Mothers feeding babies videos
Breastfeeding & baby-led attachment | Raising Children Network
Renee Kam (lactation consultant): Baby-led attachment is where a baby uses their own instincts to find the mother’s breast on their own accord. Baby-led attachment really helps to lay down the foundation for breastfeeding. A baby who has had many opportunities, particularly in the early weeks, to do baby-led attachment becomes a lot more orientated towards the breast.
Adele (mother of Charlie, 5 years, Noah, 3 years, and Holly, 4 weeks): I did baby-led attachment because I had a lot of trouble feeding my first baby and getting him to attach and when I saw a video of baby-led attachment it just looked like a natural way to do it, so I thought I would try it to see if that meant that I didn’t have attachment issues with the children I had after my first one.
Miranda (mother of Mattie, 8 years, Tacy, 6 years, Sedna, 7 months): When I had my second baby, when she was born at home and she was lying on me, she all of a sudden attached by herself, which was a wonderful feeling but I never followed-up on it because I didn’t know anything about it. So then when we moved to Australia I so wanted to try it so we tried it with this one. It really started at home, so when we got home we started doing it. You don’t have to do it straight away – baby-led attachment – it’s something that they can do for quite a few weeks after they’re born. It’s imprinted in their being, I guess.
Renee Kam: If a mother wants to do baby-led attachment the tips that I would give her would be the timing of it. So a baby will be able to follow through on their instincts best when they’re calm. So it would be when the baby’s showing early feeding cues such as turning their head from side to side with mouth open, sticking their tongue out, sucking on their hands, or it might be as soon as their baby wakes up from a sleep. So in those situations baby is typically calm and then if the baby is then placed skin-to-skin contact with the mum and the mum, say, is in a semi-reclined position, then that will help a baby to follow through on their instincts to find their mother’s breast.![]()
Narrator: Find a comfortable position. Many mothers find that a semi-reclined position with pillows behind them for support works well. A partially laid-back position allows gravity to assist the baby in moving to the breast. With as much skin-to-skin as possible between you and your baby, place your baby on your chest facing you between your breasts with her head just above your breasts. Start when your baby is calm, such as when she is showing early feeding cues like turning her head from side to side with her mouth open.
As your baby starts to instinctively move towards a breast, she will start to lift her head and bob it around. As she moves towards a breast, you may find it helpful to hug her bottom in close to you and to support her neck and shoulders with your hand and wrist. It is important to avoid putting pressure on her head as she needs her head free to instinctively move it into an extended position to help her attach and feed well.
When her head nears your nipple, she may nuzzle around to find your nipple and bring her tongue toward it. When she finds the right position, she will anchor with her chin, open her mouth wide, attach and begin sucking.
When she finds the right position, she will anchor with her chin, open her mouth wide, attach and begin sucking.
Renee Kam: Straight after a baby is born for the first 1 to 2 hours after they’re born, they’re typically alert and eager and ready to receive their first breastfeed. So when placed into skin-to-skin contact with their mother straight after birth, then that can allow the baby to do baby-led attachment, find the mother’s breasts on their own accord and receive their first breastfeed.
Adele: I did skin-to-skin with all of my children in hospital. So with the baby it probably took a few minutes before like they would kind of just be laying there for a little while and it was a few minutes before they kind of started moving around. But they did the bopping around and choosing a side and finding the nipple and all of that themselves.
Renee Kam: The great news is even if you don’t get to do baby-led attachment straight after a baby is born, babies’ instincts to find a mother’s breasts are easily reproducible for at least the first few months. When a mother and baby are in skin-to-skin contact, there are many benefits of it such as the baby’s heart rate and temperature, blood sugar levels, breathing rate are all kept stable and also when a mother and baby are in skin-to-skin contact it also helps a mother to be able to learn her baby’s feeding cues.
When a mother and baby are in skin-to-skin contact, there are many benefits of it such as the baby’s heart rate and temperature, blood sugar levels, breathing rate are all kept stable and also when a mother and baby are in skin-to-skin contact it also helps a mother to be able to learn her baby’s feeding cues.
Miranda: As with the baby-led attachment, I also did try the mother-led attachment, attachment and feeding and it was quite painful. I went to see a lactation consultant a couple of times for her to help as well. Of course, they have told me to use the baby-led attachment, which was great.
