Ways to feed baby
How will you feed your baby?
How will you feed your baby? | Pregnancy Birth and Baby beginning of content4-minute read
Listen
You’ll have lots to think about and want answers to many questions when you’re pregnant — including how to feed your baby. You can choose from several ways to feed them, depending on what best suits you both.
What are your feeding options?
Babies need milk that contains certain qualities to grow and thrive. They can’t digest any other form of nutrition until they’re around 6 months old. It’s recommended that you feed your baby only breastmilk — called exclusive breastfeeding — for the first 6 months. After that, you can introduce solid foods while you continue breastfeeding.
If you don’t plan to breastfeed, you can give your baby expressed breast milk (EBM), infant formula or a combination of EBM and formula, which is known as mixed feeding. Babies who are premature, unwell or receive care in special care nurseries can also be fed human donor milk.
When is the right time to consider how I will feed my baby?
There is no right time to decide how you will feed your baby, although you may have a clear preference before your baby is born.
You may or may not want to breastfeed. Reasons for not breastfeeding include because you take medication, have breast cancer or have had a negative experience.
What are the benefits of breastfeeding?
For your baby
Any amount of breastfeeding is beneficial, even if you choose to provide breastmilk alongside formula.
Breastmilk helps:
- improved immunity to many infectious diseases, due to the antibodies in breast milk
- support a healthy weight and prevention of obesity
- reduce the risk of sudden unexplained death in infancy (SUDI)
For you
Breastmilk helps:
- your uterus contract and return to its pre-pregnant size
- prevent a range of health issues such as heart disease, breast and ovarian cancer, and type 2 diabetes
What if I can't decide if I want to breastfeed or not?
You can undertake a few measures to help you decide if you want to breastfeed. Ask for advice from people whose opinion you respect. You can also research and fact check using quality, evidence-based sources. Try to keep an open mind.
Ask for advice from people whose opinion you respect. You can also research and fact check using quality, evidence-based sources. Try to keep an open mind.
Lots of women who try breastfeeding find that they enjoy it.
Why wouldn't breastfeeding be right for me and my baby?
Some women simply feel breastfeeding is not something that they want to do. It’s also not uncommon for women to try breastfeeding before they decide how long they want to continue.
Breastfeeding can also be challenging when a mother and her baby are separated, such as when a mother returns to work. To help manage this, you can breastfeed your baby when you are with them and provide EBM or formula when you are apart. Your partner or your baby’s other parent can also feed them EBM from a bottle. This is a good way for them to connect with each other, too.
Babies who are premature, unwell at birth or with developmental delays can struggle to learn how to suck effectively. Some women are advised to express their colostrum before giving birth, so it can be frozen and offered to the baby after birth.
Further, sometimes breastfeeding isn’t an option when a mother is unwell or has a medical condition.
Formula — what do I need to know?
Any formula which can be bought in Australia will meet a baby’s nutritional needs. It’s important to read the product information and prepare formula exactly as the manufacturer recommends.
Most Australian maternity hospitals participate in the Baby-Friendly Hospital Initiative (BFHI). If you plan to feed your baby formula from birth, you may need to take your own bottles, formula and teats to the hospital.
Top tips for deciding how to feed your baby
- Speak with your maternity care provider about what's right for you. Try not to make any firm decisions until after your baby is born.
- Understand that breastfeeding is a skill that every mother and baby can learn, and it can take time to build confidence and to get to know each other.
- Only you know what’s right for you and your baby. If you give your baby the nutrition they need, you don’t need to justify which option you choose.
- Be patient with yourself and your baby as you both learn what's involved in feeding.
- Remember, what’s important is that your baby is content and gets the nutrition they need to grow and thrive.
Sources:
Red Nose (Breastfeeding), Australian Breastfeeding Association (Antenatal expression of colostrum), Australian Breastfeeding Association (Confused about introducing solids?), Pregnancy, Birth and Baby (Donor breast milk and milk banks), World Health Organization (Nutrition), Department of Health (Marketing in Australia of Infant Formulas: Manufacturers and Importers Agreement)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: September 2020
Back To Top
Related pages
- Feeding your baby with formula
- Diet and medication while breastfeeding
- Breastfeeding your baby
Need more information?
