Supplementary feeding breastfed baby
Breastfeeding FAQs: Solids and Supplementing (for Parents)
Breastfeeding is a natural thing to do, but it still comes with its fair share of questions. Here's what you need to know about about introducing formula, solids, and more.
Is it OK to Give My Baby Breast Milk and Formula?
Breast milk is the best nutritional choice for babies. But in some cases, breastfeeding (or exclusive breastfeeding) isn’t possible or an option. What’s best for your baby's health and happiness is, in large part, whatever works for your family. So if you need to supplement, your baby will be fine and healthy, especially if it means less stress for you.
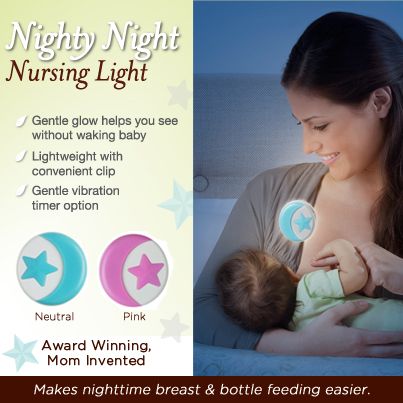
Babies who need supplementation may do well with a supplemental nursing system. This is when moms place a small tube by their nipple that delivers pumped milk or formula while a baby is breastfeeding.
Babies also can get pumped milk or formula by bottle. But it’s a good idea to wait until your baby has gotten used to and is good at breastfeeding. Lactation professionals recommend waiting until a baby is about 3-4 weeks old before offering artificial nipples of any kind (including pacifiers).
If I Give My Baby Formula, How Do I Start?
If you're using formula because you're not producing the amount of milk your baby needs, nurse first. Then, give any pumped milk you have and make up the difference with formula as needed.
If you're stopping a breastfeeding session or are weaning from breastfeeding altogether, begin to replace breastfeeding with bottle feeds. As you do this, pump to reduce uncomfortable engorgement. Engorgement is when your breasts overfill with milk and other fluids and get painful, swollen, warm, or hard. This can lead to problems with plugged ducts (when the ducts won’t drain well or at all) or a breast condition called mastitis.
When you reduce the number of nursing sessions, your milk supply will decrease. Your body will adapt to produce just enough milk to fit your new feeding schedule.
How Might a Diet With Formula Affect My Baby?
Starting your breastfed baby on formula can cause some change in the frequency, color, and consistency of your baby’s poop. Be sure to talk your doctor, though, if your baby has trouble pooping.
If your baby refuses formula alone, you can try mixing some of your pumped breast milk with it to help the baby get used to the new taste.
Is it OK for Me to Give My Baby the First Bottle?
If possible, have someone else give the first bottle. This is because babies can smell their mothers and they're used to receiving breast milk from mom, not a bottle. So try to have someone else — like a caregiver or partner — give the first bottle.
Also consider being out of the house or out of sight when your baby takes that first bottle, since your little one will wonder why you're not doing the feeding as usual. Depending on how your baby takes to the bottle, you might need to keep doing this until your baby gets used to bottle feeding.
If your baby has a hard time adjusting to this new form of feeding, be patient and keep trying. Talk to your doctor if you have questions.
Does My Breastfed Baby Need Supplements?
Breast milk contains many vitamins and minerals. But it’s a good idea to give a daily supplement for some nutrients that may be lacking. It all depends on your baby’s age.
Here are some guidelines:
- Vitamin D. Breastfed babies need to take a daily vitamin D supplement. Vitamin D is added to infant formulas. Vitamin D is made by the body when the skin is exposed to sunlight, but it is not safe for infants under 6 months to be in direct sunlight. (After 6 months, use sunscreen when in the sun to protect your baby’s sensitive skin).
- Iron. Iron is a mineral found in breastmilk during the first 4 months of life. After that, babies need an iron supplement until they begin eating enough iron-rich foods (such as cereals or meats) when they’re around 6 months old.
 If your baby gets a mix of breast milk and iron-fortified formula, talk to your doctor about whether your little one needs a supplement. After they start on solids, some babies still need iron supplements if they don’t eat enough iron-rich foods. You doctor can tell you if your baby is getting enough iron.
