Should you feed baby after vomiting
How to Know Whether You Should
Your baby just threw up all the milk they’ve chugged down so far, and you’re wondering if it’s OK to continue feeding. How soon should you feed your baby after vomiting?
It’s a good question — just about every parent has likely pondered this. Spit-up is almost a rite of passage for babies (and parents). Baby vomiting is also common and can happen for many reasons. Most of the causes aren’t serious.
The short answer — because you may have a very fussy baby on your hands and want to get back to them ASAP — is yes, you can usually feed your baby after they vomit all over your favorite sweater, sofa throw, and rug.
Here’s just about everything you need to know about feeding your baby after vomiting.
Baby vomit and spit-up are two different things — and they can have different causes. Spitting up is common in babies under the age of 1 year. It typically happens after feeding. Spit-up is usually an easy flow of milk and saliva that dribbles from your baby’s mouth. It often happens with a burp.
Spit-up is normal in healthy babies. It can happen for several reasons. About half of all babies 3 months and under have a type of acid reflux called infant reflux.
Spit-up from infant reflux is especially bound to happen if your baby has a full stomach. Being careful not to overfeed a bottle-fed infant can help. Spitting up typically stops by the time your baby is a year old.
On the other hand, vomiting is typically a more forceful throwing-up of milk (or food, if your baby is old enough to eat solids). It happens when the brain signals the muscles around the stomach to squeeze.
Vomiting (like gagging) is a reflex action that can be triggered by a number of things. These include:
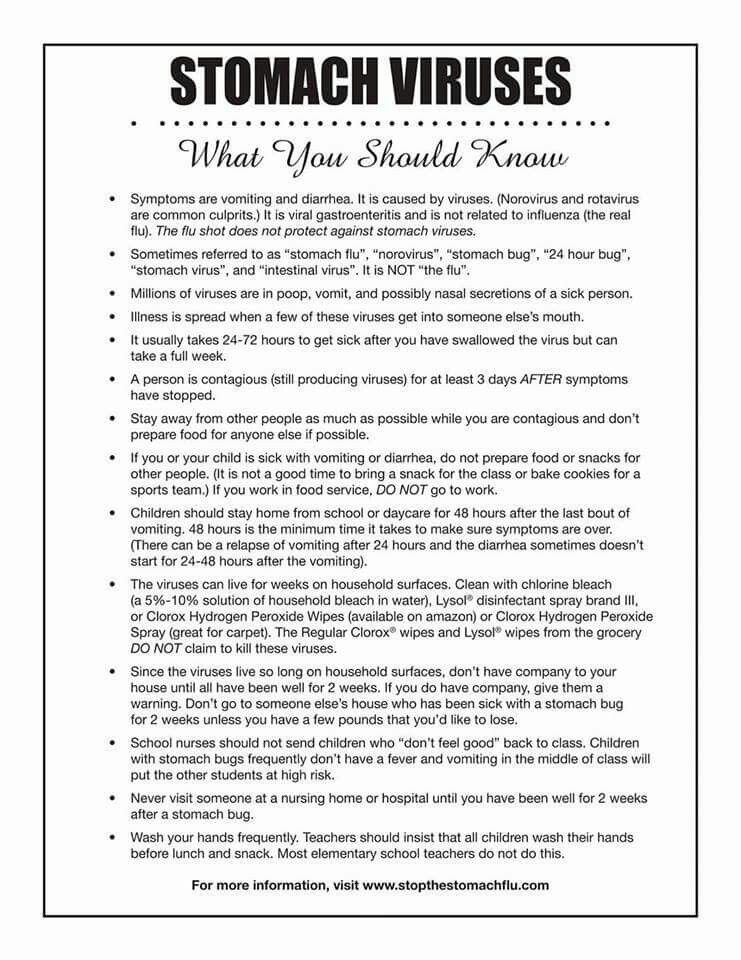
- irritation from a viral or bacterial infection, like the stomach bug
- fever
- pain, such as from a fever, earache, or vaccination
- blockage in the stomach or intestines
- chemicals in the blood, like medicine
- allergens, including pollen; very uncommon in babies under 1 year
- motion sickness, such as during a car ride
- dizziness, which might happen after being twirled around too much
- being upset or stressed
- strong smells
- milk intolerance
Vomiting is also common in healthy babies, but it might mean that your baby has caught a bug or is feeling a bit under the weather.
Too much vomiting can cause dehydration and even weight loss in very serious cases. Milk feeding can help prevent both of these. Offer your baby a feeding after they’ve stopped throwing up. If your baby is hungry and takes to the bottle or breast after vomiting, go right ahead and feed them.
Liquid feeding after vomiting can sometimes even help settle your baby’s nausea. Start with small amounts of milk and wait to see if they vomit again. Your baby might vomit the milk right back up, but it’s better to try than not.
If your little one is at least 6 months old and doesn’t want to feed after throwing up several times, offer them water in a bottle or a spoon. This can help prevent dehydration. Wait a short while and try feeding your baby again.
In some cases, it’s better not to feed a baby right after vomiting. If your baby is throwing up because of an earache or fever, they may benefit from medication first.
