What to feed a sick baby vomiting
Vomiting in children and babies
It's normal for babies and children to vomit occasionally. In most cases, it will last no longer than one to two days and isn't a sign of anything serious.
The most common cause of vomiting in children and babies is gastroenteritis. This is an infection of the gut usually caused by a virus or bacteria, which also causes diarrhoea. The symptoms can be unpleasant but your child will usually start to feel better after a few days.
However, persistent vomiting can sometimes cause your child to become severely dehydrated and occasionally it can be a sign of something more serious, such as meningitis.
This page outlines what to do if your child keeps vomiting and describes some of the common causes of vomiting in children and babies.
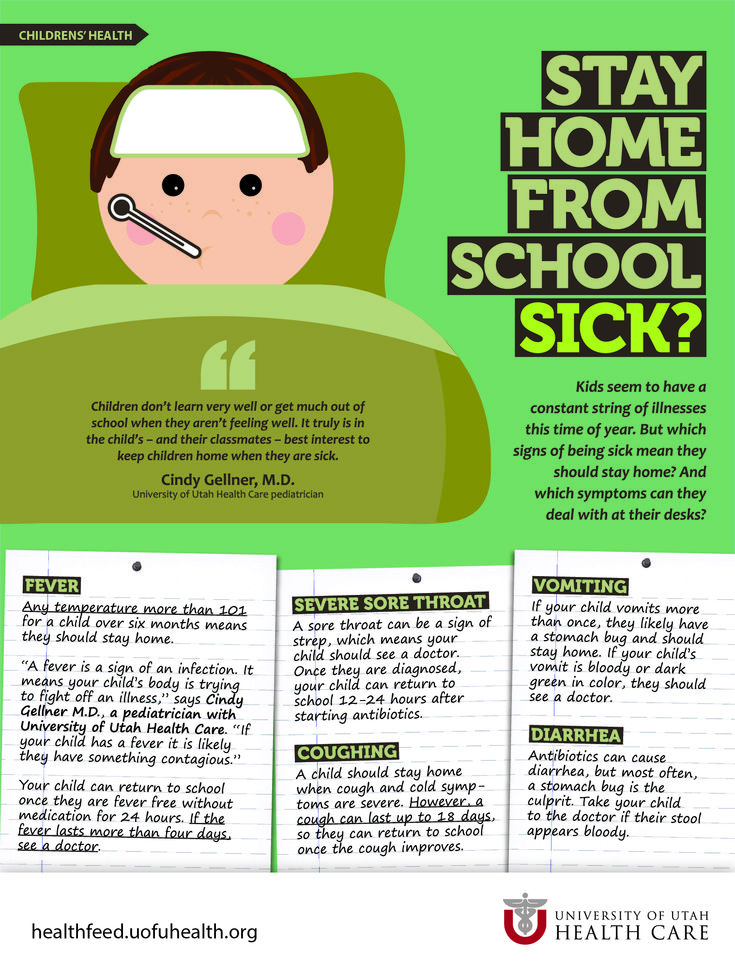
If your child has a high temperature, you can also read a separate page about fever in children.
What to do
If your child vomits, you should keep a close eye on them. Trust your instincts and contact your GP immediately if you're worried.
If the cause is just a tummy bug, your child should still be feeling well enough to eat, play and be their usual self. In this case, keep feeding them as normal and offer them regular drinks (see below).
But if they don't seem themself – for example, if they're floppy, irritable or less responsive – they may be seriously ill, so you should get medical help immediately.
When to get medical advice
You should contact your GP if:
- your child is repeatedly vomiting and is unable to hold down fluids
- you think they're dehydrated – symptoms of dehydration can include a dry mouth, crying without producing tears, urinating less or not wetting many nappies, and drowsiness
- their vomit is green or contains blood
- they have been vomiting for more than a day or two
Go to your nearest accident and emergency (A&E) department if your child is vomiting and develops sudden and severe tummy pain, or they're floppy, irritable or less responsive
Call 999 for an ambulance or go to your nearest A&E department immediately if they're vomiting and have a headache, stiff neck and a rash.
Looking after your child at home
In most cases, you can treat your child safely at home. The most important thing you can do is make sure they keep drinking fluids to prevent dehydration.
If your baby is vomiting, carry on breastfeeding or giving them milk feeds. If they seem dehydrated, they will need extra fluids. Ask your GP or pharmacist whether you should give your baby oral rehydration solution.
Oral rehydration solution is a special powder that you make into a drink. It contains sugar and salts to help replace the water and salts lost through vomiting and diarrhoea.
Children who are vomiting should keep taking small sips of clear fluid, such as water or clear broth. Fruit juice and fizzy drinks should be avoided until they're feeling better. If they're not dehydrated and haven't lost their appetite, it's fine for your child to eat solid foods as normal.
