Why won t my baby burp after feeding
How to burp a sleeping baby: Effective methods
When a baby falls asleep without burping, parents and caregivers can try a few methods to help them relieve wind while staying asleep.
The act of breastfeeding or feeding from a bottle often has a calming effect. As a result, it can make many infants fall asleep during or after their meal.
This can pose a problem if the baby has swallowed air during their feed. They may need to release air through a burp, which is more difficult to do when asleep. Their body may be too relaxed to get into a burping position, or the parent or caregiver may not wish to risk waking the baby from their slumber.
However, many people find that they must burp their baby after every feed — sleeping or not. If the baby does not release air through a burp after feeding, they may have discomfort later as it moves through the intestines and causes gas.
In addition, some babies are so sleepy at the breast or bottle that they fail to take in enough calories at their meals. It may sometimes be necessary to wake the baby during feeding to help them eat more. Burping the baby may help by eliminating some feelings of fullness and helping them stay awake longer.
A parent or caregiver will often need to decide on a case-by-case basis whether they should try to burp their sleeping baby or simply let them sleep.
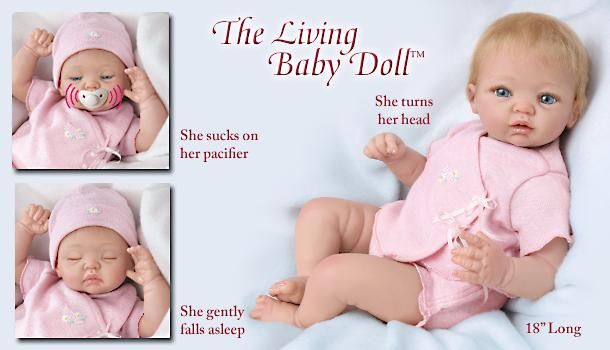
Share on PinterestBurping a baby may help relieve discomfort after feedings.As air travels upward, burping positions usually require the baby to be at least partially upright. This position encourages any air bubbles to move upward, passing through the throat and out of the mouth.
It is possible to burp a sleeping baby, often without waking them completely. Each baby is different, so people may need to try various techniques to find one that works.
Method 1: Shoulder
This method is suitable for babies who are sound sleepers. It can also be useful if a person needs to wake a baby up to continue their feeding.
- Turn the baby upright and lean them against the upper chest.
 Put one hand under their buttocks for support. The baby’s head should be on top of the shoulder.
Put one hand under their buttocks for support. The baby’s head should be on top of the shoulder. - Gently pat the baby’s back between their shoulder blades. Use an open palm to pat, being firm but gentle.
- If patting does not work, try rubbing their upper back in circular motions with the palm.
If the aim is to keep the baby awake, lightly bouncing them while they are on the shoulder may help wake them while also bringing up a burp.
Method 2: Chest
If a shoulder burp tends to wake the baby up, try a chest burp instead. Placing the baby on the chest can feel more comforting for them than the shoulder, so this position can often allow them to stay asleep after feeding.
- Gently lift the baby to the chest, putting one hand on their back and one under their buttocks.
- Avoid stretching their legs out. Allow their body to stay in a curled up position, which may make them less likely to wake up.
- Use the hand that is on their back to rub it, making circular motions first.
- If rubbing does not produce a burp, try gentle pats between their shoulders.
Method 3: Hip
The hip method works well for people who prefer to breastfeed their baby while lying down. It may help keep the baby asleep because the parent or caregiver does not have to sit up, and the baby is not fully upright.
- Gently place the baby’s tummy down over the hip or belly. Make sure that the baby’s head remains elevated above their body.
- Gently pat their back between the shoulder blades.
- Alternatively, rub their back in an upward circular motion.
Method 4: Arm hold
For smaller babies, the arm hold method can be useful. However, it is not always practical for older or larger babies.
- Place one arm under the baby’s back, allowing them to rest their body on the forearm. The baby may already be in this position for feeding.
- Carefully turn the baby’s body so that they are resting belly down on the parent’s or caregiver’s forearm with their head in the crook of the elbow.
 Place the hand between the baby’s legs, holding the baby for stability.
Place the hand between the baby’s legs, holding the baby for stability. - Rub or pat the baby’s upper back with the other hand.
- When finished, gently roll the baby toward the body. They will then be face up to continue feeding or to go to sleep.
Method 5: Lap
If the parent or caregiver is already sitting in a chair or on a couch, the lap method may work well to keep the baby asleep. It does not require the baby to be upright, which may be more soothing for them.