Most pediatricians recommend pain medications like infant Tylenol for babies in their first year. Ask your doctor about the best medication and dosage for your baby.
Ask your doctor about the best medication and dosage for your baby.
If giving pain medication based on your doctor’s advice, wait about 30 to 60 minutes after doing so to feed your little one. Feeding them too soon might cause another bout of vomiting before the meds can work.
Motion sickness isn’t common in babies under the age of 2 years, but some babies may be more sensitive to it. If your baby vomits from motion sickness, it’s better not to offer a feeding afterward.
You’re in luck if your baby likes to nod off in the car. Wait until you’re out of the car to feed your baby milk.
Baby vomiting can be worrying, but it usually goes away by itself — even if your baby has the stomach bug. Most babies with gastroenteritis don’t need medical treatment. This means that most of the time, you’ll have to bravely wait out your baby’s vomiting.
But sometimes, throwing up is a sign that something’s not right. You know your baby best. Trust your gut and call their doctor if you feel your little one is unwell.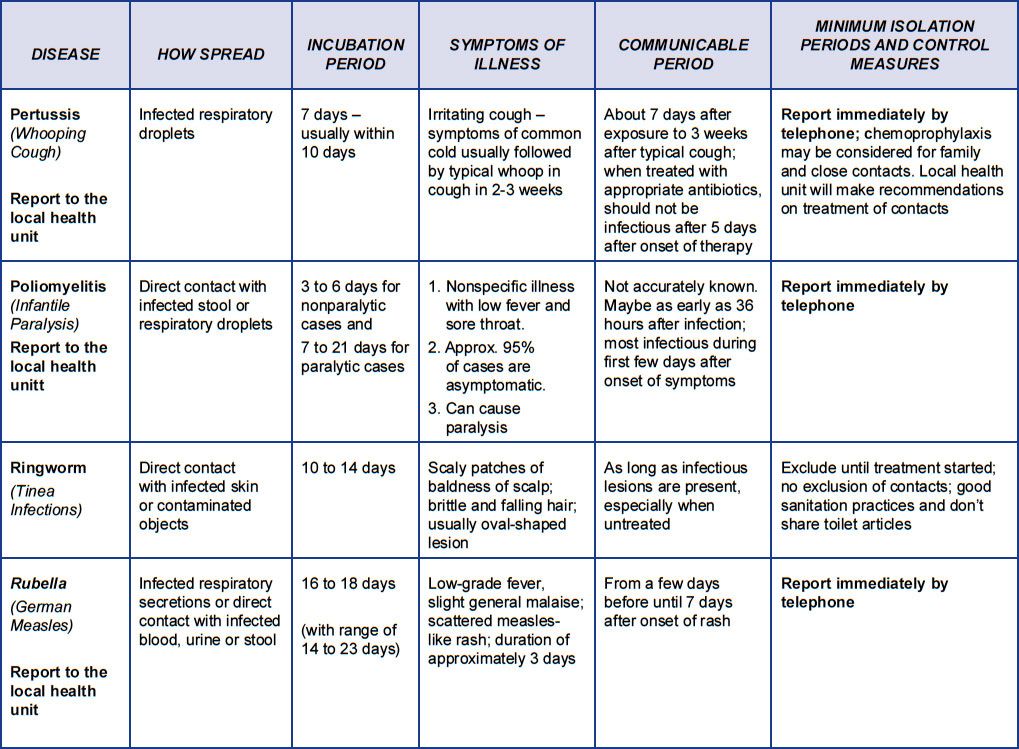
In addition, take your baby to a doctor immediately if they’ve been vomiting for 12 hours or longer. Babies and children can dehydrate quickly from too much vomiting.
Also call your baby’s pediatrician if your baby can’t hold anything down and has signs and symptoms of being unwell. These include:
- constant crying
- pain or discomfort
- refusal to feed or drink water
- diaper that hasn’t been wet for 6 hours or longer
- diarrhea
- dry lips and mouth
- crying without tears
- extra sleepiness
- floppiness
- vomiting blood or fluid with black flecks (“coffee grounds”)
- lack of smile or response
- vomiting green fluid
- bloated tummy
- blood in bowel movements
You won’t usually have any control over when or how much your baby vomits. When it happens on occasion, repeat this mantra to help you cope: “Healthy babies sometimes vomit.”
