When is it safe to feed baby honey
When Is It OK for Babies to Eat Honey?
Written by WebMD Editorial Contributors
In this Article
- Symptoms of Botulism
- Nutritional Information About Honey
- Benefits of Honey
- Types of Honey
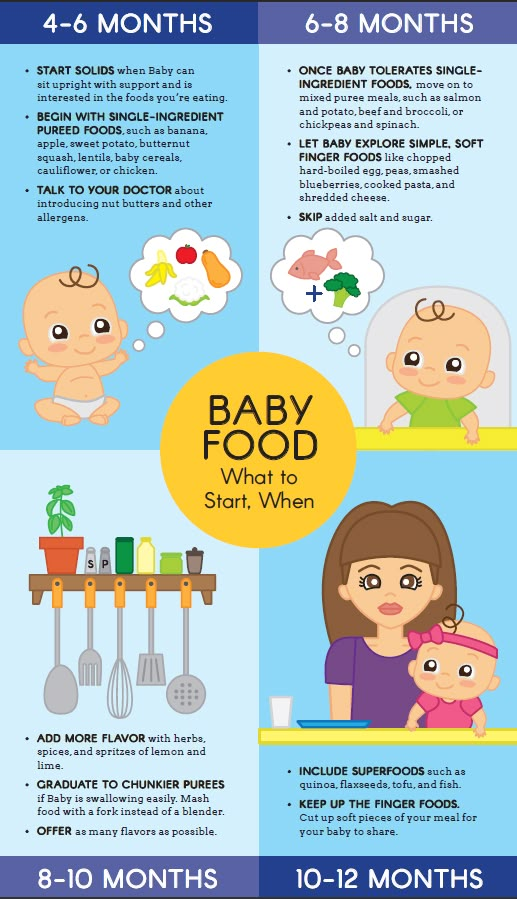
You may have heard about some of the benefits of honey. Parents looking for an alternative to sugar often turn to honey as a more natural choice. However, you should not give honey to your baby if they are under the age of one. Honey can cause botulism, which is a type of food poisoning, in babies under one year old. Babies should not have honey in any form, even cooked in baked goods.
Learn about the dangers of giving honey to babies and when it's safe for your baby to eat honey. When given at the right age, honey can be a part of your child's healthy diet.
Symptoms of Botulism
Giving honey to babies under 12 months has been associated with a rare, but serious, condition called infant botulism. Infant botulism is caused by exposure to the spores of a bacteria. Clostridium botulinum bacteria spores can grow and multiply in your baby's intestines. This produces a dangerous toxin that causes infant botulism.
Infant botulism occurs most often in babies under six months old. Most adults and older children have defenses in their intestines that prevent the spores from germinating and reproducing. Honey is not the only source of the spores that cause botulism. These spores can also be present in soil or dust. The symptoms of infant botulism can be mild or severe and can include:
- Overall weakness or floppiness
- Slow feeding
- Constipation
- Loss of facial expression
- Reduced gag reflex
Nutritional Information About Honey
Because honey is a natural sweetener, many people think it's healthier than sugar. Honey does contain trace amounts of:
- Vitamins
- Minerals
- Electrolytes
- Enzymes
- Amino acids
- Flavonoids
However, to get the benefits of these nutrients, you would have to eat far more honey than is healthy. Honey is a sugar and is high in calories. Honey is considered an added sugar, so it should be eaten in moderation.
Honey is a sugar and is high in calories. Honey is considered an added sugar, so it should be eaten in moderation.
The American Academy of Pediatrics (AAP) recommends that you not give children under the age of 2 any added sugars at all. The sugar that naturally occurs in fruits, whole grains, beans, or dairy is not considered added sugar. These natural sugars are necessary for your baby to grow and develop. Added sugars may be labeled as sucrose, dextrose, and, yes, honey. These are associated with a higher risk of insulin resistance, prediabetes, and type 2 diabetes.
Once your toddler is two, the AAP recommends they have no more than 25 grams, or 6 teaspoons, of added sugars daily. Honey can be used in place of sugar as long as it doesn't exceed the recommended amount.
Benefits of Honey
Cough suppressant. One clear benefit of honey is how effective it is as a cough suppressant. In a study of 105 children ages 2 to 18 who had upper respiratory infections, honey was more effective at relieving nighttime coughing than cough medicine. The World Health Organization (WHO) and the AAP recommend honey as a natural and effective cough suppressant.
The World Health Organization (WHO) and the AAP recommend honey as a natural and effective cough suppressant.
Wound healing. Honey has also been shown to be effective in treating some wounds and burns. Honey has anti-oxidant, anti-bacterial, and anti-inflammatory properties. Some studies have shown honey to be as effective as conventional treatments for acute wounds and superficial partial-thickness burns. However, more studies will need to be done to recommend it for medical use.
Types of Honey
There are over 300 types of honey. You can buy honey that is either raw or pasteurized. Unlike some raw foods, raw honey is considered safe to eat for children over 12 months old. Raw honey is the least processed type of honey and probably has the most nutrients. Honey's flavor and color change depending on the type of plants that bees used to make it.
Some of the different types of honey include:
- Acacia honey. This light honey has a floral scent but doesn't change the taste of foods you use it in.
