Newborn baby breathing fast after feeding
Transient tachypnea - newborn: MedlinePlus Medical Encyclopedia
URL of this page: //medlineplus.gov/ency/article/007233.htm
To use the sharing features on this page, please enable JavaScript.
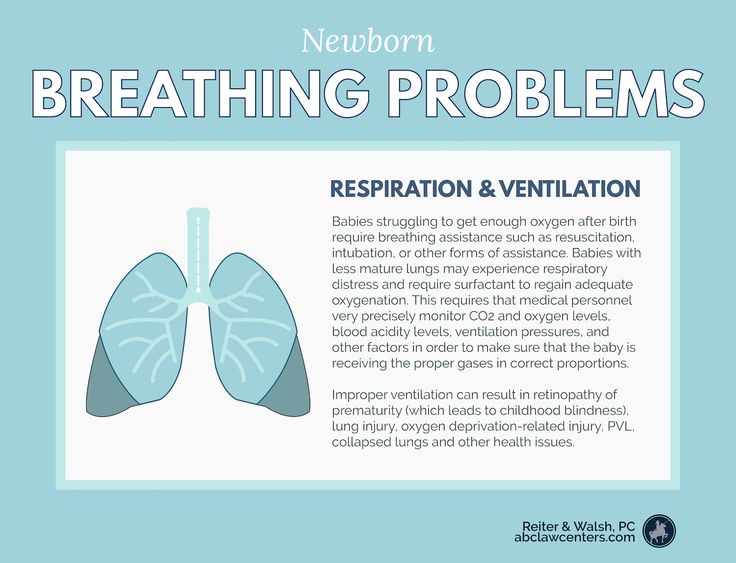
Transient tachypnea of the newborn (TTN) is a breathing disorder seen shortly after delivery, most often in early term or late preterm babies.
- Transient means it is short-lived (most often less than 48 hours).
- Tachypnea means rapid breathing (faster than most newborns, who normally breathe 40 to 60 times per minute).
As the baby grows in the womb, the lungs make a special fluid. This fluid fills the baby's lungs and helps them grow. When the baby is born at term, hormones released during labor tell the lungs to stop making this special fluid. The baby's lungs start removing or reabsorbing it.
The first few breaths a baby takes after delivery fill the lungs with air and help to clear most of the remaining lung fluid.
Leftover fluid in the lungs causes the baby to breathe rapidly. It is harder for the small air sacs of the lungs to stay open.
TTN is more likely to occur in babies who are:
- Born before 38 completed weeks gestation (preterm, or early term)
- Delivered by C-section, especially if labor has not already started
- Born to a mother with diabetes or asthma
- Twins
Newborns with TTN have breathing problems soon after birth, usually starting within 1 to 2 hours.
Symptoms include:
- Bluish skin color (cyanosis)
- Rapid breathing, which may occur with noises such as grunting
- Flaring nostrils or movements between the ribs or breastbone known as retractions
The mother's pregnancy and labor history are important to make the diagnosis.
Tests performed on the baby may include:
- Blood count and blood culture to rule out infection
- Chest x-ray to rule out other causes of breathing problems
- Blood gas to check levels of carbon dioxide and oxygen
- Continuous monitoring of the baby's oxygen levels, breathing, and heart rate
The diagnosis of TTN is most often made after the baby is monitored for 2 or 3 days. If the condition goes away in that time, it is considered to be transient.
If the condition goes away in that time, it is considered to be transient.
Your baby will be given oxygen, and sometimes CPAP (continuous positive airway pressure) as well, to keep the blood oxygen level and breathing rate stable. Your baby will often need the most support within a few hours after birth and will usually begin to improve after that. Most infants with TTN improve in less than 24 to 48 hours, but some will need help for a few days.
Very rapid breathing usually means a baby is unable to eat. Fluids and nutrients will be given through a vein until your baby improves. Your baby may also receive antibiotics until the health care team is sure there is no infection. Sometimes, babies with TTN will need help with breathing or feeding for a week or more, usually if they are premature.
