Introducing food to breastfed babies
Starting Solid Food - La Leche League GB
Human milk is the perfect first food
Introducing your baby to other foods is a big milestone, and can be fun too. The simplest approach is to continue your usual breastfeeding pattern and let your baby join you at family mealtimes. Your baby will be able to learn about new foods gradually and in their own time.
Signs of readiness for complementary foods
Babies begin eating solid foods according to their own unique timetables, just as they will walk and talk when they are ready. Readiness to try new foods is just another developmental step and it isn’t necessary to do anything special.
Babies show signs of readiness for complementary foods (to complement their milk intake) around the middle of the first year.
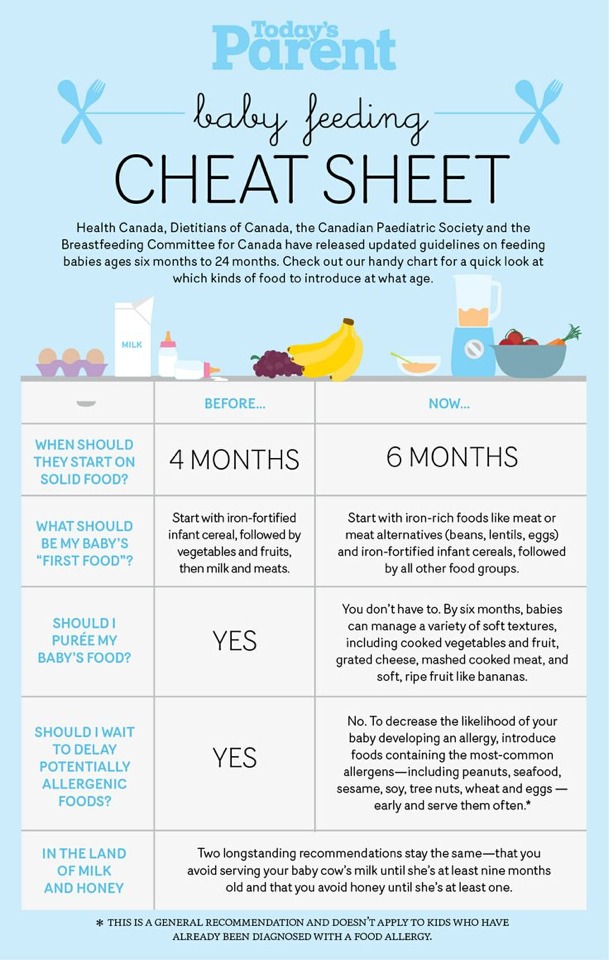
Although previous research suggested that signs of readiness for starting solids were related to developmental changes which happen at around 4 months, recent research indicates the following signs of readiness:1
Fact: Ability to sit up well when supported
Once your baby can sit up well when supported (for at least a few minutes) let them join you at family mealtimes and allow them to pick up food.
Fact: Loss of the tongue thrust reflex
Babies who have not yet lost their tongue thrust reflex will push food out of their mouth with their tongue. The tongue thrust reflex is a sign that they are not developmentally ready for solid food.
Fact: Ability to pick up food, put it in their mouth and chew
A baby who is able to reach out and grab a piece of food, then bring it to their mouth and chew it is generally ready for solids. Research indicates that the ideal time to start solid food in terms of oral-motor developmental readiness is between six and eight months. As with other developmental stages, babies learn to chew when they are ready, not because solid food has been introduced by six months.
Myth: Breastfeeding more often
Your baby may ask to breastfeed more, yet still not be ready for solid food. They may just be unwell, having a growth spurt, teething, or reacting to stress. Offering your baby both breasts during each feed may be all that is needed.
Myth: Waking at night
Waking at night is normal and common behaviour and is not a sign that a baby is ready to start other foods even if they have previously slept for longer periods.
Myth: Watching you eat
Babies are interested in and want to copy what they see around them, so watching others eat does not necessarily mean they are ready to start eating solid foods.
Why follow your baby’s cues?
Human milk is the most important food in your baby’s diet during their first year, providing them with most of the calories and fluids they need, as well as a wide range of nutrients. Allowing solids to replace breastmilk too quickly may lead to undernutrition, imbalance of nutrients, or poor weight gain. Breastfeeding continues to be a valuable source of nutrition and calories if your baby is unwell or teething, and doesn’t want to eat solid food.
Breastfeeding provides your baby with antibodies, other immune factors, stem cells, and many other components unique to breastmilk.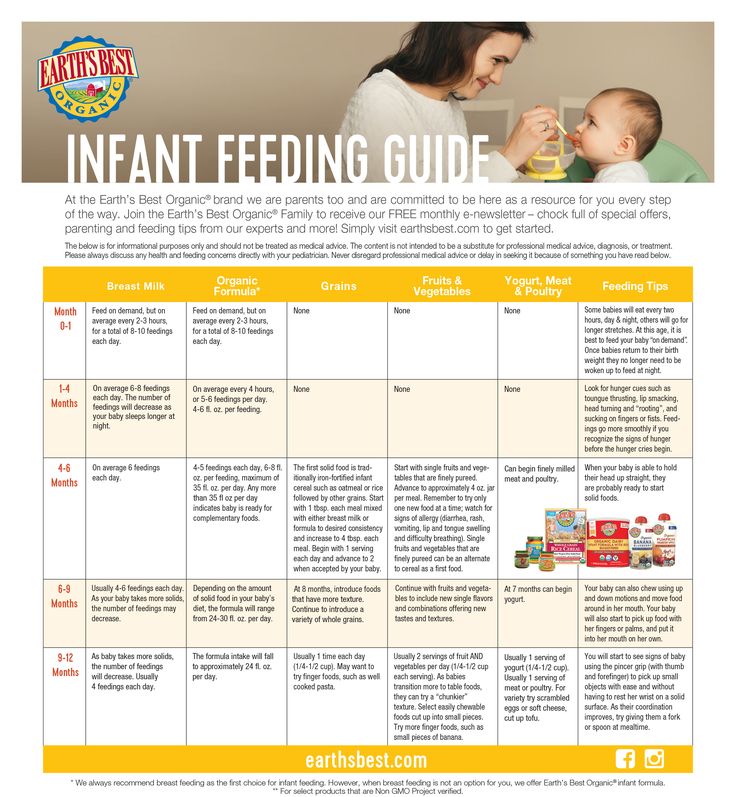 Breastfeeding alongside introducing solids helps to prevent harmful bacteria, such as E.coli, growing in your baby’s gut. Replacing your milk with solid food too early reduces the level of protection they receive.
Breastfeeding alongside introducing solids helps to prevent harmful bacteria, such as E.coli, growing in your baby’s gut. Replacing your milk with solid food too early reduces the level of protection they receive.
Developmental readiness inside and out
Your baby’s digestive system gradually matures during the first six months. Introducing solids when your baby is developmentally ready means they will be able to eat and digest these new foods.
Preterm babies, babies with special needs or developmental delay may not be ready for solids until later than six months. Following their readiness signs will help you know when to offer solids. Speak to your baby’s healthcare team regarding their individual nutritional needs.