- While in a sitting position, gently turn the baby over onto their tummy and allow them to rest on the parent’s or caregiver’s thighs.
- Place one arm under the baby’s chin and chest to raise their upper body slightly.
- Use the other hand to pat their back or rub it in circular motions.
- When finished, turn the baby back over onto their back.
The baby may not always burp during or after feeding. In some cases, this may be because the baby did not swallow much air.
Sometimes, however, it takes a little persistence to get a burp out. Here are some helpful tips for parents and caregivers in these instances:
- Burp the baby during the feed. When a baby has finished feeding, they may be especially drowsy and may have swallowed more air. Try burping them before switching breasts or when they are halfway through their bottle.
- If the baby does not burp after 5 minutes of trying, gently lie them down on their back, either in their crib or on another safe surface, such as a playpen. After a few minutes, carefully pick the baby up and try burping them again. Sometimes, lying down helps move the air bubbles around, making them easier to release.
- Keep the baby upright after their feed. Using a baby wrap or sling can be a good way to let the baby sleep in a semi-upright position, allowing the air bubble to escape without any work from the parent or caregiver.
- There is no need to stress if the baby does not burp. There are times when a baby will not burp or has no air to release.
 If the baby does not burp despite using the methods above, do not worry. One study found that burping does not significantly reduce colic episodes.
If the baby does not burp despite using the methods above, do not worry. One study found that burping does not significantly reduce colic episodes.
The best way to help prevent excess gas in a baby is to try to prevent them from swallowing too much air. Swallowing air is often the result of the baby eating too quickly.
When bottle feeding, follow these tips to help prevent gas:
- Use a slow flow nipple on bottles, especially for newborns. Fast flow nipples may cause the baby to swallow more air.
- Angle the bottle so that air is not getting into the milk or formula while feeding. Doing this usually means tipping the bottle upward at an angle and keeping it tipped as the baby finishes the bottle.
- Test the flow of a bottle’s nipple before giving it to the baby. Tip it upside down and allow a few drops to come out. If the liquid comes out quickly, the nipple may have become worn out.
- Replace bottle nipples if the hole gets bigger, or the nipple shows signs of wear.

When breastfeeding, follow these tips to help prevent gas in the baby:
- Watch for signs of a fast letdown of milk from the breast. If the milk comes out too quickly at the beginning, and the baby is gulping or gasping, take the baby off the breast for a few seconds. Catch the excess milk in a towel or cloth if necessary. Once the milk flow has slowed down, put the baby back on the breast.
- Experiment with different breastfeeding positions. Different babies and women find that certain positions allow them both to breastfeed comfortably. It may help to ask a lactation consultant for tips.
- Make sure that the baby has latched on correctly. The baby’s lips should be sealed and spread out around the nipple. Their lips should not turn inward.
There are ways to burp a sleeping baby without waking them, but no method is foolproof. Parents and caregivers may need to experiment with different burping methods to find which ones work best for them and the baby.
While many babies fall asleep while breastfeeding or bottle feeding, it is important to follow the American Academy of Pediatrics‘ safe sleep guidelines for babies. Following these guidelines may help prevent sudden infant death syndrome (SIDS) and sleep-related infant deaths.
Babies should have regular checkups with a pediatrician to be sure that they are feeding and gaining weight as necessary.
Burping Your Baby (for Parents)
Reviewed by: Madhu Desiraju, MD
Primary Care Pediatrics at Nemours Children's Health
en español Hacer eructar a su bebé
An important part of feeding a baby is burping. Burping helps to get rid of some of the air that babies tend to swallow during feeding. Not being burped often and swallowing too much air can make a baby spit up, or seem cranky or gassy.
