Tube feeding premature babies
Tube feeding | Bliss
Your baby may be fed using tube feeding while on the neonatal unit. Find out why this might be and information about caring for your baby while they are being tube fed.
What is tube feeding?
During tube feeding, breast milk or formula is given through a tube passed into your baby’s nose or mouth to their stomach. Types of tube feeding include the following:
- Nasogastric tube feeding (also called an NG tube) - This is when a baby is fed through a small soft tube, which is placed in the nose and runs down the back of the throat, through the food pipe (oesophagus) and into the stomach.
- Orogastric tube feeding - This is when a baby is fed through a small soft tube, which is placed in the mouth and runs down the back of the throat, through the food pipe (oesophagus) and into the stomach.
Babies who are very premature or sick may need to be fed using parenteral nutrition (PN) at first.
Why does my baby need to be fed using tube feeding?
Tube feeding is often used to feed premature and sick babies as they can be too small and sick to breastfeed or bottle feed at first. Babies born premature or sick have a low supply of energy and nutrients, so it is important that they are able to have small nutritional feeds often, without lowering their energy levels.
In babies born premature, the coordination of sucking, swallowing and breathing needed for effective feeding is usually not fully established until about 32 to 34 weeks’ gestation (although this is different for different babies). Babies born at term and sick may also take longer to co-ordinate feeding. Tube feeding will help your baby receive enough nutrition to grow and develop.
Can I be involved in caring for my baby if they are being tube fed?
Yes, you can. Staff on the neonatal unit will encourage you to be as involved as possible in the care of your baby on the neonatal unit.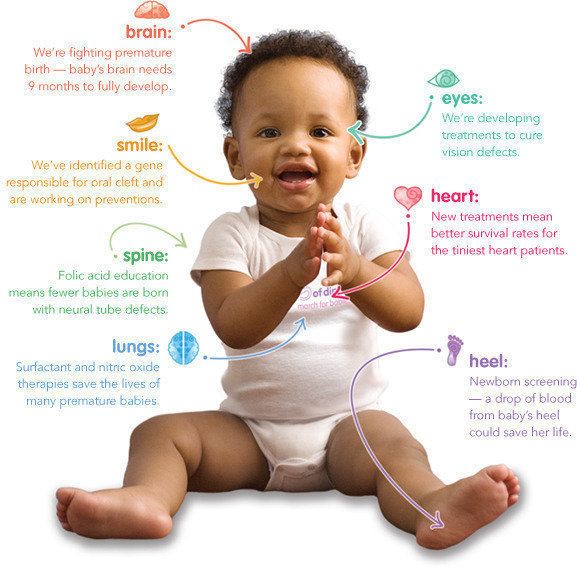 If you feel comfortable doing so, they should show you and your partner how to give tube feeds. Staff on the neonatal unit will explain how tube feeding works and will teach you how to:
If you feel comfortable doing so, they should show you and your partner how to give tube feeds. Staff on the neonatal unit will explain how tube feeding works and will teach you how to:
- Check the tube is in the correct position before feeding
- Prepare the milk and fill the syringe that is connected to the feeding tube
- Position your baby correctly for tube feeds
- Give the milk slowly to support comfortable digestion
- Know what to look for during a feed.
This can feel quite scary at first, but with practice you should gain confidence. You will have the time to give the milk very slowly which helps your baby to digest more comfortably.
If your baby is well enough to come out of the incubator, you and your partner can also practice skin-to-skin contact with your baby while they are tube feeding. Skin-to-skin contact has lots of benefits for you and your baby, and helps parents to feel closer to their baby and more confident in caring for them.
When can my baby stop tube feeding?
In time, you may notice your baby demonstrating feeding cues during a tube feed. For example, they may open and close their mouth, put out their tongue or suck their fingers during a tube feed. This shows that they might be ready to practise breastfeeding or bottle feeding.
If you are planning to breastfeed and your baby is well enough to come out of the incubator, giving them lots of opportunities to be close to the breast may help them to learn to breastfeed. During a tube feed may be a good time to do this. When they are more mature and interested enough, some babies will start licking milk and in time practice sucking. As your baby starts to take more breast and bottle feeds, they will not need as many top-ups of milk from the feeding tube. This will depend on your baby’s energy levels and their ability to coordinate sucking, swallowing and breathing.