- Clover honey. This is the most common type of honey in the US. It's a light honey with a sweet taste. It has a bit of a bitter aftertaste.
- Buckwheat honey. This is dark, full-flavored honey that is good in marmalade. This is also the type of honey that was used in the study as a cough suppressant.
Manuka honey. This is a dark honey that is made from the Manuka bush in New Zealand. It contains antioxidants, along with antibacterial and antifungal properties. It has been used topically to treat burns, cuts, and sores.
When Can Babies Eat Honey? Risks, Benefits, and Tips
When Can Babies Eat Honey? Risks, Benefits, and Tips- Health Conditions
- Featured
- Breast Cancer
- IBD
- Migraine
- Multiple Sclerosis (MS)
- Rheumatoid Arthritis
- Type 2 Diabetes
- Articles
- Acid Reflux
- ADHD
- Allergies
- Alzheimer's & Dementia
- Bipolar Disorder
- Cancer
- Crohn's Disease
- Chronic Pain
- Cold & Flu
- COPD
- Depression
- Fibromyalgia
- Heart Disease
- High Cholesterol
- HIV
- Hypertension
- IPF
- Osteoarthritis
- Psoriasis
- Skin Disorders and Care
- STDs
- Featured
- Discover
- Wellness Topics
- Nutrition
- Fitness
- Skin Care
- Sexual Health
- Women's Health
- Mental Well-Being
- Sleep
- Product Reviews
- Vitamins & Supplements
- Sleep
- Mental Health
- Nutrition
- At-Home Testing
- CBD
- Men’s Health
- Original Series
- Fresh Food Fast
- Diagnosis Diaries
- You’re Not Alone
- Present Tense
- Video Series
- Youth in Focus
- Healthy Harvest
- No More Silence
- Future of Health
- Wellness Topics
- Plan
- Health Challenges
- Mindful Eating
- Sugar Savvy
- Move Your Body
- Gut Health
- Mood Foods
- Align Your Spine
- Find Care
- Primary Care
- Mental Health
- OB-GYN
- Dermatologists
- Neurologists
- Cardiologists
- Orthopedists
- Lifestyle Quizzes
- Weight Management
- Am I Depressed? A Quiz for Teens
- Are You a Workaholic?
- How Well Do You Sleep?
- Tools & Resources
- Health News
- Find a Diet
- Find Healthy Snacks
- Drugs A-Z
- Health A-Z
- Health Challenges
- Connect
- Breast Cancer
- Inflammatory Bowel Disease
- Psoriatic Arthritis
- Migraine
- Multiple Sclerosis
- Psoriasis
Medically reviewed by Karen Gill, M. D. — By Ashley Marcin on April 4, 2018
D. — By Ashley Marcin on April 4, 2018
Overview
Exposing your baby to a variety of new foods and textures is one of the most exciting parts of the first year. Honey is sweet and mild, so parents and caregivers may think it’s a good choice as a spread on toast or a natural way to sweeten other items. However, experts recommend waiting until after your baby’s first birthday to introduce honey into their diet. This includes mass-produced honey, raw and unpasteurized honey, and local honey. This food rule also applies to all foods and baked goods containing honey.
Read on to learn more about introducing honey to your baby, including risks, benefits, and how to introduce it.
Risks
The primary risk of introducing honey too soon is infant botulism. Babies under 6 months of age are at the highest risk. While this condition is rare, most of the cases reported are diagnosed in the United States.
A baby can get botulism by eating Clostridium botulinum spores found in soil, honey, and honey products. These spores turn into bacteria in the bowels and produce harmful neurotoxins in the body.
These spores turn into bacteria in the bowels and produce harmful neurotoxins in the body.
Botulism is a serious condition. Some 70 percent of babies who get botulism may require mechanical ventilation for an average of 23 days. The average hospital stay for botulism is around 44 days. There may be many small improvements followed by setbacks. Most babies recover with treatment. The fatality rate is less than 2 percent.
Other liquid sweeteners, like molasses and corn syrup, may also carry a risk for botulism. Maple syrup is generally considered safe because it comes from inside a tree and cannot be contaminated by soil. Still, some doctors do not recommend giving babies sweeteners until after their first birthday. It’s best to check with your pediatrician before offering sweeteners as part of your child’s diet.
Botulism symptoms
The most common symptoms of botulism include:
- weakness, floppiness
- poor feeding
- constipation
- lethargy
Your baby may also be irritable, have trouble breathing, or have a weak cry. A few babies may also experience seizures.
A few babies may also experience seizures.
Symptoms typically show up within 12 to 36 hours of eating contaminated foods and often begin with constipation. However, some infants with botulism may not show signs until 14 days after exposure.
Some of the symptoms of botulism, like lethargy and irritability, may lead to an incorrect diagnosis of other conditions, like sepsis or meningoencephalitis, so it’s important to let your baby’s doctor know if they’ve eaten honey. Getting a proper diagnosis will ensure your baby gets the appropriate treatment.
If your baby has any symptoms of botulism and has recently consumed honey, you should treat it as an emergency. Head to your local emergency room as soon as possible.
Benefits of honey
Honey has been suggested to have a number of nutritional benefits that your baby can enjoy after they reach 12 months in age. Honey contains trace amounts of:
- enzymes
- amino acids
- minerals
- antioxidants
It also contains modest amounts of B vitamins and vitamin C. The nutritional value in your honey depends on the sources, as there are over 320 varieties.