Carry on breastfeeding
Starting solid food is a new experience for your baby and is about taste, texture and learning new skills, not about replacing your milk. Babies are more likely to try something new if they aren’t too hungry – they may refuse solids when they really want to breastfeed.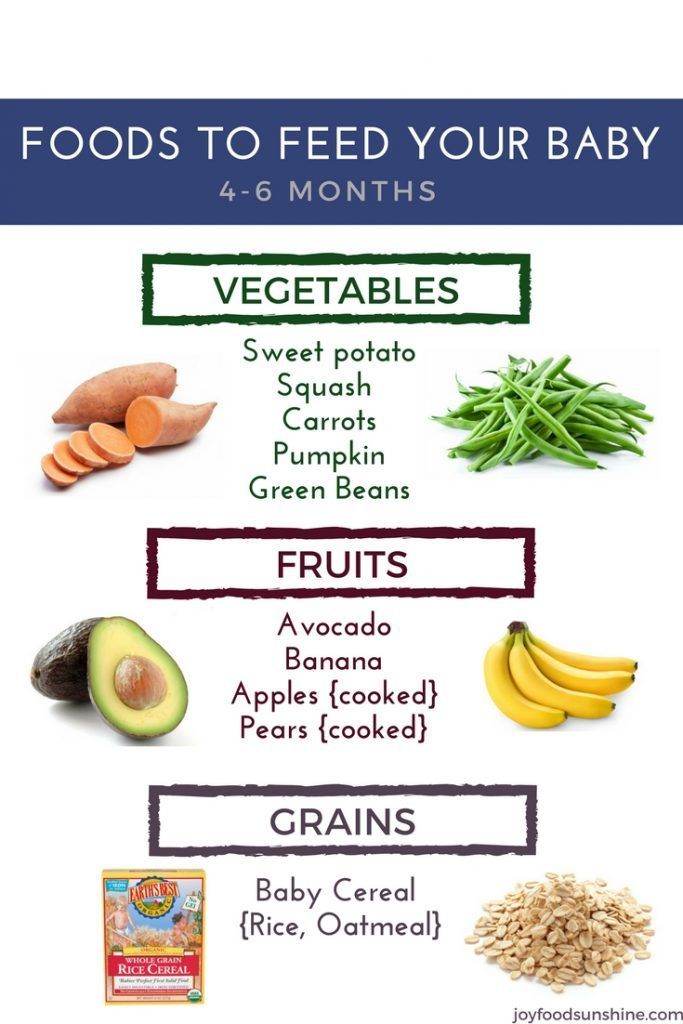 Remember that your baby isn’t likely to eat very much to start with.
Remember that your baby isn’t likely to eat very much to start with.
You may feel pressured into limiting breastfeeds so that your baby will take more solid food, but this can have the opposite effect. If your baby is happy and content after a breastfeed they may be more open to the idea of trying some new foods.
Breastmilk gradually and gently introduces babies to the foods their mother eats because traces of those appear in her milk. This provides a variety of flavour experiences in a natural way, helping prepare the baby for the foods they will eat at the family table. Babies will want to eat whatever food is on the table, so this is a good opportunity to review the whole family’s diet.
First tastes
Baby–led weaning
The principle behind baby-led weaning is that babies will instinctively start to feed themselves when they are developmentally ready, given the opportunity. The skills to feed themselves and readiness of their body to process food occur naturally and do not need to be taught.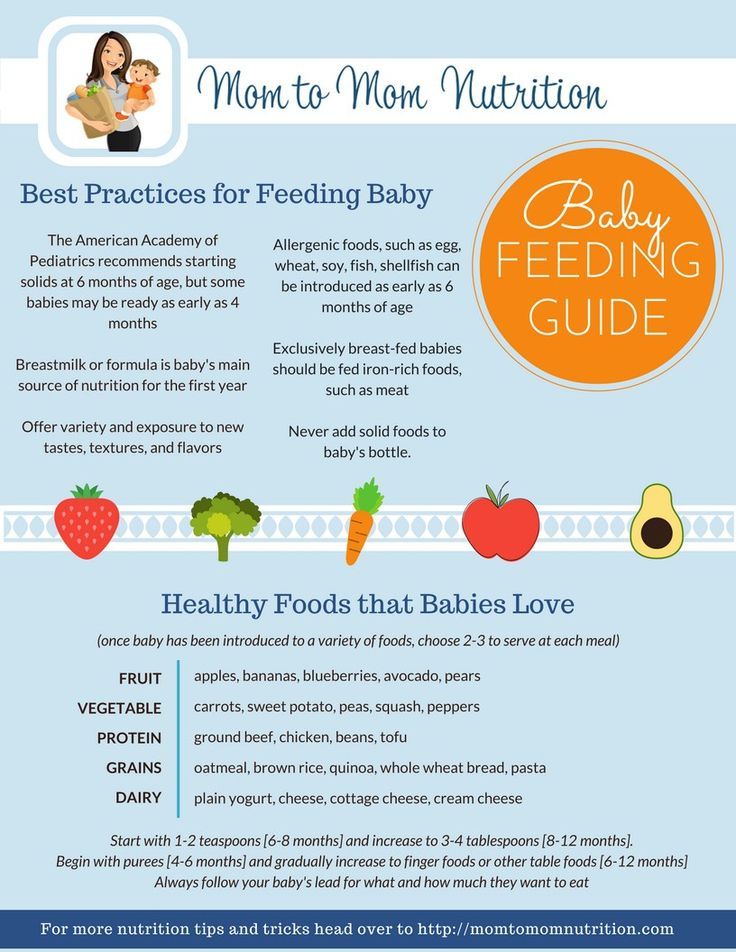
Babies who are in control of feeding themselves (in contrast with spoon feeding) will only be able to pick up food, put it in their mouth and chew it when they are developmentally ready. This approach also lets babies determine which foods and how much they want to eat: they will naturally progress at their own pace and reduce breastfeeds when they are ready.
Allowing babies to join in with family mealtimes will expose them to a wide variety of different foods, enable them to copy how other children and adults eat, and help make eating a pleasant experience, encouraging a positive lifelong relationship with food. A baby who is allowed free choice of good, nutritious foods tends to balance their own diet.
For more information on baby-led weaning, see book Baby-led Weaning: The Essential Guide (2019).
How to present food – shapes and sizes
Babies love to use their hands, so offer foods that they can easily hold and put into their mouth. Until they have developed a pincer grip, babies can’t pick up small pieces of food.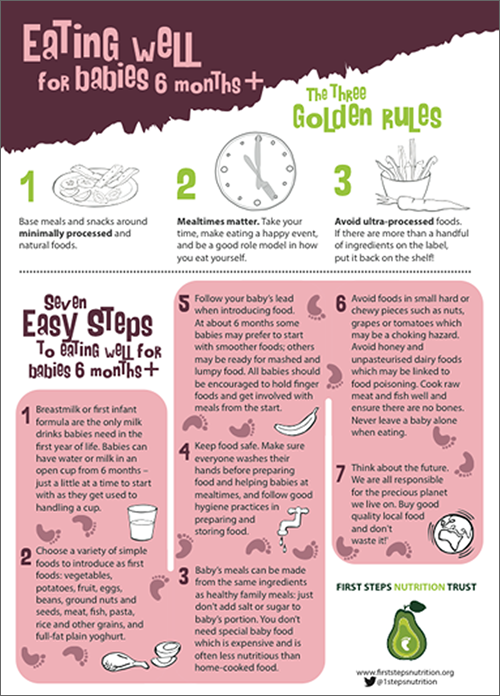 Offer sticks or pieces of food the shape/size of an adult’s finger. Most 6-month-old babies will be able to pick up the piece, hold it in their fist and gnaw the end sticking out of their fist.