Some parents have concerns about their baby changing from tube feeding to breastfeeding, as it is more difficult to measure how much milk their baby is having. Your baby will show signs that they are receiving enough milk, such as feeding cues and wet and dirty nappies. The healthcare team supporting you will monitor your baby’s feeding and will manage any top-ups that might be needed. Talk to a member of staff on your unit if you have any concerns.
Your baby will show signs that they are receiving enough milk, such as feeding cues and wet and dirty nappies. The healthcare team supporting you will monitor your baby’s feeding and will manage any top-ups that might be needed. Talk to a member of staff on your unit if you have any concerns.
What will happen if my baby needs to go home from the neonatal unit with a feeding tube?
If your baby is going home with a feeding tube, a member of unit staff will show you how to feed and care for the tube yourself. It may be you or your community neonatal nurse who will replace the tube when you go home. This will depend on your baby’s needs, your preferences, and the support the unit provides.
Support will always be available if you do not feel comfortable with replacing the tube yourself. If you have any questions or concerns, talk to the unit staff.
Related content
The 9 reasons why preemies are more often tube dependent than infants born at term
11/6/2015
If you’re reading this blog, chances are your child was born prematurely.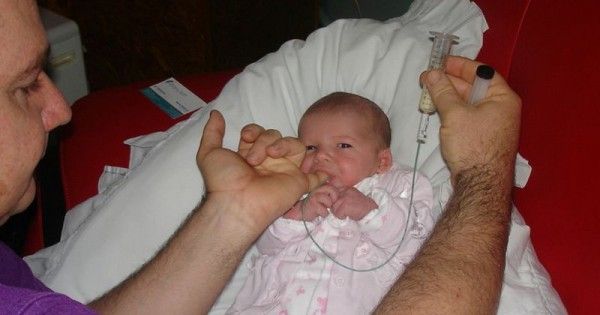 This article specifically deals with preemies that were not only born prematurely, but also continue to receive their nutrition by means of a feeding tube.
This article specifically deals with preemies that were not only born prematurely, but also continue to receive their nutrition by means of a feeding tube.
As a first message I would like to say that it is neither your fault that your child has a feeding tube nor has anything gone wrong in the treatment and taking care of your baby. However, the focus and attention of all the care offered has not been specifically directed at transitioning to oral feeds. We will be talking about why this would be an important step if the medical necessity for the tube has ceased to exist, how this can and should be organized, how you can help your infant catch up with it’s delayed or suppressed eating development and also how it can catch up to its current general developmental level without any medical risk.
When preterm babies should learn to eat without a feeding tube
Any infant born prematurely between the 23rd and 32nd gestational weeks should be discharged home from the neonatal intensive care unit (NICU) or the aftercare unit as an orally eating baby unless major ongoing medical complications require the feeding tube to stay in place for the time being. For preemies whose tube is no longer necessary to be able to successfully transition from tube to oral feeding, parents (under the guidance of their medical team) and the medical team themself will need to encourage oral function already on a non-nutritive level long before the infant is ready to accept any substantial oral feeding. If all goes well the whole transitioning process to full oral feeding should be completed at around the 34th gestational week. At this point the baby will probably weigh around 4.5-5.5 lbs. Latest, the preemie should be eating by the time of the formerly calculated term birthday. Medical studies have clearly shown that there are significant benefits to oral stimulation by finger or pacifier in preterm babies and that it is desirable to achieve oral feeding as soon as possible.
For preemies whose tube is no longer necessary to be able to successfully transition from tube to oral feeding, parents (under the guidance of their medical team) and the medical team themself will need to encourage oral function already on a non-nutritive level long before the infant is ready to accept any substantial oral feeding. If all goes well the whole transitioning process to full oral feeding should be completed at around the 34th gestational week. At this point the baby will probably weigh around 4.5-5.5 lbs. Latest, the preemie should be eating by the time of the formerly calculated term birthday. Medical studies have clearly shown that there are significant benefits to oral stimulation by finger or pacifier in preterm babies and that it is desirable to achieve oral feeding as soon as possible.
Which doctors are capable of releasing preterm babies without a feeding tube
As for instance in all institutions focused around the issues of self-regulation and sensitive individualized care, as is the case in most clinical centers following the guidelines and the recommendations of the NIDCAP® (neonatal individual developmental care assessment program), the ambition is explicitly to not discharge any infants - including preemies - on tube feeds. This goal is realistic and can be met by helping all preemies learn to suck and swallow in a self-regulated and coordinated manner so that they learn how the entire process works. Then, step by step and these children are guided towards being fully self sustaining by mouth and only then will the tube be removed.
