Is it normal for babies to choke while feeding
Help! My Baby Is Choking on Milk!
Many parents look forward to feeding time with their baby. It’s a chance to bond and also gives you a few minutes of peace and quiet.
But for some, bottle feeding or breastfeeding can lead to gagging or choking sounds, which are alarming if you’re a new parent. Fortunately, there are things you can do to help prevent your baby from choking on milk or formula.
If your baby seems to gag a lot while eating, don’t panic. “Choking and gagging during feeding is common in young infants,” says Robert Hamilton, MD, FAAP, a pediatrician at Providence Saint John’s Health Center in Santa Monica.
Hamilton says babies are born with an exaggerated but protective “hyper-gag reflex,” which can cause gagging while feeding. Plus, babies gag easily due to their own neurologic immaturity.
“Babies are growing and learning new ways to use their body (and mouths) every day,” says Amanda Gorman, CPNP and founder of Nest Collaborative, a collection of International Board Certified Lactation Consultants.
“Often, just stopping the feed and positioning the baby upright with good head and neck support will give them a few seconds to manage the problem.”
Gina Posner, MD, a pediatrician at MemorialCare Orange Coast Medical Center, says if your baby begins to choke, let them stop feeding for a little bit and pat their back. “Typically, if they’re choking on liquids, it will resolve quickly,” she says.
The most common reason a baby chokes during breastfeeding is that milk is coming out faster than your baby can swallow. Usually, this happens when mom has an oversupply of milk.
According to the La Leche League International (LLLI), common signs of oversupply include restlessness at the breast, coughing, choking, or gulping milk, especially at let down, and biting on the nipple to stop the flow of milk, among others.
You might also have an overactive let down, which causes a forceful flow of milk into your baby’s mouth. When your breasts are stimulated by your baby suckling, oxytocin causes the let-down reflex that releases the milk.
If you have an overactive or forceful let down, this release happens too fast for your baby to respond appropriately, causing them to gulp or choke while breastfeeding.
How do I prevent my baby from choking on milk when breastfeeding?
One of the first things you can do to help prevent your baby from choking while eating is to change the feeding position.
“For breastfeeding mothers who appear to have overactive let down, we typically recommend they nurse in a laid-back position, which reverses gravity’s effect and allows baby to have more control,” says Gorman.
Posner recommends pulling your baby off the breast every once in a while to help them catch their breath and slow down. You can also take your baby off the breast for 20 to 30 seconds when your milk first lets down.
In addition to a laid-back position, the LLL recommends lying on your side so your baby can allow milk to dribble out of his mouth when it flows too quickly.
Furthermore, expressing milk for 1 to 2 minutes before bringing your baby to your breast can help. Doing so allows the forceful let down to happen before baby latches. That said, be careful with this technique, as pumping for too long will tell your body to make more milk and worsen the problem.
Doing so allows the forceful let down to happen before baby latches. That said, be careful with this technique, as pumping for too long will tell your body to make more milk and worsen the problem.
When your baby gags when drinking from a bottle, it’s often due to the positioning. Lying your baby on their back while bottle feeding will lead to a faster milk flow, making it harder for your baby to control the rate of feeding.
“Tilting the bottom of the bottle higher than the nipple increases the rate of milk flow, as will a nipple with too large of a hole for the infant’s age,” Gorman advises. Tilting the bottle too high can lead to involuntary increases in intake and contribute to problems like reflux.
Instead, when bottle-feeding an infant, try using a technique called paced bottle-feeding. “By keeping the bottle parallel to the ground, the baby remains in control of the milk flow, as they are at the breast,” Gorman says.
This technique allows your baby to actively pull milk out of the bottle using their sucking skills and lets them easily take a break when needed. Otherwise, gravity is in control.
Otherwise, gravity is in control.
For babies who are bottle-fed by multiple caregivers, Gorman says all of the people who administer feeds should be educated on paced bottle-feeding.
Finally, you should never prop the bottle up to feed your baby and walk away. Since they can’t control the flow of the milk, it will keep coming even if your baby is not ready to swallow.
“The mechanism of swallowing is complicated and requires several muscle groups working together in concert and in the right time sequence,” Hamilton says. Fortunately, gagging usually diminishes as children get older and become better at swallowing.