The condition most often goes away within 48 to 72 hours after delivery. In most cases, babies who have had TTN have no further problems from the condition. They will not need special care or follow-up other than their routine checkups. However, there is some evidence that babies with TTN may be at a higher risk for wheezing problems later in infancy.
However, there is some evidence that babies with TTN may be at a higher risk for wheezing problems later in infancy.
Late preterm or early term babies (born more than 2 to 6 weeks before their due date) who have been delivered by C-section without labor may be at risk for a more severe form known as "malignant TTN."
TTN; Wet lungs - newborns; Retained fetal lung fluid; Transient RDS; Prolonged transition; Neonatal - transient tachypnea
Ahlfeld SK. Respiratory tract disorders. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 122.
Crowley MA. Neonatal respiratory disorders. In: Martin RJ, Fanaroff AA, Walsh MC, eds. Fanaroff and Martin's Neonatal-Perinatal Medicine: Diseases of the Fetus and Infant. 11th ed. Philadelphia, PA: Elsevier; 2020:chap 66.
Greenberg JM, Haberman BE, Narendran V, Nathan AT, Schibler K. Neonatal morbidities of prenatal and perinatal origin. In: Creasy RK, Lockwood CJ, Moore TR, Greene MF, Copel JA, Silver RM, eds. Creasy and Resnik's Maternal-Fetal Medicine: Principles and Practice. 8th ed. Philadelphia, PA: Elsevier; 2019:chap 73.
In: Creasy RK, Lockwood CJ, Moore TR, Greene MF, Copel JA, Silver RM, eds. Creasy and Resnik's Maternal-Fetal Medicine: Principles and Practice. 8th ed. Philadelphia, PA: Elsevier; 2019:chap 73.
Updated by: Kimberly G. Lee, MD, MSc, IBCLC, Clinical Professor of Pediatrics, Division of Neonatology, Medical University of South Carolina, Charleston, SC. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
What’s Normal and When You Should See a Doctor
Baby Breathing Fast: What’s Normal and When You Should See a DoctorMedically reviewed by Karen Gill, M.D. — By Taylor Norris on August 9, 2018
Introduction
Babies do a lot of things that surprise new parents. Sometimes you pause and laugh at their behavior, and sometimes you might become genuinely concerned.
The way newborns breathe, sleep, and eat can be new and alarming for parents. Usually, there’s no cause for concern. It’s helpful to learn about newborn breathing to keep you informed and take the best care of your little one.
Usually, there’s no cause for concern. It’s helpful to learn about newborn breathing to keep you informed and take the best care of your little one.
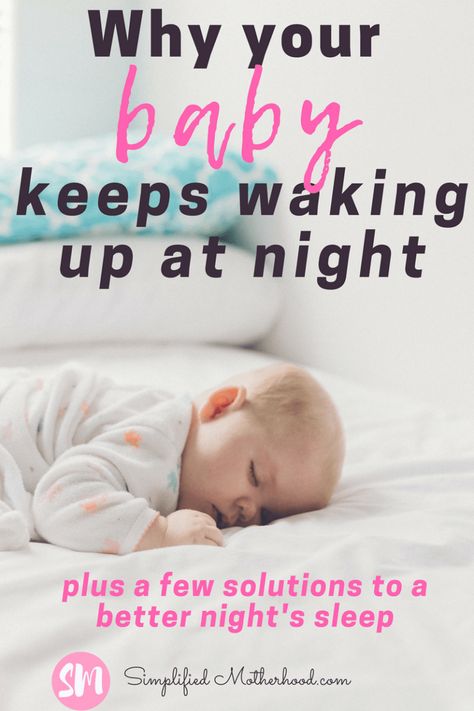
You might notice your newborn breathing fast, even while sleeping. Babies can also take long pauses between each breath or make noises while breathing.
Most of these come down to a baby’s physiology. Babies have smaller lungs, weaker muscles, and breathe mostly through their nose. They’re actually just learning to breathe, since the umbilical cord delivered all of their oxygen straight to their body by way of their blood while in the womb. A child’s lungs are not fully developed until ages 2 to 5.