Breastfeeding and smoking | Australian Breastfeeding Association
Research has found that smokers are less likely to begin or persist with breastfeeding compared with non-smokers. However, this is not thought to be due to an inability to breastfeed, but rather to do with the background of a mother who smokes.1,2
However, this is not thought to be due to an inability to breastfeed, but rather to do with the background of a mother who smokes.1,2
Read more on Australian Breastfeeding Association website
Newborn essentials
Here is a newborn's essentials checklist including vaccinations and immunisations, health checks, nappy changing and breastfeeding and bottle feeding.
Read more on Pregnancy, Birth & Baby website
Feeding your baby
Whether you have already had your baby or are currently pregnant planning on what is to come, learn about breastfeeding, bottle feeding and introducing solids.
Read more on Pregnancy, Birth & Baby website
Breastmilk & breastfeeding: benefits | Raising Children Network
Breastmilk – designed by nature for human babies. Breastmilk and breastfeeding have many health and practical benefits for mothers and babies. Read more.
Breastmilk and breastfeeding have many health and practical benefits for mothers and babies. Read more.
Read more on raisingchildren.net.au website
Pregnancy & Breastfeeding - Allergy & Anaphylaxis Australia
If you have a family history of allergic conditions, it makes sense to try and reduce the risk of your children developing allergic diseases. There are some simple steps you can take: Don’t smoke during pregnancy; Breast feed your baby for at least six months, if possible; Delay the introduction of infant formula or solid foods until the child is 4-6 months of age; Introduce foods one at a time in small portions, waiting 2-3 days before introducing another new food.&
Read more on Allergy and Anaphylaxis Australia website
Mixed feeding | Australian Breastfeeding Association
Regardless of whether a mother exclusively breastfeeds, exclusively uses formula or does a combination (mixed feeding), she has done her very best and has made decisions that were right at the time, based on the support and information she had available to her.
Read more on Australian Breastfeeding Association website
Feeding multiple babies
Feeding multiple babies, such as triplets or more, can be challenging at first, but even breastfeeding is possible with some expert help.
Read more on Pregnancy, Birth & Baby website
When can babies drink water?
You may wonder when it is safe to start giving your baby water. Whether you are breastfeeding or formula feeding, learn how and at what age to get started.
Read more on Pregnancy, Birth & Baby website
How to wean off formula supplements | Australian Breastfeeding Association
Seek guidance from your child health nurse and/or lactation consultant
Read more on Australian Breastfeeding Association website
Guide to feeding your baby formula / breastmilk substitutes | Australian Breastfeeding Association
It is not always easy to find information about how to prepare formula / breastmilk substitutes safely and correctly— information that is unbiased, accurate and free from commercial interests.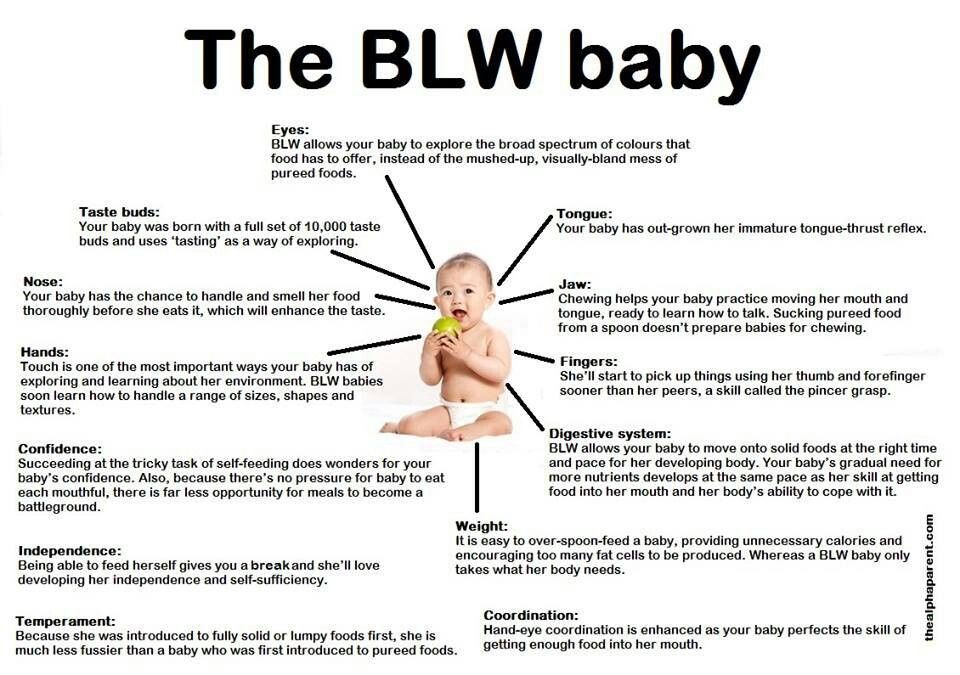 Below are some links to documents which provide you with information which is unbiased, accurate and free from commercial interests about how to minimise the risks to your baby when you sterilise equipment and prepare and give formula.