How to Burp Your Baby
When burping your baby, repeated gentle patting on your baby's back should do the trick. Cup your hand while patting — this is gentler on the baby than a flat palm.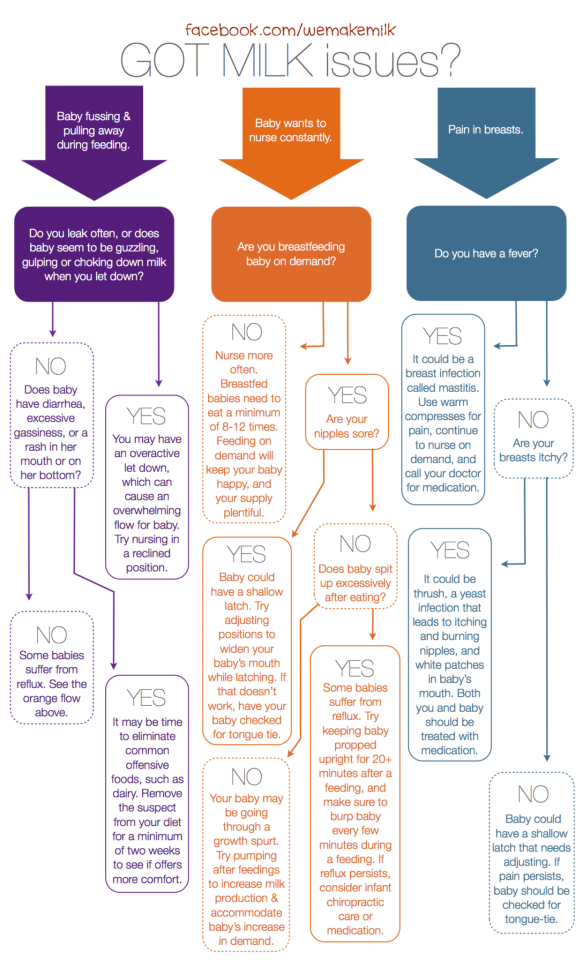
To prevent messy cleanups when your baby spits up or has a "wet burp," you might want to place a towel or bib under your baby's chin or on your shoulder.
Try different positions for burping that are comfortable for you and your baby. Many parents use one of these three methods:
- Sit upright and hold your baby against your chest. Your baby's chin should rest on your shoulder as you support the baby with one hand. With the other hand, gently pat your baby's back. Sitting in a rocking chair and gently rocking with your baby while you do this may also help.
- Hold your baby sitting up, in your lap or across your knee. Support your baby's chest and head with one hand by cradling your baby's chin in the palm of your hand. Rest the heel of your hand on your baby's chest, but be careful to grip your baby's chin, not the throat. Use the other hand to pat your baby's back.
- Lay your baby on your lap on his or her belly.
 Support your baby's head and make sure it's higher than their chest. Gently pat your baby's back.
Support your baby's head and make sure it's higher than their chest. Gently pat your baby's back.
If your baby seems fussy while feeding, stop the session, burp your baby, and then begin feeding again. Try burping your baby every 2 to 3 ounces (60 to 90 milliliters) if you bottle-feed and each time you switch breasts if you breastfeed.
Try burping your baby every ounce during bottle-feeding or every 5 minutes during breastfeeding if your baby:
- tends to be gassy
- spits a lot
- has gastroesophageal reflux (GER)
- seems fussy during feeding
If your baby doesn't burp after a few minutes, change the baby's position and try burping for another few minutes before feeding again. Always burp your baby when feeding time is over.
To help prevent the milk from coming back up, keep your baby upright after feeding for 10 to 15 minutes, or longer if your baby spits up or has GERD. But don't worry if your baby spits sometimes. It's probably more unpleasant for you than it is for your baby.
It's probably more unpleasant for you than it is for your baby.
Sometimes your baby may awaken because of gas. Picking your little one up to burp might put them back to sleep. As your baby gets older, don't worry if your child doesn't burp during or after every feeding. Usually, it means that your baby has learned to eat without swallowing too much air.
Babies with colic (3 or more hours a day of continued crying) might have gas from swallowing too much air during crying spells, which can make the baby even more uncomfortable. Check with your pediatrician before giving your baby anti-gas drops.
Reviewed by: Madhu Desiraju, MD
Date reviewed: June 2022
How to help the baby when regulating
Support icon ofKeywords for searching
Home ›!! How to help a child in sprinkling
Home Home ›!! How to help a child in regurgitation
↑ Verki
Breastal feeding - completely special time for mom and her newborn baby. Together with the feeling of closeness and affection that feeding brings, understanding its nuances cannot but raise many questions, including the question of how to help an infant spit up. Regurgitation in a newborn is by no means always the result of a simple pat on his back. nine0015
Together with the feeling of closeness and affection that feeding brings, understanding its nuances cannot but raise many questions, including the question of how to help an infant spit up. Regurgitation in a newborn is by no means always the result of a simple pat on his back. nine0015
In this article, we'll talk about the basics of helping a newborn spit up, as well as other questions you may have about spitting up.
Why do babies spit up?