Again, speak to your GP or pharmacist if you're concerned about dehydration. They may recommend an oral rehydration solution for your child. Contact your GP or practice nurse if your child is unable to hold down oral rehydration solution.
Contact your GP or practice nurse if your child is unable to hold down oral rehydration solution.
If your child has diarrhoea and is vomiting, they shouldn't go to school or any other childcare facility until 48 hours after the last episode of diarrhoea or vomiting.
Read more about treating gastroenteritis in children.
Causes of vomiting in children
There are a number of possible causes of vomiting in children, which are described below.
Gastroenteritis
Gastroenteritis is an infection of the gut. It's a common cause of vomiting in children and usually lasts a few days.
Food allergy
Food allergies can cause vomiting in children, as well as other symptoms, such as a raised, red, itchy skin rash (urticaria) and swelling of the face, around the eyes, lips, tongue or the roof of the mouth.
Watch out for foods that may bring on vomiting and see your GP for a diagnosis if you think your child may have a food allergy.
Other infections
Vomiting can sometimes be a sign of an infection other than gastroenteritis, such as urinary tract infections (UTIs), middle ear infections, pneumonia or meningitis.
Contact your child's GP if they're vomiting and experiencing additional symptoms of an infection, such as a high temperature (fever) and irritability.
Appendicitis
Appendicitis is a painful swelling of the appendix, a finger-like pouch connected to the large intestine. It causes severe tummy pain that gets worse over time.
If your child has tummy pain that's gradually getting worse, contact your GP, or if they aren't open call NHS 24's 111 service immediately. You should call 999 for an ambulance if they have pain that gets worse quickly and spreads across their tummy.
In most cases of appendicitis, the appendix will need to be surgically removed as soon as possible.
Poison
Accidentally swallowing something poisonous can cause your child to vomit. If you think this is the case, contact your GP immediately or take your child to your nearest accident and emergency (A&E) department.
Causes of vomiting in babies
These include:
- gastroenteritis
- a food allergy or milk intolerance
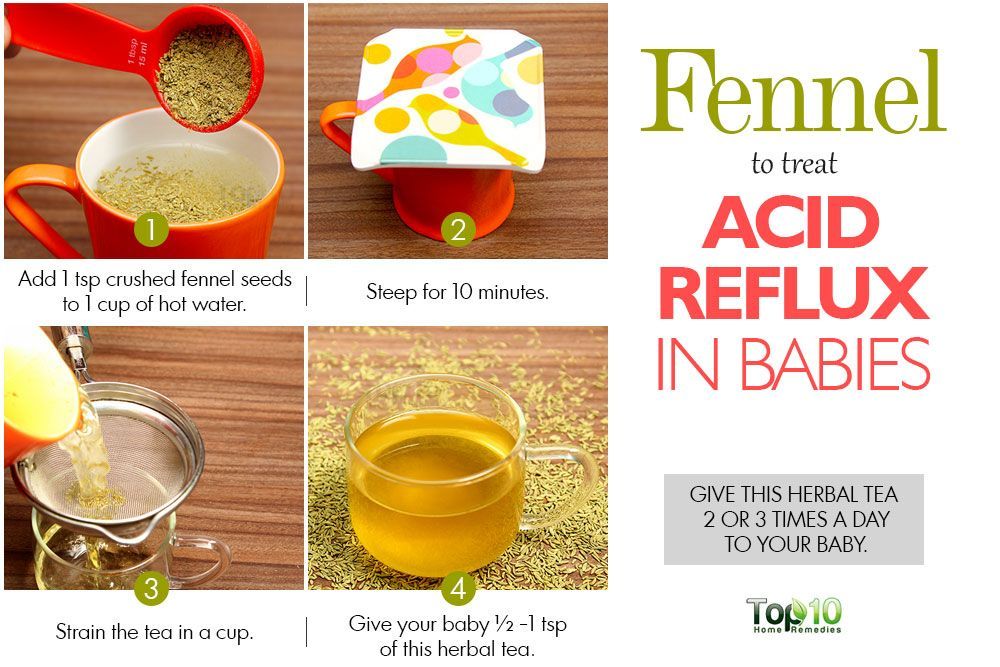
- gastro-oesophageal reflux – where stomach contents escape back up the gullet
- too big a hole in the bottle teat, which causes your baby to swallow too much milk
- accidentally swallowing something poisonous
- congenital pyloric stenosis – a condition present at birth where the passage from the stomach to the bowel has narrowed, so food is unable to pass through easily; this causes projectile vomiting
- a strangulated hernia – your baby will vomit frequently and cry as if they are in a lot of pain; this should be treated as a medical emergency
- intussusception (where the bowel telescopes in on itself) – as well as vomiting, your baby may look pale, floppy and have symptoms of dehydration
Vomiting (0-12 Months)
Is this your child's symptom?
- Vomiting (throwing up) stomach contents
- Other names for vomiting are puking, barfing and heaving
Causes of Vomiting
- Viral Gastritis.