Renee Kam: Even if the mother doesn’t have any breastfeeding problems, by using baby-led attachment frequently, particularly in the early weeks, it can help to reduce the risk of developing any breastfeeding problems such as the baby simply not attaching at all or sore nipples.
Miranda: Persevering with the baby-led attachment actually did help to heal the wounds and I think it was around 3 weeks that we had a happy breastfeeding relationship.
Renee Kam: A mother can do baby-led attachment whenever it’s right for her and her baby to do so. By having done baby-led attachment whenever she feels comfortable to do so, then it means that when she is breastfeeding in public, it makes it easier because baby knows what they’re doing and baby attaches easier to the mum’s breast.
Adele: So I think the baby-led attachment improved my confidence by I was able to see them feeding well, when I could look at them and I could see that they were attached really well and I could hear the swallowing and I knew we were having a good feed and so I didn’t have to really think about what I was doing with them.
Miranda: It helps to know about the fact that everyone is different. With baby-led attachment, it doesn’t matter because babies just go for the breast; they know what to look for.
Renee Kam: Baby-led attachment – it helps a mum and baby get breastfeeding off to a really good start. Then, it may help a mum to be able to breastfeed for as long as she wanted to and reach her own breastfeeding goals.
Then, it may help a mum to be able to breastfeed for as long as she wanted to and reach her own breastfeeding goals.
International BreastFeeding Centre | Breastfeeding videos
Breastfeeding Videos
REALLY GOOD DRINKING
The pause in the chin as the baby opens his mouth to the maximum, just before closing his mouth, indicates his mouth is filling up with milk; the longer the pause, the more milk the baby is taking in. Thus, it is obvious that the advice to feed the baby 20 minutes (10 minutes, 30 minutes, whatever) on each makes no sense. A baby who drinks as this baby drinks for 20 minutes on the first side could easily refuse to take the second side since he would be full. Even a shorter period of time drinking as he does could easily fill him up.
Compare this baby to the baby in the “nibbling” video. The baby in the “nibbling” video could easily spend hours on the breast and not get enough. The whole notion of feeding a baby by the clock makes no sense at all. The pause can also be seen in the first few days of life. See the videos of the 2 day old, 28 hour old and 10 hour old babies
The baby in the “nibbling” video could easily spend hours on the breast and not get enough. The whole notion of feeding a baby by the clock makes no sense at all. The pause can also be seen in the first few days of life. See the videos of the 2 day old, 28 hour old and 10 hour old babies
GOOD DRINKING
Note the position of the baby at the breast. Chin in the breast, nose not touching, baby’s lower lip covering more of the areola with the lower lip than the upper. An asymmetric latch.
The pause in the chin as the baby sucks means the baby just got a mouth full of milk. The longer the pause, the more milk he got.
A baby who drinks like this for 20 minutes straight (for example, we are not recommending feeding by the clock), might not take the other side, he would be full.
Timing feedings makes no sense.
NIBBLING
This baby is eight weeks old and is doing almost no drinking, though very occasionally one sees a short pause in the baby’s chin. A baby who breastfeeds only with this type of sucking could stay on the breast for hours and still not get enough milk. Something needs to be done here and if achieving a better latch, using compression doesn’t help, the baby almost certainly needs to be supplemented. The best way to supplement the baby is with a lactation aid at the breast. Why?
1. Babies learn to breastfeed by breastfeeding
2. Mothers learn to breastfeed by breastfeeding
3. The baby continues breastfeeding and thus continues getting milk from the breast and thus increases the mother’s milk production
4. The baby is not likely to refuse to latch on
5. There is much more to breastfeeding than breastmilk, as important as the breastmilk is
There is much more to breastfeeding than breastmilk, as important as the breastmilk is
See the video clip “Inserting a Lactation Aid”
2 DAY OLD/COMPRESSIONS
The baby in this video is only 40 hours old.
Baby has a pretty good latch. Notice his chin is in the breast, his nose is away from the breast and he covers more of the areola with his lower lip than the upper lip.
During the first part of the video, the baby has an occasional pause in the chin, but is mostly “nibbling” without drinking.
Mother is using compressions, but not always as we recommend. She should compress while the baby sucks, but does not drink and not while he’s not sucking at all.