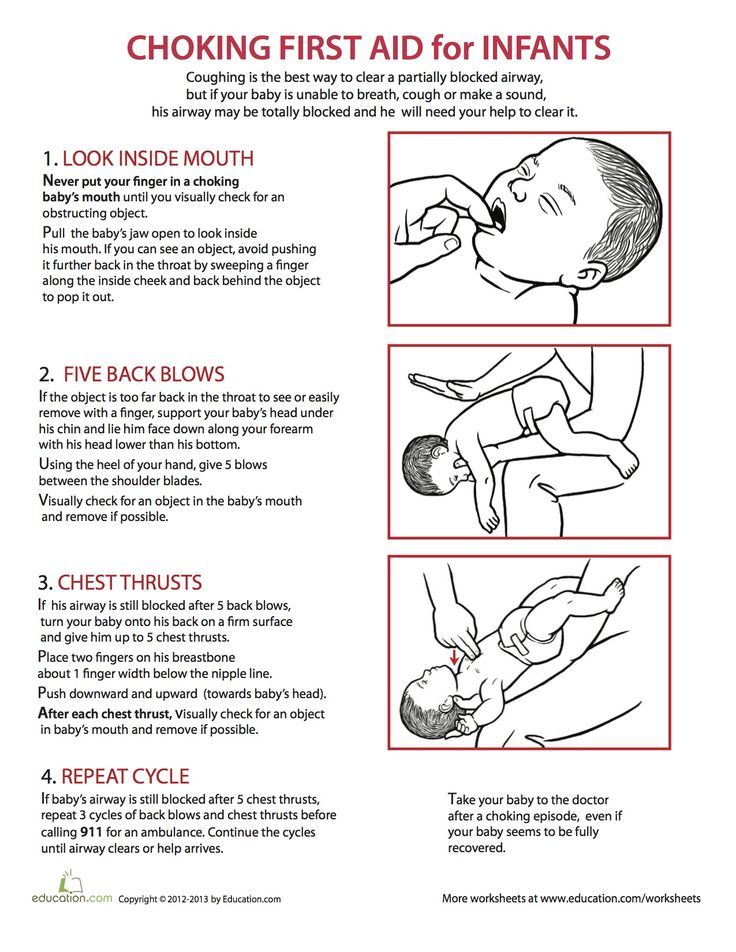
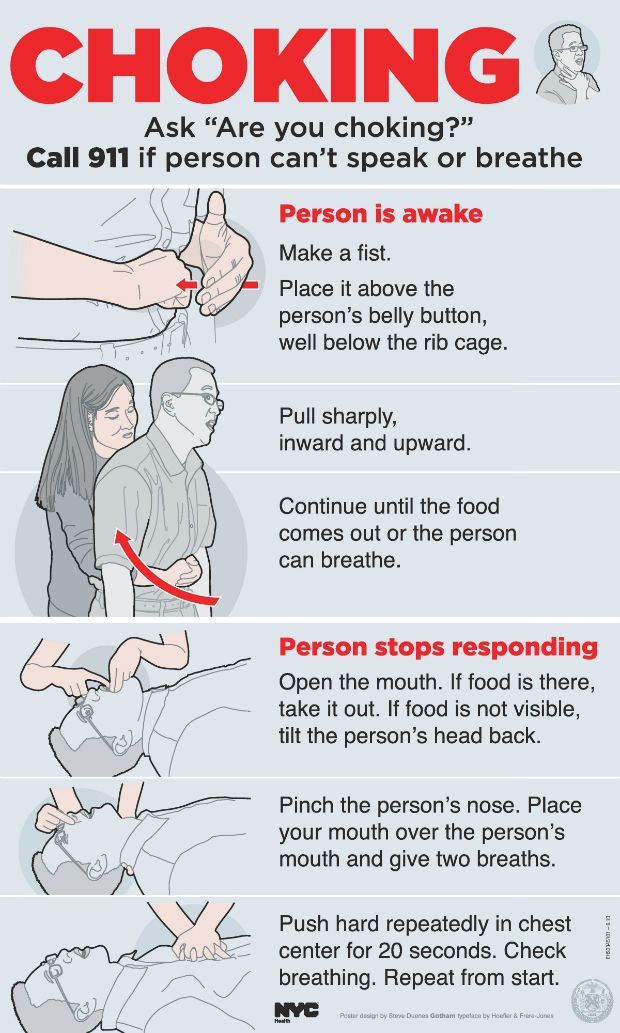
Still, if you’re a new parent or caregiver, it’s smart to take infant cardiopulmonary resuscitation (CPR). While rare, a choking episode that caused your baby to turn blue or lose consciousness would be an emergency.
