New baby feeding problems
Common breastfeeding problems - NHS
If you have any problems with breastfeeding, it's important to ask for help from your midwife, health visitor or a breastfeeding specialist as soon as possible.
That way issues like sore nipples or breast engorgement can be sorted out early.
Here are some of the problems breastfeeding mums sometimes have, plus tips on how to tackle them.
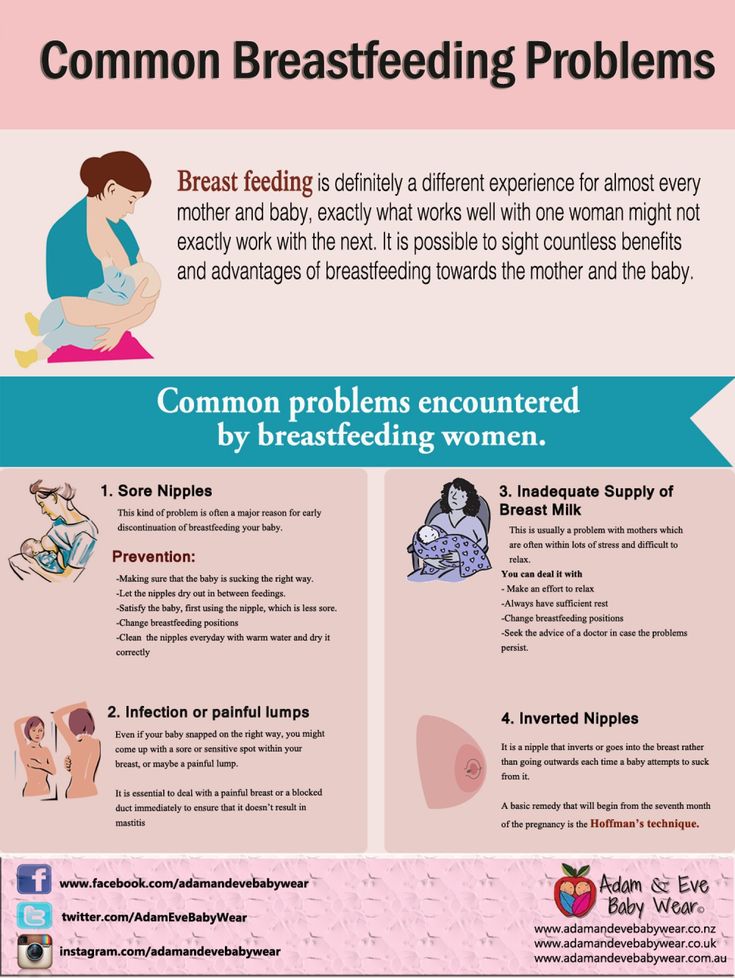
Sore or cracked nipples
Sore nipples usually happens because your baby is not well positioned and attached at the breast.
Putting up with it could make pain or discomfort worse, so it's important to get help from your midwife, health visitor or breastfeeding specialist as soon as you can.
See more advice on sore nipples.
Not enough breast milk
When you first start breastfeeding, you may worry that your baby is not getting enough milk. It can take a little while before you feel confident that your baby is getting what they need.
Learn the signs that your baby is getting enough milk.
Offering your baby both breasts at each feed and alternating which breast you start with will help to stimulate your milk supply. So will keeping your baby close and holding them skin to skin.
Speak to your midwife, health visitor or a breastfeeding specialist if you're worried your baby is not getting enough milk.
Breast engorgement
Breast engorgement is when your breasts get too full of milk. They may feel hard, tight and painful.
Engorgement can happen in the early days when you and your baby are still getting used to breastfeeding. It can take a few days for your milk supply to match your baby's needs.
Engorgement can also happen when your baby is older and not feeding so frequently, perhaps when they start having solid foods.
See how to manage breast pain while breastfeeding.
Baby is not latching on properly
Breastfeeding is a skill that you and your baby need to learn together. It may take you both a while to get the hang of it.
If you are finding breastfeeding painful or your baby does not seem to be satisfied after feeds, they may not be latching onto the breast properly.
Find out how to latch your baby on.
Learn the signs that your baby is well attached.
Video: How do I know if my baby is properly latched?
In this video, a midwife talks about how to check if your baby is latched on properly when breastfeeding.
Media last reviewed: 4 October 2022
Media review due: 4 October 2025
Too much breast milk
Occasionally women make too much breast milk and their babies struggle to cope.
It's best to get your midwife, health visitor or breastfeeding specialist to watch a feed to see if they can spot why this is happening. They can also show you different positions to help your baby cope with large amounts of milk.
Breastfeeding and thrush
Thrush infections can sometimes happen when your nipples become cracked or damaged. This means the candida fungus that causes thrush can get into your nipple or breast.
If you suspect you or your baby has a thrush infection, see your health visitor or GP.
See how to spot the signs of thrush while breastfeeding.
Blocked milk duct
If breast engorgement continues, it can lead to a blocked milk duct. You may feel a small, tender lump in your breast.
Frequent feeding from the affected breast may help. If possible, position your baby with their chin pointing towards the lump so they can feed from that part of the breast.
If possible, position your baby with their chin pointing towards the lump so they can feed from that part of the breast.
See more help for breast pain, including pain from blocked milk ducts.
Mastitis
Mastitis (inflammation of the breast) happens when a blocked milk duct is not relieved. It makes the breast feel hot and painful, and can make you feel very unwell with flu-like symptoms.
It's important to carry on breastfeeding. Starting feeds with the tender breast may help.
See more help for breast pain, including pain from mastitis.
If you are no better within 12-24 hours, or if you feel worse, contact your GP or out-of-hours service as you may need antibiotics.
Breast abscess
If mastitis is not treated, or if it does not respond to treatment, it can lead to a breast abscess, which may need an operation to drain it.
Read more about breast abscesses.
Breastfeeding and tongue tie
In some babies, the strip of skin that attaches the tongue to the floor of the mouth (frenulum) is shorter than usual. This is known as tongue tie.