This goal is realistic and can be met by helping all preemies learn to suck and swallow in a self-regulated and coordinated manner so that they learn how the entire process works. Then, step by step and these children are guided towards being fully self sustaining by mouth and only then will the tube be removed.
Why releasing children without a feeding tube matters - The negative side effects of tube feeding
The work it takes by parents/doctors to help their child/little patient make this transition is well worth it, as oral fed infants suffer much less from the well known troubling negative side effects of feeding tubes.
In a recent study observing the largest population of tube-fed infants ever documented, the parents of 425 tube-fed infants (with both nasogastric (NG) and Percutaneous endoscopic gastrostomy (PEG) tubes) were asked to document their children’s reactions to their feeding tube. Nearly all of these children had been tube-fed since birth. The study showed that over 56% of these tube-fed children fight with gagging and retching episodes daily and 50% vomit frequently. As expected, depending on which tube the children had, their side effects varied. What’s astonishing though is that both tubes (nasogastric (NG) and percutaneous gastrostomy (PEG) tube) come with significant negative side effects and that no significant correlations could be found between age, sex, underlying medical diagnoses, type of feeding tube, feeding schedules (bolus or continuous), and parental and child’s behavior regarding the feeding situation and duration of tube feeding. This means that these side effects are endemic to the tube and unless the tube is removed, they will remain!
The study showed that over 56% of these tube-fed children fight with gagging and retching episodes daily and 50% vomit frequently. As expected, depending on which tube the children had, their side effects varied. What’s astonishing though is that both tubes (nasogastric (NG) and percutaneous gastrostomy (PEG) tube) come with significant negative side effects and that no significant correlations could be found between age, sex, underlying medical diagnoses, type of feeding tube, feeding schedules (bolus or continuous), and parental and child’s behavior regarding the feeding situation and duration of tube feeding. This means that these side effects are endemic to the tube and unless the tube is removed, they will remain!
This is a serious problem, especially since f.e. frequent vomiting can lead to malnutrition. Recent statistics in this field show that more than 33% of all tube fed children aged 0-12 months are malnourished as defined by the criteria of the World Health Organization (WHO).
The fact of avoiding these typical tube related symptoms by early tube weaning in itself also sets lots of developmental energy free which the infant will then be able to invest into its general and motor development.
Now, what are some of the reasons why transitioning to oral feeds can be difficult or seem nearly impossible for your baby?
As a medical doctor, I’ve spent more than 30 years of my professional career working in and with NICU’s around the world. Examining and observing thousands of pre-term babies and their first attempts at eating, these are some of the most common challenges I’ve seen them struggle with:
- The development of the intrauterine sucking-swallowing coordination process is interrupted by the premature birth
- The lungs are immature and not yet equipped to breathe without mechanical and/or medical support
- The ability to thermoregulate needs to be taken care of first, so there’s no space to take care of feeding
- The dominance of stabilizing safe breathing patterns and other airway problems interfere with the emerging swallow coordination
- The premature born infant might be too sick and fragile to manage breathing and eating challenges at the same time
- Repeated aversive intraoral actions (intubation, repeated suctions etc.