The nutritional value in your honey depends on the sources, as there are over 320 varieties.
Honey is also sweeter than standard sugar. That means you can use far less of it than you would sugar and still get great flavor.
Other possible benefits include:
- It may act as a cough suppressant, but shouldn’t be used in children under 12 months of age.
- It may help with wound healing when applied topically. Again, this method should not be used in children younger than 12 months because botulism can enter the body through broken skin.
If you’re looking to get the nutritional benefits of honey, it may be best to stick with varieties that are not processed. Even then, you’d need to eat quite a bit to truly get nutritional value. In fact, a tablespoon of honey doesn’t provide your body with much benefit beyond added calories. So, this ingredient is best when used sparingly. Also, read your labels carefully, as some regular varieties may contain added sugars and other ingredients.
Is raw honey better than other types of honey?
Raw honey is honey that hasn’t been filtered or processed in any way. It comes directly out of the beehive and contains all the natural vitamins, minerals, and other healthy compounds found in filtered and processed honey. Raw honey may contain a slightly higher pollen count, so if you’re using honey to try to relieve seasonal allergies, raw honey may provide more benefits.
Raw honey can still cause botulism when consumed by babies under 1 year. Raw honey may also be more expensive than filtered or processed honey.
How to introduce honey
As with all added sweeteners, you don’t need to be in a hurry to give honey to your baby. If you want to introduce honey, incorporating it may be as simple as adding a bit to their favorite foods. As with any new food, it’s a good idea to introduce honey slowly. One method is the “four-day wait” approach to see if your little one has a reaction. To use this method, give your child (if they’re older than 1 year) honey, and then wait four days before adding it in another totally new food. If you see a reaction, contact your pediatrician.
If you see a reaction, contact your pediatrician.
To add honey to your baby’s diet, try any of the following:
- Mix honey into oatmeal.
- Spread honey onto toast.
- Mix honey into yogurt.
- Squeeze honey into a homemade smoothie.
- Use honey instead of maple syrup on waffles or pancakes.
If your child is too young to try honey, consult with your pediatrician. You may try using maple syrup as a substitute in recipes. Agave nectar is another option that is similar to honey without the risk of infant botulism.
Baking substitution
You can also swap honey for sugar in your favorite baking recipes. For every 1 cup of sugar called for in a recipe, substitute in 1/2 to 2/3 cups of honey. How much you use is up to you. Honey tends to taste sweeter than sugar, so you may want to start with less and add more to taste. Here are some other tips for substituting honey for sugar:
- For every 1 cup of honey you’re using in a recipe, reduce the other liquids by 1/4 cup.

- Add a 1/4 teaspoon of baking soda for each cup of honey to help reduce acidity.
- Consider reducing your oven temperature by about 25°F and keep a close eye for browning.
What about breastfeeding?
Infant botulism cannot be transmitted through breast milk. If your baby does contract botulism, experts recommend continuing to nurse or providing expressed breast milk while your baby is sick.
Takeaway
Honey can be a nice addition to your baby’s diet, but it’s important to wait until after 12 months of age. Foods to avoid include liquid honey, whether mass produced or raw, and any baked or processed foods containing honey. Read labels carefully to see if processed foods contain honey.
If you have additional questions about infant feeding and when to introduce certain foods, contact your pediatrician. Recommendations may change from year to year, and your child’s doctor should have the most up-to-date information.
Last medically reviewed on April 4, 2018
- Parenthood
- Baby
- 06 Months 1 Year
How we reviewed this article:
Healthline has strict sourcing guidelines and relies on peer-reviewed studies, academic research institutions, and medical associations..jpg) We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
We avoid using tertiary references. You can learn more about how we ensure our content is accurate and current by reading our editorial policy.
- Abassi J. (2014). Placebo better than watchful waiting when treating young children’s coughs.
news.psu.edu/story/332029/2014/10/27/research/placebo-better-watchful-waiting-when-treating-young-childrens - Beals K, et al. (2013). Effects of processing on the pollen and nutrient content of honey. DOI:
10.1096/fasebj.27.1_supplement.859.7 - Cox N, et al. (2002). Infant botulism.
aafp.org/afp/2002/0401/p1388.html - Da Silva PM, et al. (2016,). Honey: Chemical composition, stability, and authenticity [Abstract]. DOI:
10.1016/j.foodchem.2015.09.051 - Frequently asked questions (FAQs) about infant botulism. (2010).
infantbotulism.org/general/faq.php - HealthyChildren.org. (2015). Botulism.
healthychildren.org/English/health-issues/conditions/infections/Pages/Botulism. aspx
aspx - Mayo Clinic Staff. (2017). Honey.
mayoclinic.org/drugs-supplements-honey/art-20363819 - New York State Department of Health. (2011). Botulism (foodborne botulism and infant botulism).
health.ny.gov/diseases/communicable/botulism/fact_sheet.htm - Wellness Team. (2013). Sweeteners: Get the scoop. How best to satisfy your sweet tooth?
health.clevelandclinic.org/the-scoop-on-sweeteners/
Our experts continually monitor the health and wellness space, and we update our articles when new information becomes available.