Some babies who have a tongue tie do not seem to be bothered by it. In others, it can stop the tongue moving freely, which can make it harder for them to breastfeed.
The good news is that tongue tie easily treated.
Find out more about tongue tie
Got a breastfeeding question?
Chat to the Start4Life Breastfeeding Friend chatbot on Amazon Alexa, Facebook Messenger or Google Home for fast, friendly, trusted NHS advice anytime, day or night.
How to tell if your baby has a feeding problem
COVID-19 Information Center: get the latest on vaccines, testing, screening, visitor policy and post-COVID support >>
Back to Healthy Driven Blog Home
November 26, 2019
|
by Alexis Rodriguez, M. D.
D.
Categories: Healthy Driven Moms
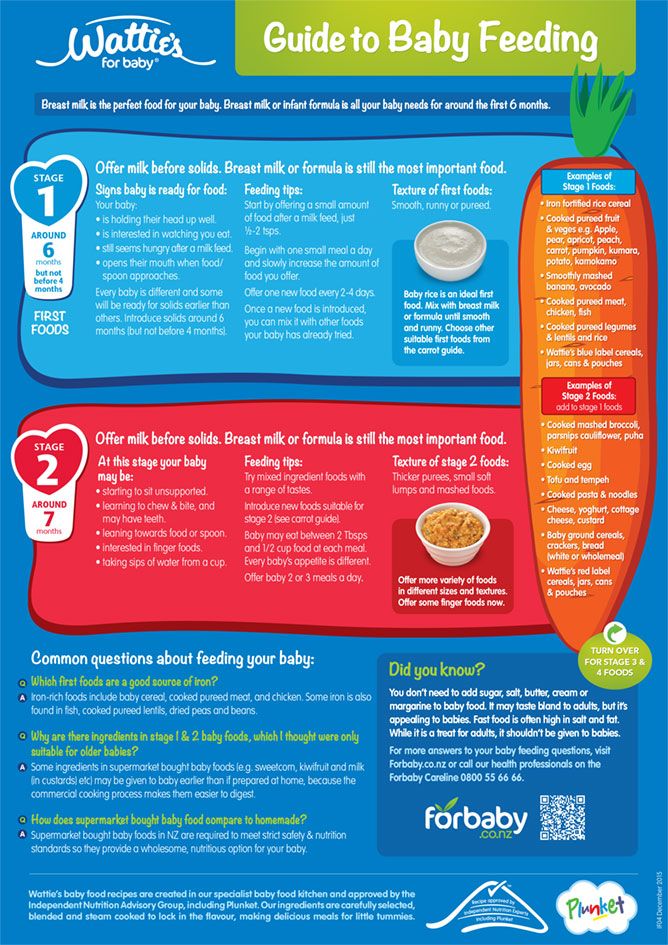
Some babies have trouble eating and drinking at first. They may spit up, avoid new foods or refuse to eat certain foods. They may have trouble holding food and liquid in their mouth. These issues are usually normal and temporary.
A child with a feeding problem or disorder will keep having trouble. Twenty-five percent of all children will experience feeding difficulties during infancy and early childhood that can affect their overall health and development.
When a baby doesn’t like solids, it’s easy to assume they are a “picky eater.” But poor feeding is different from picky eating, which doesn’t usually start until your baby becomes a toddler. A baby may have a feeding problem when they can’t eat or drink enough of the right things to stay healthy.
Feeding problems may include difficulty swallowing, called dysphagia. This is the inability of food or liquid to pass easily from the mouth to the throat, through the esophagus and into the stomach. Dysphagia can result in aspiration, which may cause pneumonia and/or other serious lung conditions.
Dysphagia can result in aspiration, which may cause pneumonia and/or other serious lung conditions.
How do you know if your baby has a feeding problem or disorder? Some common red flags include:
- Refuses to eat and drink
- Isn’t gaining weight or growing as expected
- Arches back or stiffens when feeding
- Cries or fusses when feeding
- Regularly takes a long time to eat (more than 30 minutes)
- Falls asleep or isn’t alert when feeding
- Avoids foods with certain textures
- Drools a lot, coughs or gags when feeding
- Has problems chewing and swallowing
- Has trouble breathing while eating and drinking
- Frequently spits up or vomits
- Has a hoarse or raspy voice during or after feeding
Feeding difficulties in babies may happen because of breastfeeding challenges. Lactation consultants can teach you how to feed your baby and help with latching difficulties, painful nursing, low milk production and other issues.
Poor feeding may also be caused by temporary illnesses, including ear infections and colds. These can make feeding uncomfortable for babies and will normally stop when the illness is treated. Other factors that may affect a baby’s ability to feed are stress, pain from teething and medication side effects.
Babies with certain health problems or conditions may also have feeding difficulties. Some possible causes for infant feeding and swallowing problems include:
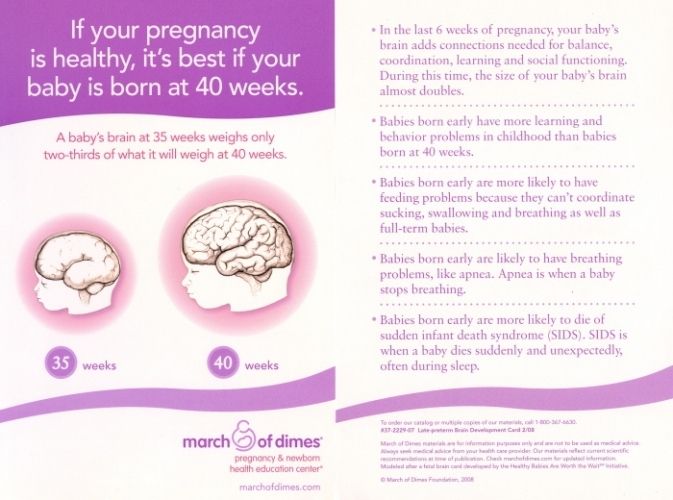
- Prematurity, low birth weight
- Certain traumatic birth injuries (cerebral palsy)
- Structural abnormalities (cleft lip, cleft palate)
- Reflux or other stomach problems
- Lung or respiratory problems (asthma)
- Heart disease
- Nervous system or muscle problems (muscular dystrophy)
- Developmental delays or disabilities (autism)
If left untreated, feeding problems can negatively affect your baby’s health. Malnutrition is a top concern. Babies need to feed and digest the necessary nutrients to develop and grow properly. If they don’t get the necessary nutrition, it can lead to a condition known as failure to thrive.