Below are some links to documents which provide you with information which is unbiased, accurate and free from commercial interests about how to minimise the risks to your baby when you sterilise equipment and prepare and give formula.
Read more on Australian Breastfeeding Association website
Disclaimer
Pregnancy, Birth and Baby is not responsible for the content and advertising on the external website you are now entering.
OKNeed further advice or guidance from our maternal child health nurses?
1800 882 436
Video call
- Contact us
- About us
- A-Z topics
- Symptom Checker
- Service Finder
- Linking to us
- Information partners
- Terms of use
- Privacy
Pregnancy, Birth and Baby is funded by the Australian Government and operated by Healthdirect Australia.
Pregnancy, Birth and Baby is provided on behalf of the Department of Health
Pregnancy, Birth and Baby’s information and advice are developed and managed within a rigorous clinical governance framework. This website is certified by the Health On The Net (HON) foundation, the standard for trustworthy health information.
This site is protected by reCAPTCHA and the Google Privacy Policy and Terms of Service apply.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Baby-Led Weaning is a New Way of Feeding Your Baby - Learn More About it
Every parent remembers when they first introduced their baby to solid foods. This momentous occasion of spoon-feeding them pureed food is considered a major milestone for babies and their parents.
Today however, more and more parents are opting to skip the applesauce and mashed sweet potatoes and instead are adopting a new feeding technique called “baby-led weaning” ( or BLW) for their babies. This alternative approach to feeding, first introduced in the UK a decade ago, involves introducing solid chunks of foods much earlier on by placing them on the baby’s high chair and letting them grasp the food and feed themselves directly. As the name implies, feeding time is led by the baby as they determine the pace and the amount of food they consume; basically, baby-led weaning puts the baby in charge.
This alternative approach to feeding, first introduced in the UK a decade ago, involves introducing solid chunks of foods much earlier on by placing them on the baby’s high chair and letting them grasp the food and feed themselves directly. As the name implies, feeding time is led by the baby as they determine the pace and the amount of food they consume; basically, baby-led weaning puts the baby in charge.
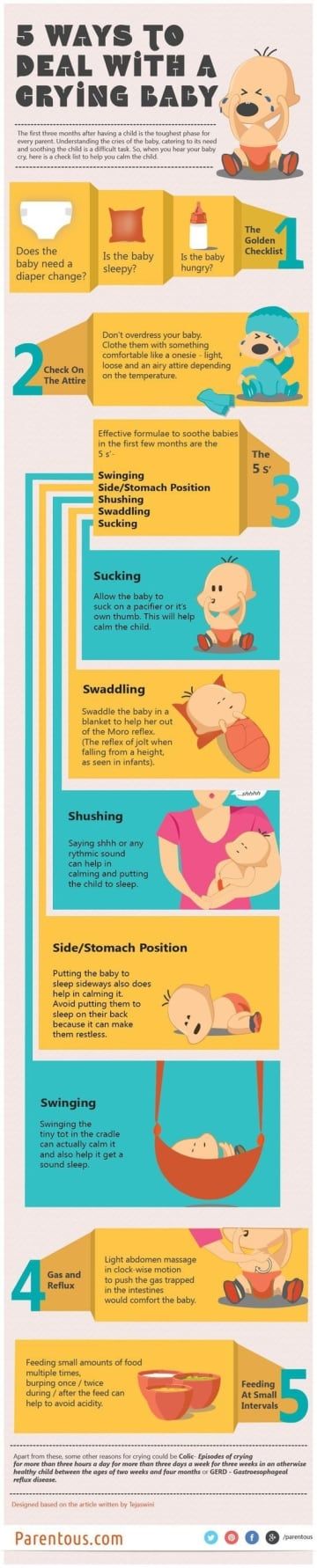
While children all develop at different paces, advocates of baby-led weaning agree that this method of eating shouldn’t be introduced until the baby is ready. Cues to begin BLW include making sure that your baby can sit up straight unassisted, have good neck strength and be able move food to the back of their mouth with up and down jaw movements. Most babies develop these skills by the sixth month, but some babies may not fully develop them until they are nine months old.