If your baby gets a mix of breast milk and iron-fortified formula, talk to your doctor about whether your little one needs a supplement. After they start on solids, some babies still need iron supplements if they don’t eat enough iron-rich foods. You doctor can tell you if your baby is getting enough iron. - Fluoride. Babies younger than 6 months do not need a fluoride supplement. After your baby is 6 months old, you can start supplementing with fluoride if your water supply lacks fluoride. Well water, bottled water, tap water in some communities, and ready-to-feed formulas do not have fluoride.
It’s important to find out if your water supply has fluoride in it. You can ask your doctor, dentist, or local water utility agency if the water in your community is fluoridated. Giving a child too much fluoride can cause white marks on the teeth, so there is no need to give a fluoride supplement if your child gets enough fluoride from water.
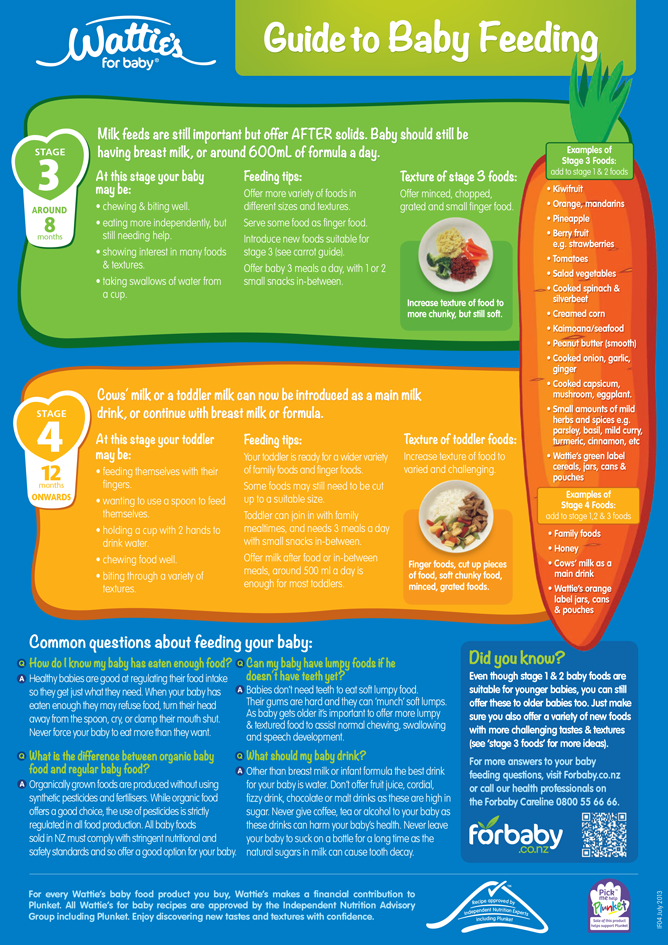
When Should I Introduce Solid Foods?
The best time to introduce solid foods is when your baby has the skills needed to eat, usually between 4 and 6 months of age. This is when your baby:
This is when your baby:
- has good head and neck control
- can sit up
- has lost the tongue-thrust reflex (which causes babies to push food out of the mouth)
- has the motor skills needed to transfer food to the back of the mouth to swallow
- shows an interest in food (by watching others eat, reaching for food, or opening the mouth as food approaches)
By this age, babies usually weigh twice their birth weight, or close to it.
Wait until your baby is at least 4 months old and shows these signs of readiness before starting solids. Many babies exclusively breastfeed until 6 months of age, which is perfectly healthy.
Babies who start solid foods before 4 months are at a higher risk for obesity and other problems later on. They also aren't coordinated enough to safely swallow solid foods and may choke on the food or inhale it into their lungs.
How Should I Start Solids?
When the time is right, start with a single-grain, iron-fortified baby cereal. Rice cereal has traditionally been the first food for babies, but you can start with any you prefer. Start with 1 or 2 tablespoons of cereal mixed with breast milk, formula, or water. Never add cereal to a baby's bottle unless your doctor recommends it.
Rice cereal has traditionally been the first food for babies, but you can start with any you prefer. Start with 1 or 2 tablespoons of cereal mixed with breast milk, formula, or water. Never add cereal to a baby's bottle unless your doctor recommends it.
Another good first option is an iron-rich puréed meat. Feed your baby with a small baby spoon.
At this stage, solids should be fed after a nursing session, not before. That way, your baby fills up on breast milk, which should be your baby's main source of nutrition until age 1.