Offer sticks or pieces of food the shape/size of an adult’s finger. Most 6-month-old babies will be able to pick up the piece, hold it in their fist and gnaw the end sticking out of their fist.
Softer foods can be spread on unsalted oat cakes, rice cakes or crackers, or dipped into with a suitable piece of food so your baby can manage by themselves. For tastes of soup, yoghurt or porridge, offer your baby a spoon with a small amount of food on, or let them dip their fingers in and lick off the food.
Different tastes and textures
It is important to offer your baby a wide variety of different foods as this will expose them to a range of tastes and textures. The ability to explore the different taste, texture,colour and smell of food may help babies to have a healthier relationship with food.
Aim to offer tastes of a wide variety of foods in as close to their natural state as possible. Given access to a range of food groups, your baby will show you what they need. If they don’t want a certain food, try something else, but do offer it again.
If they don’t want a certain food, try something else, but do offer it again.
You don’t need to purée foods or even mash them. Puréeing often requires liquid to be added, diluting the nutritional content. Solid (un-mashed) food aids development of chewing skills, which babies don’t get from sucking puréed food. Early exposure to different textures can also prevent a baby refusing to eat lumpy food later on.
Gagging and choking
Gagging happens when food triggers a baby’s gag reflex and the food is pushed forwards to prevent it from blocking the airway. A baby gagging will usually be calm and breathing normally. Gagging is a natural protective mechanism to prevent choking and usually doesn’t need any intervention.
Choking happens when a baby’s airway is (fully or partially) blocked and they can’t breathe. A baby choking will be coughing or silent (unable to make any noise), not breathing, and their face or lips may change colour.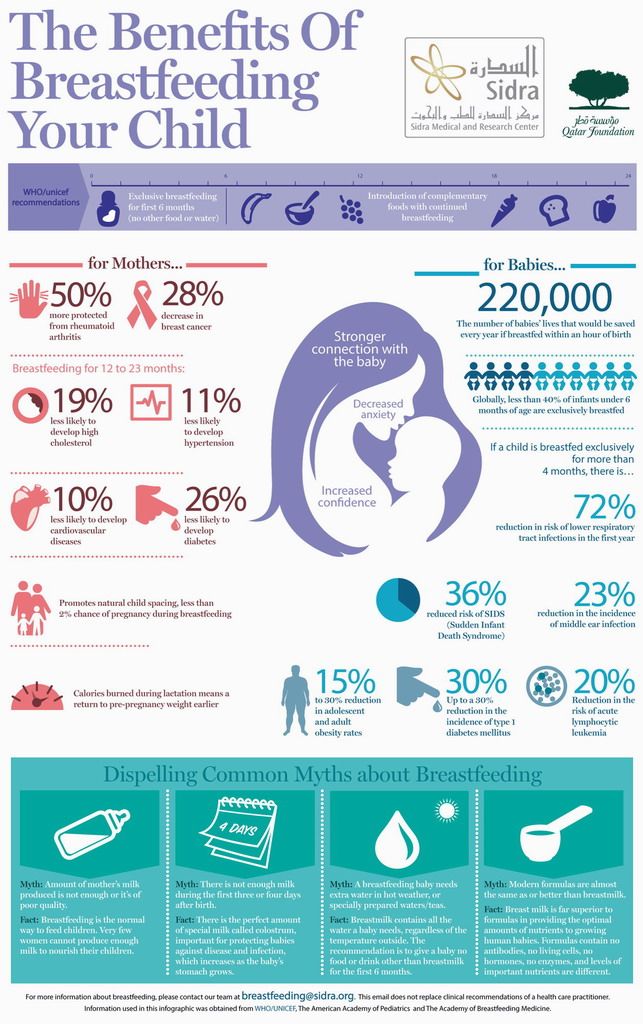 Choking is an emergency and they may need first aid to clear the blockage.
Choking is an emergency and they may need first aid to clear the blockage.
Babies are less likely to choke on food if they are sitting upright and feeding themself. Research shows baby-led weaning is not associated with an increased risk of choking.2
Certain foods are a choking risk for children under three years of age and should be avoided, including whole grapes, whole cherry tomatoes, popcorn, large amounts of peanut butter and any food that could break off in large chunks, such as raw carrot, hard apple or celery sticks. Nuts are a choking risk up to five years of age.
At first, you may want to check your baby’s mouth for unswallowed food after a meal, including their cheeks and palate. Never leave your baby alone with food or when they are eating.
Plan for a little mess!
Solid foods are another part of the world your baby is exploring and they will do this as much by touch and smell as by taste. This can be messy, but is an important learning experience for them. To make cleaning up easier, roll up their sleeves, use a bib or apron and put a clean plastic cloth on the floor so you can safely re-offer dropped foods.
To make cleaning up easier, roll up their sleeves, use a bib or apron and put a clean plastic cloth on the floor so you can safely re-offer dropped foods.
Natural appetite control
It is normal for your baby’s appetite to go up and down over the course of days, weeks and months. Don’t worry. Just offer more of any food they ask for and stop when they don’t want any more. There is no need to ‘top them up’ with a spoon if they haven’t eaten much at a meal. Allowing a baby to feed themselves and take their time over a meal helps them to tune in to their feelings of fullness and to stop eating, which is important throughout their life.
If your baby refuses food, they are not rejecting you or your efforts. They may simply not be hungry. If they are ill or teething, unrestricted breastfeeding will ensure they receive good nutrition and will comfort them until they feel well and interested again.
Allergy & Food Intolerance
Common allergens
The most common allergens (in order of incidence) are:
- Milk and other dairy products such as butter, yoghurt, cheese, whey, casein, caseinate, lactose
- Egg
- Peanut and tree nuts (almonds, hazelnuts, walnuts, cashews, etc.
 )
) - Soy
- Wheat
- Fish and Shellfish: crustaceans (e.g. crab, lobster, crayfish, shrimp, prawn), molluscs (e.g. mussels, oysters, squid)
- Sesame seeds (in tahini and hummus)
- Lupin/lentils (including chickpeas which are in hummus)
- Fenugreek (closely related to peanuts)
- Celery and celeriac
- Mustard
Introducing peanut and egg
Peanut and hen’s egg are common allergens for babies. Current guidance recommends that foods containing peanut or hen’s egg need not be differentiated from other solid foods and can be introduced from around 6 months along with other foods.