Compressions at this age (before milk “comes in”), often work only after several series of compressions, unlike later, when the milk supply is greater, when compression usually works immediately.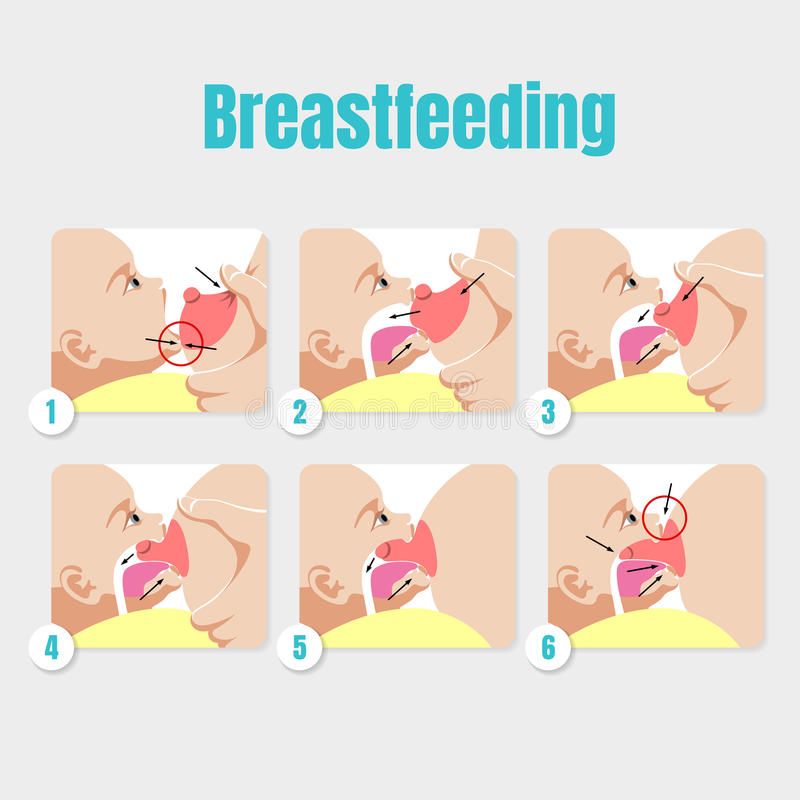
Around 1 minute into the video, the baby starts pulling a little at the breast, becoming impatient with the slow flow.
Then, about 1 minute and 14 seconds, the baby starts to drink vigorously, and you can see several pausing type sucks in a row.
The mother maintains compression until baby no longer drinks, then releases (at 1 minute 30 seconds).
The baby starts sucking again at about 1 minute 37 seconds. Babies who are latched on and hungry will start sucking on their own. No need to tickle their feet or put cold cloths on their foreheads.
Babies do not fall asleep at breast because they are tired, but rather because the flow is slow. How to maintain the flow?
1. A good latch
2. Compressions when the baby is sucking but not drinking
See the how the baby in the video clip Introducing a lactation aid wakes up and drinks vigorously when the flow of milk increases again. Notice around two minute mark, the compression once again works well.
NOT YET LATCHING, FINGER FEED TO LATCH
Finger feeding is to be used primarily to prepare a baby who does not latch on to take the breast.
Note that finger feeding is done only long enough to calm the baby and to get the baby sucking well. This rarely takes more than 60 seconds.
It should not be used as a method of supplementation when the baby does take the breast. In such a case supplementation, if necessary, should be given at the breast with a lactation aid.
We filmed this baby because he had already latched on after being finger fed.
Why did he not latch on to the right side in this video?
• Because he already had fed on the right side, the flow of milk from the breast was slower: babies like fast flow and even if the lactation aid would provide him with more flow, it wasn’t enough
Why did he latch on to the left side?
• Because he hadn’t yet fed on the left side, the breast was “fuller” and the flow was rapid: babies like fast flow
Note that we do not try to force a baby to stay at the breast. If the baby struggles, allows the breast into his mouth but doesn’t suck, or cries, then we let him come away from the breast and try again.
If the baby struggles, allows the breast into his mouth but doesn’t suck, or cries, then we let him come away from the breast and try again.
• If the baby latches on, there is no need to try to force him to stay, he’s latched on
• If the baby does not latch on, trying to force him to stay at the breast is futile and likely to make him angrier or “go limp”
INSERTING A LACTATION AID
This baby needs to receive supplementation. It is best that the baby receive this via lactation aid because:
1. The baby is still on the breast and breastfeeding.
2. Babies learn to breastfeed by breastfeeding.
3. Mothers learn to breastfeed by breastfeeding.
4. The baby is still getting milk from the breast thus helping increase the mother’s milk production.
5. The baby is not likely to reject the breast as he would if he were supplemented by bottle or by any method not on the breast.