Proponents of BLW believe that it holds many benefits, including enhancing baby’s hand-eye coordination and other fine motor skills, including using their thumb and index finger to grasp their food. They also feel that it will produce healthier eaters than spoon-fed babies because BLW eaters get to choose how much they eat as opposed to traditional feeding methods, which sometimes results in force feeding. Other advantages that BLW supporters claim to be true is that it creates a more enjoyable feeding experience for babies and less stress on their parents.
They also feel that it will produce healthier eaters than spoon-fed babies because BLW eaters get to choose how much they eat as opposed to traditional feeding methods, which sometimes results in force feeding. Other advantages that BLW supporters claim to be true is that it creates a more enjoyable feeding experience for babies and less stress on their parents.
Detractors of baby-led weaning feeders point out that these babies are generally underweight as compared to spoon-fed babies because they simply do not ingest that much when they are first introduced to this way of eating due to difficulties grabbing food. BLW babies also tend to be iron-deficient because they aren’t consuming the iron-fortified cereals that spoon–fed babies typically eat. Lastly, a big concern for many parents is the increased choking hazards associated with BLW, and while the American Academy of Pediatrics doesn’t have opinion of BLW, they do state that babies are ready for solid food once they are ready to sit up on their own and bring their hand to their mouth.
If you are considering baby led weaning for your child, here are a few tips:
- Continue breast feeding and / or formula feeding as this will continue to be your baby’s biggest source of nutrition until they are 12 months old.
- Begin BLW feedings with softer foods, such as ripe fruits, cooked egg yolks, and shredded meats, poultry and fish.
- Avoid foods that can pose as choking hazards, such as nuts, grapes, popcorn, or foods cut into coin shapes, like hot dogs.
- Do not leave your child unattended during BLW feeding times. Continue to supervise and socialize with them while they eat and to have them eat when the rest of the family does.
- Don’t panic if your baby gags as it is a safe a natural reflex. Instead of overreacting, prepare for a choking event by familiarizing yourself with the infant-specific Heimlich maneuver.
- Introduce new foods one at a time to pinpoint potential food allergies. A recommended length of time is three to four days between foods.
- The goal of BLW is to let your baby explore eating at their own pace. This may include the smashing, smearing, or dropping of food, so prepare for a mess.
Before you decide to adopt BLW to your child, it is a good idea to discuss with your child’s pediatrician as it may not be a good idea for all babies, especially those babies with known developmental delays or neurological issues.
To make an appointment with a pediatrician at Flushing Hospital’s Ambulatory Care Center, please call 718-670-5486.