Current Version
Apr 4, 2018
Written By
Ashley Marcin
Edited By
Nizam Khan (TechSpace)
Medically Reviewed By
Karen Richardson Gill, MD
Share this article
Medically reviewed by Karen Gill, M.D. — By Ashley Marcin on April 4, 2018
related stories
Is It Safe for Babies to Eat Eggs?
When Can Babies Eat Cheese?
When Can Babies Eat Beans?
When Can Babies Have Peanut Butter?
When Do Babies Start Eating Baby Food?
Read this next
Is It Safe for Babies to Eat Eggs?
Medically reviewed by Karen Gill, M.
 D.
D.You may have heard that you should wait to feed a baby eggs until their first birthday, but is this true? Learn when it’s safe for babies to eat eggs…
READ MORE
When Can Babies Eat Cheese?
Medically reviewed by Jillian Kubala, MS, RD
Your baby can eat cheese made from pasteurized milk shortly after it's safe to introduce solids. Here are some benefits — and risks — to know about.
READ MORE
When Can Babies Eat Beans?
This article looks at the potential health benefits of beans for babies — and how and when to safely add them into your little one’s increasingly…
READ MORE
When Can Babies Have Peanut Butter?
Medically reviewed by Karen Gill, M.D.
When babies eat peanut butter for the first time, parents need to watch out for symptoms of an allergic reaction.
 Here’s what else you need to know.
Here’s what else you need to know.READ MORE
When Do Babies Start Eating Baby Food?
Medically reviewed by Karen Gill, M.D.
As your little one grows you'll want to know when to start adding new foods to their diet. Learn more about when to introduce solids, how to choose…
READ MORE
What Is Baby-Led Weaning? Everything You Need to Know
By Alina Petre, MS, RD (NL)
Baby-led weaning introduces your child to their first foods without relying on spoon feeding. This article reviews baby-led weaning, including its…
READ MORE
The 10 Cutest Smash Cake RecipesREAD MORE
Kidney Problems in the Premature Baby
Medically reviewed by Karen Gill, M.D.
A baby's kidneys usually mature quickly after birth. Problems balancing the body's fluids, salts, and wastes can occur during the first four to five…
READ MORE
The Best Breast Pumps for 2023
Medically reviewed by Meredith Wallis, MS, APRN, CNM, IBCLC
Finding the best breast pump for you can be a challenge.
 That's why we've put together this list of options based on experience from moms who have…
That's why we've put together this list of options based on experience from moms who have…READ MORE
Signs and Symptoms of Group B Strep
Medically reviewed by Meredith Goodwin, MD, FAAFP
The symptoms of group B strep disease differ in babies and adults. Learn more about the signs of this condition in newborns and other high risk…
READ MORE
Feeding when sick | Medela
If you or your baby are unwell, you may wonder if it is safe to breastfeed. The great news is that breastfeeding when you're sick is most often good for both of you. Read more about this in our article.
Share this information
Did you know that a breastfed baby is usually much less prone to illness? Although it is impossible to avoid them completely, the protective properties of breast milk help babies get sick less often 1 and recover faster than formula-fed babies.
Breast milk contains antibacterial and antiviral agents. 2 The longer you breastfeed your baby, the lower the risk of colds and flu, ear and respiratory infections, nausea and diarrhea. 1 Scientists are already exploring the use of breast milk to treat everything from conjunctivitis to cancer. 3.4
Should a sick baby be breastfed?
Yes. Breastfeeding promotes recovery and also helps to calm the baby. Breast milk contains antibodies, white blood cells, stem cells, and protective enzymes that help fight infections and help your baby recover faster. 1,5,6 In addition, the composition of breast milk (the balance of vitamins and nutrients) is constantly adjusted to the baby's body to help him recover as soon as possible. Thus, you will spend less time on sick leave and visit the doctor less often. 7
“Breastfeeding gives the baby everything she needs when she is sick. This is his medicine, food, drink and comfort. For a baby, this is the best thing in the world,” says Sarah Beeson, a health visitor from the UK.
For a baby, this is the best thing in the world,” says Sarah Beeson, a health visitor from the UK.
Surprisingly, when a child becomes ill, the composition of breast milk changes. When you come into contact with pathogens of bacterial and viral infections, your body begins to produce antibodies to fight them, which are then passed through milk to your baby. 8 When your baby is sick, your milk also spikes in immune-boosting cells (white blood cells). 5
In addition, breast milk is very easy to digest, making it ideal for babies with indigestion.
“At 12 months my daughter contracted norovirus and could only breastfeed,” recalls Maya, a mother of two in Spain. produce more milk. It was amazing. After 48 hours, I was able to meet the daily requirement for milk. It saved my baby from a drip."