6. There is more to breastfeeding than breastmilk; the baby and mother are in close physical contact.
One way to introduce the tube is to insert it while the baby is at the breast as in this video clip. The other is to line up the tube with the nipple and latch the baby on the breast and lactation aid tube at the same time.
Note the position of the baby:
1. The baby’s chin touches the breast but nose does not touch.
2. The baby covers more of the areola with his lower lip than his upper lip.
3. The baby is slightly tilted up towards the mother.
The baby has now fed from both breasts and is not getting much milk flow (mostly nibbling at the breast—see video clips of babies drinking or not drinking). It is time to supplement.
Note the following:
1. The breast tissue is eased out of the way so that the corner of the baby’s mouth is visible.
2. The fact that the baby is tilted slightly upwards makes it easier to find the corner of the baby’s mouth and insert the tube.
3. The tube is inserted in the corner of the baby’s mouth.
4. The tube is pushed almost straight back towards the back of the baby’s throat but also slightly upward toward the roof of the baby’s mouth.
5. The milk moves down the tube to the baby’s mouth, but the baby does not drink (see video clips of babies drinking or not drinking). Something is not working.
6. The mother is attempting compression, but compression should be done when the baby is sucking and not drinking, not when the baby is not sucking at all. Moreover, compression while the baby is being supplemented at the breast with a lactation aid is not necessary.
7. At 21 seconds into the video, I fiddle with the tube placement, and now it starts working. The baby is drinking.
8. Notice the baby pops his eyes open when he starts getting milk again. Babies are not “lazy”; they respond to milk flow. Young babies such as this one tend to fall asleep when the flow of milk is slow, not necessarily if they have had enough.
9. More fiddling with the tube at about 35 seconds. If the baby is well latched on and tube is well placed, supplementing using the lactation aid takes no more time than giving the baby the bottle or finger feeding. Using finger feeding to supplement when the baby takes the breast is not the best approach either.
10. At about 1 minute into the video, I pull the baby’s chin down a bit. Remember, good latch and good placement of the tube make this system work best. Pulling down the chin gets more of the breast into the baby’s mouth.
11. At about 1 minute and 18 seconds, we bring the baby around even more asymmetrically by having the mother push the baby’s bottom in with her forearm.
12. At about 1 minute and 55 seconds, milk comes out of the baby’s mouth means something is not right. Baby has slipped off the breast or the tube has moved. Fiddling with the tube again makes it work properly again.
10 HOUR OLD BABY
This baby is only 10 hours old. Notice the asymmetric latch: chin touches the breast, but not the nose and the baby covers more of the areola with his lower lip than his upper lip. He is also tilted up somewhat towards the mother.
He is drinking milk from the breast. You can tell because of the pause in the chin just as he opens his mouth to its widest before closing again. The pause is subtle here because the baby is getting only small amounts of colostrum—as nature intended! If necessary, compression can help the baby get more milk (see the video clip of the 2 day old baby at this site). The very large amounts of formula an artificially fed baby gets in the first few days is not physiologic or natural or normal or ever been proved to be safe.
BABY 28 HOURS OLD ASSISTED LATCHING
Shows latching on. Not perfect, but good enough. The mother had no pain. It did take two tries to get the baby to latch on, but that’s okay; there’s no point in trying to force a baby who does not take the breast to stay on the breast. It won’t work. Note the baby has an “asymmetric” latch, with the chin touching the breast, the nose not touching the breast, and he covers more of the areola with his lower lip than the upper.
Compressions help the baby get more milk.
BABY 28 HOURS OLD – BABY-LED MOTHER-GUIDED LATCHING
The baby starts searching for the breast. The mother guides him towards the nipple. The baby opens up fairly wide, but the mother does not bring the baby on as well as she could and the baby has a shallow latch. He should have more of the breast in his mouth.
He should have more of the breast in his mouth.
The baby is mostly nibbling at first though there is an occasional pause in the movement of the chin (see other videos showing good drinking).
The mother starts compressing around 1 minute and 10 seconds, and the baby responds by starting to have pausing-types of sucks that indicate he is getting milk well.
