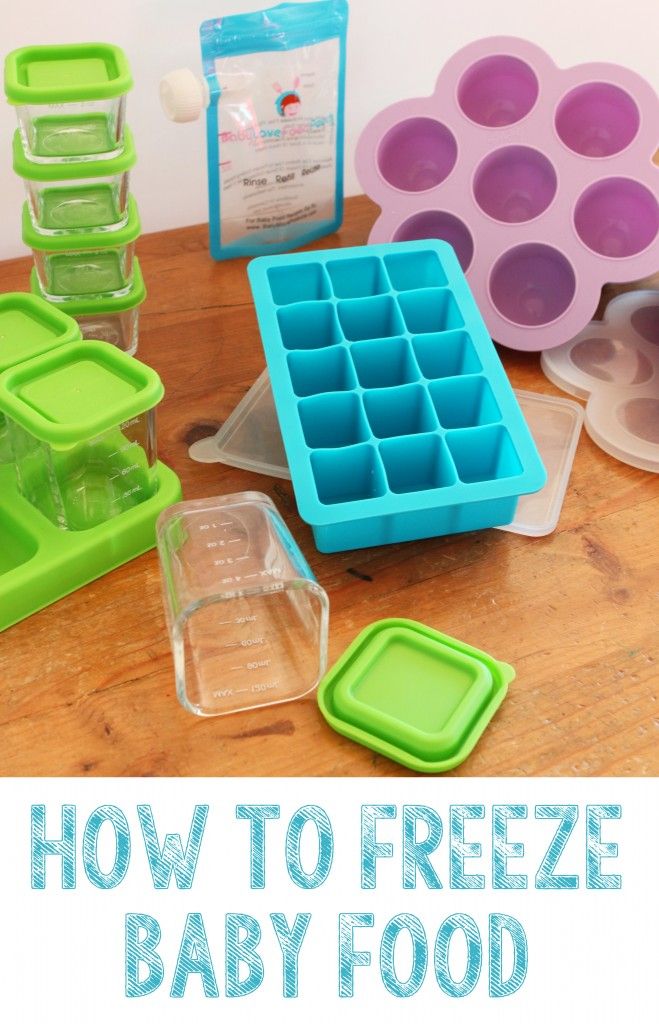
Preparing Bottles
- Wash everything—bottles, nipples, and caps—in hot, soapy water before using.
- Check with your baby's doctor about the need to use cooled, boiled water for mixing and the need to boil clean utensils, bottles, and nipples in water before use.
- To prepare your baby's formula, make sure you follow the label directions.

- Once prepared, infant formula can spoil quickly.
- After opening, containers of liquid formula need to be fed immediately or covered and refrigerated and used within 48 hours.
- Formula prepared from powder needs to be fed immediately or covered and refrigerated and used within 24 hours (check product label for specific guidelines).
- Most babies don't seem to mind whether their bottle is warmed or straight out of the refrigerator. Some may prefer a consistent temperature from one feeding to the next.
- If you want to warm a bottle that has been in the refrigerator, run warm tap water over the bottle or place the bottle in a pan of hot (not boiling) water. Take care that the cap and nipple do not get wet.
- Shake the bottle occasionally while warming. The warming time should be less than 15 minutes.
- Test the formula temperature before feeding; it should not feel warm or cold when dropped on your hand—neutral is close to body temperature (about 100°F).
 Warmed formula should be discarded within one hour.
Warmed formula should be discarded within one hour. - Discard formula remaining in the bottle within one hour after feeding begins.
WARNING: Never warm formula in a microwave. Serious burns can result.
» Return to top
Feeding Your Baby
Whether you're breastfeeding or bottle-feeding your baby, use these guidelines as you learn more about your baby's feeding schedule:
- Support your baby's head during feedings, keeping it higher than her stomach. This aids in digestion and helps avoid ear infections.
- Your baby will eat at her own pace. You'll soon recognize her pattern of swallowing and breathing. Babies who eat slowly seem to take more milk at each feeding and may be satisfied and sleep longer between feedings.
- If your baby ever seems to have trouble catching her breath while eating, or is coughing, choking, or sputtering, sit her up until she seems ready to eat again.
- Keep feedings relaxed, with as few interruptions as possible.