The deliberate exclusion of peanut or hen’s egg beyond 6 to 12 months of age may increase the risk of allergy to the same foods. Once introduced, and where tolerated, these foods should continue to be part of your child’s usual diet. If initial exposure is not continued as part of your child’s usual diet, then this may increase the risk of sensitisation and subsequent food allergy. 3
3
Eczema
If your baby has eczema, suspected food allergy, or a family history of food allergy you may wish to seek medical advice before introducing allergenic foods. If eczema is well-controlled (i.e. mild or cleared), it is easier to assess your baby’s tolerance to new foods.
Offer allergenic foods in very small amounts and watch carefully for any symptoms of an allergic reaction. If eczema becomes difficult to manage after food introduction, stop the allergen and seek medical advice.
Allergic reactions and symptoms to watch for
In very rare cases allergy can cause a severe life-threatening reaction called anaphylactic shock. If your baby has a severe and immediate allergic reaction, which may include swelling of the lips, tongue, eyes or face, seek emergency medical care.
Food sensitivity reactions can include eczema, nettle rash (urticaria), a sore bottom, wheezing, asthma, colic, vomiting, constipation and diarrhoea. If a food causes a mild reaction, talk to your health visitor or doctor about whether you should continue to give it. For further information, see Allergies & Food Intolerances.
If a food causes a mild reaction, talk to your health visitor or doctor about whether you should continue to give it. For further information, see Allergies & Food Intolerances.
Nutrition Requirements
Vitamins and minerals
The UK Department of Health recommend that all babies be given supplements including vitamins A, C and D from 6 months, and a vitamin D supplement from birth for breastfed babies and those receiving less than 500ml of formula per day.4
Iron
A healthy full-term baby has sufficient iron stores at birth, and delayed cord clamping helps to increase a baby’s iron levels. Iron is present in human milk and bioavailable to the baby, which is sufficient for the first 6 months of a baby’s life. Introduce iron rich foods from six months such as meat, poultry, fish, egg, pulses/legumes (e.g. chickpeas and lentils) and fortified cereals.
Vitamin D
This is produced when our bodies are exposed to sufficient sunlight. Wearing clothes and suncream to protect against skin cancer limits how much vitamin D we can produce. Vitamin D supplements are particularly important for babies who have limited exposure to sunlight and for babies with darker skin colour living in the UK. Breastmilk doesn’t contain high levels of vitamin D as, in the past, babies would absorb most of their vitamin D from exposure to sunlight.
Wearing clothes and suncream to protect against skin cancer limits how much vitamin D we can produce. Vitamin D supplements are particularly important for babies who have limited exposure to sunlight and for babies with darker skin colour living in the UK. Breastmilk doesn’t contain high levels of vitamin D as, in the past, babies would absorb most of their vitamin D from exposure to sunlight.
Vitamin B12
This is found in animal protein. Your baby may need vitamin B12 supplements if you eat a strict vegetarian or vegan diet.5
Nutritional needs of preterm babies
A premature baby does not have a good iron store at birth. If your baby was born before 34 weeks, they may already be receiving iron, zinc and vitamin supplements. Your preterm baby’s healthcare team will be able to give more specific guidance regarding their individual nutritional needs.
Good First Foods
Offering your baby a wide variety of foods in as close to their natural state as possible will ensure they receive a range of nutrients. Highly processed, low-fat or ready-prepared adult foods are not suitable for babies. You don’t need to buy ready-prepared baby food. These foods are expensive, often come in over-large portions and may contain added ingredients your baby doesn’t need. If you choose to buy convenience foods, check labels carefully.
Highly processed, low-fat or ready-prepared adult foods are not suitable for babies. You don’t need to buy ready-prepared baby food. These foods are expensive, often come in over-large portions and may contain added ingredients your baby doesn’t need. If you choose to buy convenience foods, check labels carefully.
To preserve nutrients as much as possible, bake, steam or cook foods in water. Take out a small portion for your baby before adding any salt or sugar to the rest. Allow it to cool to a suitable temperature. Offering finger foods avoids the need to add extras your baby may not be ready for, such as milk or butter.
Note: Some foods can trigger allergic reactions in some babies. See further down this article for more information.
| Food | Serving Suggestion | Notes |
|---|---|---|
| Vegetables (e.g. carrot, pea, sweet potato, potato) | Cook lightly to soften if needed. Give sticks or adult finger-sized pieces.  | Remove skin if needed. Avoid small chunks of raw hard vegetables, such as carrots, which could cause choking. |
| Fruit (e.g. apple, banana, avocado) | Give your baby a whole fruit or large piece to hold. | Remove skin and stones if needed. Small chunks can cause choking |
| Poultry (e.g. chicken) Meat | Give large pieces of lean cooked meat, moisten with meat juices. | Make sure to remove any bones and gristle. |
| Fish | Poach in a little water (no salt) or oven bake. | Check carefully for bones. Fish can be allergenic so introduce it with caution. Don’t introduce shellfish, smoked fish or pickled fish until your baby is over 12 months. |
| Rice cakes Oat cakes Crackers | Spread soft foods on, or use them for dipping. | Plain, unsalted rice cakes, oat cakes and crackers are useful alternatives to rusks. |
| Beans Lentils | Cooked beans and lentils can be mashed to make a spread or dip.  | Cook all beans and lentils thoroughly. |
| Dried fruit | Cut up larger fruits such as apricots. Apricots and prunes can be cooked in a small amount of water to make a nutritious spread. | Although rich in nutrients, dried fruit can stick to teeth and if given frequently can cause tooth decay even if you clean your baby’s teeth regularly. |
| Wholegrain cereals such as oats, corn (maize) and wheat | Can be cooked with water, without salt, sugar or sweetener. Choose unsweetened breakfast cereals. | Most cereals contain a protein called gluten, a potential sensitizer, so avoid mixed-grain cereals until you know your baby can tolerate each one individually. |
| Bread Pasta Rice | Bread and pasta are easy finger foods. Serve pasta plain, with butter or grated cheese. | Avoid pasta made with eggs until you know your baby can tolerate egg. |
| Cottage cheese, yoghurt, fromage frais, butter, unprocessed cheese | Your baby can use a spoon or their fingers.  Useful with cooked vegetables. Grate cheese or serve slices. Useful with cooked vegetables. Grate cheese or serve slices. | Use unsalted butter. |
| Eggs | Can be served scrambled, boiled, poached, in an omelette, etc. | If lion-stamped, egg can be served raw. Otherwise, cook until both white and yolk are solid. |
| Nuts and seeds (e.g. peanut butter, tahini) | Should be spread thinly. Only use smooth varieties. | Never give whole nuts or seeds until 5 years of age. Crunchy nut butter varieties can cause choking. |
Foods to avoid
Salt can overload a baby’s system and too much can cause kidney failure. Highly salted foods may foster a taste for salty foods. Avoid and minimize the use of processed foods, packet mixes, crisps, savoury snacks, gravy and condiments such as ketchup, yeast extract, mustard and brown sauce. When buying convenience foods look for low salt versions, including tinned beans and vegetables canned only in water.
White sugar contains virtually no nutrients and is a major factor in tooth decay. When checking food labels watch for other names for sugars – such as glucose, dextrose, sucrose, corn syrup and fructose. Molasses, maple syrup and honey are also almost pure sugar and can displace healthy nutritious foods. Many processed foods which are advertised for babies have high sugar content and should be avoided, including teething biscuits and baby rusks.