Babies need to feed and digest the necessary nutrients to develop and grow properly. If they don’t get the necessary nutrition, it can lead to a condition known as failure to thrive.
Feeding issues can also put infants at risk for dehydration, aspiration, pneumonia or other lung infections, and delayed physical and mental development which can lead to speech, cognitive and behavioral problems.
The earlier the problem is addressed, the better the long-term outcome. Treatment for feeding disorders varies based on what’s causing the issue and the symptoms involved. A team approach, including the child’s doctor, dietitians and speech-language pathologists, is often the best way to treat these issues.
For instance, babies and children with dysphagia are often able to swallow thick fluids and soft foods better than thin liquids. A speech-language pathologist can suggest techniques for feeding that may help improve swallowing problems.
Treatment may also include medicines for reflux, trying different foods or textures, changing the temperature of food, changing the feeding schedule (e. g., smaller, more frequent meals), changing your child’s position while eating, and/or switching feeding methods. In severe cases, your child may need to get nutrition in other ways, such as through a feeding tube.
g., smaller, more frequent meals), changing your child’s position while eating, and/or switching feeding methods. In severe cases, your child may need to get nutrition in other ways, such as through a feeding tube.
If you think your baby is having trouble with feeding, let your child’s doctor know right away. While feeding problems are usually minor, your doctor will want to rule out an underlying medical issue.
Some warning signs of feeding problems include wetting fewer than four diapers per day, infrequent or hard stools in the first month, your baby becomes more yellow instead of less during the first week.
If your baby shows any signs of emergency, such as a fever over 100 degrees, wheezing, bloody vomit or stool, or constant crying, get immediate medical attention. Signs of an allergy or digestive disturbance include vomiting after feeding, frequent loose or watery stools, blood in the stools or a severe skin rash.
The Edward-Elmhurst Health Pediatric Feeding Clinic takes a comprehensive approach to the full spectrum of feeding disorders in children of all ages and concentrates on feeding, nutrition and growth. Our multidisciplinary team includes a pediatric dietitian, pediatric speech-language pathologist, pediatric gastroenterologist and a pediatric nurse. For questions, please call 630-527-5409.
Our multidisciplinary team includes a pediatric dietitian, pediatric speech-language pathologist, pediatric gastroenterologist and a pediatric nurse. For questions, please call 630-527-5409.
Explore children’s services at Edward-Elmhurst Health.
Related blogs:
Should I be worried about my baby’s growth?
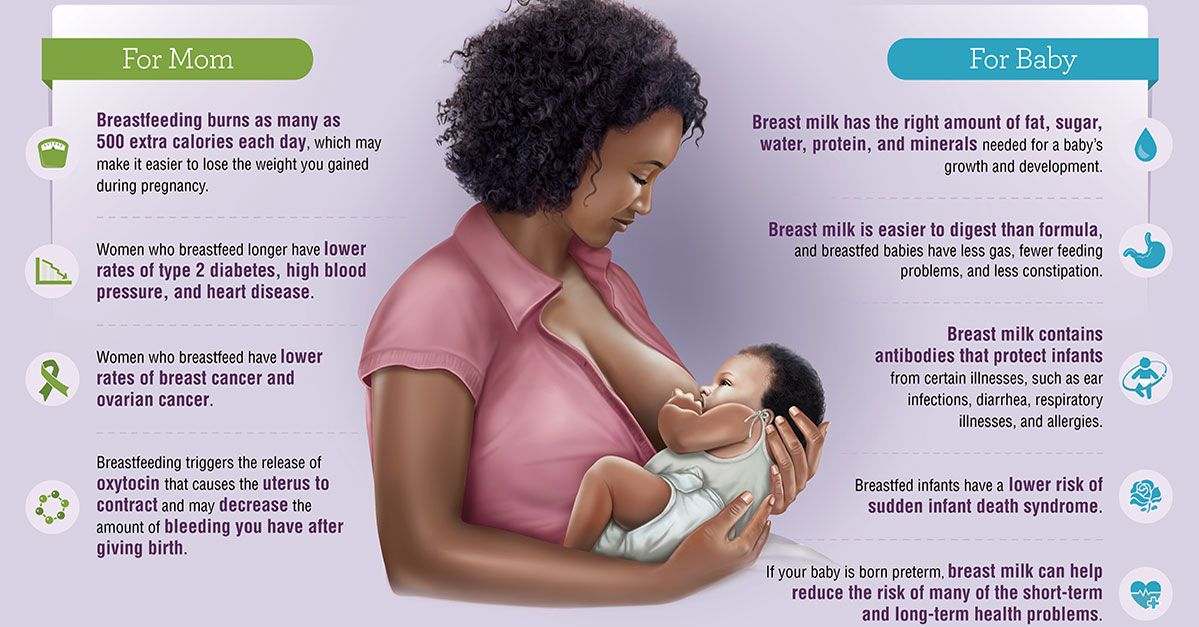
Breast or bottle? Which will you choose?
Is my newborn normal?
The diseases you may have forgotten about, thanks to vaccines
What to do if your teen is being cyberbullied
Halloween without the health scare
Featured Expert
Alexis Rodriguez, M.D. Specialty: Pediatric Gastroenterology
Dr. Rodriguez specializes in pediatric gastroenterology. Read More >>
Read More >>
Blog Category
Healthy Driven Stories with Mary Lou Mastro
Our very own President & CEO Mary Lou Mastro will post about what our patients want to know, from the latest buzz in our hospitals to what’s new in health care.
Healthy Driven Life
We’ve got fresh new ideas about how to lead a healthier life! Our physicians and other experts will post about exercise and fitness, recipes, wellness advice and more.