- Keep your baby from swallowing air by keeping the bottle nipple full of formula. She shouldn't suck on an empty bottle or drain the bottle.
- When your baby is finished eating, the nipple will fall out of her mouth and her whole body will become relaxed. Your baby will probably need about 20 to 30 minutes to finish her bottle.
- If she seems finished after only 15 or 20 minutes, you may want to wake her and try to get her to eat for a little longer. If possible, you want her to feel full enough to be satisfied for another few hours.
Feeding Tips
- It's important to hold the bottle at a 45-degree angle so your baby can get the right suction.
- Your baby may need to eat on demand—or may feed well on a newborn schedule. A breastfed baby usually has 8 to 12 feedings in 24 hours, while a bottle-fed baby may have 8 to 10 feedings during that time. Whatever feeding method you choose, your baby will need small, frequent feedings around the clock.
- You may need to wake your baby every three hours or so if she's sleeping through a feeding. Wake your baby gently by removing her blanket or stroking her arms and legs. Don't rush her or she may be too upset to eat.
- Once she's wide awake, hold her, and touch your nipple, or the bottle nipple, to her cheek or lip. She'll be encouraged to open her mouth and turn toward it to eat.
- If your baby takes less than 15 minutes to eat, you may want to use a nipple with a smaller hole. If she takes longer than normal and doesn't seem to be sucking actively, make sure the nipple hole isn't clogged.
» Return to top
How To Tell If Your Baby's Getting Enough To Eat
- The best way to tell if your baby's getting enough to eat is to check her growth. She should be gaining about an ounce a day during the first few weeks home from the hospital.
- During the first few months, her doctor will carefully watch her weight gain to make sure it's increasing steadily.
 Also, if your baby has six or more wet diapers a day and seems happy between feedings, she's probably getting plenty to eat.
Also, if your baby has six or more wet diapers a day and seems happy between feedings, she's probably getting plenty to eat. - Your baby may give you signs when she's had enough to eat. She may fall asleep or close her mouth and turn away from her bottle. She may also bite or play with the bottle nipple, or even fuss if you keep trying to feed her. Follow your baby's lead.
If you're worried that your baby isn't eating like she should, talk with the pediatrician. If you notice any of these signs, take your baby to the doctor:
- Constant or inconsolable crying
- You cannot wake your baby
- Consistent feeding refusals
- Persistent coughing, choking, or breathing problems
- Noticeably fewer wet or soiled diapers
» Return to top
What You Can Learn From Her Diaper
Breastfed babies usually have softer, yellow stools. Formula-fed babies usually have yellow, brown, or green stools. Occasional changes in the color and consistency of stools are normal.
» Return to top
You may also like
Premature and Small Birth Formulas: The Best Milk Formulas for Weight Gain
09/23/2019 Reading time: 3.5 min 56261
Contents of the article
- Premature babies - who are they?
- What is the best formula for premature babies?
- What should be in the pre-blend?
- How long should the pre-mix be used?
Premature babies - who are they?
Premature is considered to be children who, for some reason, were born prematurely - before the 38th week of pregnancy (with a period of less than 37 full weeks).
What is the best formula for premature babies?
For newborns born before the planned date of birth, breast milk is definitely the best food. The milk of a mother who gave birth to a baby earlier than expected is energetically more valuable and nutritious, it has a higher content of proteins, fats and protective immune substances. Unfortunately, a woman who has given birth to a child prematurely cannot always fully provide the baby with breast milk, and sometimes milk does not come at all.
To solve this problem, specialized milk formulas for premature babies have been developed. Such mixtures can be recognized by the presence of the word "PRE" in the title. All milk PRE-mixes are distinguished by a higher nutritional and energy value. Infant formula for premature babies contains more proteins, fats and other important nutritional nutrients that an immature baby needs. Also in these mixtures, the amount of lactose is reduced to avoid additional burden on the child's digestion.
What should be in the pre-mix?
Infant formula for premature babies should contain an increased amount of the main food ingredients: proteins, fats, the energy value of the pre-mixture is higher. When choosing a mixture, pay attention to the presence of certain components in the composition:
- Omega-6 and omega-3 - essential fatty acids for the development of the child's intelligence and brain
- Nucleotides - are necessary for the proper formation of immunity and digestion
- Inositol - promotes lung development
- Choline - needed to improve the functioning of the cells of the brain and nervous system
- MCT (medium chain triglycerides) - fatty component in a special, easily digestible form
- L-carnitine- improves fat absorption
How long should I use the pre-mix?