Normal newborn breathing
Newborns breath a lot faster than older babies, kids, and adults.
On average, newborns younger than 6 months take about 40 breaths per minute. That looks pretty fast if you’re watching them.
Breathing may slow down to 20 breaths per minute while newborns sleep. In periodic breathing, a newborn’s breathing may stop for 5 to 10 seconds and then begin again more rapidly — around 50 to 60 breaths per minute — for 10 to 15 seconds. They shouldn’t pause more than 10 seconds between breaths, even when resting.
They shouldn’t pause more than 10 seconds between breaths, even when resting.
Familiarize yourself with your newborn’s normal breathing pattern while they’re healthy and relaxed. This will help you notice if things ever change.
What to watch for in an infant’s breathing
Fast breathing by itself isn’t a cause for concern, but there are a few things to pay attention to. Once you have a sense of your newborn’s normal breathing pattern, watch closely for signs of change.
Premature newborns may have underdeveloped lungs and have some problems breathing. Full-term babies delivered by cesarean are at increased risk for other breathing issues right after birth. Work closely with your child’s pediatrician to learn what signs you need to monitor.
Newborn breathing problems include:
- deep cough, which may be a sign of mucus or infection in the lungs
- whistling noise or snoring, which may require suctioning mucus from the nose
- barking and hoarse cry that could indicate croup
- fast, heavy breathing which could potentially be fluid in the airways from pneumonia or transient tachypnea
- wheezing which could stem from asthma or bronchiolitis
- persistent dry cough, which may signal an allergy
Tips for parents
Remember that coughing is a good natural reflex that protects your baby’s airways and keeps germs out. If you’re concerned about your newborn’s breathing, monitor them over a few hours. You’ll soon be able to tell if it’s a mild cold or something more serious.
If you’re concerned about your newborn’s breathing, monitor them over a few hours. You’ll soon be able to tell if it’s a mild cold or something more serious.
Take a video of any worrisome behavior to either bring or email to your doctor. Find out if your child’s practitioner has an app or online interface for fast communication. This will help you let them know your child is mildly sick. In a medical emergency, you should call 911 or visit an emergency room.
Tips for taking care of a sick baby:
- keep them hydrated
- use saline drops to help clear mucus
- prepare a warm bath or run a hot shower and sit in the steamy bathroom
- play calming music
- rock the baby in their favorite position
- ensure the baby gets enough sleep
You shouldn’t use vapor rub as a treatment for children younger than age 2.
The American Academy of Pediatrics recommends always putting babies to sleep on their back for the best breathing support. It might be difficult to settle your baby down on their back when they’re sick, but it remains the safest sleeping position.
It might be difficult to settle your baby down on their back when they’re sick, but it remains the safest sleeping position.
When to see the doctor
A very sick baby will look and act very different than normal. But it can be difficult to know what’s normal when you’ve only known your baby for a few weeks. Over time, you’ll get to know your baby better and your confidence will grow.
You can call your child’s doctor whenever you have questions or concerns. Most offices have an on-call nurse who can offer tips and guidance.
Call your child’s doctor or go for a walk-in appointment for any of the following:
- trouble sleeping or eating
- extreme fussiness
- deep cough
- barking cough
- fever above 100.4°F or 38°C (seek immediate care if your baby is under 3 months)
If your baby has any of these major signs, call 911 or go to an emergency room right away:
- a distressed look
- trouble crying
- dehydration from lack of eating
- trouble catching their breath
- breathing faster than 60 times per minute
- grunting at the end of each breath
- nostrils flaring
- muscles pulling in under the ribs or around the neck
- blue tinge to the skin, especially around lips and fingernails
Takeaway
Any irregular breathing in your child can be very alarming.![]() Watch your baby and learn about their normal behavior so that you can act quickly if you notice that they’re having trouble breathing.
Watch your baby and learn about their normal behavior so that you can act quickly if you notice that they’re having trouble breathing.