However, if your baby often vomits (or spits up) after feeding, you may be able to take some preventative steps. Try these tips:
Try these tips:
- avoid overfeeding
- give your baby smaller, more frequent feeds
- burp your baby often between feeds and after feeds
- prop up your baby so they’re upright for at least 30 minutes after feeding (but don’t prop your baby up for sleep or use anything to position them in their crib or elevate their mattress)
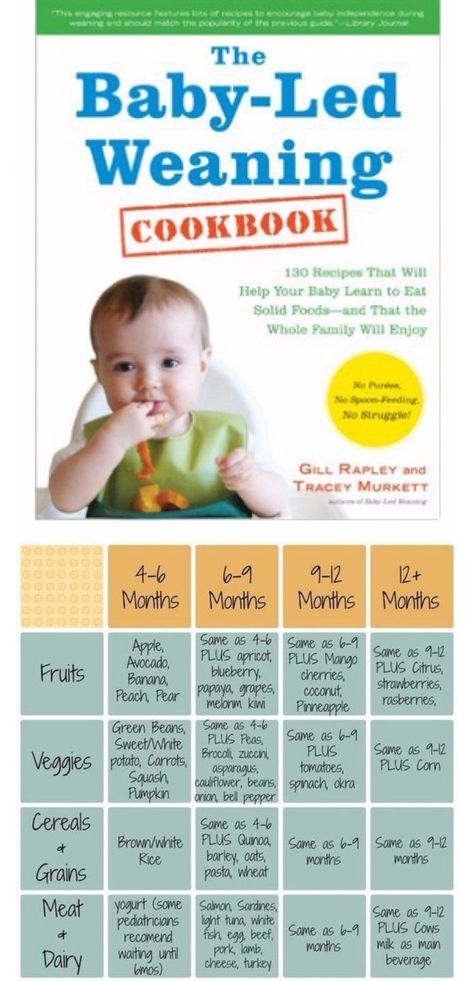
If your baby has a tummy bug and is old enough to eat solid foods, avoid feeding solids for about 24 hours. A liquid diet can help the stomach settle after a bout of vomiting.
Vomiting and spit-up are common in healthy babies. In most cases, you can milk feed shortly after your baby vomits. This helps to prevent your baby from getting dehydrated.
In some cases it’s best to wait a little while before trying to feed your baby again. If you’re giving your child medication like pain and fever relievers, wait a bit so the meds don’t come back up.
If your baby is vomiting a lot or seems otherwise unwell, call your pediatrician immediately. If you’re unsure if your baby’s vomiting or spit-up is cause for concern, it’s always best to check with your doctor.
If you’re unsure if your baby’s vomiting or spit-up is cause for concern, it’s always best to check with your doctor.
How to Know Whether You Should
Your baby just threw up all the milk they’ve chugged down so far, and you’re wondering if it’s OK to continue feeding. How soon should you feed your baby after vomiting?
It’s a good question — just about every parent has likely pondered this. Spit-up is almost a rite of passage for babies (and parents). Baby vomiting is also common and can happen for many reasons. Most of the causes aren’t serious.
The short answer — because you may have a very fussy baby on your hands and want to get back to them ASAP — is yes, you can usually feed your baby after they vomit all over your favorite sweater, sofa throw, and rug.
Here’s just about everything you need to know about feeding your baby after vomiting.
Baby vomit and spit-up are two different things — and they can have different causes. Spitting up is common in babies under the age of 1 year. It typically happens after feeding. Spit-up is usually an easy flow of milk and saliva that dribbles from your baby’s mouth. It often happens with a burp.
It typically happens after feeding. Spit-up is usually an easy flow of milk and saliva that dribbles from your baby’s mouth. It often happens with a burp.
Spit-up is normal in healthy babies. It can happen for several reasons. About half of all babies 3 months and under have a type of acid reflux called infant reflux.
Spit-up from infant reflux is especially bound to happen if your baby has a full stomach. Being careful not to overfeed a bottle-fed infant can help. Spitting up typically stops by the time your baby is a year old.
On the other hand, vomiting is typically a more forceful throwing-up of milk (or food, if your baby is old enough to eat solids). It happens when the brain signals the muscles around the stomach to squeeze.
Vomiting (like gagging) is a reflex action that can be triggered by a number of things. These include:
- irritation from a viral or bacterial infection, like the stomach bug
- fever
- pain, such as from a fever, earache, or vaccination
- blockage in the stomach or intestines
- chemicals in the blood, like medicine
- allergens, including pollen; very uncommon in babies under 1 year
- motion sickness, such as during a car ride
- dizziness, which might happen after being twirled around too much
- being upset or stressed
- strong smells
- milk intolerance
Vomiting is also common in healthy babies, but it might mean that your baby has caught a bug or is feeling a bit under the weather.
Too much vomiting can cause dehydration and even weight loss in very serious cases. Milk feeding can help prevent both of these. Offer your baby a feeding after they’ve stopped throwing up. If your baby is hungry and takes to the bottle or breast after vomiting, go right ahead and feed them.
Liquid feeding after vomiting can sometimes even help settle your baby’s nausea. Start with small amounts of milk and wait to see if they vomit again. Your baby might vomit the milk right back up, but it’s better to try than not.
If your little one is at least 6 months old and doesn’t want to feed after throwing up several times, offer them water in a bottle or a spoon. This can help prevent dehydration. Wait a short while and try feeding your baby again.
In some cases, it’s better not to feed a baby right after vomiting. If your baby is throwing up because of an earache or fever, they may benefit from medication first.