All content of this newsletter is intended for general information purposes only and is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. Please consult a medical professional before adopting any of the suggestions on this page. You must never disregard professional medical advice or delay seeking medical treatment based upon any content of this newsletter. PROMPTLY CONSULT YOUR PHYSICIAN OR CALL 911 IF YOU BELIEVE YOU HAVE A MEDICAL EMERGENCY.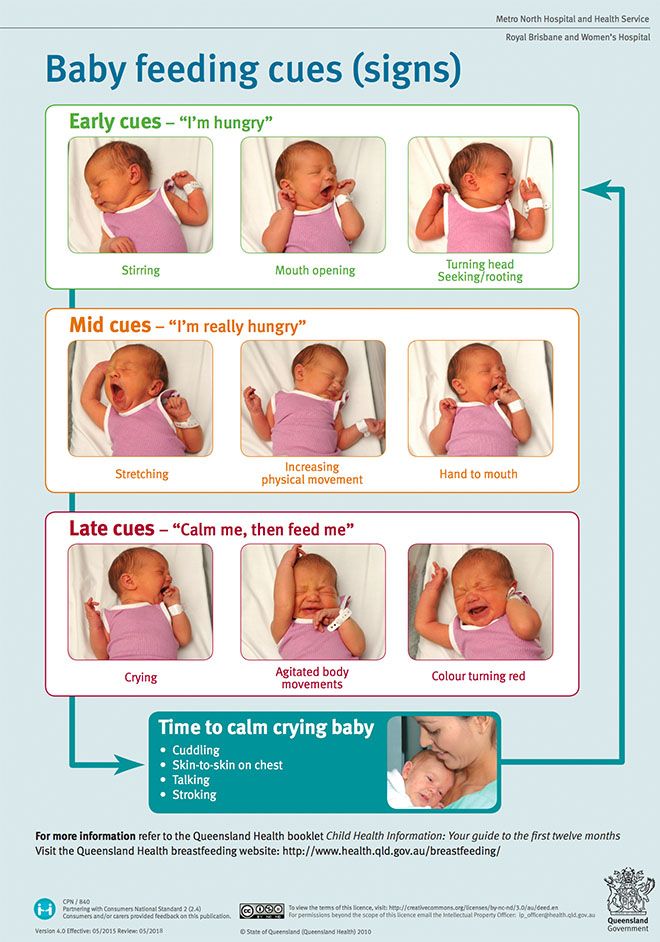
Various breastfeeding positions
Try different breastfeeding positions to find the one that works best for you and your baby. You can see the options in our selection of photos
Share this information
There is no right or wrong way to hold the baby while
feeding, and mom and baby are sure to find their favorite position.
It is important that both you and your child feel comfortable. 1.2 It's good to learn a few different breastfeeding positions and techniques because life's circumstances often require us to be flexible, especially as your baby gets older and you start to leave the house more often.
Whatever position you choose to breastfeed your baby, remember a few simple rules.
- Prepare everything you need before feeding, including drinks, food, mobile phone, TV remote control, book or magazine. And do not forget to go to the toilet - the feeding process can take a long time!
- Make sure your baby is comfortable.
 Whichever position you choose, it's important to keep your baby strong, level, and provide good support for their head, neck, and spine.
Whichever position you choose, it's important to keep your baby strong, level, and provide good support for their head, neck, and spine. - You should also be comfortable. Don't stress. If necessary, use pillows of different sizes or rolls of towels to support your back or arms.
- Make sure your baby is latching on correctly. Proper grip is the key to comfort when breastfeeding.
- If your baby does not latch on well or you experience pain while feeding, contact a lactation consultant for help. The specialist will also be able to show you how to hold your baby more comfortably.
1. Relaxed feeding or reclining position
The relaxed feeding position, also known as biological feeding, 1 is often the first position for most mothers. If, immediately after birth, the baby is placed on the mother’s chest or stomach, normally, he instinctively reaches for the breast and tries to grab the nipple. This phenomenon is known as the breast seeking reflex. Skin-to-skin contact stimulates the infant's feeding instinct, and gravity helps him to latch onto the breast and maintain balance.
Skin-to-skin contact stimulates the infant's feeding instinct, and gravity helps him to latch onto the breast and maintain balance.
But it's not just newborns that can be fed in the reclining position - this position is great for babies of all ages. It can be especially helpful if your baby does not latch well in other positions or does not like to be touched during feeding, and also if you have too much milk flow or too large breasts. Isabelle, a mother from the UK, shares her experience: “I had large breasts, and the baby was born small - 2.7 kg, so it was not easy to find a comfortable position at first. After a few weeks, it became clear that there was no “correct” posture for me. As a result, I most often fed lying down, putting the baby on my chest. ”
It is more convenient to feed not lying flat on your back, but half-sitting, leaning on pillows. So you will have a back support and you will be able to watch the baby during feeding.
2. Cradle position
This is the classic
first thought of breastfeeding. Mom sits straight
Mom sits straight
, and the baby lies on her side on her arm, pressing his stomach against her stomach. 3 Although this is a very popular position, it is not always easy to master with newborns because it gives the baby less support. Try putting a pillow under your back, and put a special breastfeeding pillow on your knees and lean on it with your hands. So you can more reliably support the child, without overstraining your back and shoulders. Just make sure that the baby does not lie too high on the pillow for feeding. The breast should remain at a natural level so that the baby can grab it without effort, otherwise sore nipples cannot be avoided.