Honey may contain botulism spores and should not be given to babies younger than one year.
Teething biscuits are often high in sugar. Your baby can teethe using anything hard and safe to chew on, including unsalted rice cakes or crusty bread.
Artificial sweeteners are present in many processed foods and drinks aimed at babies and children, including juice drinks, ready meals and jars, and snack foods. Children who eat food with artificial sweeteners may be more likely to develop a ‘sweet tooth’ and a preference for sweet food in later life.
Children who eat food with artificial sweeteners may be more likely to develop a ‘sweet tooth’ and a preference for sweet food in later life.
Artificial flavourings and food colouring are unnecessary chemicals.
Foods high in saturated fats. While babies need fats in their diet, foods containing unnecessary saturated fats, such as fried foods, should be offered only in moderation.
Very hot spicy food. Many babies like spicy food, but very hot spices, especially chillies, may be unpleasant for a baby.
Shark, swordfish and marlin all contain high levels of mercury.
Drinks
Water, human milk and formula are the only recommended drinks until 1 year old.
At mealtimes offer some plain tap water in a baby-sized (shot glass size) cup. You don’t need to use bottles or spouted cups but, if you do, a free flow cup is better than one with a non-spill valve on which a baby needs to bite to get the drink to flow.
Avoid juices, sugary drinks and those with artificial sweeteners. Even unsweetened juices contain natural fruit sugars and acids that can damage teeth. They can leave no room for nutritious foods and it can be hard to limit them once you start them.
Avoid giving bottled water, which may have high mineral levels, and drinks that contain caffeine. This includes fizzy and other soft drinks, tea and coffee.
Can I offer cow’s milk as a drink?
Cow’s milk is not suitable as a drink until after 12 months. Instead offer water, human milk or formula. However, you can use cow’s milk when cooking for your baby, for example in porridge and sauces. Other dairy products can be offered to your baby as a food e.g. cheese, yogurt, cream.
After 1 year of age, cow’s milk can be given as a drink. Follow-on and toddler formulas are not necessary.
Further Reading
The Womanly Art of Breastfeeding. LLLI. London: Pinter & Martin, 2010.
My Child Won’t Eat. González, C. MD. London: Pinter & Martin, 2020.
Baby-Led Weaning The Essential Guide. Rapley, G. & Murkett, T. Experiment, 2019.
Why Starting Solids Matters. Brown, A. Pinter & Martin, 2017.
Starting Solids DVD. LLLGB, 2007.
How Weaning Happens. Bengson, D. Schaumburg, IL: LLLI, 1999.
LLLGB articles (and Leaflets & Information Sheets available from our LLLGB Shop)
Allergy and Food Intolerance
Amazing Milk
Thinking of Weaning?
Still Nursing
Toddlers and Food
Online Information
First Steps Nutrition Trust firststepsnutrition.org/ eating-well-infants-new-mums
NHS: Your baby’s first solid foods
Start 4 life nhs.uk/start4life/weaning/safe-weaning
Unicef unicef.org/nutrition
GP Infant Feeding Network gpifn.org.uk/introducing-solids/
References
1Why Starting Solids Matters. Brown, A. Pinter & Martin, 2017.
2LLLGB: Baby-led weaning and choking
3Scientific Advisory Committee on Nutrition. Feeding in the First Year of Life, July 2018:
4NHS: Vitamins for Children
5NHS: Vegetarian and vegan diets Q&A
Working Together: Breastfeeding and Solid Foods
Breastfeeding, like many other aspects of parenting, is a gradual process of increasing independence and self-mastery on your baby’s part and a gradual stepping back on yours. You may have already experienced the beginnings of this process during the first half year of life as your baby learned to enjoy drinking expressed breast milk from a bottle or cup and you began to go places without her. Still, the two of you were closely tied to each other in a nutritional sense: your child thrived on your breast milk alone, which provided the nutrients she needed.
During the second half of the year, your breast milk will continue to provide the great majority of necessary nutrients as she starts to sample a variety of new foods.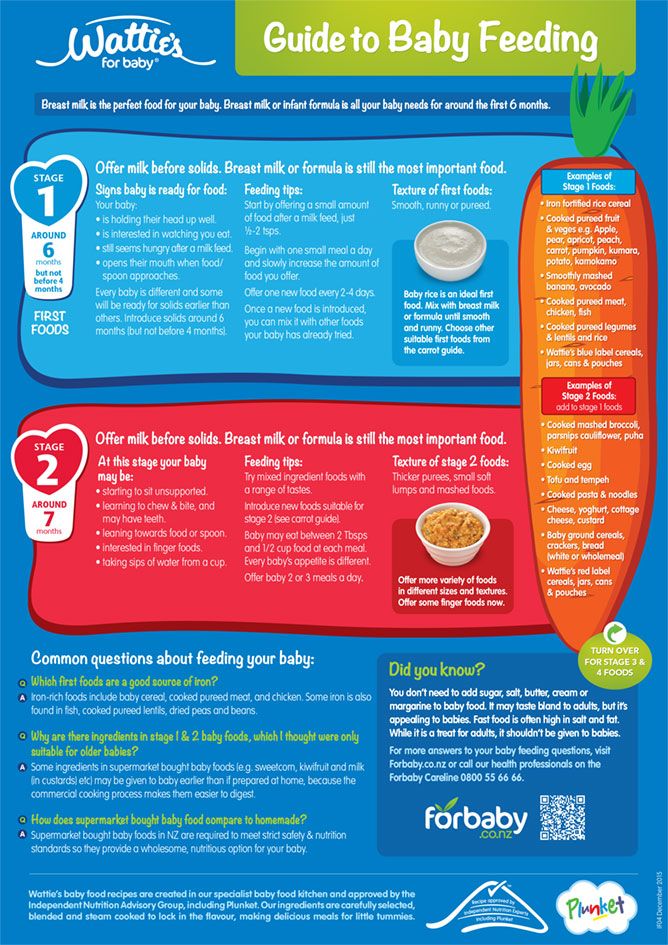 Though your baby will no doubt greatly enjoy the introduction of new tastes and textures in her life, her experiences with solid food are still just practice sessions for the future. It’s important to make sure she continues getting enough breast milk to meet her nutritional needs.
Though your baby will no doubt greatly enjoy the introduction of new tastes and textures in her life, her experiences with solid food are still just practice sessions for the future. It’s important to make sure she continues getting enough breast milk to meet her nutritional needs.
Introducing foods
The American Academy of Pediatrics recommends breastfeeding as the sole source of nutrition for your baby for about 6 months. When you add solid foods to your baby’s diet, continue breastfeeding until at least 12 months. You can continue to breastfeed after 12 months if you and your baby desire. Check with your child’s doctor about vitamin D and iron supplements during the first year.
Parents with food allergies are often advised to avoid foods that commonly cause allergic reactions (such as cow’s milk, dairy products, and foods made from peanuts or other nuts). But recent research found that the late introduction of certain foods may actually increase your baby’s risk for food allergies and inhaled allergies. You should discuss any concerns with your pediatrician.
You should discuss any concerns with your pediatrician.