Feeding with a special PRE-mixture should be continued until the baby reaches a weight of 3000 g, after which the child is gradually transferred to the usual adapted infant formula.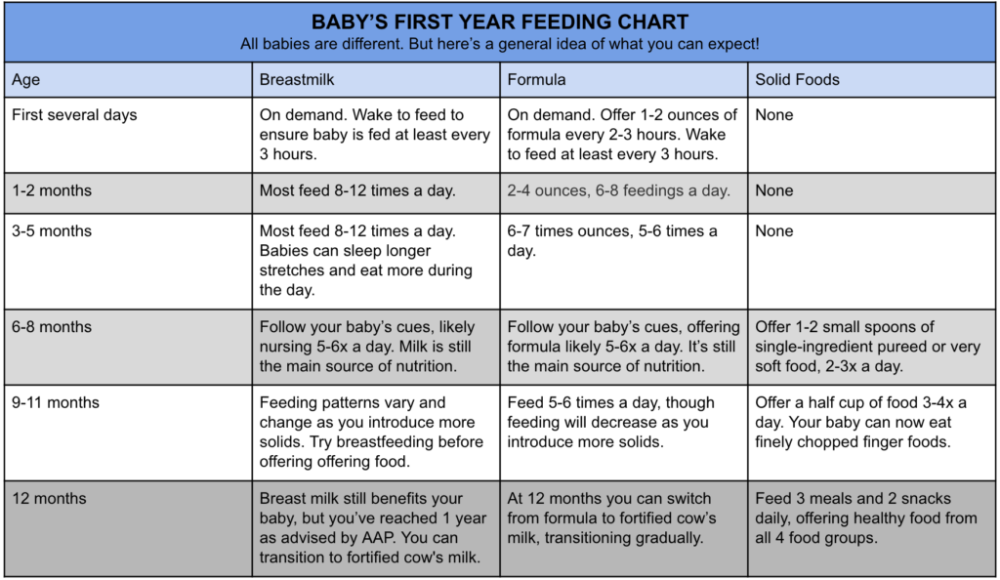
If necessary and according to the indications of a doctor, infant formula for premature babies can remain in the baby's diet for several months in the amount of 1-2 feedings.
Premature and LBW Formulas: Milk Formulas for Weight Gain - Baby Food for PrematurityWhat does Nutrilak offer?
Nutrilak Premium PRE - Premature Infant Formula is formulated to meet all the needs of preterm babies.
This is the only formula for premature babies that contains milk fat. The presence of this important component brings composition 9 as close as possible0039 Nutrilak Premium PRE for breast milk. Milk fat contains important nutrients necessary for the formation of the brain, and is also a source of energy for the speedy growth of premature babies. Nutrilak Premium PRE contains all the components necessary for a premature baby: MCT (medium chain triglycerides), high levels of inositol and choline, nucleotides, essential omega-3 and 6 fatty acids, prebiotics.
Powdered milk formula Nutrilak Premium PRE was created jointly with the Scientific Center for Children's Health of the Ministry of Health of the Russian Federation.
(14 ratings; article rating 3.0)
Formulas for premature babies in the category "Products for children"
PreNAN Powdered milk formula for premature and small babies from birth, 400 g
in warehouse
Delivery in Ukraine
420 UAH
Buy
Smartik
Military Children's Children's Friso Premature Special for premature and small -scale children 400 g 900 Gr
900 9000YouBuyMore
Nestogen 2 powdered milk formula for babies from 6 to 12 months, 1000 g
In stock
Delivery across Ukraine
372.21 UAH
Buy
Giraffe Children's food store
Dry Milk mixture Nutrilon 1 Premium+ for children from birth, 1000 g
in warehouse
Delivery in Ukraine
508 UAH
Giraffe
9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000in warehouse
Delivery in Ukraine
305 UAH
Buy
Giraffe Baby Store
Dry Milk mixture Nutrilon 4 Premium+ for children from 18 months, 600 g
at warehouse
9000 332 332 332 332 332 332 332 332 332 332 332 332 332 332 uahBuy
GIRAFFA baby food store
Natures Plus, Animal Parade, Kid Greenz, Mix of vegetables for children, 90 tablets
In stock in Bila Tserkva
Delivery across Ukraine
490 UAH
Buy
beOrganic
Bioray, Kids, NDF Tummy, probiotic mix with 11 strains, for children, raspberry, 2 fl. UN
UN
in warehouse
Delivery in Ukraine
1 020 UAH
Buy
olgabiomed
Nan 1 sour -milk mixture for children from birth, 400 g
at warehouse
9000 278 GRNBuy
Smartik
NAN SUPREME Powdered formula 3 800g with oligosaccharides for feeding children from birth.