It should be taken into account that sometimes during an illness it is necessary to change the habitual breastfeeding regimen. For example, with a cold, a baby may want to eat more often, but little by little, both to calm down and because of nasal congestion, which makes it difficult to apply to the chest for a long time.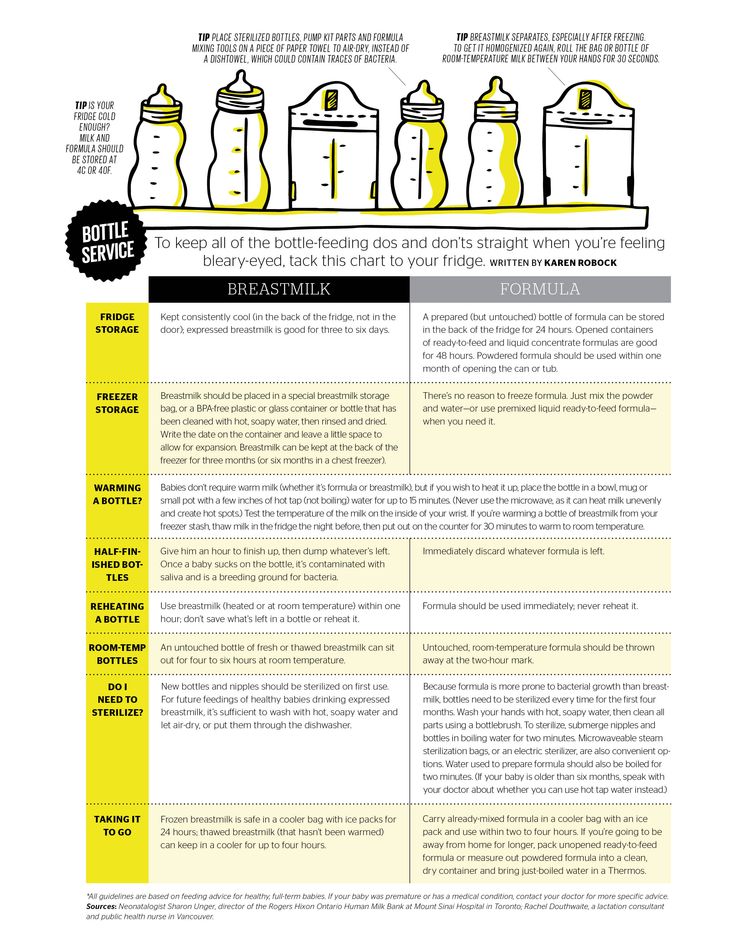 If your baby has a stuffy nose, an upright breastfeeding position may be more comfortable, so don't be afraid to try different breastfeeding positions.
If your baby has a stuffy nose, an upright breastfeeding position may be more comfortable, so don't be afraid to try different breastfeeding positions.
What should I do if my baby is seriously unwell and cannot breastfeed?
Occasionally, if a child feels unwell, they may not have an appetite or the strength to feed. If your baby is not eating well, seek advice from your healthcare provider, nurse practitioner, or lactation consultant to help prevent dehydration.
You may be asked to express milk to feed your baby with a bottle, a Soft Cup*, or other suitable method that requires minimal effort from the baby. Pumping on a regular breastfeeding schedule will also help keep your milk supply stable.
You can express milk with one of our convenient breast pumps, such as the modern electronic Swing Flex** or the Harmony** manual breast pump. Rest assured, freshly expressed breast milk is just as good as breast milk, so your baby will get all the protection and support it needs.
If you have concerns about your baby's health or how much milk they are drinking, see your doctor as soon as possible.
Can I continue to breastfeed if I become ill myself?
You may not want to do this if you feel unwell, but in most cases it is best to continue breastfeeding. If you have a cold, runny nose, diarrhoea, vomiting, or mastitis, continue breastfeeding as normal with your doctor's approval. The baby is unlikely to become infected through breast milk. What's more, the antibodies in your milk will help reduce your baby's risk of contracting the same 13 virus.
“Breastfeeding when sick is not only safe most of the time, but also beneficial. Your baby is the least at risk of catching your upset stomach or cold, as he is already in close contact with you and receives a daily dose of protective antibodies from milk, ”says Sarah Beeson.
If there is a risk of contracting a viral infection by airborne droplets, it is advisable to temporarily switch to expressing breast milk and bottle feeding.
In order not to lose the amount of milk produced when the body is still weakened by the disease, it is best to use the Swing Maxi Flex ** double breast pump, which helps to stimulate lactation, increase the amount of milk (by 18% on average) and increase its fat content (+1% ) 14 .
However, breastfeeding and pumping when sick can be very tiring. You need to take care of yourself so that you can take care of the baby. Try to drink more fluids, eat when you can, and get plenty of rest. Crawl under the covers for a few days and ask family or friends to help care for your baby if possible, so you can put all your energy into recovery.
“Don't worry about your milk supply, it will last. Most importantly, do not stop breastfeeding abruptly so that mastitis does not develop, ”adds Sarah.