Let's get it straight: why do newborns need to burp in the first place? During feeding, children usually swallow extra air - this is called aerophagia. Spitting up helps prevent this air from entering the intestines, as well as vomiting, gas, and crankiness in the baby. To avoid the return of milk after feeding, you should give the baby the opportunity to burp more often. nine0003
How to help a newborn spit up?
During the first six months, the baby should be kept upright in a column for 10-15 minutes after each feed. This will help keep the milk in his stomach, but if the baby occasionally burps anyway, parents need not worry. While carrying your baby in an upright position, you can put a baby diaper or wipes on your shoulder to keep your clothes clean.
This will help keep the milk in his stomach, but if the baby occasionally burps anyway, parents need not worry. While carrying your baby in an upright position, you can put a baby diaper or wipes on your shoulder to keep your clothes clean.
We've already seen why spitting up is important, now let's find out how to help your baby spit up. Parents should gently pat the baby on the back with a hand folded in a handful until he burps. Folding your hand into a handful is important because clapping with a flat palm may be too strong for an infant.
Every baby is different and there is no one right position for spitting up. To get started, you can try the following options:
- Sitting position with the baby on the chest. In this position, the parent puts the baby's head with his chin on his shoulder and with one hand supports the baby under the back. With the other hand, you can gently pat the baby on the back. This method is most effective in a rocking chair or when the baby is gently rocking.
 nine0044
nine0044 - Holding the child upright on your legs. With one hand, parents can hold the baby by the back and head, supporting his chin and placing his palm on the baby’s chest, with the other hand, you can gently pat him on the back. At the same time, it is important to be careful: do not press the child on the throat, but only gently support his chin.
- Holding a baby on your lap while lying on your tummy. Make sure his head is above his chest and gently pat your baby on the back until he burps. nine0015
Here are some tips on how best to help your newborn spit up:
- Let your baby spit up during feeding. If the baby is restless or has swallowed air, it is worth giving him the opportunity to burp during feeding, and not just after.
- When bottle feeding, let the newborn burp after every 50-60 ml.
- When breastfeeding, let the baby burp at every breast change. nine0015
It is important to let your baby spit up after eating, even if he spit up during feeding!
If your baby is gassy, spit up more often. Also, if he vomits frequently or suffers from gastroesophageal reflux disease (GERD), have him spit up after every 30 ml bottle-feeding or every five minutes while breastfeeding.
Also, if he vomits frequently or suffers from gastroesophageal reflux disease (GERD), have him spit up after every 30 ml bottle-feeding or every five minutes while breastfeeding.
How long should a baby be held for it to burp? It's different for everyone, but generally keeping a newborn upright for 15 to 20 minutes after a feed helps the milk stay in the baby's stomach. nine0003
Minimize the amount of air you swallow. Gas production and regurgitation result from aerophagia during feeding. The baby will inevitably swallow air, but there are ways to prevent it from swallowing too much. Whether you bottle feed your baby or combine breastfeeding with bottle feeding, the Philips Avent anti-colic bottle with AirFree valve is designed so that the nipple is always filled with milk without excess air, even in a horizontal position, thus preventing the baby from swallowing excess air during feeding. nine0015
Reducing the amount of air your baby swallows can help reduce your baby's risk of colic, gas, and spitting up.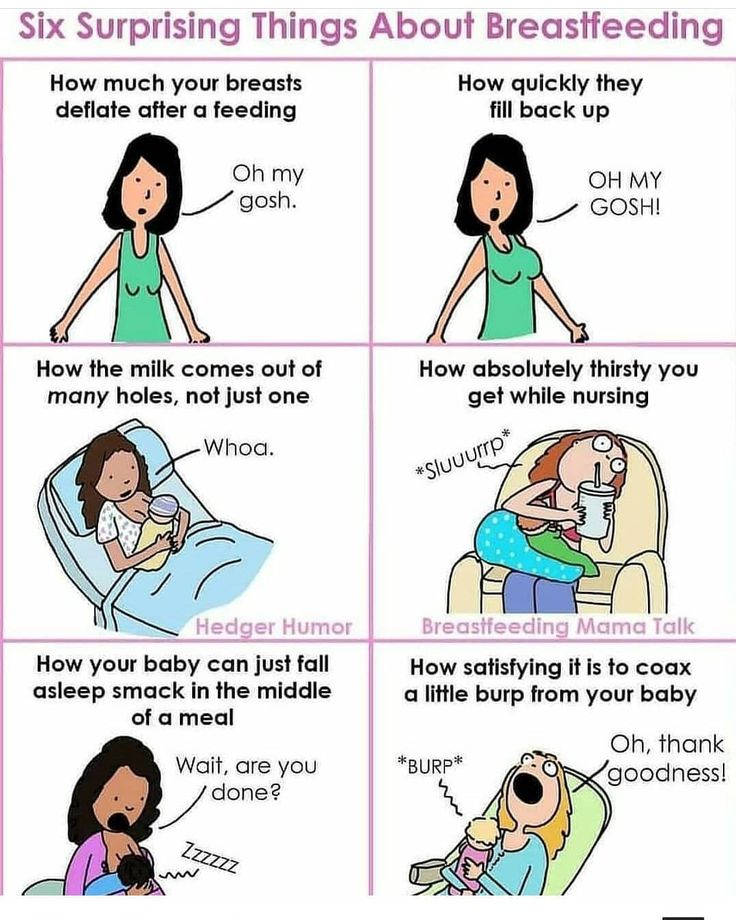
Breastfeeding is a wonderful time to strengthen the bond between parent and baby. Every mom and every baby is different, so learning to help your newborn burp properly can take time and practice.