If no allergies are present, simply observe your baby for indications that she is interested in trying new foods and then start to introduce them gradually, one by one. Signs that the older baby is ready for solids include sitting up with minimal support, showing good head control, trying to grab food off your plate, or turning her head to refuse food when she is not hungry. Your baby may be ready for solids if she continues to act hungry after breastfeeding. The loss of the tonguethrusting reflex that causes food to be pushed out of her mouth is another indication that she’s ready to expand her taste experience.
First foods
Since most breastfeeding babies’ iron stores begin to diminish at about six months, good first choices for solids are those rich in iron. Current recommendations are that meats, such as turkey, chicken, and beef, should be added as one of the first solids to the breastfed infant’s diet. Meats are good sources of high-quality protein, iron, and zinc and provide greater nutritional value than cereals, fruits, or vegetables.
Iron-fortified infant cereal (such as rice cereal or oatmeal) is another good solid food to complement breast milk. When first starting infant cereal, check the label to make sure that the cereal is a single- ingredient product—that is, rice cereal or oatmeal—and does not contain added fruit, milk or yogurt solids, or infant formula. This will decrease the likelihood of an allergic reaction with the initial cereal feedings. You can mix the cerealwith your breast milk, water, or formula (if you’ve already introduced formula to your baby) until it is a thin consistency. As your baby gets used to the taste and texture, you can gradually make it thicker and increase the amount.
Once your child has grown accustomed to these new tastes, gradually expand her choices with applesauce, pears, peaches, bananas, or other mashed or strained fruit, and such vegetables as cooked carrots, peas, and sweet potatoes. Introduce only one new food at a time and wait several days before you add another new food, to make sure your child does not have a negative reaction.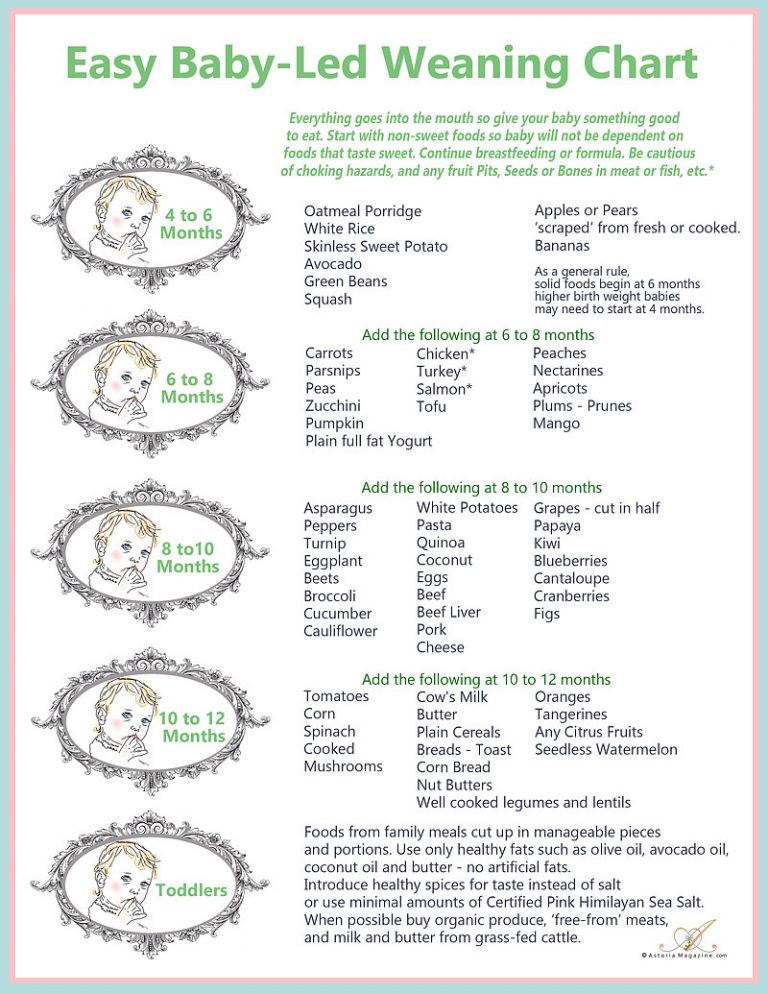
As you learn which foods your baby enjoys and which ones she clearly dislikes, your feeding relationship will grow beyond nursing to a more complex interaction— not a replacement for breastfeeding, certainly, but an interesting addition to it. Remember to keep exposing your baby to a wide variety of foods. Research indicates that some babies need multiple exposures to a new taste before they learn to enjoy it. The breastfed baby has already been experiencing different flavors in the mother’s breast milk, based upon her diet, so solid foods often have a familiar taste when introduced to the breastfed baby.
Babies need only a few spoonfuls as they begin solids. Since these first foods are intended as complements and not replacements for your breast milk, it’s best to offer them after a late afternoon or evening feeding, when your milk supply is apt to be at its lowest and your baby may still be hungry.
Some pediatricians recommend an iron supplement. If this is the case, be careful to give the exact dose prescribed by your doctor.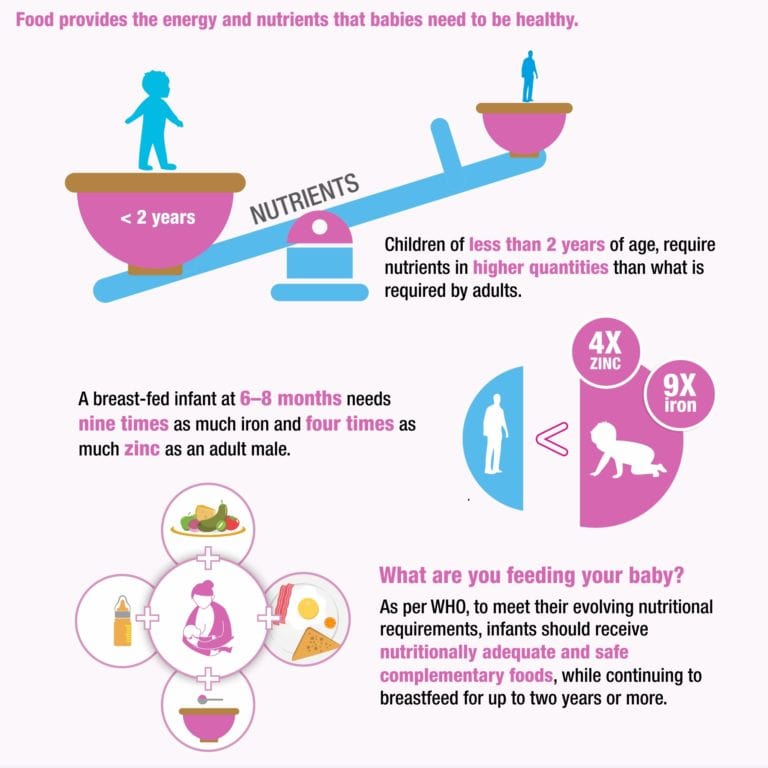 Always store iron and vitamin preparations out of the reach of young children in the household, since overdoses can be toxic.
Always store iron and vitamin preparations out of the reach of young children in the household, since overdoses can be toxic.