Proper hygiene is very important to reduce the risk of spreading the disease. Wash your hands with soap and water before and after breastfeeding and pumping, preparing and eating food, using the toilet and changing diapers.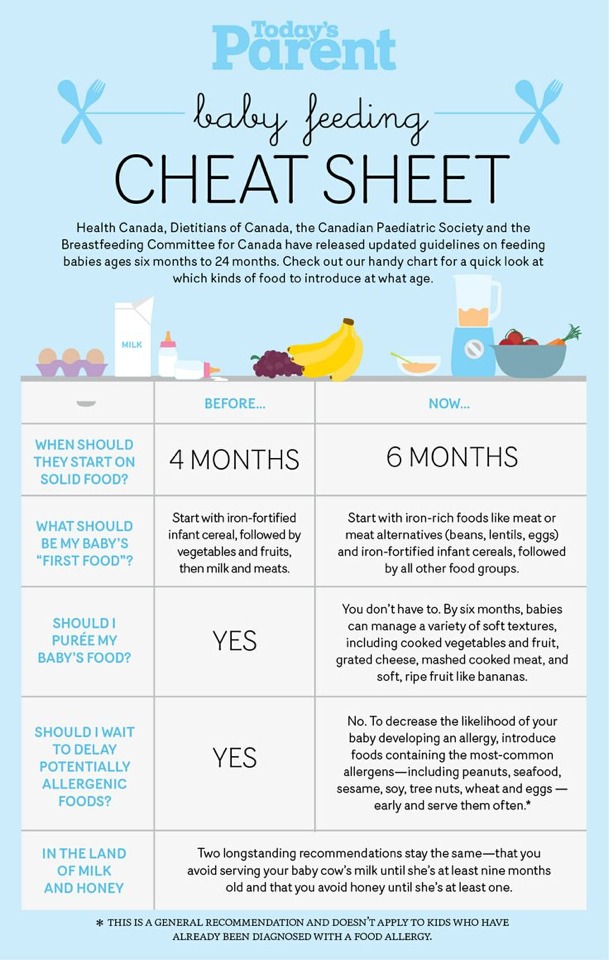 Use a tissue when coughing and sneezing, or cover your mouth with the crook of your elbow (not your palm) if you don't have a tissue handy. Be sure to wash or sanitize your hands after coughing, sneezing, and blowing your nose.
Use a tissue when coughing and sneezing, or cover your mouth with the crook of your elbow (not your palm) if you don't have a tissue handy. Be sure to wash or sanitize your hands after coughing, sneezing, and blowing your nose.
Can I take medication while breastfeeding?
In agreement with the attending physician and compliance with the dosage, certain medications are allowed. 9.10
.
“When talking to a doctor or pharmacist for any reason, always state that you are breastfeeding,” she continues.
What about long-term treatment?
If you are on long-term treatment for diabetes, asthma, depression, or other chronic conditions, the benefits of breastfeeding may outweigh the risks. “Breastfeeding is often possible for almost any disease, with the exception of some very rare conditions,” Sarah says, “you will be very familiar with the drugs you are taking, and during pregnancy you can discuss them with your doctor or other specialist. There is guidance on the safe use of various medicines that all healthcare professionals use.” In any case, you should consult with your doctor.
There is guidance on the safe use of various medicines that all healthcare professionals use.” In any case, you should consult with your doctor.
“I was on high doses of epilepsy medication, but I was still able to breastfeed,” recalls Nicola, a mother from the UK. “I saw a neurologist to ensure my son was safe and to minimize the risk of a seizure. Seizures can happen due to lack of sleep, and I fed day and night, but I took good care of myself, and my husband supported me. It was a positive experience."
What if I have to go to the hospital?
If you need to be hospitalized or urgently hospitalized, there are different ways to continue feeding your baby healthy breast milk so that you can return to normal breastfeeding after you are discharged.
“Express and freeze breast milk so that the caregiver can feed the baby. Practice at home ahead of time and be sure to let your doctors know that you are a breastfeeding mother, both before entering the hospital and while in it, ”recommends Sarah.
“If the baby is very small, you may be allowed to take him with you. Find out if the hospital has a supervising doctor or lactation consultant to contact. This specialist will support you, especially if you are in a general ward. If hospitalization is urgent, warn the doctors that you have a baby so that they take this into account.
Surgery under local or general anesthesia does not necessarily mean that breastfeeding will have to be stopped, or milk will need to be pumped and discarded. By the time you recover from surgery and can hold your baby, the amount of anesthetic in your breast milk will be minimal, so breastfeeding will be safe in most cases. 10 However, it is always best to consult your doctor or attending physician beforehand.
To ensure that the situation of treatment or departure does not affect the baby's diet, it is advisable to create a breast milk bank. This should be done daily by expressing one extra serving and freezing it in the handy, durable Medela Breast Milk Storage Bags. Even stored for several months and then thawed, your carefully prepared milk will still be incomparably healthier than formula.
Even stored for several months and then thawed, your carefully prepared milk will still be incomparably healthier than formula.
For hygienic and easy pumping, use a breast pump with 2-Phase Expression technology for a fast, full flow of milk. For example, the ultra-comfortable Swing Flex** breastpump that adapts to the shape of your breasts and allows you to pump milk in a comfortable position, even lying back on the pillows 15 .
Don't forget to sterilize your breast pump with the Quick Clean microwave bags. Medela milk storage bags do not need to be handled as they are aseptically packaged and ready to use immediately.
Are there times when breastfeeding is not allowed?
In some cases, for the safety of the baby, breastfeeding should be stopped for a while, and instead, milk should be expressed and discarded to maintain milk production until the end of treatment. This includes radiotherapy and chemotherapy for cancer, herpes sores on the chest, and infections such as tuberculosis, measles, or blood poisoning that can be transmitted through breast milk. 11.12 Consult with a qualified professional about your condition to decide whether breastfeeding can continue in such cases.
11.12 Consult with a qualified professional about your condition to decide whether breastfeeding can continue in such cases.