If you’re having problems related to breastfeeding, contact a LLL leader or International Board Certified Lactation Consultant (IBCLC). They can help you with your baby’s latch, positioning, oversupply issues, and forceful let-down problems.
They can help you with your baby’s latch, positioning, oversupply issues, and forceful let-down problems.
If you’re having problems related to bottle feeding, contact your child’s pediatrician. They can help you with bottle and nipple selection, as well as feeding positions that prevent choking on milk or formula.
If your baby continues to choke even after slowing down the rate of feeding, you should contact your pediatrician to rule out any anatomical reasons why swallowing may be challenging.
When you hear your baby gagging or choking during feeding, don’t panic. Take baby off the nipple and prop them up to help them clear their airway.
Often it will take a little time for your baby to learn suckle with ease. In the meantime, try keeping your baby upright during feedings and make the flow of milk slower, if possible. Soon enough, feeding time will be a sweet snuggle session!
Why Baby Chokes On Breastmilk And What To Do About It
Stop feeding, hold them upright, and pat their back until choking subsides.
Research-backed
MomJunction believes in providing reliable, research-backed information to you. As per our strong editorial policy requirements, we base our health articles on references (citations) taken from authority sites, international journals, and research studies. However, if you find any incongruencies, feel free to write to us.
Image: Shutterstock
If you see your baby choking on breastmilk, it could be because their swallowing skills aren’t fully developed. Choking when breastfeeding can result in innocuous coughing. Further, milk can sometimes make its way into the lungs, causing aspiration pneumonia (1).
If your baby has rapid breathing, turns blue, or becomes unconscious from choking on breast milk, get emergency medical attention. If your baby has experienced many choking incidents, you might want to see a pediatrician.
Read on to learn more about the reasons for choking in babies, preventive measures, and what to do if you find yourself in this scenario.
Why Does A Baby Choke While Breastfeeding?
A baby can choke on breastmilk due to various reasons ranging from normal immature swallowing to feeding problems due to anatomical or functional disorders. It can also be due to maternal factors.
The main causes of choking while breastfeeding can be (2):
- Oversupply of breast milk: Faster milk flow is one of the major causes of choking on breast milk. Infants may not be able to swallow quickly. This may often happen if the mother has an oversupply of breast milk. The baby may bite while breastfeeding due to the overflow of milk, thus making swallowing further difficult.
- Overactive letdown: It is the forceful ejection of milk when your baby is sucking. Let down reflex is controlled by oxytocin hormones. Increased release of breast milk can cause gulping, coughing, or choking in infants.
Infants who have feeding difficulties are associated with a high risk of choking while breastfeeding or bottle-feeding. The following congenital abnormalities may result in feeding problems (3)
The following congenital abnormalities may result in feeding problems (3)
.
- Developmental delay
- Neurological issues such as cerebral palsy
- Down’s syndrome
- Structural anomalies of oral, respiratory, or feeding structures, such as cleft lip and palate and Pierre Robin syndrome
- Gastrointestinal issues, such as tracheoesophageal fistula
- Congenital heart diseases
- Lung and liver diseases
A healthcare provider should examine if there is frequent choking while feeding. Early intervention could reduce the risk of aspiration pneumonia and other complications.
What To Do If A Baby Chokes While Breastfeeding?
Gagging and choking during nursing is common in young babies. Most of the time, babies can protect themselves from aspiration due to hyper-gag reflex.
The following can be done if your baby chokes while nursing (4).
- Stop feeding if the baby chokes on milk.
- Hold the baby in an upright position for a few seconds. This could help babies to manage the problem.
- Provide good head and neck support while holding younger infants in an upright position.
- Patting the baby’s back may help them.
If the baby turns blue or becomes unconscious after choking, seek emergency medical care. You should also contact a pediatrician if choking occurs in bottle-fed infants.
How to Prevent Choking While Breastfeeding?
The following remedies may help reduce or prevent the incidence of choking on breast milk (1).
- Changing the feeding position is the best way to prevent choking while nursing. The laid-back feeding position is recommended for mothers who have an overactive letdown. This may help slow down milk flow due to gravity, and the baby could manage the flow better.
- You may try to take the baby off the breast for a few minutes during the initial letdown after sucking.
- Lying on the side may also reduce choking incidents. This position may allow the baby to let go of the breast and let the milk flow outside their mouth, to avert choking.