When your baby gets the hang of eating the first food, introduce others, such as puréed fruits, vegetables, beans, lentils, or yogurt. Wait a few days between introducing new foods to make sure your baby doesn't have an allergic reaction.
Experts recommend introducing common food allergens to babies when they're 4–6 months old. This includes babies with a family history of food allergies. In the past, they thought that babies should not get such foods (like eggs, peanuts, and fish) until after the first birthday.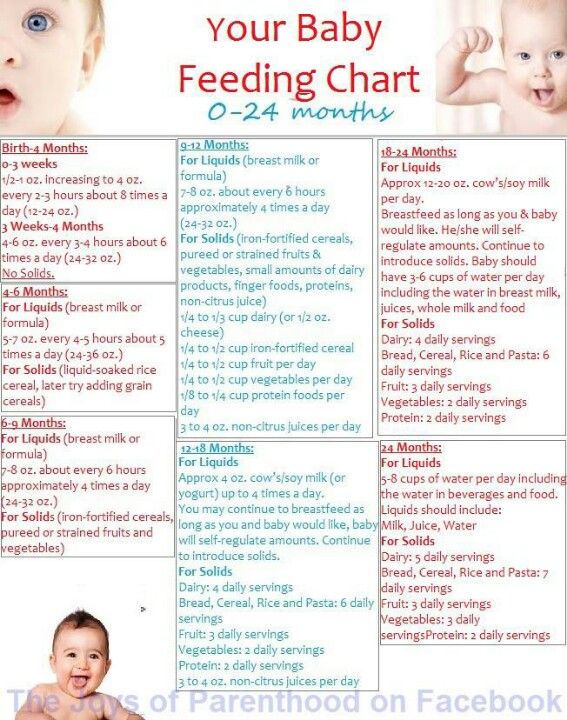 But recent studies suggest that waiting that long could make a baby more likely to develop food allergies.
But recent studies suggest that waiting that long could make a baby more likely to develop food allergies.
Offer these foods to your baby as soon as your little one starts eating solids. Make sure they're served in forms that your baby can easily swallow. You can try a small amount of peanut butter mixed into fruit purée or yogurt, for example, or soft scrambled eggs.
When Can I Give My Baby Water?
In their first few months, babies usually don't need extra water. Breast milk and formula supply all the fluids that your baby needs. On very hot days, most babies do well with extra feedings.
When your baby starts eating solid foods, you can offer a few ounces of water between feedings, but don't force it.
What About Juice?
Fruit juices are not recommended for babies. Juice offers no health benefits, even to older children. Juice can fill them up (leaving little room for more nutritious foods), promote obesity, cause diarrhea, and even put a baby at risk for cavities when teeth start coming in.
Supplemental feedings for the breastfed baby
With good instruction and support, most moms can breastfeed their babies exclusively for the first six months (and continue breastfeeding beyond). Unfortunately, many U.S. newborns are still fed something other than their own mother’s milk during their initial hospital stay. These supplemental, or supplementary, feedings are typically artificial infant formula, but they may be donor human milk or glucose water. Because unnecessary supplementation in the hospital has been associated with less exclusive breastfeeding, as well as a shorter duration of any breastfeeding, the Academy of Breastfeeding Medicine (ABM) has issued guidance on when otherwise healthy babies need supplementation or not.
When supplementation may not be necessary
The ABM encourages parents and health care providers to adopt a preventive approach to supplementation with:
- prenatal education
- in-hospital breastfeeding support
- breastfeeding immediately after birth
- skin-to-skin care after birth
- rooming-in
- instruction on milk expression (if necessary, such as when the mother and her infant must be separated)
In some cases, concern about a baby’s weight loss is identified as a reason for supplemental feedings. All babies do lose weight after birth. While this can be scary to new parents, it doesn’t necessarily mean that their baby isn’t feeding well; many factors influence the baby’s birth weight and weight changes, including gestational age, the method of birth (vaginal or cesarean), and the amount of fluid the mother received during labor. As long as the infant is “feeding well, urinating and stooling adequately,” and has weight loss “in the expected range” while “bilirubin levels are not of concern,” the ABM recommends adopting a watch and wait approach.