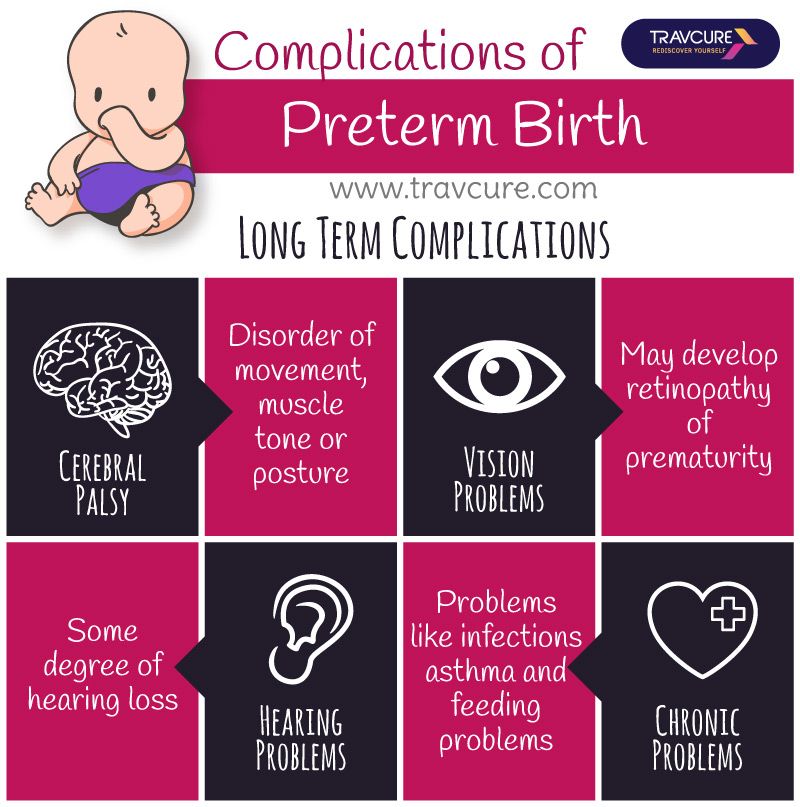 ) can be traumatic for the baby
) can be traumatic for the baby - Increased physiological reflux due to very low muscular tone can lead to an oral aversion
- Additional medical complications like sepsis or surgeries make tube weaning impossible
- Lacking aftercare structures in the hospital, no tube management-maintenance team, no exit strategy
Guidelines for what to do with a tube-fed preemie
Given that all of these challenges exist and are present in one child or another, it is very hard to give general recommendations. However, there are some guidelines which make sense for almost any situation where a preemie baby has been born and is fed with a feeding tube.
Elements to follow:
- If your baby could not be discharged from the NICU as an orally drinking infant, please ask your team for the reasons and ask for clearly defined nutritional goals to be met before embarking on a tube weaning trial at home together with the medical team of your choice.

- As shown above, enteral nutrition support does not guarantee sufficient growth, so inquire with your medical team whether malnourishment is present and if the tube has been present for some months, how they plan on leading your child to a healthy state
- If your child is not malnourished, ask your medical team why the feeding tube is still in and what elements are needed for it to be removed. It is the medical teams’ responsibility to provide you with a clear exit strategy unless underlying medical conditions make the feeding tube absolutely necessary (f.e. if the child has no swallow reflex).
- If you want to tube wean your child, a developmentally adjusted and highly individualized approach is necessary for each child, please ask your nurse and medical staff how they feel about the issue of discontinuation of tube feeds and look for the most specialized place you can find. Tube weaning is not an easy operation that any hospital can do and you really want to make sure you’re getting the best support you can.

- Please don’t ever try to force feed your child before, during or after tube weaning (even when someone tells you to), the literature has clearly found that it is harmful at all times.
Find out if your medical team specifically wishes the tube feeding to be continued or gives your baby permission to transition to oral feeding. If you receive permission, start thinking about which medical organization you want to do the tube weaning with. Please, from the bottom of my heart, don’t try this alone on your own, it is potentially life-threatening for your child if you don’t know what you’re doing.
Since you’re not the first to go through this, I’ve asked a mother of a formerly tube-fed preemie to share with me how she went about choosing a medical partner for tube weaning her preemie. You can find her guide here.
Having helped wean hundreds of preemies from their feeding tube with my multi-disciplinary team at NoTube. com, these are some of the lessons I’ve learnt. Preemies are fighters and extremely tough. They’ve gone through so much to get to where they are and they will continue fighting! When challenged to learn how to eat orally by an experienced medical team advising parents what to do, preemies are well able to transit to oral feeding from and be fully orally sustaining by the 34th week or, in some cases, slightly earlier. During the tube weaning phase, a period of 2-4 weeks of slowed down weight development is normal and must be accepted. But it’s important to know that the task of tube weaning in prematurely born infants can only be achieved by intensive cooperation and trust between the nurses, doctors and parents!
com, these are some of the lessons I’ve learnt. Preemies are fighters and extremely tough. They’ve gone through so much to get to where they are and they will continue fighting! When challenged to learn how to eat orally by an experienced medical team advising parents what to do, preemies are well able to transit to oral feeding from and be fully orally sustaining by the 34th week or, in some cases, slightly earlier. During the tube weaning phase, a period of 2-4 weeks of slowed down weight development is normal and must be accepted. But it’s important to know that the task of tube weaning in prematurely born infants can only be achieved by intensive cooperation and trust between the nurses, doctors and parents!