- You may also express milk a few minutes before feeding to reduce overflow and help to control let down.
- It is recommended to seek help from international board-certified lactation consultants (IBCLC) to manage overflow and hyperactive letdown issues. A pediatrician may also help to choose the right bottles and positions to prevent choking while formula feeding.
Note: You should be cautious while expressing or pumping milk since doing it for a longer duration may worsen the outcome. Consult a board-certified lactation consultant who can teach you the correct way to express or pump breast milk.
1. Can babies choke on milk while sleeping on their backs?
No. The common belief that babies may choke while sleeping on their backs is false. Your baby’s gag reflex and airway anatomy prevent them from choking and enable them to sleep comfortably (5).
2. Can reflux cause babies to choke?
Yes, since some food and stomach acid travel back to the food pipe during reflux, it may cause babies to choke. However, the condition does not cause any worry as long as your baby is healthy. Further, sleeping on the back may help babies with reflux (6) (5).
If you are worried about your baby choking on breastmilk, you must understand that the feeding skills of babies improve as they grow older. It is improbable for older babies to choke while nursing as they should be well acquainted with the procedure by now. However, if your little one lacks the age-appropriate ability to suck and swallow milk efficiently, they may be facing feeding difficulties. In such situations, you must consult your baby’s pediatrician to understand ways to avoid this problem and evaluate how to manage the situation.
Key Pointers
- Feeding difficulties, oversupply, and overactive letdown can cause the babies to choke on breastmilk.
- It is recommended to stop feeding and keep the baby in an upright position immediately when they choke while feeding.
- You may change feeding position, manage oversupply, or express milk before feeding to reduce choking while nursing.
References:
MomJunction's articles are written after analyzing the research works of expert authors and institutions. Our references consist of resources established by authorities in their respective fields. You can learn more about the authenticity of the information we present in our editorial policy.
1. Aspiration pneumonia; U.S. National Library of Medicine
2. Oversupply; La Leche League International (LLLI)
3. Choking On Milk; My Health; The Government of Malaysia
4. Infant choking while breastfeeding; New Kids-center
5. How to Keep Your Sleeping Baby Safe: AAP Policy Explained; Healthy children; AAP
How to Keep Your Sleeping Baby Safe: AAP Policy Explained; Healthy children; AAP
6. Breastfeeding challenges; NHS
The following two tabs change content below.
- Reviewer
- Author
Dr. Bisny T. Joseph is a Georgian Board-certified physician. She has completed her professional graduate degree as a medical doctor from Tbilisi State Medical University, Georgia. She has 3+ years of experience in various sectors of medical affairs as a physician, medical reviewer, medical writer, health coach, and Q&A expert. Her interest in digital medical education and patient education made... more
Rebecca Koyf is an International Board Certified Lactation Consultant (IBCLC), Registered Lactation Consultant (RLC),Certified Lactation Counselor (CLC) and a LaLeche League volunteer. She has a Bachelor's degree in Accounting and worked as an Auditor for the NYC Comptroller’s Office for 8 years. Her own breastfeeding struggles made her change her career and pursue the field in lactation. She has her... more
She has her... more
Why Do Babies Rub Their Eyes And How To..
Why Do Babies Rub Their Eyes And How To..
Blue Mongolian Spots In Newborn:..
Blue Mongolian Spots In Newborn:..
Bad Breath During Pregnancy: Causes,..
Bad Breath During Pregnancy: Causes,..
Is It Normal For Your Vagina To Smell..
Is It Normal For Your Vagina To Smell..
Baby Vaccination Schedule And Chart In..
Baby Vaccination Schedule And Chart In..
Fever During Pregnancy: Symptoms,..
Fever During Pregnancy: Symptoms,..
Cough In Pregnancy: Causes, Home..
Cough In Pregnancy: Causes, Home..
C-Section Scar Wound Infection
C-Section Scar Wound Infection
5 Causes Of High Amniotic Fluid..
5 Causes Of High Amniotic Fluid..
The child chokes when feeding: what to do?
Nikulina Anastasia Anatolyevna
pediatrician
A newborn chokes when feeding for various reasons. Some of them the mother can eliminate, while others depend on the health of the baby. The pediatrician Anastasia Anatolyevna Nikulina will explain the causes and solutions to this problem.
Some of them the mother can eliminate, while others depend on the health of the baby. The pediatrician Anastasia Anatolyevna Nikulina will explain the causes and solutions to this problem.