Most pediatricians recommend pain medications like infant Tylenol for babies in their first year.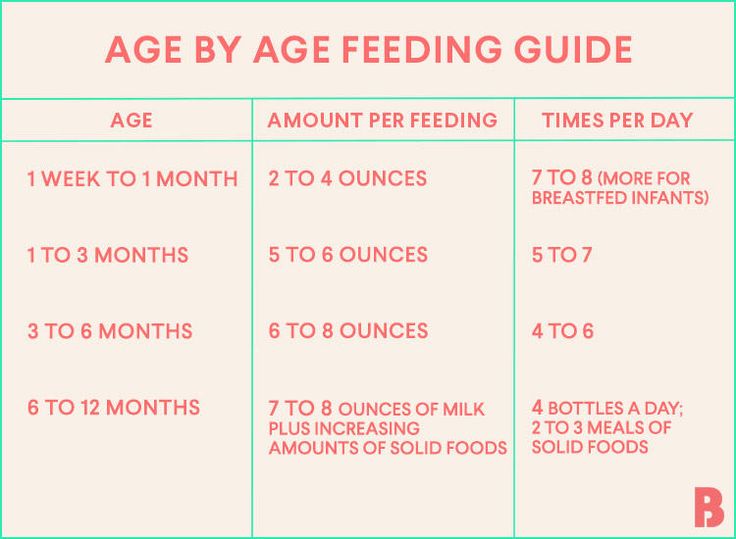 Ask your doctor about the best medication and dosage for your baby.
Ask your doctor about the best medication and dosage for your baby.
If giving pain medication based on your doctor’s advice, wait about 30 to 60 minutes after doing so to feed your little one. Feeding them too soon might cause another bout of vomiting before the meds can work.
Motion sickness isn’t common in babies under the age of 2 years, but some babies may be more sensitive to it. If your baby vomits from motion sickness, it’s better not to offer a feeding afterward.
You’re in luck if your baby likes to nod off in the car. Wait until you’re out of the car to feed your baby milk.
Baby vomiting can be worrying, but it usually goes away by itself — even if your baby has the stomach bug. Most babies with gastroenteritis don’t need medical treatment. This means that most of the time, you’ll have to bravely wait out your baby’s vomiting.
But sometimes, throwing up is a sign that something’s not right. You know your baby best. Trust your gut and call their doctor if you feel your little one is unwell.
In addition, take your baby to a doctor immediately if they’ve been vomiting for 12 hours or longer. Babies and children can dehydrate quickly from too much vomiting.
Also call your baby’s pediatrician if your baby can’t hold anything down and has signs and symptoms of being unwell. These include:
- constant crying
- pain or discomfort
- refusal to feed or drink water
- diaper that hasn’t been wet for 6 hours or longer
- diarrhea
- dry lips and mouth
- crying without tears
- extra sleepiness
- floppiness
- vomiting blood or fluid with black flecks (“coffee grounds”)
- lack of smile or response
- vomiting green fluid
- bloated tummy
- blood in bowel movements
You won’t usually have any control over when or how much your baby vomits. When it happens on occasion, repeat this mantra to help you cope: “Healthy babies sometimes vomit.”
However, if your baby often vomits (or spits up) after feeding, you may be able to take some preventative steps. Try these tips:
Try these tips:
- avoid overfeeding
- give your baby smaller, more frequent feeds
- burp your baby often between feeds and after feeds
- prop up your baby so they’re upright for at least 30 minutes after feeding (but don’t prop your baby up for sleep or use anything to position them in their crib or elevate their mattress)
If your baby has a tummy bug and is old enough to eat solid foods, avoid feeding solids for about 24 hours. A liquid diet can help the stomach settle after a bout of vomiting.
Vomiting and spit-up are common in healthy babies. In most cases, you can milk feed shortly after your baby vomits. This helps to prevent your baby from getting dehydrated.
In some cases it’s best to wait a little while before trying to feed your baby again. If you’re giving your child medication like pain and fever relievers, wait a bit so the meds don’t come back up.
If your baby is vomiting a lot or seems otherwise unwell, call your pediatrician immediately. If you’re unsure if your baby’s vomiting or spit-up is cause for concern, it’s always best to check with your doctor.
If you’re unsure if your baby’s vomiting or spit-up is cause for concern, it’s always best to check with your doctor.
Treatment of food poisoning in a child
Food poisoning is an acute infectious-toxic pathology. It occurs when eating poor-quality products that contain pathogens, toxic substances and poisons. The main manifestations are diarrhea, vomiting, fever, signs of dehydration and severe intoxication. The task of treatment is to quickly stop the symptoms of poisoning, replenish fluid deficiency, and prevent the development of complications.
Class
Food poisoning is referred to as toxic infection or intoxication. Pathology develops after the use of low-quality food, water, plant, chemical or medicinal toxic substances.
There are two types of food poisoning in children:
- Infectious. The causative agents are microbes and their toxic waste products.
- Non-infectious. Caused by toxic substances of plant, animal origin, toxic impurities.
The asymptomatic or latent stage of food poisoning begins from the moment the toxins enter the body until the first symptoms appear. The duration depends on the individual characteristics and age of the child, the amount and rate of absorption of poisons. This stage is most favorable for therapy, since toxic substances have not yet penetrated into the blood.
The toxicogenic stage begins with the appearance of the first symptoms of poisoning and lasts until bacteria and poisons are completely eliminated from the body. This period is characterized by the manifestation of all symptoms of poisoning. In order for the treatment to be effective, it is necessary to identify toxins and accelerate the process of elimination.