BABY-LED MOTHER-GUIDED STARTED UPRIGHT LEFT BREAST, LATCHES
When the baby does not yet take the breast or refuses it completely, this technique can help to put the baby in a state where he can accept the breast. The baby is skin to skin with the mother and indicates when he is ready to search for the breast. When he starts searching, the mother helps him, guiding him toward the breast, supporting his back and neck. The mother is careful not to hold his head. Babies need to have their necks supported but not their heads. See the information sheets The Importance of Skin to Skin Contact and When the Baby Does Not Yet Latch.
The mother is careful not to hold his head. Babies need to have their necks supported but not their heads. See the information sheets The Importance of Skin to Skin Contact and When the Baby Does Not Yet Latch.
4 DAY OLD AFTER TONGUE-TIE RELEASE WITH COMPRESSIONS
The baby just had a tongue tie release.
The mother is doing compressions appropriately. She waits to see if the baby is drinking or not (pause in the chin). If the baby is not drinking, she compresses, holds the compression until the baby stops sucking or stops drinking and then releases. She waits for the baby to start sucking and if the baby starts sucking but does not drink, she repeats the process.
SQUEEZING NIPPLE DEMONSTRATING DIFFERENCE BETWEEN POOR LATCH
When the baby latches on to the nipple only, he gets very little milk.
When the baby latches on where he should, the milk flows rapidly.
CUP FEEDING
A good alternative to the bottle. Particularly useful for the baby who is refusing the breast.
Note that the baby laps the milk up with his tongue. One does not pour the milk down his throat.
JIGGLING AND PULLING
This is an older baby, about 3 or 4 months of age, whose mother’s production has decreased. See the information sheet Slow Weight Gain Following Early Good Weight Gain for some reasons this decrease in milk production might occur. Some of the reasons that may result in a decreased milk production include the mother’s using a hormonal birth control method (including hormone releasing intrauterine devices or intravaginal hormone releasing rings), the mother’s feeding one breast at a feeding “as a rule” instead of “finishing” one side and then offering the other. But the most common reason is the one discussed in the paragraph “This reason (number 11) requires more explanation”.
Some of the reasons that may result in a decreased milk production include the mother’s using a hormonal birth control method (including hormone releasing intrauterine devices or intravaginal hormone releasing rings), the mother’s feeding one breast at a feeding “as a rule” instead of “finishing” one side and then offering the other. But the most common reason is the one discussed in the paragraph “This reason (number 11) requires more explanation”.
The baby is jiggling and unsettled at the breast because the flow of milk is slow. Note that he hardly drinks at the breast (very few pauses, see the videos Really Good Drinking, and Good Drinking), though his chin is a little bit difficult to see.
This sort of behaviour is often said to be due to an over rapid milk flow but by watching the chin one can see that this behaviour in this case is due to too slow milk flow. However, babies pull at the breast more frequently because the flow of milk is slow rather than because the flow of milk is “too rapid”.
Note that giving such babies bottles, may quickly result in their refusing to latch on.
TONGUE–TIE RELEASE
A simple and quick procedure that can make a significant difference in breastfeeding success. The research supporting tongue-tie release is compelling.
VASOSPASM TURNS PINK
This mother’s nipples turn white after baby has finished feeding. They turn white for some time and then eventually turn pink again. This change in colour is sometimes accompanied by throbbing and burning in the nipples. This is often due to poor latching and/or a yeast infection.
If our free resources have been helpful, make a donation today!Support ibc!
Lactation support is not funded by any level of Canadian government. Your support helps us continue to offer the services for which it has become renowned – helping and supporting families to achieve their own breastfeeding goals. It also helps us to provide free support and resources via our website to families and health care providers unable to visit us in person.
Your support helps us continue to offer the services for which it has become renowned – helping and supporting families to achieve their own breastfeeding goals. It also helps us to provide free support and resources via our website to families and health care providers unable to visit us in person.
Individual donations represent the single largest source of support for ibc. Thank you!
Donations can be made at canadianbreastfeedingfoundation.org. Please direct your donation (Fund/Designation) to ibc – The International Breastfeeding Centre.
Charitable tax receipts are available.