— Anastasia Anatolyevna, at what age do children most often choke while feeding?
— In the first weeks of life, when the swallowing reflex is still very weak, it is difficult to dose milk supply from the breast. From the bottle, the flow of formula is controlled by the opening in the nipple and the tilt. If the hole in the nipple is not age appropriate, it is tight, then the newborn swallows air. Excess air with the mixture will enter the intestines, causing discomfort to the baby.
Why does the baby choke while breastfeeding or bottle feeding
- Baby position or bottle angle not optimal. in the optimal position. In the right position, the hand of the woman who holds the child lies on the support. Hold the baby by the back and shoulders, directing the head to the chest.
 You can’t press hard on the head - the baby will recline it back reflexively.
You can’t press hard on the head - the baby will recline it back reflexively. - Anatomical features of the mother's breast, in which a woman produces enough breast milk, but it is difficult for a child to suck it out, to eat. Before feeding, the mother needs to express some of the milk or massage the breast: it will become soft, and it will be easier for the baby to suck.
- Large nipples are difficult for a baby to grab - to solve the problem, there are special nipple covers through which newborns are fed. You can feed your baby with expressed milk through a bottle and a nipple that is correctly selected for age.
- Hyperlactation. Pressurized breast milk squirts into the baby's mouth. Before feeding, some of the foremilk is expressed, and the following, more fatty, does not form a strong flow. Breaks in the sucking process also help.
- Frequent breastfeeding. The absence of long breaks between attachments to the breast prevents children from hunger and, with it, the rush to feed.

- Incorrect bottle delivery method. The neck of the bottle must be completely filled with milk: this way there will be no air in the milk. The nipple is selected taking into account the age of the baby.
- Disease. Nasal obstruction or cough interferes with feeding. Relief of the symptoms of the disease will improve nutrition. For some children, problems can be caused by improper swallowing or reflux.
- To understand why the baby is having difficulty swallowing, you need to gradually eliminate each of the possible causes. Even the environment matters. During feeding hours, it is desirable for a woman to be alone with the child, nothing should distract him from the process. If the mother finds it difficult to identify the cause, a pediatrician will help her.
— What should I do if my child chokes on milk or formula?
- Spontaneous cough is the main symptom that appears when the act of sucking and swallowing is disturbed. The baby is crying and refuses to eat.
First aid for choking children
If you can’t cough up excess milk on your own or the baby chokes on saliva and starts to choke, you need to do the following, dosing the force of your actions:
- Place the baby on one hand with the belly down, with your free hand apply pressure on the area above the navel (on the area of the baby's stomach), supporting the chin.
- Tilt the child slightly forward, lightly pat on the back. This will increase the cough and help restore breathing.
- Can I continue feeding after the baby clears his throat, or should I take a break?
- Feeding can be continued after the baby clears his throat. It is advisable to vilify it with a column for two to three minutes, so that excess air comes out, and then resume feeding.
- Does increasing the interval between feedings help with the problem?
- On the contrary, the prevention of flooding will be frequent feeding. With numerous attachments, less milk accumulates in the woman’s breast, it becomes easier for the mother to feed.
With numerous attachments, less milk accumulates in the woman’s breast, it becomes easier for the mother to feed.
If the child is choking, feeding should be interrupted. The baby will cough, rest and continue to suck. If the situation recurs frequently, be sure to consult your pediatrician. Your doctor can help you find the best breastfeeding or formula-feeding method for you.
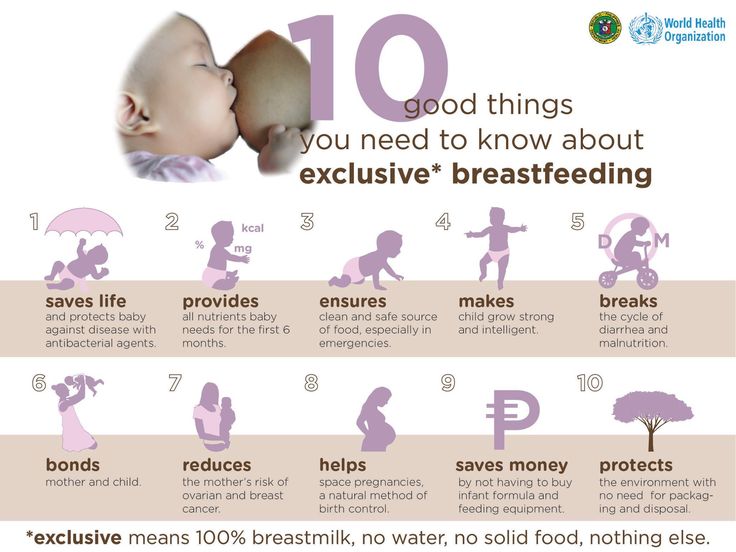
* Breast milk is the best food for babies. WHO recommends exclusive breastfeeding for the first 6 months of a child's life and continued breastfeeding after complementary foods are introduced until the age of 2 years. Before introducing new products into the baby's diet, you should consult with a specialist. The material is for informational purposes and cannot replace the advice of a healthcare professional. For feeding children from birth. The product is certified.