At the last stage of convalescence, the disturbed functions of the organs of the digestive, excretory, and immune systems are restored.
Causes
Food poisoning is one of the most common problems in pediatrics. In children, intoxication is more severe than in adults.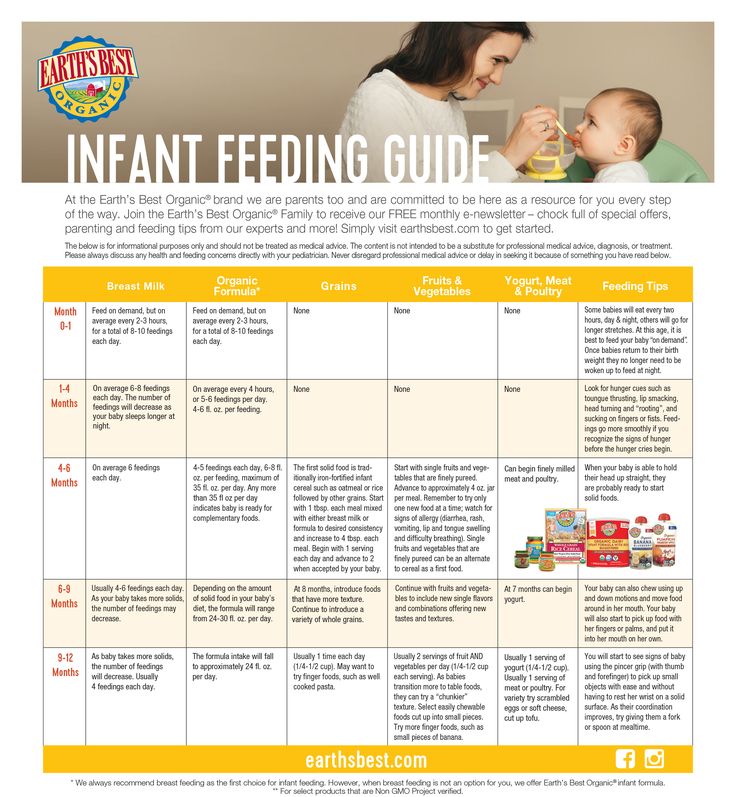 This is due to the characteristics of the child's body: low acidity of gastric juice, incompletely formed intestinal microflora, rapid absorption of poisons and the spread of toxins throughout the body.
This is due to the characteristics of the child's body: low acidity of gastric juice, incompletely formed intestinal microflora, rapid absorption of poisons and the spread of toxins throughout the body.
The main causative agents of food poisoning in children are staphylococci, proteus, klebsiella, enterotoxigenic strains of E. coli, clostridia. Pathogens enter the body only with food, in which they multiply, release toxins.
Causes of violation of food quality:
- non-compliance with sanitary and hygienic standards;
- violation of the rules for storage, preparation and sale of food products;
- contamination of food by people with intestinal infections, purulent pathologies - tonsillitis, furunculosis, panaritium, mastitis, streptoderma;
- contamination of soil and plants by animal feces.
Spoiled products may have an unpleasant taste, smell, uncharacteristic texture, but often organoleptic indicators remain within the normal range.
Non-infectious poisoning - a consequence of accidental consumption of poisonous berries or plants, mushrooms. Intoxication can occur after eating agricultural products that are contaminated with poisonous fungicides, insecticides.
Which products are classified as potentially hazardous?
In children, food poisoning often occurs after drinking unboiled water, missing milk or dairy products.
Dangerous products include:
- eggs;
- cream confectionery;
- fish and seafood;
- sausages;
- meat, vegetable preserves;
- mushrooms.
Food poisoning is most often diagnosed in summer and autumn. During this period, the conditions for the reproduction of microbial pathogens are the most favorable.
Symptoms of food poisoning in a child
Despite the variety of toxic infections, clinical manifestations are largely similar. The latent stage lasts an average of 2-6 hours, sometimes no more than 30 minutes or more than a day. Signs of poisoning are manifested by symptoms of gastroenteritis, intoxication, dehydration.
Signs of poisoning are manifested by symptoms of gastroenteritis, intoxication, dehydration.
Poisoning always begins acutely - nausea, repeated vomiting with particles of undigested food. The child complains of abdominal pain, watery stools, mucous membranes, green impurities, blood streaks. Bowel emptying occurs up to 5-10 times a day.
Simultaneously with dyspeptic disorders, the temperature rises to 38–39 degrees. Signs of intoxication quickly increase: refusal to eat, headache and muscle pain. Symptoms of dehydration appear: the skin is pale and dry, facial features are sharpened, the number of urination decreases, the mucous membranes dry out. In infants, the fontanel sinks. With food poisoning, convulsions often occur, acidosis develops.
In most cases, signs of poisoning gradually disappear after 2-3 days, but weakness and abdominal pain may persist for several weeks.
Severe forms of food poisoning are predominantly observed in young children with weakened immunity. The risk of developing complications against the background of intoxication increases with prematurity, malnutrition and dysbacteriosis in history.