Video classes on preparing women for childbirth and breastfeeding
Dear visitors, we invite you to familiarize yourself with video classes on preparing women for childbirth and breastfeeding:
Topics:
1. What a pregnant woman needs to know
https:/ /www.youtube.
 com/watch?v=0hiGCClXywo&list=PLO2-hQiMHj9MHGIXC7Z0D5wEd-t7zxzEP&index=8
com/watch?v=0hiGCClXywo&list=PLO2-hQiMHj9MHGIXC7Z0D5wEd-t7zxzEP&index=8 Conducted by: Botvinyeva Svetlana Viktorovna, psychologist, obstetrician of the antenatal clinic, St. Petersburg City Hospital No. 40
2. Medical genetic counseling. Inheritance of diseases and how to eliminate risks. https://www.youtube.com/watch?v=g3pulJCN1is&list=PLO2-hQiMHj9MHGIXC7Z0D5wEd-t7zxzEP&index=3
Conducted by: Dmitry Maksimovich Botalov, geneticist, City Medical Genetic Center.
3. Preparation for admission to the maternity hospital; 1, 2 and 3 periods of childbirth; How to anesthetize yourself during childbirth; Partner families.
https://www.youtube.com/watch?v=eURchldnekk&list=PLO2-hQiMHj9MHGIXC7Z0D5wEd-t7zxzEP&index=16&t=185s
Conducted by: Pryalukhin Ivan Alexandrovich, candidate of medical sciences, obstetrician-gynecologist, St. Petersburg City Perinatal Center No. 1
4. Therapeutic exercise during pregnancy.
 Women after childbirth. School of motherhood. https://www.youtube.com/watch?v=1d_6K8TKWzU&list=PLO2-hQiMHj9MHGIXC7Z0D5wEd-t7zxzEP&index=19
Women after childbirth. School of motherhood. https://www.youtube.com/watch?v=1d_6K8TKWzU&list=PLO2-hQiMHj9MHGIXC7Z0D5wEd-t7zxzEP&index=19 Conducted by: Nadezhda Stanislavovna Kuritsyna, physiotherapist, St. Petersburg Maternity Hospital No. 100003
5. 10 principles for successful breastfeeding. How to breastfeed correctly? https://www.youtube.com/watch?v=5B7epy2Pwrc&list=PLO2-hQiMHj9MHGIXC7Z0D5wEd-t7zxzEP&index=18
Conducted by: Zheglova Elena Valentinovna, nutritionist, nutritionist, breastfeeding specialist. First GMU them. Academician I.P. Pavlova
6. Breastfeeding: how and when to end it gently and without harm to mother and baby https://www.youtube.com/watch?v=Fb9cCwkbAH0&list=PLO2-hQiMHj9PPokgPmKNw1Pk13wKFszbw&index=11&t=1484s
Conducted by: Semenenko Anna Alexandrovna, psychologist, midwife, specialist in prenatal preparation, lactation and child care consultant 1 year of life
emotional development of the child in the first year of life.

https://www.youtube.com/watch?v=ax-h2N12_zM&list=PLO2-hQiMHj9MHGIXC7Z0D5wEd-t7zxzEP&index=2
Conducted by: Dmitry Khinin, psychologist, St. Petersburg Maternity Hospital No. 10
8. Why is art therapy necessary during pregnancy? Keeping calm in preparation for childbirth https://www.youtube.com/watch?v=4RinNPzkNQk&list=PLO2-hQiMHj9MHGIXC7Z0D5wEd-t7zxzEP&index=4
Conducted by: Chebotareva Ekaterina Petrovna, medical psychologist, Furshtatskaya Maternity Hospital
9. The film "The Miracle of Life"
https://www.youtube.com/watch?v=Lv5XvI_DnM0&list=PLO2-hQiMHj9MHGIXC7Z0D5wEd-t7zxzEP&index=6CITY CENTER FOR MEDICAL PREVENTION/ #rugsmp. GCMP #PregnancyPregnancy #Pregnancy
Breastfeeding with pierced, flat or inverted nipples
The shape and size of nipples can vary greatly from woman to woman. Our practical tips will help you make breastfeeding easier, no matter what your nipples are.
Share this information
Most women's nipples protrude, enlarge and swell when touched, but some have flat or even inward nipples. In addition, some women pierce one or both nipples. Usually flat, inverted or pierced nipples do not cause problems when breastfeeding, but in some cases additional help may be needed. nine0071
“Don't panic if you have flat or inverted nipples. As a rule, this does not interfere with breastfeeding in any way,” says Shawnad Hilton, a lactation consultant, health visitor and newborn care specialist who has worked with Medela in the UK for more than a decade. “Remember that your baby takes into his mouth not only the nipple, but also part of the breast.”