“I breastfed in the cradle position because it suited me perfectly! It was comfortable and I loved just sitting and looking at my little one,” recalls Rachel, a mother of two from Italy.
3. Cross Cradle
This breastfeeding position looks almost the same as Cradle, but the baby is on the other arm. 3 This gives your baby support around the neck and shoulders so he can tilt his head to latch on. This position is great for breastfeeding newborns and small babies, as well as for babies who do not latch well. Since the baby lies completely on the other hand, it becomes easier to control his position and you can adjust the chest with your free hand.
3 This gives your baby support around the neck and shoulders so he can tilt his head to latch on. This position is great for breastfeeding newborns and small babies, as well as for babies who do not latch well. Since the baby lies completely on the other hand, it becomes easier to control his position and you can adjust the chest with your free hand.
Julie, a UK mother of two, finds this position very practical: “I usually breastfeed my youngest in the cross cradle position. So I have a free second hand, and I can take care of an older baby at the same time. ”
Do not hold the baby's head at first, otherwise you may inadvertently press his chin against his chest. Because of this, the child will not be able to take the breast deeply, because the nipple will rest against the base of the tongue, and not against the palate, which will lead to inflammation of the nipples. As the child grows, this position becomes more comfortable, and he can rest his head on your palm (as shown in the photo above).
4. Underarm breastfeeding
In this position, also known as the “ball grip”, the mother sits with the baby lying along her arm at the side, legs towards the back of the chair (or any other seat). 3 Another comfortable position for newborn breastfeeding, you can give your baby good support, full control of his position and a good view of his face. And the baby feels safe in close contact with the mother's body. This position is especially good for those who have had a caesarean section or a premature birth, as well as mothers of twins and women with large breasts.
“When I breastfed my first daughter, I had very large K-sized breasts—twice the size of her head,” recalls Amy, an Australian mother of two. - I put rolls of towels under each breast, because they were very heavy, and fed my daughter in a pose from under the arm, but only sitting straighter so as not to crush her. This position was also convenient because I had a caesarean section and could not put the baby on my stomach. ”
”
5. Side-lying position
The side-lying position is ideal for a relaxed
nighttime feeding in bed or on the couch. If you had a
caesarean section or ruptures during childbirth, this position may be more comfortable than sitting down. 3 In this position, mother and baby lie side by side, tummy to tummy.
“It was difficult for me to sit during endless night feedings, firstly because of the caesarean section, and secondly because of lack of sleep,” recalls Francesca, a mother from the UK. “And then I discovered that you can feed your baby lying on your side and rest at the same time.”
“Because of the short tongue frenulum, Maisie could only properly latch on to her breasts while lying on her side. The lactation consultant showed me how it's done. In this position, the flow of milk was optimal for my daughter, and it was easier for her to keep the nipple in her mouth. As she got older, she became much better at grabbing her breasts in normal positions,” says Sarah, mother of two from Australia.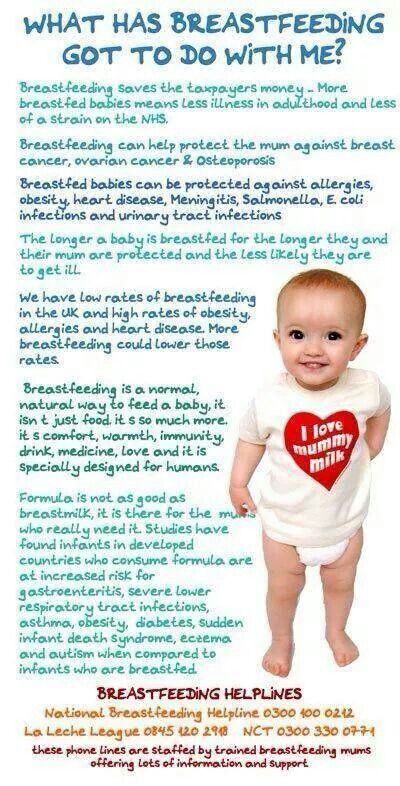
6. Relaxed breastfeeding after caesarean section
If you can't find a comfortable position for breastfeeding after caesarean section, 3 try holding the baby on your shoulder in a reclining position – this does not stress the postoperative suture and allows you to breastfeed your baby comfortably. You can also try side feeding.