The risk of developing complications against the background of intoxication increases with prematurity, malnutrition and dysbacteriosis in history.
If a child is poisoned by poisonous plants, berries, lesions of the central nervous system are observed:
- retardation of reactions;
- euphoria;
- hallucinations;
- impaired speech, vision;
- convulsions.
If the cardiovascular system is damaged by toxins, the heart rate speeds up or slows down, blood pressure decreases.
Mushroom poisoning is very dangerous for children. After eating a pale toadstool, indomitable vomiting, cholera-like diarrhea with impurities of blood in the feces begins. Other symptoms are intestinal colic, respiratory disorders, convulsions. Toxins adversely affect the liver, which leads to the development of toxic hepatitis. AT 90% of cases are fatal due to acute liver failure.
Signs of fly agaric poisoning are increased salivation, shortness of breath, severe vomiting, convulsions, bronchospasm, hallucinations, nystagmus or strabismus.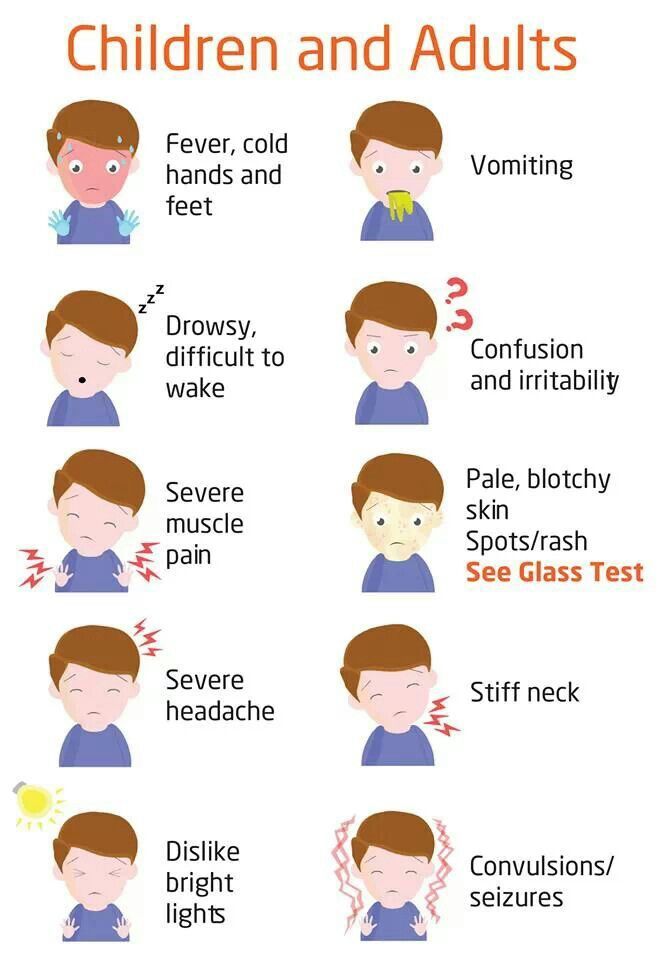 But the mortality rate is less than 1%.
But the mortality rate is less than 1%.
Botulism develops when poor-quality canned food is consumed. The toxin affects the nervous system, which manifests itself in the form of paralysis and paresis. Poisoning in children can cause the development of acute respiratory failure, heart rhythm disturbances. The first symptoms appear after 4-6 hours. Worries about pain in the epigastric region, nausea, vomiting, diarrhea. Sometimes there are problems with vision. When the respiratory system is affected, shortness of breath begins, the skin in the region of the nasolabial triangle turns blue, and arrhythmia develops.
First aid for child poisoning
Act immediately. First aid rules:
- In case of poisoning with mushrooms, berries, medicines, induce vomiting.
- Gastric lavage with clean water to remove toxins from the intestines. Babies should not do the washing themselves, as the child can inhale the vomit. Instead, you can do a cleansing enema.
 The volume of water for gastric lavage - 16 ml / kg for children 3-6 years old, over 7 years old - 14 ml / kg.
The volume of water for gastric lavage - 16 ml / kg for children 3-6 years old, over 7 years old - 14 ml / kg. - Taking enterosorbents - these drugs collect toxins in the intestinal lumen, remove them with feces.
- More to drink. You need to drink in small portions, but often. You can give your child water with a weak saline solution, weak tea, mineral water without gas.
- Call a doctor.
Timely first aid will help to avoid the development of complications of poisoning.
In case of poisoning, children should not:
- give painkillers, drugs, drugs for vomiting and diarrhea;
- apply hot or cold compresses to the abdomen;
- use soda to induce vomiting, potassium permanganate to wash the stomach;
- give milk and dairy products.
Diagnosis of food poisoning in a child
Diagnosis of food poisoning in a child can be done by a pediatrician or an infectious disease specialist. The examination begins with the collection of anamnesis, examination of the patient.
The examination begins with the collection of anamnesis, examination of the patient.