Last medically reviewed on August 9, 2018
- Parenthood
- Baby
How we vetted this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations. We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- American Academy of Pediatrics announces new safe sleep recommendations to protect against SIDS, sleep-related infant deaths. (2016.)
aap.org/en-us/about-the-aap/aap-press-room/pages/american-academy-of-pediatrics-announces-new-safe-sleep-recommendations-to-protect-against-sids.aspx - Breathing problems. (n.d.)
stanfordchildrens.org/en/topic/default?id=breathing-problems-90-P02666 - Emergency symptoms not to miss.
 (2018.)
(2018.)
seattlechildrens.org/medical-conditions/symptom-index/emergency-symptoms-not-to-miss/ - Gallacher DJ, et al. (2016). Common respiratory conditions of the newborn. DOI:
10.1183/20734735.000716 - Reuter S, et al. (2014). Respiratory distress in the newborn. DOI:
10.1542/pir.35-10-417 - Transient tachypnea of the newborn. (n.d.)
stanfordchildrens.org/en/topic/default?id=transient-tachypnea-of-the-newborn-90-P02420
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Aug 9, 2018
By
Taylor Norris
Edited By
Nizam Khan (TechSpace)
Medically Reviewed By
Karen Richardson Gill, MD
Share this article
Medically reviewed by Karen Gill, M.D. — By Taylor Norris on August 9, 2018
Read this next
Is My Newborn’s Heavy Breathing Typical?
Medically reviewed by Carissa Stephens, R.
 N., CCRN, CPN
N., CCRN, CPNBabies often make unusual noises when they breathe, so it's not likely a concern. Learn their breathing patterns to know what's typical — and what's…
READ MORE
What Is a Normal Respiratory Rate for Adults and Children?
Medically reviewed by Cynthia Taylor Chavoustie, MPAS, PA-C
For children, a normal respiratory rate varies by age. For adults, it's typically between 12 to 20 breaths per minute. Learn more.
READ MORE
Lung Opacity: What You Should Know
Opacity on a lung scan can indicate an issue, but the exact cause can vary.
READ MORE
Causes of Cough and Rash
Medically reviewed by Kevin Martinez, M.D.
Both a cough and a rash are reactions to an irritant or underlying medical condition. Several different infections and other medical conditions can…
READ MORE
Yes, Vaccines are Safe Even After a Study Looked at Potential Link to AsthmaREAD MORE
What Causes Violent Coughing Fits and How Can I Stop Them?
Find out what explosive coughing attacks indicate, how to treat them at home, and when you should visit a doctor.

READ MORE
12 Laryngitis Home Remedies
Medically reviewed by Nicole Leigh Aaronson, MD, MBA, CPE, FACS, FAAP
Laryngitis happens when your vocal cords become inflamed from overuse, irritation, or infection, causing voice distortion. We’ll talk about 12 home…
READ MORE
The baby gets tired quickly when feeding and breathes often: symptoms, diagnosis
With the advent of the baby, all the mother's attention is focused on feeding the baby. After all, I really want the baby to gain weight well. But often during feeding, a woman notices that the baby gets tired quickly. In such a situation, the baby's breathing quickens, which prevents him from eating the prescribed norm. If such a picture is observed with frightening frequency, it is necessary to find out the cause of the problem.
In pediatric cardiology, there are several important signs that indicate heart problems in a young patient. The children's cardiologist of the multidisciplinary center "Edkarik" will be able to figure out what caused the difficulties in feeding. At the first negative symptoms in the baby, parents should contact us to exclude the presence of a serious heart pathology in the crumbs.
The children's cardiologist of the multidisciplinary center "Edkarik" will be able to figure out what caused the difficulties in feeding. At the first negative symptoms in the baby, parents should contact us to exclude the presence of a serious heart pathology in the crumbs.
Features of breathing in infants
It should be noted right away that difficulty breathing during feeding is not always an indicator of an existing heart pathology. Such a symptom is typical for respiratory diseases, breathing difficulties may be associated with structural features of the nasal septum. This problem is often observed in the first weeks due to undeveloped breasts in the mother. The child has to make every effort to get the right portion of food. Therefore, he quickly gets tired, and his breathing goes astray from the normal rhythm.