For quality lactation support during this period, you can use the dual electronic breast pump with innovative Flex technology or rent a Symphony Clinical Breast Pump** if available. A list of cities where you can rent a breast pump can be found on the "Rent a Medela Clinical Breast Pump" page.
Literature
1 Victora CG et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet . 2016;387(10017):475-490. - Victor S.J. et al., "Breastfeeding in the 21st century: epidemiology, mechanisms and long-term effects". Lancet 2016;387(10017):475-490.
2 Lönnerdal B. Bioactive proteins in breast milk. J Pediatric Child Health. 2013;49 Suppl 1:1-7. - Lönnerdahl B., "Biologically active proteins of breast milk". F Pediatrician Child Health. 2013;49 Suppl 1:1-7.
F Pediatrician Child Health. 2013;49 Suppl 1:1-7.
3 Australian Breastfeeding Association [Internet]. Topical treatment with breastmilk: randomized trials. [ cited 2018 Apr 4]. Available from https://www.breastfeeding.asn.au - Australian Breastfeeding Association [Internet]. "Topical treatment with breast milk: a randomized trial". [cited 4 April 2018] See article at https://www.breastfeeding.asn.au
4 Ho JCS et al. HAMLET–A protein-lipid complex with broad tumoricidal activity. Biochem Biophys Res Commun. 2017;482(3):454-458. - Ho J.S.S. et al., "HAMLET - a protein-lipid complex with extensive antitumor activity". Biochem Biophys Res Comm. 2017;482(3):454-458.
5 Hassiotou F et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clin Transl Immunology . 2013;2(4): e 3. - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
Clin Transl Immunology . 2013;2(4): e 3. - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
6 Hassiotou F, Hartmann PE. At the dawn of a new discovery: the potential of breast milk stem cells . Adv Nutr . 2014;5(6):770-778. - Hassiot F, Hartmann PI, "On the threshold of a new discovery: the potential of breast milk stem cells." Adv. 2014;5(6):770-778.
7 Ladomenou F et al. Protective effect of exclusive breastfeeding against infections during infancy: a prospective study. Arch Dis Child . 2010;95(12):1004-1008. - Ladomenu, F. et al., "The effect of exclusive breastfeeding on infection protection in infancy: a prospective study. " Arch Dis Child. 2010;95(12):1004-1008.
" Arch Dis Child. 2010;95(12):1004-1008.
8 Hanson LA. Breastfeeding provides passive and likely long-lasting active immunity. Ann Allergy Asthma Immunol . 1998;81(6):523-533. — Hanson, L.A., "Breastfeeding provides passive and likely long-term active protection against disease." Ann Allergy Asthma Immunol. 1998;81(6):523-533.
9 Hale TW, Rowe HE. Medications and Mothers' Milk 2017. 17th ed. New York, USA: Springer Publishing Company; 2017. 1095 p . — Hale T.W., Rowe H.I., Medications and Breast Milk 2017. 17th edition. New York, USA: Publishing House Springer Publishing Company ; 2017. p. 1095.
10 Reece-Stremtan S et al. ABM Clinical Protocol# 15: Analgesia and anesthesia for the breastfeeding mother, Revised 2017. Breastfeed Med . 2017;12(9):500-506. - Rees-Stromtan S. et al., AVM Clinical Protocol #15: Analgesia and Anesthesia for Nursing Mothers, 2017 edition. Brestfeed Med (Breastfeeding Medicine). 2017;12(9):500-506.
Breastfeed Med . 2017;12(9):500-506. - Rees-Stromtan S. et al., AVM Clinical Protocol #15: Analgesia and Anesthesia for Nursing Mothers, 2017 edition. Brestfeed Med (Breastfeeding Medicine). 2017;12(9):500-506.
11 Lamounier JA et al. Recommendations for breastfeeding during maternal infections. J Pediatr 2004;80(5 Suppl ):181-188. - Lamunier J.A. et al., Guidelines for Breastfeeding during Maternal Infectious Diseases. J Pediatrician (Journal of Pediatrics) (Rio J). 2004;80(5 Suppl):181-188.
12 Hema M et al., Management of newborn infant born to mother suffering from tuberculosis: Current recommendations & gaps in knowledge. Indian J Med Res . 2014;140(1):32-39. - Hema M. et al., "Working with the Infant Born to a Mother with Tuberculosis: Current Recommendations and Gaps. " Indian W Med Res. 2014;140(1):32-39.
" Indian W Med Res. 2014;140(1):32-39.
13 Lönnerdal B. Nutritional and physiologic significance of human milk proteins. Am JClin Nutr. 2003;77(6):1537S-1543S. Lönnerdahl B., "Biologically active proteins of breast milk". F Pediatrician Child Health. 2013;49 Suppl 1:1-7
14 Prime et al., Simultaneous Breast Expression in Breastfeeding Women Is More Efficacious Than Sequential Breast Expression, Breastfeed Med. Dec 2012; 7(6): 442–447. Prime DK and co-authors. "During the period of breastfeeding, simultaneous pumping of both breasts is more productive than sequential pumping." Brestfeed Med (Breastfeeding Medicine). 2012;7(6):442-447.
15 ClinicalTrials.gov [Internet]. Bethesda MD: National Library of Medicine, USA, data on file: NCT03091985. Clinical Research.gov [Internet]. Bethesda MD: National Library of Medicine, USA, data on file: NCT03091985.