7. Sitting upright breastfeeding or “koala pose”
When breastfeeding in an upright position or “koala pose”, the baby sits with a straight back and a raised head on the mother's hip. 4 This position can be tried even with a newborn if it is well supported, but it is especially convenient for feeding a grown child who can already sit up by himself. The upright sitting position, or “koala pose,” is great for toddlers who suffer from reflux or ear infections and feel better sitting. In addition, this pose may be suitable for children with a shortened frenulum of the tongue or reduced muscle tone.
“When my daughter got a little older, I would often feed her in an upright position, which was more comfortable for both of us, and I could still hold her close,” recalls Peggy, a mother from Switzerland. “Besides, it was possible to discreetly breastfeed her in public places.”
“Besides, it was possible to discreetly breastfeed her in public places.”
8. Overhanging position
In this position, the baby lies on his back, and the mother bends over him
on all fours so that the nipple falls directly into his mouth. 4 Some moms say this breastfeeding position is good to use occasionally for mastitis, when touching the breasts is especially unpleasant. Some say that this breastfeeding position helps with blockage of the milk ducts, although there is no scientific evidence for this yet. You can also feed in the “overhanging” position while sitting, kneeling over the baby on a bed or sofa, as well as reclining on your stomach with support on your elbows. Pillows of various sizes that you can lean on will help you avoid back and shoulder strain.
“I have breastfed several times in the 'overhang' position for clogged milk ducts when no other means of dissolving the blockage worked. And this pose seems to have helped. I think it's because of gravity, and also because the breasts were at a completely different angle than with normal feeding, and my daughter sucked her differently, ”says Ellie, a mother of two from the UK.
Feeding in the "overhanging" position is unlikely to be practiced regularly, but in some cases this position may be useful.
“I used to breastfeed in the overhang position when my baby was having trouble latch-on,” says Lorna, mother of two in the UK. - This, of course, is not the most convenient way, but then I was ready for anything, if only he could capture the chest. We succeeded and have been breastfeeding for eight months now!”
9. Breastfeeding in a sling or in a sling
Breastfeeding in a sling takes some practice, but it can be used to go out, look after older children, or even do a little household chores.
The sling is also useful if the baby does not like to lie down or is often attached to the breast. Lindsey, a mother of two in the US, notes: “I used the carrier frequently for both of my children. When we were out of the house, I tied the sarong around my neck and covered the carrier with it. Under such a cape, the baby can eat as much as he wants until he falls asleep.
This breastfeeding position is best when the baby is already good at breastfeeding and can hold his head up by himself. Any slings are suitable for breastfeeding, including elastic and rings, as well as carrying bags. Whichever option you choose, the main thing is that you can always see the face of the child, and his chin does not rest against his chest.
10. Double hand-held breastfeeding
Double hand-held breastfeeding (or “double-ball grab”) is great for mothers of twins—you can breastfeed both at the same time and keep your arms relatively free. 4 When feeding in this position, it is advisable to use a special pillow for breastfeeding twins, especially at first. It will provide extra support and help keep both babies in the correct position, as well as reduce the burden on the abdomen if you had a caesarean section. In addition, the hands are freer, and if necessary, you can deal with one child without interfering with the second.
“My twins were born very tiny and had to be fed every two hours at any time of the day or night. Very soon it became clear: if I want to do anything besides feeding, I need to feed them both at the same time, - says Emma, mother of two children from the UK. “I breastfed them two by hand using a breastfeeding pillow.”
Very soon it became clear: if I want to do anything besides feeding, I need to feed them both at the same time, - says Emma, mother of two children from the UK. “I breastfed them two by hand using a breastfeeding pillow.”
Other good positions for breastfeeding twins are two criss-cross cradles, one baby in the cradle and the other close at hand, reclining feeding, or sitting upright (one baby on one side, the other on the other).