Healthy Driven Heroes
Our stories about patients who bravely and proactively improved their health, and the caregivers who helped them along the way, are sure to motivate and inspire.
Healthy Driven Moms
Our physicians and other experts will post about all things moms and moms-to-be want to know.
Healthy Driven Cancer Fight
Our physicians and other experts will post about issues that matter most to people affected by cancer.
Healthy Driven Hearts
Our physicians and other experts will post about the latest treatments and more for living a heart healthy life.
Healthy Driven Minds
Our physicians and other experts will post about improving mental health and well-being.
Healthy Driven Voices of Diversity
By creating platforms and opportunities that allow us to come together, we can begin to know and understand each other.
Healthy Driven Community
Read stories that illustrate our commitment to keeping our community healthy.
Healthy Driven Chicago®
Our physicians and other experts will post about the steps you can take today to stay healthy and fit for years to come.
Solutions to six breastfeeding problems in the first week
Are you having difficulty breastfeeding your newborn baby? Read on for expert advice on tackling the main challenges of the first week of breastfeeding.![]()
Share this information
Cathy Garbin, child health nurse, midwife and lactation consultant:
Cathy, a mother of two, was a research fellow at the renowned Human Lactation Research Institute, founded by Peter Hartmann, for seven years, providing support to breastfeeding mothers in clinics and at home. Today, she still works as a family counselor, and also conducts seminars for attending physicians and speaks at international conferences.
Breastfeeding is not always easy, so if
you are having difficulty, know that you are not alone. A US study found that out of 500 new mothers surveyed, 92% experienced breastfeeding problems by the third day. 1 Fortunately, most early breastfeeding problems are easy to resolve. Below you can read recommendations for solving the main problems that mothers often face in the first week of feeding.
Problem #1. Breastfeeding hurts!
Pain during feeding is usually associated with tenderness or inflammation of the nipples, especially when milk "comes" on the second to fourth day after birth. 2 The baby will beg for a breast every couple of hours, and this can quickly aggravate the problem: some mothers' nipples crack, bleed, or blister. This is, of course, very annoying.
2 The baby will beg for a breast every couple of hours, and this can quickly aggravate the problem: some mothers' nipples crack, bleed, or blister. This is, of course, very annoying.
Solutions 3
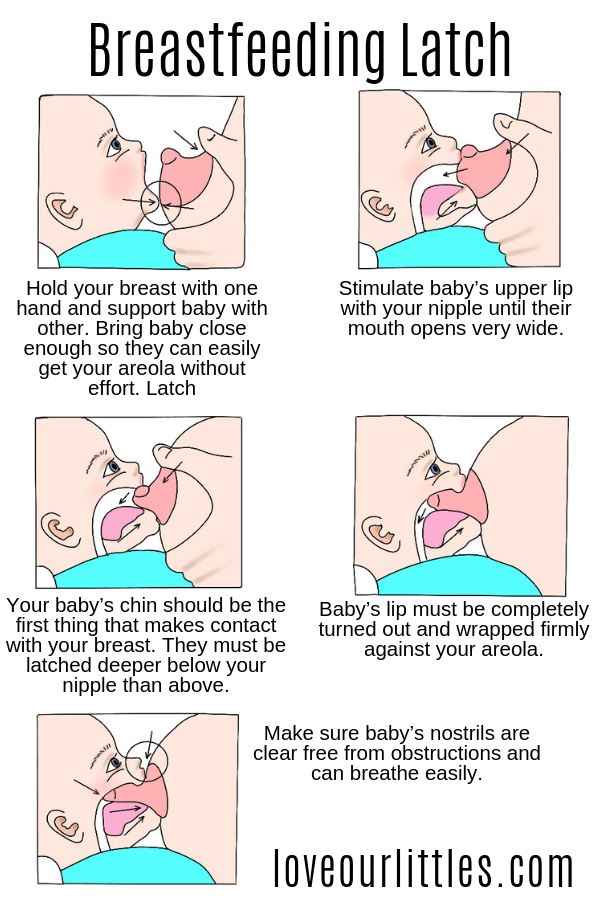
- Check how the baby latch on. An incorrect latch is one of the most common causes of pain during breastfeeding. A newborn baby should take most of the lower half of the areola (dark skin around the nipple) into his mouth, and your nipple should rest against his palate, supported from below by the tongue.
- Contact a lactation consultant or healthcare professional to make sure your baby's mouth and torso are properly positioned during feeding and there are no other latch-on problems. The doctor may also examine the baby's mouth for physical abnormalities.
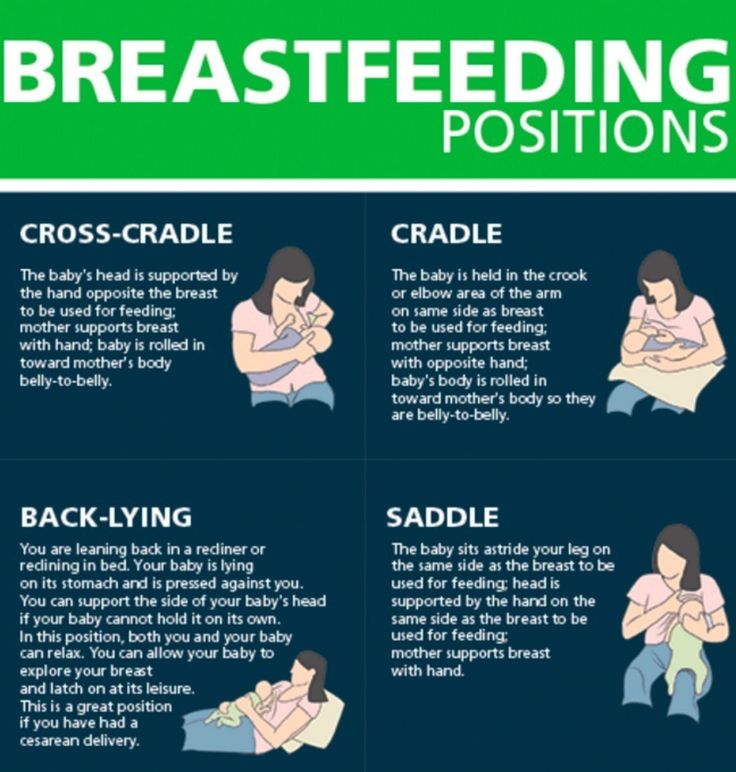
- Try other feeding positions. Reclining, cross cradle, underarm, or lying positions can relieve pressure on the most painful areas of your breasts.