However, in the early days, when the baby's mouth is still very small and suckling skills have not developed, inverted or flat nipples can make feeding difficult, especially if the baby is unwell or born prematurely. nine0071
“Flat or inverted nipples may not reach the baby's palate and therefore not trigger the sucking reflex,” Schoned explains. “That is, the baby may have trouble grasping and holding the breast in the mouth, and the baby will not get enough milk.”
“That is, the baby may have trouble grasping and holding the breast in the mouth, and the baby will not get enough milk.”
How to tell if you have flat or inverted nipples
Flat nipples 1 do not protrude much from the areola (the darker
area surrounding the nipple) even when stimulated.
Inverted nipples seem to be recessed in the center. They may look like this all the time or only if they are stimulated. Sometimes inverted nipples are on the same level with the areola, and sometimes even sink deep into the breast tissue. nine0071
This feature may occur on one or both nipples. It is estimated that approximately 10% of nulliparous women have at least one retracted nipple. 2 If you're not sure what type of nipples you have, try a simple pinch test: Gently squeeze your breast with your thumb and forefinger on both sides of the areola. The nipple should come forward. If your nipple hides inside, creating a depression, then it is retracted.
Preparing inverted and flat nipples during pregnancy
You may have noticed that your breasts have changed during pregnancy and your nipples have become more protruding. If this does not happen and you are worried that the shape of your nipples will make breastfeeding difficult, try using nipple formers* in consultation with your doctor. These are soft and flexible silicone discs that are discreetly placed in the bra and slightly squeeze the nipples, helping to pull them out.
“In a normal pregnancy, nipple formers can be worn as early as 32 weeks,” advises Schoned. - Start wearing them for an hour a day, gradually increasing the time to eight hours. If you have an incompetent (weakened) cervix or are at risk of preterm labor, check with your healthcare provider about when you can start using shapers, as nipple stimulation can trigger contractions.” nine0071
“Nipple formers can continue to be worn after childbirth,” adds Schoned. “Try to put them in a bra 30 to 60 minutes before feeding. ”
”
“I have inverted nipples, and after two or three weeks of constantly trying to latch on, I almost switched to formula,” recalls Nina, a mother from Germany. “I turned to La Leche Liga for help, and one nice woman came to me and supported me to continue to feed. She suggested trying nipple shapers and they really helped me. Somehow my baby began to understand what to do! Breastfeeding went well and I nursed him until he was 21 months old.” nine0071
How to help your baby latch on to flat or inverted nipples
If your baby enjoys sucking on your thumb but isn't as interested in your breast, chances are your nipple isn't reaching the palate. The baby may become nervous, push off the breast and cry or even fall asleep on your chest. If this happens, ask a lactation consultant or healthcare professional to check the grip.
There are several tricks you can use before each feed to make your nipples more comfortable to latch on to. Schoned recommends the following:
- twist the nipple between thumb and forefinger so that it protrudes better;
- place your fingers in a "V" or "C" shape and squeeze the breast just behind the areola to push out the nipple;
- apply a cold compress or ice cube to the nipple to push it forward;
- Express milk manually or with a breast pump for a couple of minutes before feeding so that the nipple comes out more.

“I had a flat nipple but I only found out when I noticed that Austin was having a hard time sucking on that side,” says Jennifer, mother of two in the UK. “From an anatomical point of view, there is nothing abnormal in this, it’s just that my nipple does not protrude so much, and this requires some skill when feeding. Before giving this breast, I always pinched and squeezed the nipple a little and tried to put it into the baby's mouth. It was a little difficult at first, but over time I learned.” nine0071
Using nursing pads
If none of the above work and your baby still has difficulty latch-on, your lactation consultant or healthcare professional may recommend that you breastfeed with a nursing pad*. They are thin and flexible nipple-shaped silicone funnels with holes at the tip through which milk will flow.