Check out the instructions, consult with a specialist
* Ru FSZ 2010/07353 dated 07/19/10
** RU No. FCZ 2010/06525 dated 17/03/2021
FCZ 2010/06525 dated 17/03/2021
9000 9000 9000 9000 9000
000 Is it possible to eat honey while breastfeeding a nursing mother
Home » Breastfeeding
Contents
A nursing mother has to carefully monitor her diet, some foods are excluded from the diet due to their allergenicity. Unfortunately, they include honey. On the one hand, when breastfeeding, honey is a rather useful product, as it has a unique composition, but on the other hand, the pollen contained in it can cause severe allergies in the baby.
- If a mother eats honey while breastfeeding, her milk becomes sweet and pleasant. Whether this has any meaning for the child is unknown, but perhaps it brings him some pleasure;
- The nutritional properties of milk are significantly increased by the use of this product by the nurse. Honey is a natural dietary supplement, as it contains a large amount of vitamins (C, K, PP, H, E), trace elements (potassium, iron, calcium, copper and others), and also contains 76% sugars (fructose and glucose) in easily digestible form;
- During breastfeeding, honey is an excellent sugar substitute for mom.
 It reduces the recovery period after childbirth due to its beneficial effect on the entire body: it normalizes metabolic processes and helps a woman to get in shape sooner. In addition, honey perfectly stimulates the production of milk;
It reduces the recovery period after childbirth due to its beneficial effect on the entire body: it normalizes metabolic processes and helps a woman to get in shape sooner. In addition, honey perfectly stimulates the production of milk; - Honey has a sedative effect, helps mom cope with postpartum depression. It has been observed that children who receive milk from a mother who eats honey have a more stable nervous system, are less naughty and sleep better.
Hazards of honey during breastfeeding
Raw honey may contain spores of the bacteria Clostridium botulinum , which are extremely dangerous for children under 6 months of age. Once in the baby's body, they can cause a dangerous disease - children's botulism, which manifests itself as acute poisoning. After six months, the child's digestive system becomes more resistant to this disease, and adults do not get sick at all, since the pathogen completely dies in the acidic gastric environment of an adult. Therefore, the breast milk of a mother who consumes honey cannot contain toxic spores and is absolutely safe for the baby in this sense. Children under 1 year of age should not be given pure honey, even if they do not have an allergic reaction to it.
Therefore, the breast milk of a mother who consumes honey cannot contain toxic spores and is absolutely safe for the baby in this sense. Children under 1 year of age should not be given pure honey, even if they do not have an allergic reaction to it.
Before using honey while breastfeeding, make sure your baby is not allergic to it. The first month after childbirth, it is better to wait with honey, and then start with 1 teaspoon in 2 to 3 days and watch the baby's reaction. If there is no allergy, you can safely eat honey every other day for 1 teaspoon for up to 6 months, and for six months - 1 teaspoon every day.
According to the latest data, not so many people are allergic to honey, or rather to the pollen in it. Most often, an allergic reaction occurs to antibiotics given to bees or to sugar syrups and additives contained in fake honey.
How to choose good honey
If you are a breastfeeding mother and you decide that you will not refuse honey, then you must be sure that it is of high quality. Ideally, honey should be taken from familiar beekeepers or in an apiary, where it is more likely that it is natural and does not undergo additional processing. Real honey is always candied after a few months, so if you see amber honey in the supermarket in winter, know that it has been heat-treated. It is known that honey loses its valuable properties when heated above 40 0 C, so it makes no sense to use it with hot tea or add it to boiling water.
Ideally, honey should be taken from familiar beekeepers or in an apiary, where it is more likely that it is natural and does not undergo additional processing. Real honey is always candied after a few months, so if you see amber honey in the supermarket in winter, know that it has been heat-treated. It is known that honey loses its valuable properties when heated above 40 0 C, so it makes no sense to use it with hot tea or add it to boiling water.
The least allergenic is honey of light varieties, especially from white locust: it is rich in vitamin A and has a pronounced calming effect, which is important for a nursing mother.
Signs of real honey:
- Fresh honey should be transparent. Various additives give it a hazy hue;
- Real honey must have flavor;
- Dip a wooden stick in honey, if it is natural, it will slowly and evenly flow from it in a continuous thread. Honey with added sugar flows intermittently or in drops;
- Put some honey on a paper towel.
 If wet spots appear on it, then the honey is immature. Honey is considered mature if it contains no more than 20% moisture;
If wet spots appear on it, then the honey is immature. Honey is considered mature if it contains no more than 20% moisture; - Dilute honey in water at room temperature and add iodine to it. In the presence of starch in the composition, a blue color will occur;
- 1 liter of mature honey has a mass of at least 1.4 kg;
- Over time, honey thickens and becomes cloudy - this is a natural crystallization process and a sign of good quality.
How to check whether honey is natural or fake:
With all the value of this product, it should be remembered that the benefits of honey are not in its quantity, but in regular use. And, of course, if the baby is allergic to it, then honey should be excluded from the diet.
Reading on the topic LB: the most important tips for breastfeeding mothers
Do you want to be the first to read our materials? Subscribe to our telegram channel or VKontakte group.