- Gently wipe soaked nipples with water-dampened cotton swabs after each feed to remove milk residues that can cause infection.
- Air dry nipples or blot with a clean, soft muslin or flannel cloth to prevent bacterial growth in a humid environment. Use disposable or reusable bra pads to absorb leaking milk and remember to change them regularly.
- Soften your nipples. An ultra-pure lanolin treatment will help relieve inflammation and dry skin. You can also apply a few drops of your own breast milk to your nipples. In both cases, you do not have to wash your breasts before the next feeding. You can also apply refrigerated hydrogel pads* to your nipples. They soothe the nipples and help relieve pain during feeding, as well as speed up healing.
- Protect your nipples. Nipple shields* protect the sore area from rubbing against clothing.
- Be patient. The inflammation usually resolves after a few days as your body adjusts to breastfeeding and your baby learns to suckle.

- Seek medical attention, if pain during feeding does not go away after a few days. Constant inflammation of the nipples may indicate an infection that requires prompt treatment.
Problem #2. Baby doesn't latch on properly
Some newborns do not latch on properly right away. Maybe both of you just need more time to learn how to breastfeed, or maybe the baby was born prematurely, feels unwell after a difficult birth, or mom has flat or inverted nipples.
Solutions
- Contact a lactation consultant or healthcare professional who can help identify the cause of the problem and suggest solutions.
- Flat or inverted nipples must be pulled out. Nipple formers* fit comfortably in the bra and apply gentle pressure to the nipples to help them come out for easier feeding.
- Try different positions and ways to support your newborn. The baby needs to feel supported.
 He must be comfortable and breathe freely in order to suckle properly. Do not hold the child by the head and do not put pressure on it. Lean back and let your child take the lead. This stimulates his natural reflexes and helps him find and latch on to his breasts. 4
He must be comfortable and breathe freely in order to suckle properly. Do not hold the child by the head and do not put pressure on it. Lean back and let your child take the lead. This stimulates his natural reflexes and helps him find and latch on to his breasts. 4 - When feeding, try to find the optimal position. Instead of putting your baby on and off, stressing both of you, try to position him in a way that is easy and comfortable for him. Hold the torso and legs of the baby close to you, support him by the shoulders and hold him firmly so that he feels safe. Let the baby's head rest freely on your arm so that he can tilt it back slightly and breathe freely. The chin should be pressed against your chest. If these small adjustments don't make feeding more comfortable for your baby, seek help from a lactation consultant or healthcare professional.
- Use nursing pads. If your baby is having difficulty latch-on, a lactation consultant or healthcare professional may suggest trying nursing pads*.
 A nipple with an overlay is more convenient to take in the mouth, so it is larger and more rigid. Do not use nursing pads for a long time.
A nipple with an overlay is more convenient to take in the mouth, so it is larger and more rigid. Do not use nursing pads for a long time.
Problem #3. Not enough breast milk
You will produce little breast milk at the very beginning, as the hormonal changes that trigger milk production occur slowly and do not end until the second or fourth day after birth. 2 You may be worried that your baby is not getting enough milk, but in the early days his stomach is still too small and feedings are frequent, so don't worry. The only things to worry about these days are excessive weight loss, too few wet and soiled diapers, or signs of dehydration in the baby. For more information on how often a newborn should urinate and void, see Breastfeeding Newborns: What to Expect in the First Week.
Solutions
- Contact a Lactation Consultant or your healthcare provider who can determine if you have problems with milk production.
 The sooner you do this, the better.
The sooner you do this, the better. - Feed your baby on demand, not on a schedule. In the first week after birth, your baby will ask to breastfeed every two to three hours (or more often!), both day and night. Such frequent feeding helps to establish the production of breast milk.
- Take care of yourself. It's not always easy with a newborn, but try to rest whenever you can, eat right, and accept any help around the house or with older children that your loved ones can give you to fully focus on breastfeeding.
- Try expressing milk. If a baby is feeding frequently but not gaining any weight, a lactation consultant or doctor may recommend pumping to increase breast milk production. If milk is not coming out at all, you can try the Medela Symphony Dual Electric Clinical Breast Pump**. It features an Initiate program that mimics a baby's natural sucking rhythm for the first few days.
Problem #4.
 Breast full and heavy
Breast full and heavy Your breasts will become fuller and heavier as milk comes in.
If the baby suckles well and often, this should not cause any problems. However, in some women, the breasts become so full that they become hard and painful. This condition, called breast swelling, can cause discomfort. The swollen chest seems to be “burning”, now all the activity of your body is concentrated in it, resembling a busy traffic at rush hour. Fortunately, this condition usually resolves within 24 to 48 hours. However, due to the swelling of the mammary glands, the nipples can become flat and the baby may have difficulty latch-on. 5
Solutions
- Feed your baby often. Try to breastfeed at least 8-12 times a day. This is the main way to alleviate this condition. For more tips and tricks, see the article on Breast Swelling. 6.7
- Call your healthcare provider, if symptoms persist for more than 48 hours, you have a fever, or your baby is unable to breastfeed due to swelling.

Problem #5. Milk is leaking
Breast leakage is very common in the early days of breastfeeding when milk production begins. Milk may leak from one breast while you are feeding the other, when you sleep on your stomach, or when something accidentally triggers the milk flow reflex, such as when you hear a baby crying in a store. The leakage usually stops after about six weeks.
Solutions
- Protect clothes from stains will help disposable or reusable bra pads to be used day and night.
- Don't waste precious drops! Breast milk collection pads* fit inside the bra and allow you to collect any leaking milk. This is a very useful thing when there is too much milk and the pads are not absorbing well, or when one breast is leaking while you are feeding the other. If you want to save the collected milk, use only the milk collected at the feeding. Place it in a sterile container and refrigerate immediately if you are not supplementing with it right away.