The breathing of children in the first months of life has its own characteristics. Babies need twice the amount of oxygen, but their respiratory system is not yet completely formed. Certain difficulties in the respiratory function are imposed by narrow nasal passages and weakness of the pectoral muscles. Therefore, breathing in children up to a year is uneven. The child often takes quick breaths, so his breathing is shallow and intermittent.
Certain difficulties in the respiratory function are imposed by narrow nasal passages and weakness of the pectoral muscles. Therefore, breathing in children up to a year is uneven. The child often takes quick breaths, so his breathing is shallow and intermittent.
The norm of respiratory movements in babies of the first month of life is 40-60, from the end of the fourth week and up to 3 months - up to 45, in the period of 4-6 months - 35-40. By the year, the baby is already taking about 30-35 breaths per minute, which is considered the norm.
Mom can determine the respiratory rate on her own. To do this, put the baby on his back, and use a stopwatch to count the number of breaths. Since babies "breathe" with their tummies, such a calculation is easy to make. The main condition for performing this procedure is that the child must be calm.
When there is no reason to worry
The nervous system of young children is still imperfect, so they cannot control their breathing. During active games and crying, the frequency of respiratory movements increases, and in a dream they often sniffle. If such features are observed sporadically, you should not worry. The sniffing nose can be washed with boiled water, and then carefully remove the dried mucus.
During active games and crying, the frequency of respiratory movements increases, and in a dream they often sniffle. If such features are observed sporadically, you should not worry. The sniffing nose can be washed with boiled water, and then carefully remove the dried mucus.
What should cause alarm
You need to see a doctor if the baby:
- holds his breath for a long time;
- exhales noisily;
- if breathing is accompanied by wheezing and wheezing.
Typically, such symptoms can be traced against the background of an acute period of respiratory diseases. Timely treatment will help to quickly eliminate these negative signs, after which the child will be able to breastfeed normally again.
Which symptoms require special attention
We have listed physiological breathing problems. But sometimes the situation is much more serious than the usual runny nose. We list the signs that should be a strong argument for parents to urgently visit a pediatric cardiologist.
- Cyanosis
If holding the breath during feeding is accompanied by a blue nasolabial triangle, this sign indicates a lack of oxygen. In severe forms of cardiac pathologies, the chin and fingers of the baby turn blue. This symptom is characteristic of congenital malformations of both the heart and vascular anomalies.
- Shortness of breath
This symptom also indicates a lack of oxygen. Since the child has to expend more energy during sucking, this symptom is more pronounced than at rest. A cause for concern can be considered frequent breaks for rest during suckling. Normally, there are no more than two such pauses, and a child with heart disease takes breaks after 2-3 sips.
- Fatigue
Infants with congenital heart defects are much less active than healthy children. They are not able to suck out the norm during feeding, so they lose weight. The problem is aggravated by frequent breathing. The child simply suffocates under tension.
The child simply suffocates under tension.
- Chest pain
Infants may not complain of such a symptom, but an observant mother will notice under what circumstances and how often the child begins to worry.
If all the described signs are repeated from the baby during feeding regularly, it is urgent to consult a pediatric cardiologist. A full-scale examination will determine the cause of the problem, and an experienced pediatric cardiologist will prescribe adequate therapy for the child.
Peculiarities of diagnosing infants
Babies under one year old cannot describe the symptoms that prevent them from developing normally. Therefore, all hope for an objective examination. During the initial examination of the infant, the pediatric cardiologist:
- evaluates the general condition;
- notes the color of the skin;
- listens to the baby's heart;
- performs heart rate monitoring and saturation level measurement.

The doctor pays special attention to taking an anamnesis, since such information can indicate the cause of the problem. For example, an infection transmitted by a woman during her mother's pregnancy can provoke the development of congenital heart defects. An important factor is heredity, especially if there were cases of premature death (up to 50 years) among close relatives in the family. After collecting the data, the pediatric cardiologist will definitely prescribe the following types of diagnostic procedures:
- ECG with daily monitoring;
- ultrasound of the heart;
- Chest x-ray;
- Laboratory tests.