I truly hope this article was helpful to you and would be glad to answer any comments here or to get in touch with me directly, just send me a message here!
Written by Marguerite Dunitz-Scheer, MD of notube.
Features of feeding premature babies
Successful nursing of premature newborns, in addition to therapeutic measures, largely depends on the creation of optimal external conditions and adequate nutrition. According to the modern theory of nutrition programming , the quantity and quality of nutrients supplied during the prenatal period and the first months of a child's life determines the nature of metabolism and, as a result, affects a person's health throughout later life. nine0003
According to the modern theory of nutrition programming , the quantity and quality of nutrients supplied during the prenatal period and the first months of a child's life determines the nature of metabolism and, as a result, affects a person's health throughout later life. nine0003
Proper and nutritious nutrition in the early stages of life affects the overall development of the child, and also contributes in direct proportion to reducing the development of chronic diseases in adulthood (such as diabetes and arterial hypertension).
The purpose of enteral nutrition is to provide the body with the nutrients it needs to grow and develop.
Providing a premature newborn with an optimal amount of nutrients is quite difficult, given the morphofunctional immaturity of the digestive system and the lability of metabolic processes. The relatively high need of premature infants for nutrients is in conflict with the limited ability to assimilate them. nine0003
nine0003
Feeding methods for premature babies are determined by the severity of their condition and depend on the body weight and gestational age of the baby at birth.
Successful feeding of a newborn is possible when sucking, swallowing and breathing become well coordinated.
The swallowing reflex is well developed already by 28-30 weeks of gestational age, but it is very quickly depleted. Fully matures by 34 weeks of gestation. When does sucking and swallowing coordinate? Already at 28 weeks of gestational age, all the components of sucking and swallowing take place, but the child is not yet able to coordinate them. Partially, this occurs by 32-34 weeks of gestation. Coordination of sucking and swallowing fully matures around 36-38 weeks of gestational age. From 37 to 38 weeks of gestational age, newborns are able to coordinate sucking, swallowing, and breathing without difficulty. nine0003
When feeding premature babies, you should pay attention to four points: when, what, how much, what method to feed.
The first feeding should be started as soon as it becomes clinically possible. Earlier introduction of breast milk helps to reduce the frequency of infections, maturation of the gastrointestinal tract, immune functions, and improved calcium metabolism.
Newborns weighing more than 2000 g and gestational age more than 33 weeks, who do not have other diseases, can be attached to the mother's breast as early as the first day of life. In this case, you should carefully monitor the appearance of signs of fatigue (cyanosis of the nasolabial triangle, shortness of breath, etc.). Their appearance is an indication for the transition to feeding expressed breast milk from a bottle. Efforts should be aimed at preserving breast milk as much as possible, taking into account the special biological value of mother's native milk for an immature child and the important role of mother-child contact during feeding. For premature babies, free feeding is unacceptable due to their inability to regulate the amount of sucked milk and the high incidence of perinatal pathology. nine0003
nine0003
Babies born before 33 weeks' gestation are usually tube-fed to avoid the risk of aspiration resulting from a lack of coordination between sucking and swallowing. With a non-severe condition of the child and a body weight approaching 2000 g, a trial feeding from a bottle can be carried out, with unsatisfactory sucking activity, tube feeding is prescribed in full or in part. In order to maintain and maintain lactation in the mother, regular expression of breast milk is necessary. nine0003
Enteral feeding of very preterm infants (weighing less than 1500 g and less than 30 weeks' gestation) is carried out through a tube.
The caloric method is used to calculate the required amount of feeding for premature babies. The calorie content of the diet of a prematurely born child increases gradually and daily.
Caution and Graduality Feeding Guidelines for Premature Babies Less Than 33 Weeks Gestational Age Less Than 2000g
For a premature baby, the best bioavailability is the milk of a woman who has given birth prematurely, then formulas for premature babies, and then the milk of a woman who has given birth at term.