 Collected milk must be used within 24 hours. The breast milk collection sleeves should not be worn for more than two to three hours at a time.
Collected milk must be used within 24 hours. The breast milk collection sleeves should not be worn for more than two to three hours at a time.
Problem #6. There seems to be too much milk
Sometimes when milk comes in, too much is produced! In the first few weeks there may be an overabundance of milk, but usually everything returns to normal soon. 7 Up to this point, the breasts may be heavy and sore almost all the time, even immediately after a feed, and a lot of milk may leak. A strong flush can cause a baby to cough or choke, vomit immediately after a feed, have tummy discomfort, or have hard, frothy, greenish stools. These are all signs that you are having too much milk, but the problem may resolve itself as your breasts get used to the new function.
Solutions
- Express some milk by hand at the beginning of each feed to ease the force of the flush.
- Try to feed while leaning back: this will help your baby control the flow of milk.
 The "cradle" position is also good: hold the baby obliquely by the shoulders so that the head can lean back slightly while on your arm. The torso of the baby will be located diagonally on you.
The "cradle" position is also good: hold the baby obliquely by the shoulders so that the head can lean back slightly while on your arm. The torso of the baby will be located diagonally on you. - Be kind and patient. Let your baby rest and absorb milk both during and after feeding. Don't move your baby too much or too fast, as this can make him nauseous. As the baby grows, he will learn to better cope with the rush of milk, which is likely to weaken anyway.
- Use the towel or swaddle to soak up spilled milk if the baby can't handle the flush, and place the breast milk collection pad on the other breast to catch any spilled milk.
- Contact a lactation consultant or doctor if problems persist after a few weeks . He will examine you and may suggest one-sided feedings or hourly breast changes (“breast duty”) to reduce your milk supply.
Related materials: Difficulties in breastfeeding in the next few weeks and problems with breastfeeding after the first month
Literature
1 Wagner EA et al. Breastfeeding concerns at 3 and 7 days postpartum and feeding status at 2 months. Pediatrics . 2013: peds -2013. - Wagner I.A. et al., "Breastfeeding Problems at Days 3 and 7 of a Baby's Life and Type of Feeding at 2 Months of Age". Pediatrix (Pediatrics). 2013:e865–e875.
Breastfeeding concerns at 3 and 7 days postpartum and feeding status at 2 months. Pediatrics . 2013: peds -2013. - Wagner I.A. et al., "Breastfeeding Problems at Days 3 and 7 of a Baby's Life and Type of Feeding at 2 Months of Age". Pediatrix (Pediatrics). 2013:e865–e875.
2 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J Mammary Gland Biol Neoplasia 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." G Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
3 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women ’ s 2007;52(6):638-642. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
— Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
4 Colson SD et al. Optimal positions for the release of primitive neonatal reflexes stimulating breastfeeding. Early Hum Dev . 2008;84(7):441-449. - Colson S.D. et al., "Optimal Positions for Provoking Primitive Innate Reflexes to Induce Breastfeeding." Airlie Hume Dev. 2008;84(7):441-449.
5 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe Frauenheilkd. 2013;73(12):1202-1208. - Jacobs A. et al., "Recommendations S -3 for the treatment of inflammatory diseases of the breast during breastfeeding. Geburtskhilfe und Frauenheilkünde. . ABM Clinical Protocol# 4: Mastitis , Revised March 2014. Breastfeed - 9020: 5): 5) H., Academy of Breastfeeding Protocol Committee, AVM Clinical Protocol #4: Mastitis, March 2014 edition of Brestfeed Med (Breastfeeding Medicine). 2014;9(5):239-243.
Breastfeed - 9020: 5): 5) H., Academy of Breastfeeding Protocol Committee, AVM Clinical Protocol #4: Mastitis, March 2014 edition of Brestfeed Med (Breastfeeding Medicine). 2014;9(5):239-243.
7 Academy of Breastfeeding Medicine Protocol Committee. ABM clinical protocol # 20: Engorgement. Breastfeed Med . 2009;4(2):111-113. - Protocol Committee of the Academy of Breastfeeding Medicine, "AVM Clinical Protocol No. 20: Engorgement, Revision 2016". Brestfeed Med (Breastfeeding Medicine). 2009;4(2):111-113.
Read instructions before use. Consult a specialist about possible contraindications.
* RU No. ФСЗ 2010/07352 of 07/19/10
** RU No. ФСЗ 2010/06525 of 03/17/2021 breastfeeding in the first month.
Share this information
Cathy Garbin, child health nurse, midwife and lactation consultant:
Cathy, a mother of two, was a research fellow at the renowned Human Lactation Research Institute, founded by Peter Hartmann, for seven years, providing support to breastfeeding mothers in clinics and at home. Today, she still works as a family counselor, and also conducts seminars for attending physicians and speaks at international conferences.
Today, she still works as a family counselor, and also conducts seminars for attending physicians and speaks at international conferences.
Breastfeeding is as much a skill as driving a car, and in the first month mother and baby may encounter some obstacles along the way. It takes time and experience to make it familiar to both of you. Solving breastfeeding problems in the first month helps to establish good milk production and increase the duration of breastfeeding in the future. Below you will find tips on how to overcome the main breastfeeding challenges that mothers often face from the end of the first week to the end of the first month after giving birth.
Problem #1. A painful lump appeared in the breast
Lumps and bumps in the breast of a nursing woman can appear for various reasons. One of the most common is blockage of the milk ducts, which results in a hard and painful lump that can become inflamed.
Solutions 1-3
- Massage the inflamed area, especially while breastfeeding or pumping, to clear the blockage.
- Gently apply warm flannel to your breasts or take a warm shower before feeding to relieve discomfort.
- Continue breastfeeding as usual to avoid milk accumulation that can cause mastitis.
- Try to express milk from the inflamed breast after feeding to ensure that it is completely emptied. This will help to remove the blockage and restore the patency of the duct. See what breast pumps* Medela has to offer and choose the right one for you.