 Stomach infection from a stomach virus is the most common cause. Also called stomach flu. A common cause is the Rotavirus. The illness starts with vomiting. Watery loose stools may follow within 12-24 hours.
Stomach infection from a stomach virus is the most common cause. Also called stomach flu. A common cause is the Rotavirus. The illness starts with vomiting. Watery loose stools may follow within 12-24 hours. - Food Allergy. Vomiting can be the only symptom of a food reaction. The vomiting comes on quickly after eating the food. Uncommon in infants, but main foods are eggs and peanut butter.
- Coughing. Hard coughing can also cause your child to throw up. This is more common in children with reflux.
- Serious Causes. Vomiting alone should stop within about 24 hours. If it lasts over 24 hours, you must think about more serious causes. An example is a kidney infection. A serious cause in young babies is pyloric stenosis. See below for more on this.
Pyloric Stenosis (Serious Cause)
- The most common cause of true vomiting in young babies.
- Onset of vomiting is age 2 weeks to 2 months
- Vomiting is forceful.
 It becomes projectile and shoots out.
It becomes projectile and shoots out. - Right after vomiting, the baby is hungry and wants to feed. ("hungry vomiter")
- Cause: The pylorus is the channel between the stomach and the gut. In these babies, it becomes narrow and tight.
- Risk: Weight loss or dehydration
- Treatment: Cured by surgery.
Vomiting Scale
- Mild: 1 - 2 times/day
- Moderate: 3 - 7 times/day
- Severe: Vomits everything, nearly everything or 8 or more times/day
- Severity relates even more to how long the vomiting goes on for. At the start of the illness, it's common for a child to vomit everything. This can last for 3 or 4 hours. Children then often become stable and change to mild vomiting.
- The main risk of vomiting is dehydration. Dehydration means the body has lost too much fluid.
- The younger the child, the greater the risk for dehydration.

Dehydration: How to Tell
- The main risk of vomiting is dehydration. Dehydration means the body has lost too much water.
- Vomiting with watery diarrhea is the most common cause of dehydration.
- Dehydration is a reason to see a doctor right away.
- Your child may have dehydration if not drinking much fluid and:
- The urine is dark yellow and has not passed any in over 8 hours.
- Inside of the mouth and tongue are very dry.
- No tears if your child cries.
- Slow blood refill test: Longer than 2 seconds. First, press on the thumbnail and make it pale. Then let go. Count the seconds it takes for the nail to turn pink again. Ask your doctor to teach you how to do this test.
When to Call for Vomiting (0-12 Months)
Call 911 Now
- Can't wake up
- Not moving
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Dehydration suspected.
 No urine in over 8 hours, dark urine, very dry mouth and no tears.
No urine in over 8 hours, dark urine, very dry mouth and no tears. - Stomach pain when not vomiting. Exception: stomach pain or crying just before vomiting is quite common.
- Age less than 12 weeks old with vomiting 2 or more times. Exception: normal spitting up.
- Vomited 3 or more times and also has diarrhea
- Severe vomiting (vomits everything) more than 8 hours while getting Pedialyte (or breastmilk)
- Head injury within the last 24 hours
- Weak immune system. Examples are sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
- Vomiting a prescription medicine
- Fever over 104° F (40° C)
- Fever in baby less than 12 weeks old. Caution: Do NOT give your baby any fever medicine before being seen.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- All other infants (age less than 1 year) with vomiting.
 See Care Advice while waiting to discuss with doctor.
See Care Advice while waiting to discuss with doctor.
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
Care Advice for Vomiting
- What You Should Know About Vomiting:
- Most vomiting is caused by a viral infection of the stomach.
- Vomiting is the body's way of protecting the lower gut.
- The good news is that stomach illnesses last only a short time.
- The main risk of vomiting is dehydration. Dehydration means the body has lost too much fluid.
- Here is some care advice that should help.
- Formula Fed Babies - May Give Oral Rehydration Solution (ORS) for 8 Hours:
- If vomits once, give half the regular amount of formula every 1 to 2 hours.
- If vomits formula more than once, offer ORS for 8 hours. If you don't have ORS, use formula until you can get some.
- ORS is a special fluid that can help your child stay hydrated. You can use Pedialyte or the store brand of ORS. It can be bought in food stores or drug stores.
- Spoon or syringe feed small amounts. Give 1-2 teaspoons (5-10 mL) every 5 minutes.
- After 4 hours without throwing up, double the amount.
- Return to Formula. After 8 hours without throwing up, go back to regular formula.
- Breastfed Babies - Reduce the Amount Per Feeding:
- If vomits once, nurse half the regular time every 1 to 2 hours.
- If vomits more than once, nurse for 5 minutes every 30 to 60 minutes. After 4 hours without throwing up, return to regular nursing.
