Baby clicking noise when bottle feeding
Why does my baby click when they eat? — Mattos Lactation
Read time | 10 minutes
When I wrote on the causes of clicking during breastfeeding last year, I had no idea that it would quickly move to the first page of google.
I knew hearing clicking noises during feeding was a common occurrence for parents, but I couldn't have imagined that a short, poorly written post would become my highest performing post to date, with over 3,050 views since posting.
While my understanding of clicking during infant feeding hasn't changed much, my ability and desire to create easy to understand, in-depth blog posts has increased.
Therefore, I want to tackle this topic again, but in a manner that is true to me, resulting in an article that I don't shake my head and wonder, "Shondra, what were you thinking to post this unhelpful, pointless trash?"
What is Clicking?
In this context, clicking describes a short, sharp sound created from a baby's mouth. It sounds similar to a "tsk tsk" sound one makes if they're demonstrating disapproval (or "tut-tut" for my UK folks), though some might better relate to the ICONIC tongue popping sound popularized by the queen Alissa Edwards.
When it comes to baby, the clicking sound isn't as sharp or consistent as tongue pops made by adults, but once you're familiar with the general sound, identifying clicking variations during infant feeding becomes easy.
What causes clicking?
Clicking is caused whenever there is a loss of suction. This can happen both at the breast or on the bottle, and may or may not be seen in conjunction with more obvious signs of "breaking the seal" such as leaking.
How the clicking noises sound- sharp and bright or muffled- can depend on which part of the tongue loses suction, which also explains why for some, milk spilling from the baby's mouth accompanies the clicking, and for others, there's just the sound.
Note: There can be leaking without clicking too, which also provides useful information for troubleshooting feeding difficulties.
Is clicking a problem?
Though I would argue that clicking sounds aren't normal, I wouldn't say it's always a problem.
For example, if your baby makes the occasional clicking noise or if it's during a time of intense breast fullness, there's generally nothing to worry about.
Consistent clicking during feeding, however, especially in conjunction with other signs of feeding difficulties, such as nipple pain, slow weight gain, coughing, choking, gasping, panting, unlatching, grimacing, should be evaluated, even if it occurs during bottle-feeding.
Why is my baby making clicking noises?
There are many reasons possible causes for clicking.
Poor positioning/latch
A strong, forceful letdown
Engorgement
Poor tongue mobility/function (Such as tongue tie)
A weakness of the tongue
Inability to maintain a seal due to weak muscles or restricted lip (lip tie)
Body tension or physical limitations such as Torticollis
Hard Palate abnormalities
Submucosal cleft
Ear Infections
Thrush
Let's take a look at each case separately.
Poor latch & positioning
Oft, the phrases latch & position are used synonymously. Still, they describe two distinct steps- the latch refers to how your baby's mouth attaches to the breast or bottle and position relates to your baby's physical arrangement and orientation in space and in regards to the feeding parent.
To make it easy
Latch = mouth. Position = body. Latch =/= position.
A baby's position can, and often does, affect how effectively a baby latches and how well they can transfer milk ( a whole different & distinct step of feeding!)
An issue with the latch OR the position can cause clicking in some babies, in which case, mastering the latching technique and finding the right feeding position to support your baby's feeding ability may be all that's needed to achieve quiet feeding.
The act of mastering latching is many times easier said than done. Even after reading this excellent FREE 24-page latching guide, some parents will need additional latching support and troubleshooting.
Even after reading this excellent FREE 24-page latching guide, some parents will need additional latching support and troubleshooting.
Luckily, even if you live in an area short on IBCLC's, there are often many experienced lactation professionals who can help with latching basics and refer when necessary if tailored latching help doesn't resolve the issue.
A strong, forceful letdown
Just as some are "blessed" (or "cursed" depending on who you ask) with very robust milk supplies, some are "blessed" with an extraordinary rate of milk flow.
Though forceful letdowns & oversupply often go hand and hand, forceful letdowns (Overactive Milk Ejection Reflex [MER]) can happen in those with "typical" milk supplies. However, the underlying cause may be different. For example, full breasts often accompany oversupply, which may result in a forceful letdown due to the pressure build-up inside the mammary glands. The first letdown, and even the second, may be mighty as the breast releases the milk with a force that rivals Niagra Falls.
With Overactive MER, rather than the force stemming from milk volume, the power is due to an overachiever reaction on the part of the pituitary gland( which sends out the hormone that tells the 'milk sacs' to contract and send the milk out the breast).