Articles and tips from Philips Avent
Baby+ app
Download the app and track your child's development and growth with trackers, and keep those special moments forever.
Download app:
You are leaving the Philips Healthcare (“Philips”) official website. Any links to third party websites that may be included on this site are provided solely as a convenience to you. Philips makes no warranties regarding any third party websites or the information they contain. nine0003
I understand
You are about to visit a Philips global content page
Continue
You are about to visit the Philips USA website.
I understand
Infant Reflux: Symptoms and Treatment
Search Support IconSearch Keywords
Home ›› What is Reflux in Infants?
Home ›› What is reflux in babies?
↑ Top
Signs and what to do
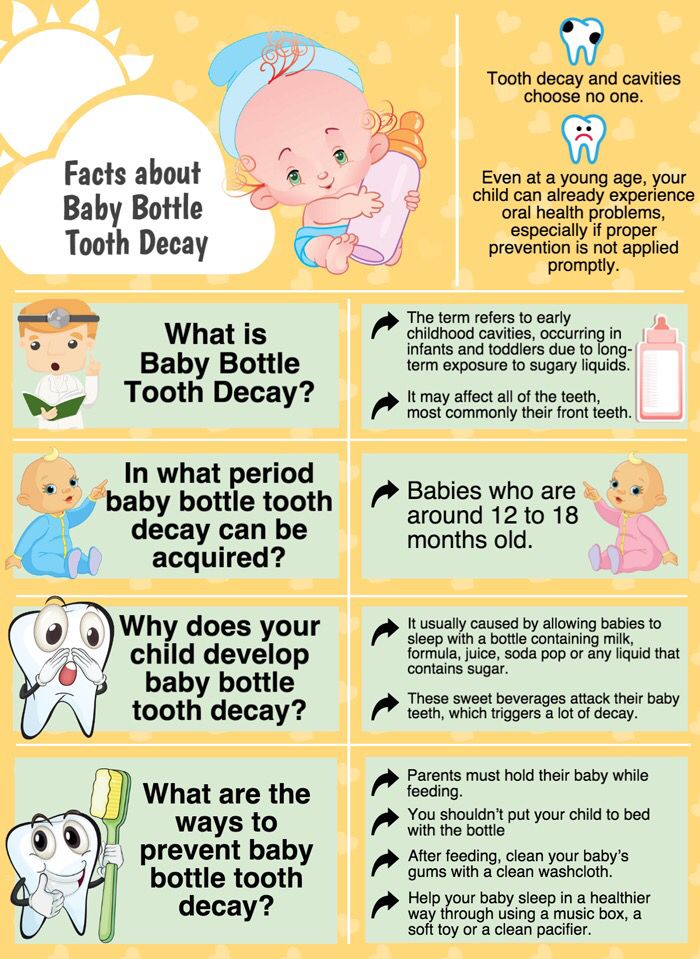
Post-feed spitting up is common in the first few months of life. This is usually harmless and completely normal, but parents should read about gastroesophageal reflux (GER) and laryngopharyngeal reflux (LPR) in infants and how long it lasts to give them peace of mind.
This is usually harmless and completely normal, but parents should read about gastroesophageal reflux (GER) and laryngopharyngeal reflux (LPR) in infants and how long it lasts to give them peace of mind.