Instrumental methods of examination with the use of modern devices will clarify the parameters of the baby's heart and the features of its anatomical structure. Ultrasound diagnostics helps to identify defects in the heart chambers and great vessels. Having the data of all studies at hand, the pediatric cardiologist will draw up an individual treatment program, or prescribe additional procedures. In severe cardiac pathologies and rhythm disturbances, the question of a surgical way to eliminate the problem can be decided.
In severe cardiac pathologies and rhythm disturbances, the question of a surgical way to eliminate the problem can be decided.
Examination and treatment in the center "Edkarik"
Among our guarantees:
- professionalism of doctors;
- high quality service;
- comfortable conditions in the clinic;
- individual approach;
- a wide range of services;
- accompanying patients during the rehabilitation period.
Our clinic is known not only in Kaliningrad, but also in other regions of the country. Parents and their kids will feel comfortable in our center, because there is everything you need to make sick children feel at home with us. You can make an appointment with a pediatric cardiologist on the official website of our center. There are also contact numbers where parents can consult on issues of concern to them.
Let the baby breathe evenly!
Mothers of babies often listen to their breathing. What do you need to know about how a newborn breathes?
Hard science
|
| For 40 weeks the family was looking forward to the birth of a baby with joy and impatience. In his mother's tummy, he was completely dependent on her. Together with her, he walked through the forest or park, received a sufficient (or insufficient) amount of oxygen. The baby begins to train to breathe already in the last month of intrauterine life, when it makes about fifty respiratory movements per minute, facilitating the flow of blood to the heart. He takes breaths with a closed glottis so as not to choke in the amniotic fluid. After birth, a number of important changes occur: the flow of nutrients and oxygen through the placenta stops. And with the first cry of a newborn, the lungs expand, and the child begins to breathe on his own. |
A child's metabolism is much faster than that of an adult, and it is more than that of an adult, and it needs oxygen more than an adult. The increased need for it is compensated by more frequent breathing.
Newborns breathe irregularly, at times their breathing becomes weak, barely audible. They breathe with their belly.
In the first three days of life, twice as much air is "pumped" through the lungs of a newborn as compared to an older child.
The baby takes a deep breath with difficult exhalation, which prevents the smallest lung chambers (alveoli) from being saved and sticking together and helps the baby to straighten the lungs, and the entire respiratory system to create high resistance to exhaled air for the first breath and the first cry of a small creature.
In cases of suffocation, or asphyxia, quite recently, in addition to spanking on the bottom, the baby was “cheered up” by dipping into cold water. Today, this method is no longer used. First, reflexes are activated by stroking the back or patting the heels. If the baby is still ill, then proceed to effective resuscitation.
Today, this method is no longer used. First, reflexes are activated by stroking the back or patting the heels. If the baby is still ill, then proceed to effective resuscitation.
Birth is a difficult test for a baby with its still imperfect respiratory system. The lungs of an infant are poorly developed, their elastic tissue is well filled with blood, but not enough with air.
Due to poor ventilation, lung tissue often collapses in young children. In the first months of life, the structure of the lungs gradually changes: connective tissue layers are replaced by elastic tissue, and the number of alveoli increases. The mobility of the chest in infants is limited, and at first the lungs grow due to the soft diaphragm. The type of breathing in the crumbs changes to diaphragmatic, or abdominal. It becomes thoracic or thoracic only after the children begin to walk.
By 6 months, breathing becomes less frequent - 35-40 breaths per minute, and by the year the child is already breathing at a frequency of 30 times per minute. In an adult, the respiratory rate normally does not exceed 18 breaths per minute.
In an adult, the respiratory rate normally does not exceed 18 breaths per minute.
Congenital reflexes
There is not a single mother who would not listen from time to time: is the baby breathing?
Don't worry too much. Remember that from birth, the baby has a set of innate reflexes. If you put the baby on his stomach, he will automatically turn his head to the side so that he can breathe. Coughing and sneezing are also such innate reflexes.