It is easier for the baby to put the feeding pad in his mouth, as it is larger and more rigid. In addition, such an overlay will reach him to the sky, causing a sucking reflex. Do not use nursing pads for a long time. If you experience pain or other problems, contact your lactation consultant or healthcare professional to check that your baby is latching on properly with a breastfeeding pad. You will also need to monitor your baby's weight gain to ensure that milk production is meeting his needs. nine0087 3
Do not use nursing pads for a long time. If you experience pain or other problems, contact your lactation consultant or healthcare professional to check that your baby is latching on properly with a breastfeeding pad. You will also need to monitor your baby's weight gain to ensure that milk production is meeting his needs. nine0087 3
Over time, as your baby learns to suckle properly and your nipples get used to breastfeeding, you will be able to breastfeed without breast pads.
“My nipples are pretty flat. The doctor advised me nursing pads, and I was successfully able to feed my two babies,” says Ann-Sophie, mother of two from Sweden. “My secret is to make them adhere better to the skin, I lightly wet the edges before use.”
Breastfeeding with pierced nipples
Many women with pierced nipples find it does not affect their ability to breastfeed. However, jewelry must be removed before feeding, as the child may choke on them or injure their tongue, gums or palate.
“I had a nipple piercing, but I got it off a year later when I got pregnant because my breasts were very sensitive,” says Kelly, mother of three from the UK. “I breastfed my daughter exclusively, and then her two younger brothers, and never had any problems. And the pierced nipple was my favorite!” nine0071
Some women report that milk can leak from piercings, while others believe that piercing scars reduce milk production 4 - but this has not been well researched.
“You can't predict how a piercing will affect breastfeeding until milk production begins,” Schoned explains. - If you are concerned, talk to a lactation consultant or healthcare professional. And remember that one breast may be enough for babies to get the nutrition they need if there are problems with the second. ” nine0071
What to do if you can't breastfeed with flat or inverted nipples
If you've tried all the options and still can't breastfeed, you still shouldn't deprive your baby of breast milk.
“Mom and baby's health is the most important thing,” says Schoned. “Maybe you should switch to full pumping and feed your baby only pumped milk. You can also try the supplemental feeding system** where the baby continues to feed at the breast while receiving additional expressed milk through a tube. That is, the baby will still suck on the breast and stimulate the production of milk, which, in turn, will help you pump even more.” nine0071
“I have inverted nipples. After the disastrous experience of breastfeeding my first son with my second, I decided to get my way after all,” says Babettli, mother of two from Italy. - On the advice of experts, I tried nipple formers and nursing pads, but everything was unsuccessful. In the end, pumping with the Medela Symphony*** Double Electronic Clinical Breast Pump proved to be the best solution for us. I fed exclusively on expressed milk for up to four months.” nine0071
Care for different types of nipples
Flat or inverted nipples may require extra care as the baby may squeeze them harder and they may become inflamed at first. Tips on how to care for sore nipples can be found in Nursing Nipple Care.
Tips on how to care for sore nipples can be found in Nursing Nipple Care.
If your nipples become inverted after a feed, any moisture can lead to inflammation and increase the risk of infections, including thrush. Blot your nipples dry after each feed before they have time to hide inside. nine0071
With swelling of the mammary glands, when even protruding nipples can become flat, flat or inverted nipples can be difficult. Read the helpful tips in the article on breast swelling.
The good news is that continuous breastfeeding or pumping can change the shape of your nipples and breastfeeding will become easier over time. With the arrival of the next child, you may not have to face this problem at all, as happened with Leanne, a mother of two from the UK. nine0071
“The second feeding was like a fairy tale,” she says. “After almost four months of pumping for my first son, my flat nipples were so extended that with my second son I no longer had to use breast pads - he was able to suck directly from the breast. The youngest is now nine months old and I still breastfeed him.”
The youngest is now nine months old and I still breastfeed him.”
Literature
1 Pluchinotta AM. The Outpatient Breast Clinic. Springer International Publishing ; 2015. - Pluchinotta A.M., "Treatment of breast diseases on an outpatient basis". Springer International Publishing. 2015.
2 Alexander JM, Campbell MJ. Prevalence of inverted and non-protractile nipples in antenatal women who intend to breast-feed. The Breast . 1997;6(2):72-78. — Alexander JM, Campbell MJ, "Prevalence of inverted and intractable nipples in pregnant women who intend to breastfeed." nine0174 Ze Brest (Chest). 1997;6(2):72-78.
3 McKechnie AC, Eglash A. Nipple shields: a review of the literature.Breastfeeding Medicine. 2010;5(6):309-314. — McKechnie A.S., Eglash A., "Nipple Covers: A Review of the Literature". Brestfeeding Medicine (Breastfeeding Medicine).