We look at signs of reflux in babies, symptoms of different types of reflux, and how to help a child with signs of reflux. If you require further information, always contact your healthcare provider. nine0003
What is reflux in babies?
So we know reflux is common, but what causes reflux in babies? Because young children have not yet fully developed the lower esophageal sphincter (LES), that is, the muscle at the bottom of the esophagus that opens and closes to let food into the stomach and keep it there, food can easily pass back up the esophagus.
Acid reflux, also known as gastroesophageal reflux (GER), is a normal reflux that occurs in babies. This type of reflux is considered normal and occurs in 40-65% of babies. nine0003
How do I know if my child has acid (gastroesophageal) reflux?
If a baby is spitting up milk after a feed, it is most likely acid reflux. As babies get older, GER usually goes away on its own without any intervention. If a baby has complications beyond just spitting up a small amount of milk (such as feeding difficulties and discomfort), they may have gastroesophageal reflux disease (GERD). nine0015
As babies get older, GER usually goes away on its own without any intervention. If a baby has complications beyond just spitting up a small amount of milk (such as feeding difficulties and discomfort), they may have gastroesophageal reflux disease (GERD). nine0015
Symptoms of GERD include:
- baby arching during or after feeding;
- crying more than three hours a day for no apparent reason;
- cough;
- gag reflex or difficulty swallowing;
- irritability, restlessness after eating;
- eating little or not eating;
- poor weight gain or loss;
- difficult breathing;
- severe or frequent vomiting. nine0015
GERD usually occurs when the muscle tone of the LES muscles fails in time, causing stomach contents to back up into the esophagus.
How do I know if my child has Laryngopharyngeal Reflux?
Another type of reflux, laryngopharyngeal reflux (LPR), also called silent reflux, is when the contents of a child's stomach leak back into the larynx, the back of the nasopharynx. This type of reflux does not always cause external symptoms, which is why it is called "silent". Babies can have GERD and silent reflux at the same time, but their symptoms are somewhat different. nine0015
This type of reflux does not always cause external symptoms, which is why it is called "silent". Babies can have GERD and silent reflux at the same time, but their symptoms are somewhat different. nine0015
The following are some of the symptoms of laryngopharyngeal reflux:
- trouble breathing;
- gag reflex;
- chronic cough;
- swallowing problems;
- hoarseness;
- regurgitation;
- poor weight gain or weight loss.
We have looked at the signs of reflux in infants, now we will move on to the treatment and duration of silent reflux in children, as well as the treatment of GERD. nine0003
How to deal with laryngopharyngeal reflux in babies while breastfeeding?
Breastfeeding mothers may need to review their diet if their babies show signs of reflux. The American Academy of Pediatrics (AAP) recommends breastfeeding mothers cut eggs and milk from their diet for two to four weeks to see if their baby's reflux symptoms improve or disappear. It may be worth eliminating acidic foods from your diet. nine0015
It may be worth eliminating acidic foods from your diet. nine0015
In most cases, GER and laryngopharyngeal reflux go away on their own. Typically, children outgrow reflux in the first year of life. If a child has persistent symptoms of laryngopharyngeal reflux, parents should consult a doctor. If your baby has severe vomiting, blood in the stool, or any of the symptoms of GERD listed above, parents should contact their pediatrician as soon as possible.
How can I help my child with reflux or GERD? nine0008
Reflux symptoms in babies usually go away on their own, but the following tips can help relieve symptoms:
- Thicken your food with rice or a special milk thickener.
- Hold the bottle at an angle that fills the nipple completely with milk to reduce the amount of air your baby swallows. This can help prevent colic, gas, and reflux.
- Try the AirFree anti-colic bottle, designed to reduce air swallowing during feeding.
 nine0044
nine0044
4. Let your baby burp during and after feeding. If the baby is bottle fed, parents can let him burp after every 30-60 ml. If the mother is breastfeeding, she may let the baby burp when changing breasts.
5. Hold baby upright after feeding. As a rule, in order for the milk to remain in the stomach, after feeding the baby, it is necessary to hold it in an upright position for 10-15 minutes. But, if the child has reflux, parents should keep him upright a little longer. nine0003
These tips may help relieve symptoms, but they do not replace a doctor's advice.
Parents should not change their infant formula without first talking to their doctor.
Don't panic! Reflux is very common in babies during the first three months of life, and most babies outgrow it without any consequences. Although GERD is a slightly more serious condition, there are many treatments, ways to manage it, and help newborns. Feel free to contact your doctor with any questions or concerns you may have.