11. Breastfeeding in the "hand-supported" or "dancer's hand" position
muscle tone (which is typical for premature babies, children suffering from various diseases or Down syndrome), try supporting his head and your chest at the same time. 4 Grasp your chest with your palm underneath so that your thumb is on one side and all the others are on the other. Move your hand slightly forward so that your thumb and forefinger form a "U" just in front of your chest. With the other three fingers, continue to support the chest. With your thumb and forefinger, hold the baby's head while feeding so that his chin rests on the part of the palm between them, your thumb gently holds the baby on one cheek, and your index finger on the other.![]() So the baby gets excellent support, and you can control his position and see if he is holding his breast.
So the baby gets excellent support, and you can control his position and see if he is holding his breast.
Literature
1 Colson SD et al. Optimal positions for the release of primitive neonatal reflexes stimulating breastfeeding. Early Hum Dev . 2008;84(7):441-449. - Colson S.D. et al., "Optimal Positions for Provoking Primitive Innate Reflexes to Induce Breastfeeding." Early Hume Dev. 2008;84(7):441-449.
2 UNICEF UK BFHI [ Internet ]. Off to the best start ; 2015 [ cited 2018 Feb ]. - UNICEF UK, Baby-Friendly Hospital Initiative, Start the Best You Can [Internet]. 2015 [cited February 2018].
3 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women's Health. 2007;52(6):638-642. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
J Midwifery & Women's Health. 2007;52(6):638-642. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." F Midwifery Women Health. 2007;52(6):638-642.
4 Wambach K, Riordan J, editors. Breastfeeding and human lactation. Jones & Bartlett Learning ; 2014. 966 p . - Wambach K., Riordan J., "Breastfeeding and female lactation". Burlington, MA: Publishing House Jones & Bartlett Learning ; 2014. Pp. 966.
Positions for breastfeeding | Medela
For most mothers, breastfeeding is a skill that needs to be learned. Therefore, mothers may need extra help in teaching breastfeeding skills. In particular, they may need guidance on how to position the baby and how to attach it to the breast in a way that is comfortable for both mother and baby. There are many breastfeeding positions that can suit every breastfeeding mother. It is very important that the mother always feels comfortable while breastfeeding. As a rule, the baby should be positioned so that his face is turned towards the mother's body, and the head, shoulders and hips are in line. The most commonly used postures are cradle, cross cradle, grip, and side lying.
It is very important that the mother always feels comfortable while breastfeeding. As a rule, the baby should be positioned so that his face is turned towards the mother's body, and the head, shoulders and hips are in line. The most commonly used postures are cradle, cross cradle, grip, and side lying.
Share this information
Cradle position
Cradle position is the most common position for feeding a baby.
The mother's hand supports the baby at the breast. The baby's head lies next to the mother's elbow, while her arm supports the baby along the back and neck. The baby's chest should be turned to the mother's chest.
Cross cradle position
In the cross cradle position, the mother takes the child with her other hand (relative to the cradle position), supporting his head and neck. With the other hand, she can support the breast and, if necessary, squeeze it, so that it is more convenient for the child to grab the nipple.
In this position, the mother can easily guide the baby to the breast when he is ready to take her.
“Capture” position
The baby is located on the side of the mother, his body and legs are at her fingertips. The mother holds the baby's head in her hand. In this position, you can also put your hand on a pillow.
This position may be optimal for mothers who have had a caesarean section because there is little or no pressure on the chest and abdomen in this position.
This position can also be beneficial for babies who are born low birth weight or who have problems latching on as the baby's head is fully supported in this position.
Side-lying position
Mother lies on her side facing the baby. The baby's mouth is on the same level as the nipple.
Mom can also use a pillow to support her back and neck.
This position may also be optimal for mothers who have had a caesarean section, as there is little or no pressure on the chest and abdomen in this position.
Literature
American Academy of Pediatrics and The American College of Obstetricians and Gynecologists. Breastfeeding Handbook for Physicians 2006). - American Academy of Pediatrics and American College of Obstetrics and Gynecology. The Doctor's Guide to Breastfeeding, 2006.
Colson, S.D., Meek, J.H., & Hawdon, J.M. Optimal positions for the release of primitive neonatal reflexes stimulating breastfeeding. Early Hum Dev . 84, 441–449 (2008). — Colson S.D., Mick J.H. and Hodon, JM, "Optimal Positions for Provoking Primitive Innate Reflexes to Induce Breastfeeding." Airlie Hume Dev. 84,441-449 (2008).
Cadwell, K. Latching-On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery Womens Health 52, 638–642 (2007).