- If continues to vomit, switch to pumped breastmilk. (ORS is rarely needed in breastfed babies. It can be used if vomiting becomes worse).
- Spoon or syringe feed small amounts of pumped milk. Give 1-2 teaspoons (5-10 mL) every 5 minutes.
- After 4 hours without throwing up, return to regular feeding at the breast. Start with small feedings of 5 minutes every 30 minutes. As your baby keeps down the smaller amounts, slowly give more.
- If vomits once, nurse half the regular time every 1 to 2 hours.
- Pumped Breastmilk Bottle-Fed Infants - Reduce the Amount per Feeding:
- If vomits once and bottle-feeding breastmilk, give half the regular amount every 1-2 hours.
- If vomits more than once within last 2 hours, give 1 ounce (30 mL) every 30 to 60 minutes.
- If continues to vomit, give 1-2 teaspoons (5-10 mL) every 5 minutes. Only if not tolerating breastmilk, switch to ORS (e.
 g., Pedialyte) for every 5 minutes for a few hours.
g., Pedialyte) for every 5 minutes for a few hours. - After 4 hours without vomiting, return to regular feedings. Start with 1 ounce (30 mL) every 30 minutes and slowly increase as tolerated.
- Stop All Solid Foods:
- Avoid all solid foods and baby foods in kids who are vomiting.
- After 8 hours without throwing up, gradually add them back.
- If on solid foods, start with starchy foods that are easy to digest. Examples are cereals, crackers and bread.
- Do Not Give Medicines:
- Stop using any drug that is over-the-counter for 8 hours. Reason: Some of these can make vomiting worse.
- Fever. Mild fevers don't need to be treated with any drugs. For higher fevers, you can use an acetaminophen suppository (such as FeverAll). This is a form of the drug you put in the rectum (bottom). Ask a pharmacist for help finding this product. Do not use ibuprofen. It can upset the stomach.

- Call your doctor if: Your child vomits a drug ordered by your doctor.
- Try to Sleep:
- Help your child go to sleep for a few hours.
- Reason: Sleep often empties the stomach and removes the need to vomit.
- Your child doesn't have to drink anything if his stomach feels upset and he doesn't have any diarrhea.
- Return to Child Care:
- Your child can return to child care after the vomiting and fever are gone.
- What to Expect:
- For the first 3 or 4 hours, your child may vomit everything. Then the stomach settles down.
- Vomiting from a viral illness often stops in 12 to 24 hours.
- Mild vomiting and nausea may last up to 3 days.
- Call Your Doctor If:
- Vomits clear fluids for more than 8 hours
- Vomiting lasts more than 24 hours
- Blood or bile (green color) in the vomit
- Stomach ache present when not vomiting
- Dehydration suspected (no urine in over 8 hours, dark urine, very dry mouth, and no tears)
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.
Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 12/02/2022
Last Revised: 09/21/2022
Copyright 2000-2022 Schmitt Pediatric Guidelines LLC.
Feeding a sick child
Publication date: 12/15/2016 08:22
April 22nd, 2016 Olga.
While the child grows up, he will be ill with various diseases more than once. About 80% is accounted for by SARS. Any disease (we are now talking about the flu, SARS) is characterized by poor health of the child - malaise, cough, runny nose, weakness, and maybe intestinal upset. And all this affects the appetite of the child. If a child has caught a cold, mothers always ask themselves the question: how to feed him properly? Proper nutrition of a sick child will help to quickly cope with the disease.
During an illness, the baby always has a poor appetite. There are physiological reasons for this:
There are physiological reasons for this:
- at elevated temperatures, blood circulation in the stomach slows down. because the body sends blood to vital organs: the heart and lungs. The process of digestion and assimilation of food slows down and the child needs less food than usual;
- during an illness, the liver actively fights toxins, the products of the vital activity of viruses and the decay of damaged cells, so a large amount of food carries an additional burden;
- the toxins themselves poison the body and the child, when he feels bad, not at all before eating;
- blocked nose, sore throat, difficult to swallow.
- Nutrition should be appropriate for the child's age;
- during illness, do not introduce new foods into the diet;
- food should be sparing - liquid or semi-liquid;
- make small meals if the baby does not want to eat, and the number of feedings can be increased;
- if the child refuses to eat, let him drink more fluids (water, compote, fruit drink, rosehip broth).
From the diet during illness should be excluded:
- Hard-to-digest foods - fatty meat, whole grain cereals, fresh vegetables and fruits.
- Foods harmful to the liver - fatty dairy products, chocolate, vegetable oil, lard, confectionery.
- Rough, which can damage the mucous membrane - nuts, seeds, crackers, cookies.
Useful menu
During an illness, a child needs food that is well absorbed by a weakened body. Therefore, chicken broth, vegetable soups, stewed and boiled vegetables are perfect for feeding a child during SARS.