You may find that the number of breastfeedings will gradually decrease as her consumption of solid food increases. A baby who nursed every two to three hours during early infancy may enjoy three or four meals of breast milk per day (along with several snacks) by her twelfth month.
Unless you intend to wean her soon, be sure to continue breastfeeding whenever she desires, to ensure your continuing milk supply. To ease breast discomfort, it may become necessary to express a small amount of milk manually on occasion, if her decreasing demand leaves you with an oversupply. Breast comfort is another reason why a gradual introduction of solid foods is advisable, since it allows your body time to adapt to changing demands. Over the span of several months, a readjustment in the supply-and-demand relationship can take place smoothly and painlessly.
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician.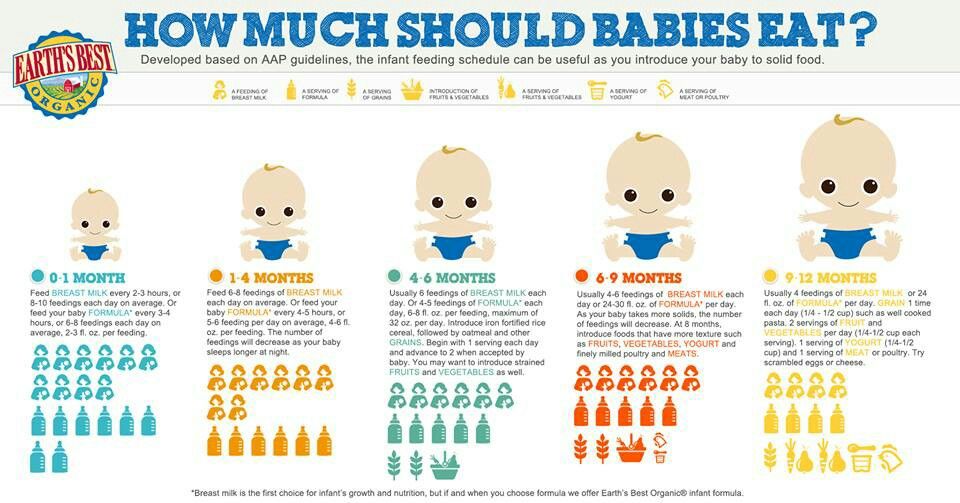 There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
Complementary foods while breastfeeding | Useful tips from the Tyoma brand
Most people are familiar with the phrase: "For breastfed children, the World Health Organization (WHO) recommends that complementary foods be introduced from 6 months."
But for some reason, many people forget (or don’t notice?) The phrase taken from the same WHO recommendations: “It is acceptable to introduce complementary foods in the interval of 4-6 months.”
Russian, European and American pediatricians unanimously support the WHO recommendation on the introduction of complementary foods for a period of 4-6 months.
It is important to note that at present there is no division according to the timing of the introduction of complementary foods, depending on what type of feeding the child is on: breastfeeding or artificial feeding.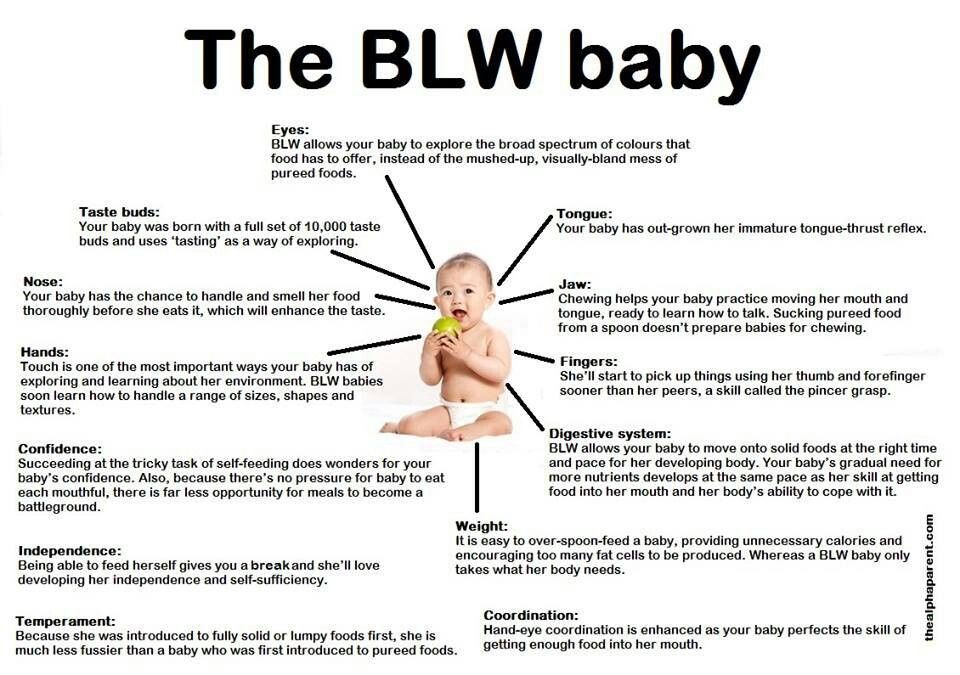 And the term itself is determined strictly individually, depending on the characteristics of the development of the child and his needs. That is why the WHO recommendation on the introduction of complementary foods from 6 months. may not be suitable for all children.
And the term itself is determined strictly individually, depending on the characteristics of the development of the child and his needs. That is why the WHO recommendation on the introduction of complementary foods from 6 months. may not be suitable for all children.
Research results
My colleagues and I from the National Medical Research Center for Children's Health of the Ministry of Health of Russia conducted a scientific study, as a result of which interesting data were obtained. Under our supervision were children on exclusive breastfeeding (ELF), whose parents introduced complementary foods to them from 4, 5 or 6 months. It was found that among children on IVF who were introduced to complementary foods after 6 months, by the age of 9months only 10% of children received all the necessary complementary foods, in most children by 9 months. such important foods as meat, fish and yolk were not introduced into the diet. And everything would be fine, but it was these children who had the lowest indicators of the body's supply of iron, the most valuable trace element necessary for the successful growth and development of the baby. Foreign studies also confirm that the late introduction of complementary foods with HBV (from 7 months and later) can lead to latent or overt iron deficiency in the child's body.
Foreign studies also confirm that the late introduction of complementary foods with HBV (from 7 months and later) can lead to latent or overt iron deficiency in the child's body.
IGI should not be an obstacle to the timely introduction of complementary foods.
According to domestic recommendations, reflected in the New Nutrition Program for 1-year-old children in the Russian Federation (http://nczd.ru/2019-12-17/), the introduction of complementary foods to children on IVF should start a little earlier than 6 months, optimally from 5-5.5 months to 7 months. the child has already received sufficient complementary foods.
These deadlines are especially necessary:
- children with iron deficiency anemia;
- children whose mothers are malnourished or do not take multivitamin complexes for pregnant and lactating women;
- children who are not gaining weight well.
Signs that a baby is ready for complementary foods while breastfeeding
- can swallow mashed food;
- interested in adult food.
Success Rules for Starting Breastfeeding Complementary Feeding
- For children who are exclusively breastfed, introduce complementary foods from 5-5.5 months.