All babies do lose weight after birth. While this can be scary to new parents, it doesn’t necessarily mean that their baby isn’t feeding well; many factors influence the baby’s birth weight and weight changes, including gestational age, the method of birth (vaginal or cesarean), and the amount of fluid the mother received during labor. As long as the infant is “feeding well, urinating and stooling adequately,” and has weight loss “in the expected range” while “bilirubin levels are not of concern,” the ABM recommends adopting a watch and wait approach.
During this time, parents can focus on:
- recognizing early feeding cues
- keeping the baby safely skin-to-skin with the awake mother
- gently awakening the baby for frequent feedings
- hand expression of drops of colostrum to be fed to the baby
Parents, with the support of health care providers, should also pay attention to the baby’s feeding behavior, including the latch, positioning, and signs of discomfort. They should also look for signs of maternal fatigue, which can interfere with breastfeeding.
They should also look for signs of maternal fatigue, which can interfere with breastfeeding.
When supplementation may be necessary
There are situations in which supplementation may be necessary, even for an infant who is born full-term and seems healthy. The ABM identifies the following reasons for supplemental feeding of the infant during the hospital stay after birth:
- hypoglycemia that has been documented by lab test and is unresponsive to frequent breastfeeding; dextrose gel or intravenous (IV) glucose can be given, and breastfeeding should continue
- inadequate milk intake, as shown by significant dehydration, weight loss outside of normal range (with other factors), delayed or persistent meconium bowel movements (black, tarry stools)
- hyperbilirubinemia, sometimes with ongoing weight loss, few bowel movements, and uric acid crystals with urine; breastfeeding should continue during evaluation
- metabolic conditions of the newborn, requiring special supplements
- delayed maternal milk supply
- insufficient maternal mammary glands (estimated to affect less than 5 percent of women)
- past breast surgery affecting milk production
- medical cause, such as chemotherapy or other medication, or separation of mother and infant
- intolerable and unrelieved pain during breastfeeding
What supplement to give
Most parents find that even if they must, temporarily, give a supplement to their breastfed baby, breastfeeding can continue. The ABM ranks possible supplements in order of preference:
The ABM ranks possible supplements in order of preference:
- Mother’s own milk, gathered by hand expression or pump; use breast massage and/or warm compresses to help with letdown and consider pumping one breast while the baby breastfeeds on the opposite breast to increase milk yield.
- Donor human milk, which is preferable to artificial supplements.
- Protein hydrolysate formula, to avoid exposure to cow’s milk protein while conveying that supplementation is temporary.
- Other artificial formula, such as cow’s milk-based or soy-based formula, as determined appropriate for the baby’s age, amount needed, and potential effect on breastfeeding.
Note that glucose water is not considered an appropriate supplement, since it doesn’t provide nutrition or reduce bilirubin, and it poses a risk of hyponatremia or “water intoxication,” due to an imbalance of water and sodium in the body.
How to give a supplement
No single device has been shown to be better for all babies, and some babies may respond better to one feeding method than another. Mothers who are breastfeeding in addition to supplementing may wish to avoid bottles until 4-6 weeks after birth, since artificial nipples require different sucking patterns and can interfere with a baby’s ability to breastfeed (nipple confusion).
Mothers who are breastfeeding in addition to supplementing may wish to avoid bottles until 4-6 weeks after birth, since artificial nipples require different sucking patterns and can interfere with a baby’s ability to breastfeed (nipple confusion).
In addition to bottles, there are many options parents can use to provide supplemental feedings to their breastfed infants including:
- supplemental feeding devices (Lact-Aid or Supplemental Nursing System)
- cup
- spoon
- dropper
- syringe
When selecting how you will administer your baby’s supplemental feeding, the ABM encourages parents and health care providers to consider the following:
- cost and availability
- ease of use and cleaning (cup-feeding is preferable when hygiene is a concern)
- long-term or short-term use
- stress to the infant
- how much supplement can be fed in 20-30 minutes
- mother’s or caregiver’s preference
- expertise of health care provider
- effect on baby’s breastfeeding skills
- effect on mother’s milk supply (supplemental nursing devices provide breast stimulation, as well as skin-to-skin contact)
In most cases, supplementation is given temporarily to help you and your baby overcome a difficulty and to get back on track with breastfeeding. While your baby is receiving supplements, be sure to take steps to maintain and, if necessary, increase your milk supply.
While your baby is receiving supplements, be sure to take steps to maintain and, if necessary, increase your milk supply.