To avoid mechanical irritation of the stomach, choose foods that are low in fiber. What foods are low in fiber? These are potatoes, cauliflower, pumpkin, rice and semolina, animal products.
Potatoes are especially delicate in fiber, so include mashed potatoes in your menu more often. You can cook mashed potatoes with sausage, cheese. Beautifully decorate the dish.
Animal protein must be present in the diet of a sick child, since it is a building material for protective antibodies. They are rich in lean meat - veal, beef, lean pork. For soups, use secondary broths from turkey meat, rabbit, chicken breast.
They are rich in lean meat - veal, beef, lean pork. For soups, use secondary broths from turkey meat, rabbit, chicken breast.
What else can you feed a child during illness? Yogurt helps out well, especially homemade, with the addition of berries.
Cook porridge for the child: semolina, oatmeal, you can also add berries from jam or defrosted.
A sick child needs vitamins. You can make vitamin drinks from rose hips, berries, cook jelly, dried fruit compote, berry juice. . Such drinks will alleviate the condition of the baby if the throat hurts. But with indigestion, milk should not be given at all.
To increase the appetite of the dish, it is desirable to arrange it beautifully so that the child immediately has a desire to eat it.
Nutrition for a convalescent child
After an acute period of illness, a period of convalescence begins, when the baby is on the mend and nutrition during this period plays an important role. The food of a recovering baby should be rich in energy in order to restore strength, contain minerals and vitamins, the food should be well absorbed.
As soon as the symptoms of the disease subside, do not rush to pounce on a child with enhanced nutrition, it will take a few more days to restore digestion. Continue to follow the diet, adding lean meat and fish, cheese, eggs, boiled vegetables and fruits to it.
Ideal for casseroles, puddings, steamed cutlets, vegetable soups. Introduce fruits and vegetables into the diet and do not forget about sour-milk products that will help restore the disturbed intestinal microflora. Let during this period the food be fractional, the child eat a little. And when the body gets stronger, the child will return to a normal diet.
Choosing tactics
When feeding a sick child, parents must remember that it is impossible to force-feed a child!
We provide a diet with easily digestible products. Some parents find it difficult to feed the baby during illness, he categorically refuses to eat. Psychologists advise not to turn feeding into a circus with musical numbers so that the child eats "well, at least one spoonful. "
"
If a child refuses to eat once, it will not bring much harm to health. He will not remain hungry, but will ask for something anyway when his appetite wakes up.
And don't scold the baby if he doesn't want to eat. Appetite will be restored.
Information from the site: deti-i-vnuki.ru/pitanie-bolnogo-rebenka/
Nutrition for intestinal infections in children
Parents of small children are especially afraid of intestinal infections. After all, it is important for a mother that her baby is full and healthy. And the presence of an intestinal infection in the body does not even allow to feed the child properly. Any meal is accompanied by vomiting, diarrhea, and in severe forms of the disease, children cannot eat at all.
Experienced grandmothers advise to keep the child on dry rations (ie, to eat crackers, dryers, biscuit cookies), others offer to treat immediately with herbal decoctions. Feeding children with an intestinal infection is a very important and delicate issue, so you should know not only how and what to feed a child, but also other important principles, for example, combating dehydration, drinking regimen, and so on. You can read about all this in the materials of this article.
You can read about all this in the materials of this article.
What is an intestinal infection
Intestinal infections are the second most common childhood disease and are more common in young children (under 3 years of age). In the morning, the child was healthy and cheerful, as after a couple of hours the baby abruptly begins to vomit, the stool is upset and the temperature rises. All these symptoms indicate the presence of an intestinal infection in the body.
Intestinal infection can be either viral or bacterial. From the names themselves it becomes clear what the difference between their pathogens is. In childhood, it is the rotovirus causative agent of intestinal infection that is more common.
As a type of intestinal infection, one can name:
- dysentery;
- salmonellosis;
- enterovirus.
At the first signs of an intestinal infection in a child, parents should not despair and become depressed. Doctors say that in 90% of cases, medical care is not needed and parents can cope with the disease on their own at home, you just need to follow the rules that will prevent dehydration.
Doctors say that in 90% of cases, medical care is not needed and parents can cope with the disease on their own at home, you just need to follow the rules that will prevent dehydration.
But, in the remaining 10%, the situation is more complicated and at home you can only aggravate the situation. This requires urgent medical intervention and qualified assistance. It is worth remembering that in acute forms of intestinal infection, rapid dehydration of the body occurs and if slowed down with treatment, it can be fatal.
An ambulance must be called if:
- Bloody manifestations have been noticed in the child's vomit or stool.
- If the child cannot get water to drink (the child cannot swallow liquid or the water comes out immediately with vomit).
- The first signs of dehydration begin to appear, such as: dry skin, dry tongue, lack of sweat, tears, urination (the child has not gone to the toilet in the last few hours).