- Try ultrasound therapy. If you have repeated blocked ducts, your lactation consultant or healthcare professional may suggest this procedure to help restore milk flow. The procedure is performed by a physiotherapist.
- Call your healthcare provider, if you notice signs of infection (breast redness and tenderness or flu-like symptoms such as fever, aches, malaise and headache), or if you think the lump is not related to breastfeeding .
Problem #2. The breast is red and sore
If one or both mammary glands are red and sore, and this is not due to blockage of the ducts, the possibility of mastitis, that is, inflammation of the breast tissue, is not excluded. Mastitis is characterized by redness, burning, and soreness of the breasts, combined with flu-like symptoms: You feel hot and cold, your joints ache, and your temperature rises above 38.5 °C (101.3 °F). Seek medical attention immediately if you experience these symptoms. Mastitis needs to be treated as soon as possible, as your condition can worsen in just a few hours. 3
Mastitis can be caused by the following causes:
- untreated blocked ducts,
- Bacteria introduced into the breast through cracked and damaged nipples,
- incorrect attachment of the child to the breast,
- long periods between feedings,
- breasts too full,
- wearing a bra that is too tight or that cuts into the skin,
- Abrupt weaning,
- excess milk.

Solutions 3
In addition to seeking medical attention:
- Continue to breastfeed or express milk frequently. Your milk is still safe for your baby. Its release will help eliminate blockage of the ducts and prevent painful accumulation of milk. Sudden cessation of feeding or pumping may exacerbate symptoms. After feeding, it is advisable to express any remaining milk.
- Give the child the inflamed breast first. This way the child can empty it completely. If it hurts too much, start feeding on the healthy breast, and when milk begins to flow, go back to the first one.
- Have a good rest, drink and eat. You need to get enough fluids and good nutrition.
- Massage the sore area under a warm shower or apply a warm flannel or warm pack to clear the blockage and relieve symptoms before feeding or pumping.
- Apply a cooling pack after feeding, , to reduce inflammation.
Problem #3. My strength is running out
Breastfeeding in the first weeks can be very tiring and seem endless. The baby will ask for a breast every few hours, day and night, and you have not yet grown stronger after giving birth.
Solutions
- Take care of yourself. This may be easier said than done when you have a newborn in your arms, but still try to get as much rest as possible, eat healthy and regular meals, and drink plenty of water. Do not refuse the help of your partner, relatives and friends, or even hire an assistant if you can afford it.
- Feed lying down. This will allow you to relax and reduce stress on sore spots, stitches or c-section scars.
- Do not skip feedings. Your partner may offer to bottle feed your baby while you are resting. However, despite this temptation, it should be remembered that milk production is best established in the first four weeks through breastfeeding.
 When breastfeeding is well established, you can give your baby expressed milk, but before that, ask family or friends to help you with other things so you can fully focus on breastfeeding.
When breastfeeding is well established, you can give your baby expressed milk, but before that, ask family or friends to help you with other things so you can fully focus on breastfeeding.
Problem #4. How can I increase breast milk production?
It's easy to question whether your breastmilk supply is adequate, especially when your baby has developmental spikes between the third and fourth weeks. It may seem to you that the child asks for breasts more often because he does not have enough milk. However, if the number of wet and soiled diapers doesn't change—see Breastfeeding: What to Expect in the First Month—the baby is likely to breastfeed more often to calm down. The baby is surrounded by many new sounds and images that are easy to get tired of, and at the breast he feels safe. 4
Solutions 4.5
- Do not try to supplement your baby with formula, unless doctors are concerned about weight gain or fluid loss.
 Continue breastfeeding your baby. This will help naturally increase breast milk production.
Continue breastfeeding your baby. This will help naturally increase breast milk production. - Do not feed on a schedule. Feed your baby on demand. Thus, the production of breast milk will adapt to his needs.
- Use the breast pump, , to help increase breast milk production while continuing to breastfeed.
Problem #5. I have too much milk
Hyperlactation, or too much milk, can also be difficult for you and your baby. You may experience discomfort from swollen and leaking breasts, and your baby may have difficulty latch-on, choke on the milk flowing too fast, and be unable to empty the breast properly. 6
Solutions
- Express some breast milk at the start of a feed to reduce the force of the flush. Don't pump too much as this can aggravate the situation - pump only as much as needed to ease the discomfort. Try hand pumping or use a breast pump (check out the Medela* breast pump range and choose the right one for you).

- Use the towel or pad to soak up excess milk, or place the milk collection pad** on the other breast while you breastfeed first.
- The child must feel supported. Hold him firmly (this gives a sense of security) and in a comfortable position so that he can turn his head. Talk to the baby during the first rapid flush, then he will not be frightened by surprise and will not push the breast.
- Contact a lactation consultant or health care professional who will monitor you and be able to suggest one-sided feedings or hourly breast changes (“breast duty”) to normalize your milk supply.
- Be patient . Problems with milk production usually go away after a few weeks.
Problem #6. I have different breasts!
You have noticed that the baby has a preference for one breast, or that one breast produces more milk than the other, and as a result, the mammary glands have acquired different sizes and shapes. This happens quite often and does not pose any problems for breastfeeding. If this does not bother you or your baby, you can leave everything as it is. If this makes you uncomfortable, try the following tricks.
This happens quite often and does not pose any problems for breastfeeding. If this does not bother you or your baby, you can leave everything as it is. If this makes you uncomfortable, try the following tricks.
Solutions
- When feeding, offer your baby the less demanded breast first because babies usually suckle more vigorously at the beginning of a feed.
- Use the breast pump to increase breast milk production in the smaller breast.
- Don't give up on bigger breasts. Breastfeeding should continue with fuller breasts to avoid blocked ducts and mastitis.
- Seek medical attention. Sometimes an ear infection is the reason for a baby to latch on only one side. However, some positions may cause him discomfort, so try to keep the child more upright. In addition, a breast infection can change the taste of milk and cause milk to be rejected as well.
Issue #7.