If there is not enough mother's milk, it is not worth supplementing with mixtures
The Center for Public Health and Medical Prevention continues its series of publications on maternal and child health.
Today's topic is breastfeeding.
Neonatologist, head of the neonatal department of maternity hospital No. 1 Lyudmila Kosteniuk told how breastfeeding affects the development of the child and mother, when it is worth supplementing the child with adaptive mixtures, and whether they can fully replace mother's milk.
How does breastfeeding affect a child's development?
Let's start with the fact that with mother's milk the child receives all the necessary nutrients, and in the first months of life - all immune cells, antibodies. This is protection from the diseases that my mother has had, as well as protection from the vaccines she has been vaccinated with.
It is also important to understand that during breastfeeding, the child does not eat large portions due to the frequency, and subsequently increasing the volume and reducing the number of feedings. Such nutrition is more logical for the development of the child. So, the child eats as much as he needs. On the first day of life with mother's milk, a healthy flora populates in the intestines of the child.
Thanks to this, in the future he will be less susceptible to allergic and gastrointestinal diseases. When a child begins to be fed with an adaptive mixture, such flora is formed in slightly smaller quantities, respectively, the baby may be susceptible to allergic diseases and gastrointestinal diseases.
Are there formulas that have become a complete substitute for mother's milk?
It is clear that there are situations when a mother does not have enough milk or a child cannot consume mother's milk for certain reasons, then the adaptive formula becomes an alternative.
But the fact is that not a single mixture corresponds to mother's milk. It is impossible to make a purely chemical composition of milk - there is no such chemical selection.
It's just that all mixtures are made different - with accents on certain points.
Is it possible to feed the baby with mixtures in parallel with mother's milk? In what cases should this be done?
Mixtures are added when mother's milk is not enough for the child.
If the child does not receive the necessary amount of nutrition, then there may be problems with his development. But there is one point - it is important that the child really has a need for additional nutrition, and not a sucking reflex, which is realized through a bottle with a nipple.
It is best to give the mixture from a glass, jar or spoon. The child must understand that only the breast should be sucked, and everything else is additional nutrition. But if the mother has enough milk volume, then it is wrong to supplement with mixtures.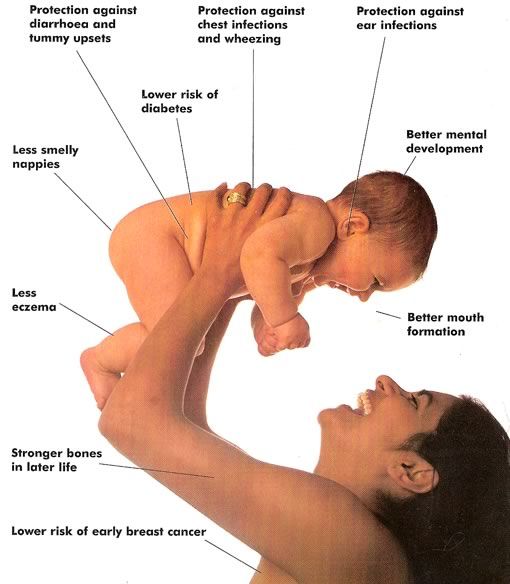
How does breastfeeding affect the mother?
Mom also gets positive emotions from breastfeeding.
When a baby suckles the breast, the mother perceives the baby as a part of herself, one whole. During breastfeeding, the child provokes contraction of the uterus after childbirth: when sucking, a reflex is triggered and the uterus contracts, and this is the physical recovery of the mother after childbirth.
Also during this process, an energy connection is established between mother and child. This connection is formed when the mother is carrying a child, and while feeding, the mother keeps and maintains this connection. In the future, when the child grows and develops, the bond between mother and child remains strong.
Can a baby be allergic to mother's milk?
Allergies can be caused by the foods that mom eats, so you need to control the process of eating. As such, there is no allergic reaction in children of the first year of life.
This is a kind of allergic reaction, the so-called toxic erythema, which can occur in children against the background of malnutrition of the mother.
This is not a pathological reaction: the child reacts to food as if it were the wrong component. Usually the reaction lasts 2-3 days, when the allergic component of the mother goes away. This situation is not dangerous and does not require treatment.
In this way, the child's body signals that he is not yet ready for a certain food that the mother eats. Outwardly, it appears as red spots on the body and is very similar to urticaria. Allergic reactions appear from the second year of life.