in warehouse
Delivery in Ukraine
990 UAH
Buy
Smartik
NAN Hypoallergenic 2 Optipro®ha Dry mix for children from 6 months, 800 g
at warehouse
9000 9000 689 UAHBuy
Smartik
NAN Powdered lactose-free formula for children from birth, 400 g
in warehouse
Delivery in Ukraine
322 UAH
Buy
Smartik
mixture for children Hero Baby 1, 700 grams (KG-5248)
in Ukraine
9000 220 GRN UA 198 UAHBuy
Nono.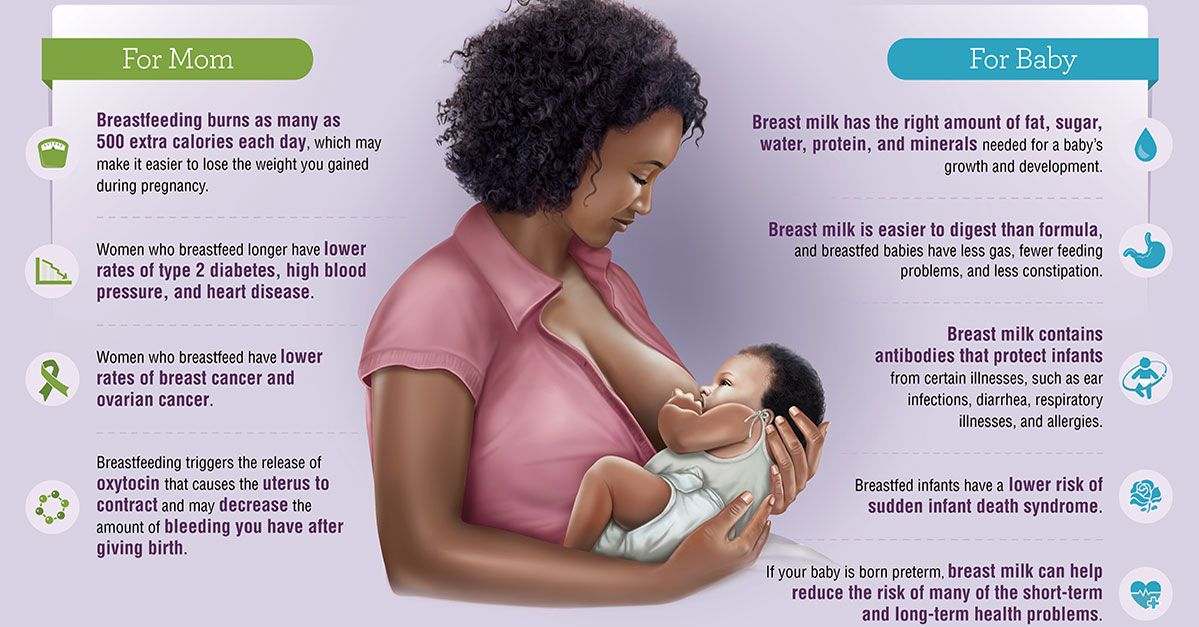 in.ua Buy profitable
in.ua Buy profitable
Children's Military mixture Nutriben Innova 1, 800 grams (KG-4856)
in warehouse
Delivery
9000 350 GRN UAH 915 UAH 915 UAH 915 UAH 915 UAH 915 UAH 915 UAH 9150010Buy now
Nono.in.ua Buy cheap
See also
NaturesPlus Source of Life Animal Parade Kid Greenz mixture of green vegetables and algae vitamins for children. 90 t
In stock
Delivery across Ukraine
500 hryvnia
Buy
VITAMINKA - Online store of vitamins, products for health and beauty
stock
Delivery within Ukraine
278.88 UAH
245.41 UAH
Buy
Giraffe Children's Power Store
Gerber, LIL BRAINIS, Three Omega of Freedy Acids and DGK, Multivotitic Supply, Kyiv
It ends
Delivery for Ukraine. 0010
332 UAH
Buy
Giraffe Children's food store
Kyolic, a mixture of probiotics for children, with the taste of vanilla, 60 chewing tablets WAK-60132