Specific diagnostic tests are prescribed to isolate the pathogen. Biomaterial - feces and vomit, gastric lavage, the remains of contaminated food. With a generalized form of infection, a blood culture is prescribed. Auxiliary methods - RIF, PCR, ELISA. Additionally, you may need to consult a neurologist, gastroenterologist, surgeon.
Be sure to carry out differential diagnosis to exclude acute gastritis, cholecystitis, pancreatitis, giardiasis, acute intestinal infection, inflammation of the appendix, meningitis. A blood test is prescribed to rule out a viral, bacterial infection, a stool test to detect infections caused by pathological bacteria.
How to treat
Treatment of poisoning in a child begins with the elimination of signs of dehydration. Apply oral, parenteral rehydration therapy.
Auxiliaries:
- enzymes;
- sorbents;
- prebiotics to restore the balance of intestinal microflora;
- antimicrobials are necessary for severe toxic infection.

In case of toadstool poisoning, emergency hemosorption is performed to cleanse the blood of toxins.
Diet for child poisoning
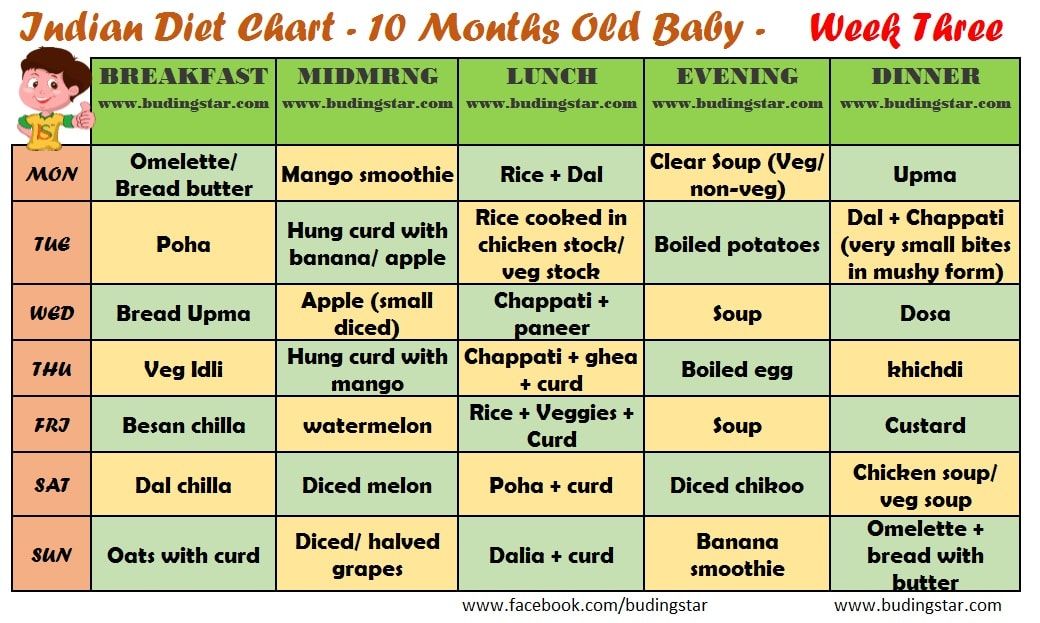
It is best not to feed the child for 12-24 hours after poisoning. When vomiting stops, a sparing diet is indicated. Breastfed babies under one year of age need to skip a few feedings.
How to feed a child after poisoning:
- liquid porridge - rice, buckwheat, cooked in a mixture of equal amounts of water and milk;
- slimy soups;
- crackers;
- kefir;
- compotes;
- after a few days - vegetable puree, children's cottage cheese or kefir, yogurt without additives;
- gradually introduce meat and fish soufflé into the menu.
List of prohibited products - pastries, whole milk, black bread, fresh white bread. You can not give your child pasta, chocolate, ice cream, chips, sweet carbonated drinks, wheat and barley porridge. From vegetables, cucumbers, tomatoes, cabbage are contraindicated.
The duration of the diet is 14 days.
Possible consequences of food poisoning in a child
Complications occur in case of severe poisoning, lack of correct and timely therapy.
Possible effects:
- dysbacteriosis;
- renal and hepatic insufficiency;
- disturbances in the functioning of the nervous and immune systems;
- chronic diseases of the gastrointestinal tract.
Prognosis and prevention
Poisoning in a child of mild and moderate severity ends in complete recovery.
Methods of prevention:
- properly store food, observe the temperature regime and other storage conditions;
- observe the rules of heat treatment, children should absolutely not be given raw fish, poorly fried meat;
- drink only boiled, purified water, do not swallow water when swimming in reservoirs;
- wash hands, vegetables and fruits thoroughly;
- store medicines, chemicals out of the reach of children;
- to tell children about poisonous mushrooms, berries, plants, the dangers of their use.

People who work in the kitchen in children's institutions should have regular medical check-ups. In the presence of pustular skin pathologies, respiratory diseases, signs of an intestinal infection, the worker is not allowed into the catering unit.
Treatment of food poisoning in Moscow
Food poisoning in a child is a dangerous condition, you should not self-medicate, you should immediately consult a doctor. Call our clinic, describe the symptoms, the patient's condition, the possible cause of the poisoning. The administrator of the "Miracle Doctor" center will write you to the doctor in the near future.