Women's milk after preterm birth has a special composition, it contains more protein, less lactose with the same total level of carbohydrates. In addition, it has a higher content of a number of protective factors, in particular lysozyme and secretory IgA. Despite the special composition, the milk of women who gave birth prematurely can satisfy the nutritional needs of only premature babies with a relatively large body weight - more than 1800-2000 g. Premature babies with a lower body weight are deficient in a number of nutrients. For them, breast milk must be further enriched with protein, calcium, phosphorus, iron, and vitamins. This can be achieved by replacing part of the required amount of breast milk with a specialized formula for premature babies or by adding breast milk enhancers. When enrichers (enhancers) are used, the main advantages of breastfeeding are preserved and at the same time the high nutritional requirements of the premature baby are ensured. With artificial feeding, specialized mixtures intended for feeding premature babies should be used. Cancellation of specialized mixtures for premature babies and their transfer to standard milk formulas is carried out gradually. The duration of use depends on the gestational age of the child. Premature babies with a gestational age of more than 31-33 weeks should receive specialized formulas until they reach a body weight of 2500-3000 g, after which they are completely transferred to standard adapted milk formulas. Babies with lower gestational age need longer-term use of specialized products (at least until they reach 40 weeks post-conceptual age). nine0003
Cancellation of specialized mixtures for premature babies and their transfer to standard milk formulas is carried out gradually. The duration of use depends on the gestational age of the child. Premature babies with a gestational age of more than 31-33 weeks should receive specialized formulas until they reach a body weight of 2500-3000 g, after which they are completely transferred to standard adapted milk formulas. Babies with lower gestational age need longer-term use of specialized products (at least until they reach 40 weeks post-conceptual age). nine0003
Such a careful approach to the nutrition of preterm infants is primarily due to the fact that achieving the required height, weight and especially head circumference is important for psychomotor development.
the pediatric department for premature babies of the Maternity Hospital No. 2 Marochkina E.M.
Continuous milk feeding via nasogastric tube versus intermittent bolus milk feeding in preterm infants weighing less than 1500 g
Survey Question
Is continuous tube feeding through the nose or mouth better than tube feeding every two to three hours in very low birth weight preterm infants?
Relevance
Premature babies born weighing less than 1500 grams are unable to coordinate sucking, swallowing and breathing. Feeding through the gastrointestinal tract (enteral nutrition) promotes the development of the digestive system and the growth of the child. Therefore, in addition to feeding through an intravenous catheter (parenteral nutrition), premature babies can be fed milk through a tube inserted through the nose into the stomach (nasogastric feeding) or through the mouth into the stomach (orogastric feeding). Typically, a predetermined amount of milk is given over 10-20 minutes every two to three hours (intermittent bolus feeding). Some doctors prefer to feed premature babies continuously. Each feeding method has potentially beneficial effects, but can also have harmful effects. nine0003
Feeding through the gastrointestinal tract (enteral nutrition) promotes the development of the digestive system and the growth of the child. Therefore, in addition to feeding through an intravenous catheter (parenteral nutrition), premature babies can be fed milk through a tube inserted through the nose into the stomach (nasogastric feeding) or through the mouth into the stomach (orogastric feeding). Typically, a predetermined amount of milk is given over 10-20 minutes every two to three hours (intermittent bolus feeding). Some doctors prefer to feed premature babies continuously. Each feeding method has potentially beneficial effects, but can also have harmful effects. nine0003
Study profile
We included nine studies with 919 infants. Another study is pending classification. Seven of the nine included studies reported data on infants with a maximum weight between 1000 and 1400 grams. Two of the nine studies included infants weighing up to 1500 grams. The search is current as of July 17, 2020.
The search is current as of July 17, 2020.
Main results
Infants receiving continuous feeding may achieve complete enteral nutrition slightly later than infants receiving intermittent feeding. Total enteral nutrition is defined as the intake of a given volume of breast milk or formula by the infant in the required manner. This promotes the development of the gastrointestinal tract, reduces the risk of infection from intravenous catheters used to provide parenteral nutrition, and may shorten hospital stays. nine0003
It is not known whether there is a difference between continuous and intermittent feeding in terms of the number of days needed to regain birth weight, days of feeding interruption, and rate of weight gain.
Continuous feeding may result in little or no difference in rate of increase in body length or head circumference compared to intermittent feeding.
It is not known whether continuous feeding affects the risk of developing necrotizing enterocolitis (a common and serious bowel disease in preterm infants) compared with intermittent feeding.