- In case of upset stool or vomiting, symptoms such as a sharp increase in temperature (in severe forms more than 38.5 C), lethargy, drowsiness, complete or partial refusal to eat, vomiting or diarrhea can be observed.
How can you get an intestinal infection?
The very moment of infection with an intestinal infection occurs when a bacterium or virus enters the body, namely, it settles in the gastrointestinal tract.
There are several ways to become infected with an intestinal infection:
- Through food - when eating poor-quality, contaminated food.
- By water - by bathing in contaminated water, swallowing water, or using poor-quality water at home.
- Contact-household - dirty hands and non-compliance with the rules of personal hygiene.
Treatment of intestinal infection
In the treatment of acute intestinal infection, special attention is paid to replenishing fluid in the body, as well as the use of a number of antibiotics.![]() There is an opinion that antibiotics should be used in moderate and severe forms of the disease. Indeed, against the background of inhibition of the viability of microbes, antibiotics weaken the body's immunity, which leads to the development of dysbacteriosis, and hence the removal of all useful substances.
There is an opinion that antibiotics should be used in moderate and severe forms of the disease. Indeed, against the background of inhibition of the viability of microbes, antibiotics weaken the body's immunity, which leads to the development of dysbacteriosis, and hence the removal of all useful substances.
Prescribe antibiotics strictly after passing a series of tests, identifying the causes of the disease and monitoring by medical personnel.
Indications for prescribing therapeutic nutrition
One of the important factors in the treatment of children who have had an intestinal infection is proper nutrition or diet therapy. With improper nutrition, prolonged diarrhea, a sharp weight loss and lactose intolerance (milk is not absorbed by the body) can be seen.
The main function of diet therapy is the ability to adjust the diet, nutrition of the child and make timely adjustments based on the form of the disease, the state of the body and the rate of recovery. Scientists have proven that even in severe forms of the disease, the gastrointestinal tract retains the function of eating and absorbing nutrients, but if food does not enter the child’s body for a long time (water-tea diets), then the body loses its recovery function, which and leads to dramatic weight loss.
Scientists have proven that even in severe forms of the disease, the gastrointestinal tract retains the function of eating and absorbing nutrients, but if food does not enter the child’s body for a long time (water-tea diets), then the body loses its recovery function, which and leads to dramatic weight loss.
Principles of nutrition in intestinal infections
The main principle of the modern approach to the nutrition of children who have had acute intestinal infections is the rejection of water-tea diets and the correct selection of products that contributed to an increase in the level of body resistance.
The type of food, the amount of servings and the amount of food consumed per day will be determined by a number of factors:
- the age of the child;
- form of the disease;
- the presence of other diseases;
- feeding form.
There are several principles that should be applied to all forms of the disease. There must be a break at night, there should not be overfeeding and force-feeding. We should not forget that in feeding you must always adhere to the regimen. In older children, the urge to vomit is associated with overeating. It is necessary to adhere to the generally accepted principle: it is better to eat more often, but in smaller portions.
There must be a break at night, there should not be overfeeding and force-feeding. We should not forget that in feeding you must always adhere to the regimen. In older children, the urge to vomit is associated with overeating. It is necessary to adhere to the generally accepted principle: it is better to eat more often, but in smaller portions.
If the child has a mild form of intestinal infection, without severe intoxication of the body, doctors advise to reduce the amount of food consumed in the first days, the lack of food can be filled with liquid. It can be unsweetened teas, compotes, decoctions of chamomile, purified non-carbonated water. P
I'm looking for a better use in pureed form (soup-puree, porridge and scrambled eggs), so it will be easier for the body to perceive it. All cooked food should be boiled or steamed. And already for 5-6 days it will be possible to return to normal life. In mild forms of diarrhea, it is recommended to reduce the amount of food by 15-20% and increase the number of meals by 1-2. By the fourth day after the onset of the disease state, the volume of food becomes the same and the diet is restored. With medium forms, it is necessary to divide meals into 5-6 approaches, the amount of food received per day is reduced by 30%. On the 6-7th day, there is a complete restoration of the volume of portions, and the number of meals.
By the fourth day after the onset of the disease state, the volume of food becomes the same and the diet is restored. With medium forms, it is necessary to divide meals into 5-6 approaches, the amount of food received per day is reduced by 30%. On the 6-7th day, there is a complete restoration of the volume of portions, and the number of meals.
In severe forms of intestinal infections, the patient is transferred to fractional food intake, and the daily volume is reduced by half - 45-50%. On the fourth day, the volume is gradually increased and only on the 8th day the diet is resumed.
Drinking regimen
First of all, in case of an intestinal infection, doctors try to restore the body's water balance. The patient is recommended to drink 1 teaspoon of pure water every 5 minutes. Water allows you to remove all toxins from the body. You can also drink decoctions of chamomile, compotes, teas. It is important to take liquid in small portions. Too much fluid taken at one time can cause repeated vomiting and severe dehydration. Instead of water, it is mono to give the child a solution of rehydron, a slightly sweet compote of dried fruits, non-carbonated mineral water.