Q&A
Why is acute poisoning dangerous for a child?
Fever, vomiting more often 3–5 times, diarrhea in a child is a reason to immediately call an ambulance.
Poisoning in a child at any age leads to a breakdown of the immune system. Dehydration is very dangerous for babies. In children under 4 years of age with profuse vomiting and loose stools, the critical phase of dehydration can occur within a few hours.
How to give water to a baby if he vomits very often?
Even if the vomiting is severe and persistent, the child must be given water. The consequences of dehydration are extremely dangerous for the child's body. You need to water the child in small portions - 1 tsp each. every 5 minutes. Water should not be cold, so as not to cause spasm and vomiting. The optimal temperature is a few degrees above body temperature.
what to feed the child, menus and recipes
In case of food poisoning, the general well-being of the child noticeably deteriorates, he begins to cry, act up, complain of pain in the abdomen. After a while, the classic signs of intoxication make themselves felt: nausea, vomiting, stool disorders. The temperature may rise, the head hurts. The severity of the condition depends on which pathogen entered the child's body with spoiled food. << In intestinal infections accompanied by chronic diarrhea, the leading mechanism is indigestion, which leads to disruption of the processes of splitting and absorption in the intestines of basic nutrients, water, vitamins, macro- and microelements, says Dina Sergeevna Rusinova, Candidate of Medical Sciences, infectious disease specialist, gastroenterologist of the MEDSI Children's Clinic on Pirogovskaya, Associate Professor of the Department of Faculty Pediatrics, Russian National Research Medical University. IN AND. Pirogov. - Developing diarrhea (loose and frequent stools) is accompanied by weight loss, the development of anemia and even osteoporosis>>.
IN AND. Pirogov. - Developing diarrhea (loose and frequent stools) is accompanied by weight loss, the development of anemia and even osteoporosis>>.
In case of poisoning, first of all, the child's stomach should be washed with boiled water at room temperature. Then give one of the sorbents.
In the photo: Dina Sergeevna Rusinova, Candidate of Medical Sciences, infectious disease specialist, gastroenterologist at the MEDSI Children's Clinic on Pirogovskaya, Associate Professor of the Department of Faculty Pediatrics of the Russian National Research Medical University. IN AND. Pirogov.
What can a child eat in case of food poisoning
First of all, a child after food poisoning, regardless of age, does not need food, but plenty of fluids - intoxication is always accompanied by a significant loss of fluid due to vomiting and diarrhea. <
Diet after poisoning
When a child is tormented by bouts of vomiting, as a rule, he does not need food - his appetite at this time disappears sharply. It is not necessary to insist, to try to force-feed the baby: nausea and vomiting will only intensify. In the acute period of the disease, as already mentioned, it is much more important to organize the correct drinking regimen. However, it is impossible to put a baby on a starvation diet. << An important point in the organization of nutrition of children with disorders of the gastrointestinal tract as a result of food poisoning or intestinal infection is the refusal of a water-tea break, as it has been proven that even with severe forms of diarrhea, the digestive function of most of the intestine is preserved, says our expert. - And a starvation diet slows down the recovery process, contributes to malnutrition and significantly weakens the body's defenses. These are the recommendations of the World Health Organization and the Russian Union of Pediatricians. The volume and composition of nutrition depend on the age of the children, the severity of the diarrheal syndrome, concomitant diseases. Rational feeding is important for the rapid restoration of bowel function and the prevention of weight loss in the child>>.
The volume and composition of nutrition depend on the age of the children, the severity of the diarrheal syndrome, concomitant diseases. Rational feeding is important for the rapid restoration of bowel function and the prevention of weight loss in the child>>.
When formulating a diet in case of poisoning in a child , pediatricians advise to adhere to the following rules.
- Feed your baby often, up to seven times a day. Portions should be small. This mode will allow the body to recover faster.
- The baby's diet should contain a sufficient amount of animal protein, primarily milk, which has a lipotropic effect. This is necessary to support the liver, which, when poisoned, experiences an increased load, neutralizing toxic elements.
- Carbohydrate-rich food should be present in the child's diet in a minimum amount, especially during the acute period of the disease - carbohydrates enhance fermentation processes in the intestines and slow down the healing process.
When compiling a diet for a child, one should take into account the manifestations of the disease: which part of the gastrointestinal tract has suffered from a toxic pathogen, how pronounced inflammation is and how functions are impaired. For example, if a child is only concerned about pain in the stomach and vomiting, the diet is based on the principle of a diet for acute gastritis. If the disease has captured the lower sections of the gastrointestinal tract and the child has diarrhea, then when compiling the menu, the specifics of digestion in the small intestine should also be taken into account. << With diarrhea, there is a violation of the absorption of carbohydrates as a result of enzyme deficiency and a fermentation process (flatulence), which is manifested by the child's anxiety, bloating, splashing foamy stools, says Dina Sergeevna. - In these cases, it is necessary to limit (in severe cases, completely eliminate) dairy products and prescribe low-lactose and lactose-free products.