 A blister has appeared on the nipple
A blister has appeared on the nipple With frequent feeding, sometimes painful friction occurs, and a blood bubble may appear on the breast,
nipple or areola. 7
Solutions
- Ask a lactation consultant or specialist to check the baby's latch on. A shallow grip can cause blistering of the nipples and areolas.
- Talk to your doctor about what medication you can take to relieve pain if needed.
- Try other feeding positions to avoid pressure on the painful area.
- Lubricate inflammation with pure lanolin.
- Use the Breast Pads** to avoid rubbing your blister with clothing and help it heal faster with air circulation, or try cooling hydrogel pads** to help relieve pain and promote healing.
- Try expressing milk. Using a breast pump can be an alternative way to get breast milk without bladder irritation.
 Choose the correct funnel size so that the nipple can move freely and the bubble does not rub against the walls of the tunnel.
Choose the correct funnel size so that the nipple can move freely and the bubble does not rub against the walls of the tunnel. - Do not pierce the vial as this may lead to infection.
- Seek medical attention, if the problem persists and causes you pain.
Issue #8. Painful white spot on nipple
When the opening of the milk duct is blocked by milk or a thin layer of skin grows over it, a small white or yellowish spot may appear on the tip of the nipple. For some, these blocked ducts, sometimes called milk vesicles or blisters, cause pinpoint pain, especially during feeding or pumping. Others do not experience any discomfort. White blisters may persist for several days or weeks until the skin breaks and hardened milk comes out. 8
Solutions
- Follow the tips above to solve friction bubble problems.
- Remove the blockage, if you see that the milk cork is starting to bulge.
 Try to squeeze it out very gently with clean nails.
Try to squeeze it out very gently with clean nails. - Continue breastfeeding or pumping, to clear the milk duct. If the milk duct clears during feeding, it will not harm the baby in any way.
- Apply hot wet flannel to the vial just before feeding or pumping. This will help open the blocked duct. You can also try rubbing the area quickly with a clean, damp cloth.
- Hand express some milk before feeding, trying to push out hardened milk clots. If this does not help, feed the baby or express milk as usual. Repeat several times a day.
- Soak a cotton swab with olive oil and place it in the bra, pressing it against the bubble nipple. This will help soften the skin.
- Seek medical attention, if problem persists. Your doctor may remove the plug with a sterile needle. This should be done immediately after feeding, when the bubble is as inflated as possible.
Issue #9. My nipples hurt while breastfeeding
At the start of breastfeeding, my nipples may become more tender, sore, and even inflamed, but this usually goes away after a few days. If your baby's latch is checked by a specialist and the inflammation persists or the nipples hurt with every feeding, you may need medical attention to resolve this problem. 2.7
The following symptoms and signs that appear on one or both breasts during or after feeding may indicate a bacterial infection or thrush:
- burning, itching or moderate to severe pain in the nipples
- pain in nipples worse on contact with clothing,
- nipple pain persists despite attempts to attach baby differently,
- nipples hurt to touch,
- stitching, shooting, burning or deep aching pain,
- chest pain during feeding and almost an hour after,
- hot pink nipples,
- discoloration and texture of the areola (hot pink, darkening, dryness or peeling),
- white rash on chest or areola.
Also check if your child has the following symptoms and signs:
- hard white patches or coating on the tongue,
- white indelible spots on the cheeks,
- bright red spotted rash on buttocks not helped by diaper rash creams.
Solutions 7
- Seek medical attention. He will most likely suggest testing for infections to make a diagnosis. Bacterial and fungal (yeast) infections are treated differently, so appropriate treatment should be started as soon as possible. There are other reasons that can cause similar nipple pain, such as eczema, psoriasis or vasospasm (narrowing of the blood vessels) in the mother and problems with latch or tongue frenulum in the child. Therefore, it is very important to make an accurate diagnosis.
- Strict hygiene. Wash hands before and after feeding and applying any medication, and after changing diapers. Change bra pads regularly, wash bras, tank tops and towels in high temperature water, thoroughly wash breast cups and anything your baby puts in her mouth, such as nipples.
- Let the nipples dry after feeding, since all infections love a warm and humid environment.
- See your doctor again if there is no improvement after a few days. Do not let the problem run its course, otherwise the situation may worsen.
Related materials. Breastfeeding: what to expect in the first month
Breastfeeding: what to expect after the first month
Breastfeeding problems after the first month
Literature
1 Academy of Breastfeeding Medicine Protocol Committee. ABM clinical protocol # 20: Engorgement. Breastfeed Med. 2009;4(2):111-113.- Breastfeeding Academy Protocol Committee, "AVM Clinical Protocol #20: Breast engorgement." Brestfeed Med (Breastfeeding Medicine). 2009;4(2):111-113.
2 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe and Frauenheilkunde . 2013;73(12):1202-1208. - Jacobs A. et al., "Recommendations S -3 for the treatment of inflammatory diseases of the breast during breastfeeding. Geburtskhilfe und Frauenheilkünde. ABM Clinical Protocol# 4: Mastitis , Revised MARCH 2014. . 23 : 50202 Med 9020 (5) H., Academy of Breastfeeding Protocol Committee, AVM Clinical Protocol #4: Mastitis, March 2014 edition of Brestfeed Med (Breastfeeding Medicine). 2014;9(5):239-243.
2013;73(12):1202-1208. - Jacobs A. et al., "Recommendations S -3 for the treatment of inflammatory diseases of the breast during breastfeeding. Geburtskhilfe und Frauenheilkünde. ABM Clinical Protocol# 4: Mastitis , Revised MARCH 2014. . 23 : 50202 Med 9020 (5) H., Academy of Breastfeeding Protocol Committee, AVM Clinical Protocol #4: Mastitis, March 2014 edition of Brestfeed Med (Breastfeeding Medicine). 2014;9(5):239-243.
4 Kent JC et al. Principles for maintaining or increasing breast milk production. 2012;41(1):114-121. - Kent J.S. et al., "Principles for Maintaining and Increasing Milk Production". F Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
5 Amir L. Breastfeeding managing ‘supply’ difficulties. Aust fam physician .