Periodic pauses in breathing are a legacy of intrauterine life. Even perfectly healthy babies have short pauses in breathing, but the duration of these breaks cannot exceed 12-15 seconds.
Pediatricians recommend that children's respiratory irregularity be treated with great attention, since apnea can be a threat due to temporary oxygen starvation of the brain.
Unobtrusive breath control is necessary not only for an immature baby, but also for a perfectly healthy, full-term baby from 3 to 8 months.
In order for the child to "remember" to breathe rhythmically, without stopping, he needs almost continuous tactile stimulation. Caress the baby more often, take it in your arms, press it to you. After about 8 months of life, the regularity of breathing in the child will improve, but until then, he needs skin-to-skin contact.
When experts believe that your baby has a special case and needs constant monitoring of breathing, different models of breathing monitors can be used. The principle of their action is as follows, if the baby has interruptions in breathing during sleep or wakefulness, its frequency becomes less than 10 respiratory movements per minute, or the respiratory arrest continues for more than 12 seconds, a loud beep will sound and the red alarm indicator will light up. This is a message that your baby needs emergency measures to restore normal breathing.
You won't run him over!
Sudden death when mother and child sleep separately occurs 3 times more often than when they sleep together!
Some mothers are afraid to crush the baby in their sleep.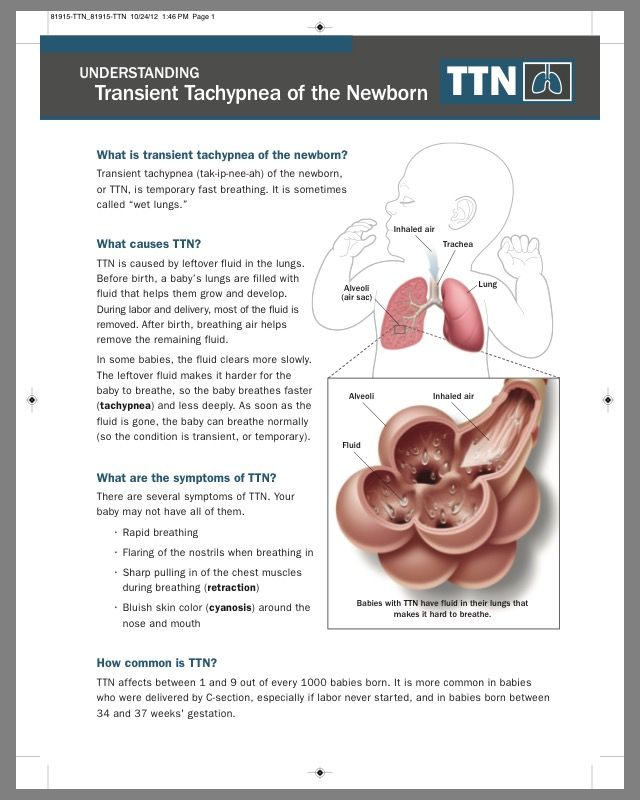 But think for yourself: you feed the baby, lying in a comfortable position, becoming at this moment, as it were, a single whole. And here the probability that you will crush your baby is absolutely excluded. Surround your baby with your warmth and love!
But think for yourself: you feed the baby, lying in a comfortable position, becoming at this moment, as it were, a single whole. And here the probability that you will crush your baby is absolutely excluded. Surround your baby with your warmth and love!
Developing easy crumbs!
How to create the best conditions for the baby?
- Ventilate the room in which the baby is present.
- Free breathing of the crumbs should not be constrained by anything. Pillows, piles of warm clothes and diapers make it difficult for him to get fresh air into his airways.
- Regular walks will help develop the baby's lungs and strengthen the immune system.
- In order for the baby to develop properly and acquire strong immunity to various diseases, it is necessary to do gymnastic and breathing exercises with him, as well as to conduct regular courses of preventive or therapeutic massage.


 Circulation and metabolism also work in a new way.
Circulation and metabolism also work in a new way.