Too much fluid taken at one time can cause repeated vomiting and severe dehydration. Instead of water, it is mono to give the child a solution of rehydron, a slightly sweet compote of dried fruits, non-carbonated mineral water.
With diarrhea and vomiting, the water-salt balance of the body is disturbed. To restore it, it is recommended to drink Regidron. This drug can be purchased at a pharmacy or prepared at home. For a liter of water, you need to take 2 tbsp. spoons of sugar, 1 tbsp. a spoonful of coarse salt (fine you need to take 0.5 tablespoons) and 0.5 teaspoons of soda. It is not worth drinking such a drink in large doses, it is necessary to alternate. A teenager will need 50 ml 1 time in 1.5-2 hours, a child no more than 1 spoon at the same intervals. If there is a shortage of food, it must be supplemented with liquid.
Do's and don'ts for children with intestinal infection
In case of intestinal infection, remember that all food should be steamed or boiled, in the form of puree, rarely soup, soufflé or scrambled eggs.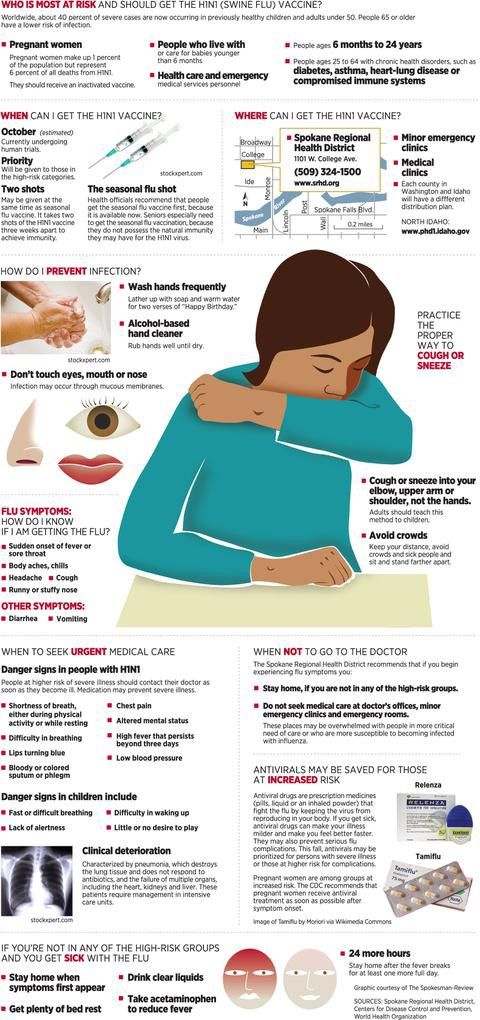 The less often and lighter the food used, the faster it is absorbed by the body. If, after eating one portion, the patient did not eat and wants more, this is a sure sign that he is on the mend. But do not rush, but rather take care of the body. In this case, try to maintain an interval of at least 30 minutes and then offer the child another meal.
The less often and lighter the food used, the faster it is absorbed by the body. If, after eating one portion, the patient did not eat and wants more, this is a sure sign that he is on the mend. But do not rush, but rather take care of the body. In this case, try to maintain an interval of at least 30 minutes and then offer the child another meal.
If an intestinal infection is transferred to the diet, you can use:
- Kissels from natural berries, preferably blueberries and dried fruits.
- Kashi on the water.
- Baked apples.
- Mashed potatoes.
- Vegetable puree.
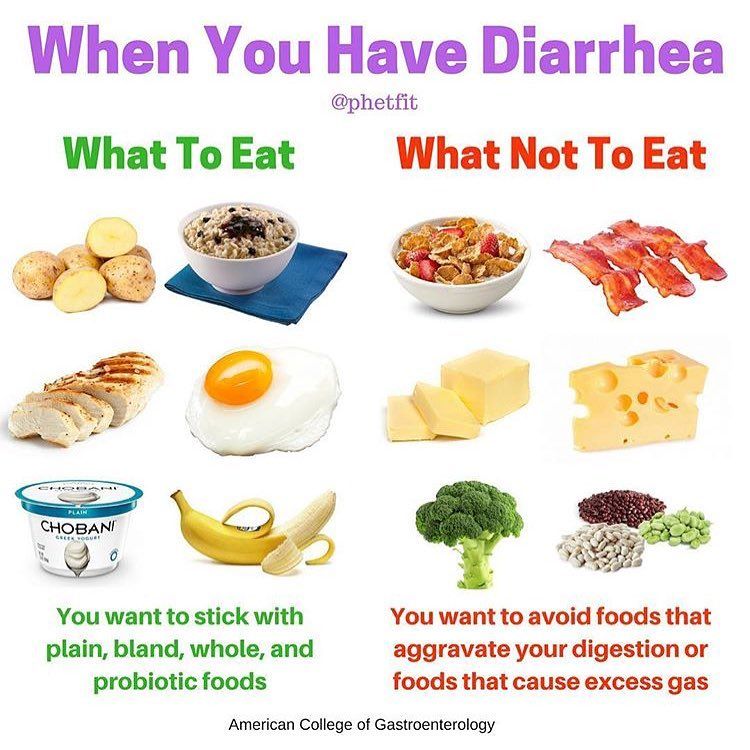
Do not eat if you have an intestinal infection:
- Whole milk.