#Tips for Mom #regurgitation 7-12 #regurgitation 12 plus
See also
Digestion in newborns and infants and its features
#Baby Digestion #breast-feeding #baby formula #Lure #Tips for mom #Baby development
Kiseleva Elena Sergeevna
Candidate of Medical Sciences, Scientific Advisor MAMAKO ®
Principles of successful lactation: checklist for mom
#Tips for Mom #breastfeeding
Yakovenko Margarita Pavlovna
Candidate of Medical Sciences, Pediatrician, Pediatric Neurologist, Medical Advisor MAMAKO ®
First tests and vaccinations: how to prepare yourself and your child
#Advice for Mom
Kizino Polina Alexandrovna
pediatrician, perinatal psychologist
How to tell if a baby has a food allergy
#allergy #Tips for mom #breast-feeding #baby formula #lure
Kiseleva Elena Sergeevna
Candidate of Medical Sciences, Scientific Advisor MAMAKO ®
Neurologist for a child under one year old: first examination
#Tips for Mom #Baby development
Yakovenko Margarita Pavlovna
Candidate of Medical Sciences, Pediatrician, Pediatric Neurologist, Medical Advisor MAMAKO ®
How to properly rock a baby to sleep
#Advice for Mom
Kizino Polina Alexandrovna
pediatrician, perinatal psychologist
Goat's milk in children's nutrition: for or against
#Food #Tips for mom #Baby digestion #breastfeeding
Javier Diaz Castro
professor, lecturer
Calendar of doctor visits during the first year of a child's life
#Advice for Mom
Kizino Polina Alexandrovna
pediatrician, perinatal psychologist
Why DHA, ARA and lutein are added to infant formula
#baby formulas #Baby development
Yakovenko Margarita Pavlovna
Candidate of Medical Sciences, Pediatrician, Pediatric Neurologist, Medical Advisor MAMAKO ®
Omicron in children: how dangerous it is and how babies get sick up to a year
#Advice for Mom
Kiseleva Elena Sergeevna
Candidate of Medical Sciences, Scientific Advisor MAMAKO ®
See all
See all
Goat's milk in children's nutrition: for or against
# Lure # Tips for Mom # Baby's digestion # breastfeeding
Javier Diaz Castro
professor, lecturer
Digestion in newborns and infants and its features
# Baby's digestion # breast-feeding # infant formula # Lure # Tips for Mom # Baby development
Kiseleva Elena Sergeevna
Candidate of Medical Sciences, Scientific Advisor MAMAKO ®
Neurologist for a child under one year old: first examination
# Tips for mom # Baby development
Yakovenko Margarita Pavlovna
Candidate of Medical Sciences, Pediatrician, Pediatric Neurologist, Medical Advisor MAMAKO ®
Calendar of doctor visits during the first year of a child's life
# Tips for mom
Kizino Polina Alexandrovna
pediatrician, perinatal psychologist
Principles of successful lactation: checklist for mom
# Tips for mom # breastfeeding
Yakovenko Margarita Pavlovna
Candidate of Medical Sciences, Pediatrician, Pediatric Neurologist, Medical Advisor MAMAKO ®
How to properly rock a baby to sleep
# Tips for mom
Kizino Polina Aleksandrovna
pediatrician, perinatal psychologist
Why DHA, ARA and lutein are added to infant formula
# infant formula # Baby development
Yakovenko Margarita Pavlovna
Candidate of Medical Sciences, Pediatrician, Pediatric Neurologist, Medical Advisor MAMAKO ®
Omicron in children: how dangerous is it and how do babies get sick under the age of
# Tips for mom
Kiseleva Elena Sergeevna
Candidate of Medical Sciences, Scientific Advisor MAMAKO ®
See all
First tests and vaccinations: how to prepare yourself and your child
# Tips for mom
Kizino Polina Alexandrovna
pediatrician, perinatal psychologist
How to understand that a baby has a food allergy
# allergy # Tips for Mom # breast-feeding # infant formula # lure
Kiseleva Elena Sergeevna
Candidate of Medical Sciences, Scientific Advisor MAMAKO ®
See all
View all
View all
90,000 how to help the baby when regulating Support icon ofKeywords for searching
Home ›› How to help a child in sprinkling
Home Home ›!! How to help a child in regurgitation
↑ Verkh 9000
Breastal feeding - completely breastfeeding - completely special time for mom and her newborn baby. Together with the feeling of closeness and affection that feeding brings, understanding its nuances cannot but raise many questions, including the question of how to help an infant spit up. Regurgitation in a newborn is by no means always the result of a simple pat on his back.