- Introduce complementary foods only BEFORE breastfeeding
- Do not start complementary foods with juices or fruit purees. Fruit puree is introduced after the introduction of the main complementary foods, but you can take your time with juices at all: their nutritional value is not at all high.
- Do not start complementary foods while your child is vaccinated or sick.
- Enter complementary foods when the child has already managed to get hungry (2.5-3 hours after breastfeeding), but does not scream with hunger, otherwise he will definitely refuse complementary foods.

- The first type of complementary foods should be dairy-free porridge or vegetable puree. Usually cereals are introduced first if the baby is not gaining weight well. Vegetables may be introduced first if the child is constipated or overweight.
- The first porridge should be dairy-free. And you can dilute it with water or expressed breast milk.
- Start introducing a new product with 1 tsp. Gradually bring to the age volume in 7-10 days. If the baby does not accept the new taste, then mix the new food with a familiar dish or add some breast milk to it.
- Increasing the amount of complementary foods should be carried out without any violence. Refusal of the child from complementary foods in the morning, may end with a favorable reception in the afternoon.
- If before complementary foods there was feeding at the request of the child, then from the moment the complementary foods are introduced, feeding at the request of the mother begins.
 What does it mean? The introduction of complementary foods should be tried to be carried out regularly and at the same time, allocating conditional time for this for the future breakfast, lunch and dinner (afternoon snack). The recommended interval between meals is 3.5-4 hours.
What does it mean? The introduction of complementary foods should be tried to be carried out regularly and at the same time, allocating conditional time for this for the future breakfast, lunch and dinner (afternoon snack). The recommended interval between meals is 3.5-4 hours.
Question answer
If the child is 4 months old, and the mother notes a lack of breast milk, what is the best way to introduce complementary foods or supplementary foods?
If the mother does not have enough milk, and the child is only 4 months old, then in this case it is better to start introducing complementary foods, and not start feeding the baby with milk formula.
And if the child is unable to eat the age norm of complementary foods at a time, what should I do?
If a child cannot eat the age-appropriate amount of complementary foods per feeding (for example, 150 g of porridge), then this amount can be divided into 2 feedings, i. e. you can give 100 g of porridge for lunch and 50 g for dinner.
e. you can give 100 g of porridge for lunch and 50 g for dinner.
Will I run out of breast milk with the introduction of complementary foods?
With the introduction of complementary foods, breast milk becomes less and less, and this is a natural process, but its amount will decrease only by the volume of complementary foods introduced, so breastfeeding during the day, as well as before bedtime and at night, can remain in the child’s diet for a long time, up to 2 years or more, as you wish.
Complementary foods while breastfeeding | Useful tips from the Tyoma brand
Most people are familiar with the phrase: "For breastfed children, the World Health Organization (WHO) recommends that complementary foods be introduced from 6 months."
But for some reason, many people forget (or don’t notice?) The phrase taken from the same WHO recommendations: “It is acceptable to introduce complementary foods in the interval of 4-6 months.”
Russian, European and American pediatricians unanimously support the WHO recommendation on the introduction of complementary foods for a period of 4-6 months.
It is important to note that at present there is no division according to the timing of the introduction of complementary foods, depending on what type of feeding the child is on: breastfeeding or artificial feeding. And the term itself is determined strictly individually, depending on the characteristics of the development of the child and his needs. That is why the WHO recommendation on the introduction of complementary foods from 6 months. may not be suitable for all children.
Research results
My colleagues and I from the National Medical Research Center for Children's Health of the Ministry of Health of Russia conducted a scientific study, as a result of which interesting data were obtained. Under our supervision were children on exclusive breastfeeding (ELF), whose parents introduced complementary foods to them from 4, 5 or 6 months. It was found that among children on IVF who were introduced complementary foods after 6 months, by the age of 9 months. only 10% of children received all the necessary complementary foods, most children by 9months such important foods as meat, fish and yolk were not introduced into the diet. And everything would be fine, but it was these children who had the lowest indicators of the body's supply of iron, the most valuable trace element necessary for the successful growth and development of the baby. Foreign studies also confirm that the late introduction of complementary foods with HBV (from 7 months and later) can lead to latent or overt iron deficiency in the child's body.
only 10% of children received all the necessary complementary foods, most children by 9months such important foods as meat, fish and yolk were not introduced into the diet. And everything would be fine, but it was these children who had the lowest indicators of the body's supply of iron, the most valuable trace element necessary for the successful growth and development of the baby. Foreign studies also confirm that the late introduction of complementary foods with HBV (from 7 months and later) can lead to latent or overt iron deficiency in the child's body.
IGI should not be an obstacle to the timely introduction of complementary foods.
According to domestic recommendations, reflected in the New Nutrition Program for 1-year-old children in the Russian Federation (http://nczd.ru/2019-12-17/), the introduction of complementary foods to children on IVF should start a little earlier than 6 months, optimally from 5-5.5 months to 7 months. the child has already received sufficient complementary foods.
These deadlines are especially necessary:
- children with iron deficiency anemia;
- children whose mothers are malnourished or do not take multivitamin complexes for pregnant and lactating women;
- children who are not gaining weight well.
Signs that a baby is ready for complementary foods while breastfeeding
- can swallow mashed food;
- interested in adult food.
Success Rules for Starting Breastfeeding Complementary Feeding
- For children who are exclusively breastfed, introduce complementary foods from 5-5.5 months.
- Introduce complementary foods only BEFORE breastfeeding
- Do not start complementary foods with juices or fruit purees. Fruit puree is introduced after the introduction of the main complementary foods, but you can take your time with juices at all: their nutritional value is not at all high.

- Do not start complementary foods while your child is vaccinated or sick.
- Enter complementary foods when the child has already managed to get hungry (2.5-3 hours after breastfeeding), but does not scream with hunger, otherwise he will definitely refuse complementary foods.
- The first type of complementary foods should be dairy-free porridge or vegetable puree. Usually cereals are introduced first if the baby is not gaining weight well. Vegetables may be introduced first if the child is constipated or overweight.
- The first porridge should be dairy-free. And you can dilute it with water or expressed breast milk.
- Start introducing a new product with 1 tsp. Gradually bring to the age volume in 7-10 days. If the baby does not accept the new taste, then mix the new food with a familiar dish or add some breast milk to it.
- Increasing the amount of complementary foods should be carried out without any violence.
 Refusal of the child from complementary foods in the morning, may end with a favorable reception in the afternoon.
Refusal of the child from complementary foods in the morning, may end with a favorable reception in the afternoon. - If before complementary foods there was feeding at the request of the child, then from the moment the complementary foods are introduced, feeding at the request of the mother begins. What does it mean? The introduction of complementary foods should be tried to be carried out regularly and at the same time, allocating conditional time for this for the future breakfast, lunch and dinner (afternoon snack). The recommended interval between meals is 3.5-4 hours.
Question answer
If the child is 4 months old, and the mother notes a lack of breast milk, what is the best way to introduce complementary foods or supplementary foods?
If the mother does not have enough milk, and the child is only 4 months old, then in this case it is better to start introducing complementary foods, and not start feeding the baby with milk formula.