It ends
9000 9000 9000 57 GrN Buy⭐FRESH⭐-natural products and cosmetics
Lactorrin - nutrition for premature babies with low birth weight, 12 sachets
Delivery in Ukraine
324 - 362 UAH
from 2 sellers
362 UAH
Buy
Kolos.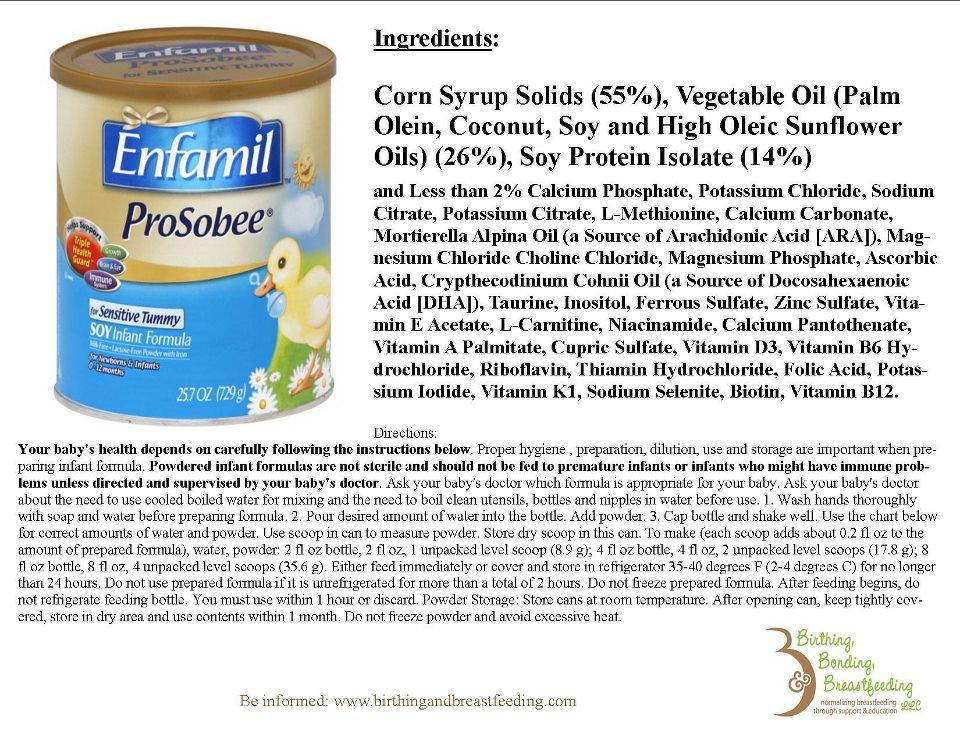 net.ua
net.ua
Mixture for children, 1 liter
Delivery
196 UAH/l
Buy
9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 V-DECOREKyolic, Children's Probiotic Blend, Vanilla, 60 Chewables WAK-60132, Original
Delivery from Kyiv0002 Dry formula for children at risk of developing food allergies "Friso HA 1" for children from 0 to 6 months, 400 gr.
Delivery from Brovary
270 UAH
Buy
Youbuymore
Dry mixture for children FRISO HA 1 from 0 to 6 months, 400 gr
Delivery from Brovary
270 GRN
9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9 YouBuyMoreExtension for a mixer for children, yellow-blue 58370001 TE, CODE: 5559479
Delivery in Ukraine
115 UAH
78.98 UAH
Buy
Internet Catalog of Discounts Techno
Dityach - Sumy for Dythechy Kimnat
in warehouse
9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 9000 Extension for a mixer for children, yellow-blue 58370001 GR, CODE: 5559479
Delivery in Ukraine
115 UAH
78.