Interviewed by A. Pribylova
Read about the "School of Motherhood" in Sevastopol at the link.
alternative ways.. Articles to help mom
H Non-bottle supplementation occurs in mothers who want to continue breastfeeding but are forced to supplement with formula or expressed milk for various reasons, for example:
- Mom needs to leave, and another adult will feed the baby.

- Mom is ill and is taking medications that are incompatible with breastfeeding (breastfeeding).
- It is necessary to give a medicine diluted in milk.
- Mom has a severe cracked nipple and breastfeeding is very painful.
- The baby is not gaining weight, and the pediatrician prescribed supplementary feeding with formula.
- Any other reason why a baby would need to be supplemented from a non-breastfeed.
The article will be useful to mothers who want to return or maintain breastfeeding after the introduction of supplementary feeding.
Why not a bottle
There is no unequivocal recommendation to give non-bottle supplements. But there is a threat that after the bottle the baby will refuse the breast or stop latching on properly.
For some children, it is enough to kiss the nipple once to start acting up at the breast. After all, milk from the breast does not flow as quickly and not as evenly as from a bottle. It does not mean at all that this will happen to you, but there is such a possibility.
It does not mean at all that this will happen to you, but there is such a possibility.
Methods of supplementary feeding according to the degree of closeness to breastfeeding
Consider the pros and cons of the methods known to us, which are recommended by the World Health Organization (WHO) and breastfeeding consultants.
Breast feeding systems
You give your baby a breast and bring a soft catheter to the nipple, through which pumped milk or formula is supplied. At the opposite end of the catheter is a container of milk. It can be a syringe or a bottle, or a glass - which is more convenient for mom. Medela has a ready-to-use breastfeeding system. This option is only suitable for babies who can breastfeed. On the Internet you will find videos on how to build such a system yourself or use a ready-made one. Google it.
Pros
The undoubted advantage of the breastfeeding system is that the baby suckles at the breast. He not only receives milk "from the breast", but also stimulates the mammary glands.
He not only receives milk "from the breast", but also stimulates the mammary glands.
Cons
You have to get used to using it. The container and catheter will have to be washed or changed frequently, interrupt feeding, or prepare milk in advance for supplementary feeding. You will spend some time learning how to secure the catheter to your chest.
Finger feeding
Very similar to the previous version, only instead of the breast, the child sucks your finger, to which the catheter is attached. Instead of a catheter, you can give milk to the corner of your mouth from a syringe without a needle. Drop by drop. It is better to choose a larger finger, usually the middle or index finger, so that the baby opens his mouth wide.
pros
The baby has skin contact while suckling and feels the warmth of your finger. In the case of using a catheter, you can hold the baby in your arms, as with breastfeeding.
Minuses
If you are syringe feeding, some of the milk will spill out at first. Stock up on stock. If a stranger is feeding the child, then it is advisable to use a glove or abandon this method so as not to create an additional burden on the intestines with an unfamiliar microflora.
Cup feeding
WHO recommends this method. You pour milk into a small cup. Even a plastic bottle cap will do. Tilt it so that the milk does not spill out, but stands at the edge. And put this edge on the baby's lower lip. He will begin to stick out his tongue and slowly lap up milk. You gradually tilt the cup so that the milk is always available to him. It is important not to pour milk into the child's mouth, otherwise it will choke.
With this method of feeding, you need to keep the baby as upright as possible.
Pros
The child eats milk at his own pace. He may take a break from lapping, as well as from breast sucking. At this point, it is important to continue to hold the cup on his lip. The kid will continue when he is ready.
He may take a break from lapping, as well as from breast sucking. At this point, it is important to continue to hold the cup on his lip. The kid will continue when he is ready.
Cons
Milk is likely to spill, prepare with a margin.
Spoon feeding
The principle is the same. Instead of a cup, you use a spoon, which you serve with a thin or wide edge - as you like - on the child's lower lip. The difference is that the spoon will have to be refilled more often. Medela has a special feeding spoon. The principle of its application is the same, but it is filled from the attached container with a light touch. Choose what is more convenient.
Syringe feeding
Give milk from a syringe without a needle to the baby's cheek. It is important to give it by the cheek and drop by drop so that the child does not choke. Take a syringe of at least 10 ml. Try different manufacturers. The piston should move as easily and without jerks as possible.