Together with the feeling of closeness and affection that feeding brings, understanding its nuances cannot but raise many questions, including the question of how to help an infant spit up. Regurgitation in a newborn is by no means always the result of a simple pat on his back.
In this article, we'll talk about the basics of helping a newborn spit up, as well as other spit-up-related questions you may have.
Why do babies spit up?
Let's get it straight: Why do newborns need to burp in the first place? During feeding, children usually swallow extra air - this is called aerophagy. Spitting up helps prevent this air from entering the intestines, as well as vomiting, gas, and crankiness in the baby. To avoid the return of milk after feeding, you should give the baby the opportunity to burp more often.
How to help a newborn spit up?
During the first six months, the baby should be kept upright in a column for 10-15 minutes after each feed. This will help keep the milk in his stomach, but if the baby occasionally burps anyway, parents need not worry. While carrying your baby in an upright position, you can put a baby diaper or wipes on your shoulder to keep your clothes clean.
This will help keep the milk in his stomach, but if the baby occasionally burps anyway, parents need not worry. While carrying your baby in an upright position, you can put a baby diaper or wipes on your shoulder to keep your clothes clean.
We've already seen why spitting up is important, now let's find out how to help your baby spit up. Parents should gently pat the baby on the back with a hand folded in a handful until he burps. Folding your hand into a handful is important because clapping with a flat palm may be too strong for an infant.
Every baby is different and there is no one right position for spitting up. To get started, you can try the following options:
- Sitting position with the baby on the chest. In this position, the parent puts the baby's head with his chin on his shoulder and with one hand supports the baby under the back. With the other hand, you can gently pat the baby on the back. This method is most effective in a rocking chair or when the baby is gently rocking.

- Holding a child upright on one's legs. With one hand, parents can hold the baby by the back and head, supporting his chin and placing his palm on the baby’s chest, with the other hand, you can gently pat him on the back. At the same time, it is important to be careful: do not press the child on the throat, but only gently support his chin.
- Holding a baby on your lap while lying on your tummy. Make sure his head is above his chest and gently pat your baby on the back until he burps.
Here are some tips on how best to help your newborn spit up:
- Let your baby spit up during feeding. If the baby is restless or has swallowed air, it is worth giving him the opportunity to burp during feeding, and not just after.
- When bottle feeding, let the newborn burp after every 50-60 ml.
- When breastfeeding, let the baby burp at every breast change.
It is important to let your baby spit up after eating, even if he spit up during feeding!
If your baby is gassy, spit up more often. Also, if he vomits frequently or suffers from gastroesophageal reflux disease (GERD), have him spit up after every 30 ml bottle-feeding or every five minutes while breastfeeding.
Also, if he vomits frequently or suffers from gastroesophageal reflux disease (GERD), have him spit up after every 30 ml bottle-feeding or every five minutes while breastfeeding.
How long should a baby be held for it to burp? It's different for everyone, but generally keeping a newborn upright for 15 to 20 minutes after a feed helps the milk stay in the baby's stomach.
Minimize the amount of air you swallow. Gas production and regurgitation result from aerophagia during feeding. The baby will inevitably swallow air, but there are ways to prevent it from swallowing too much. Whether you bottle feed your baby or combine breastfeeding with bottle feeding, the Philips Avent anti-colic bottle with AirFree valve is designed so that the nipple is always filled with milk without excess air, even in a horizontal position, thus preventing the baby from swallowing excess air during feeding.
Reducing the amount of air your baby swallows can help reduce your baby's risk of colic, gas, and spitting up.