- Milk porridge.
- Dairy products: fermented baked milk, cream.
- Rye crackers and bread.
- Vegetables, fruits rich in fiber: radish, cabbage, beets, cucumbers, radishes, lettuce, grapes, apricots and plums.
- Nuts, mushrooms and legumes.
- Bakery and confectionery products.
- Salted, smoked and pickled foodstuffs.
- Carbonated drinks and water.
- Fatty varieties of poultry and meat.
- Fatty fish.
- Rich broths and soups.
The first few days the child's diet will be as scarce as possible, but on the 4th day you can gradually introduce meatballs, steam cutlets, low-fat soups, boiled or steamed fish, eggs, bananas and peeled apples. On the recommendation of a doctor, you can enter milk porridge in a ratio of 1: 1.
Later you can add bakery products: dry biscuits, biscuits, rusks from dark bread varieties, prepared by yourself. By the end of the third week, you can gradually drive rich pastries.
Peculiarities of breastfeeding in case of intestinal infection
If the child is infancy, then you should not refuse breastfeeding, but you can increase the number of attachments, if the baby needs it, switch to feeding on demand.
The only food at this age is mother's milk. After all, it is believed that children with severe diarrhea tolerate lactose in human milk more easily, so there is no need to refuse it at all. In addition, lactose retains a large amount of useful substances and those that promote growth. All of them affect the speedy recovery of the intestine.
But it should be remembered that for children who are bottle-fed, on the contrary, doctors recommend reducing the dose of the resulting mixture and increasing the number of meals (more often, but in smaller portions). But more detailed recommendations on nutrition can only be obtained from the attending pediatrician. For children who have already been introduced to complementary foods, pediatricians recommend replacing milk porridges with water ones. May be allowed to add baked apples and dairy products to the diet. To increase the amount of pectin in the body, you can eat bananas, carrots and applesauce. You can also eat vegetable puree and mashed potatoes.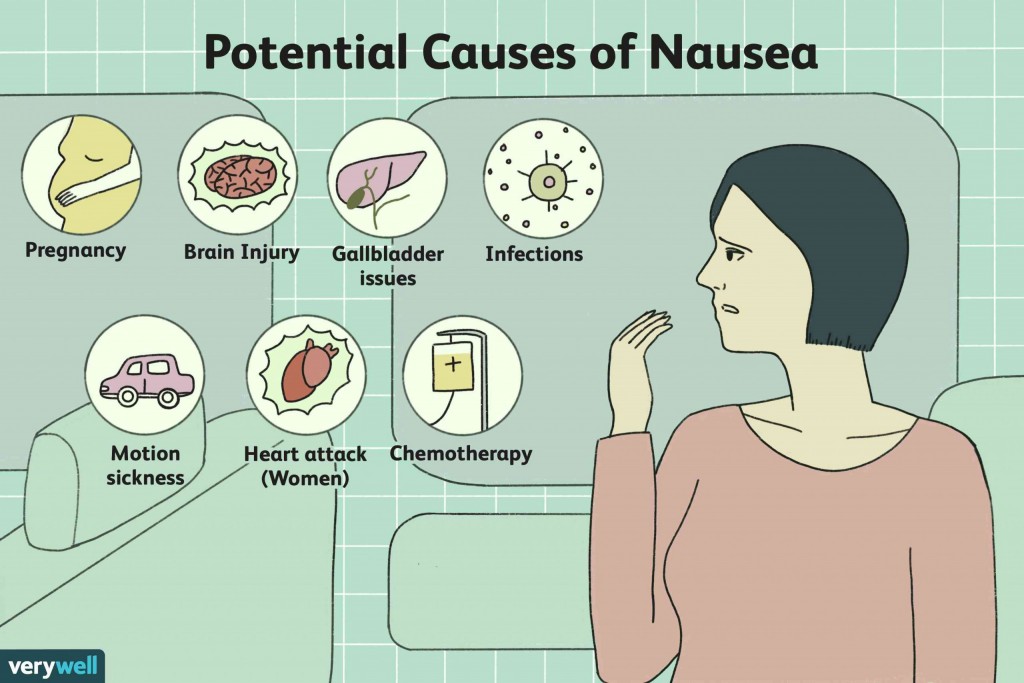
Learn more