As you may imagine, regardless of the cause, your baby can easily become overwhelmed with the rate of milk and release tongue suction to allow milk to spill from the sides of their mouth so they can breathe.
If the flow rate is the cause of the clicking, strategies tailored for managing overactive letdowns, along with more upright & laidback feeding positions, should resolve the clicking.
Engorgement
This cause is pretty simple: Full, taut breasts are hard to grasp on to, so during periods of intense engorgement or fullness, clicking may occur.
Resolve the swelling or reduce breast fullness, and the clicking should stop.
Poor tongue mobility/function (Such as tongue tie)
Poor tongue function is NOT always caused by tongue-tie, however, tongue-tie often causes poor tongue function thus impacting its range of motion (mobility).
There are many stages of the feeding and swallowing process, and a limited function of the tongue can impact each of the required steps.
The clicking sound associated with poor oral function due to tongue-tie can be broken down to this straightforward overview-
A tight frenulum doesn't allow your baby's tongue to raise to the proper placement for easy feeding OR the effort it takes your baby to overcome the resistance of a tight frenulum is such that they quickly get tired and start to lose suction.
Reduced tongue mobility is the most common cause of persistent clicking I see. There is such a strong association with clicking and tongue ties, that clicking alone is enough to prompt a tie suspicion even in the absence of "typical tongue-tie appearance."
A weakness of the tongue
The tongue is a group of muscles, and with any muscles, it can be or become weak. Weakness may be a byproduct, which is commonly seen with tongue-tie and explains the need for tongue strengthening exercises pre and post revision, but can be a stand-alone cause of clicking.
It takes an experienced and highly trained professional (such as IBCLCs who specialize in supporting tied babies) to be able to differentiate between limited tongue function caused by weakness vs. reduced tongue mobility caused by ties.
Inability to maintain a seal due to weak muscles or restricted lip (lip tie)
There is a profound link between tongue mobility and many other structures of the body (see below), to include the lips and surrounding oral muscles. Any weakness or limitation of any oral anatomy has the potential to impact tongue function.
Body tension or physical limitations such as Torticollis
See above. Insert body tension/physical limitation in place of muscle weakness/lip tie.
Hard palate abnormalities
The hard palate is the bony part of the roof of the mouth. We expect the palate to be intact with a gradual slope.
Sometimes there are abnormalities in the palate, be it due to congenital defects (such as cleft palates) or due to abnormal development caused by a lack of appropriate palate pressure in utero (ex: bubble palates).
During breastfeeding and bottle-feeding, the palate provides a platform for stabilizing the breast/teat in the oral cavity. Palatal abnormalities can impact stability, and clicking can result.
Submucosal clefts/ Velopharyngeal insufficiency (VPI)
Generally speaking, clicking sounds often come from the anterior portion of the mouth, and some may argue that clicking doesn't occur with submucosal clefts or VPI.
I wanted to add this category because how parents and providers interpret clicking is subjective. And because clicking noises already vary in sound and intensity, I don't think it's too much of a stretch to include sounds that may be loosely considered clicking.
Milk leaking from the nose during feeding is a classic symptom of submucosal clefts/VPI and will always require a referral for further evaluation. However, sometimes a soft puffy "clicking-esque" noise may be present due to loss of suction of the soft tissues near the throat and would also warrant a referral.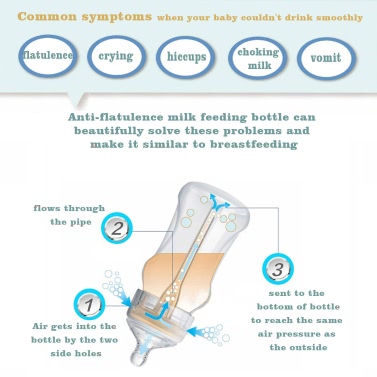
Ear Infections/ Thrush
Thrush & ear infections both can change the way your baby eats, and temporary clicking may occur. Once the thrush or ear infection resolves or the pain disappears, the clicking noises should stop as well.
I'll admit, I'm biased, but ff your baby suddenly starts to click and around the same time, you notice you're having some breast pain, it would be good practice to schedule a lactation consultation. During the consult, we will assess what's causing the pain and develop a care plan to reduce the discomfort.
As you may see, there are a lot of possibilities for your baby’s clicking. In many cases, when clicking persists despite position changes and after engorgement passes, the clicking is due to something structural.
I often find myself asking if there’s any clicking present during feeding when parents complain of pain, slow weight gain/weight loss (baby), and low supply.
The reason?
Babies need a proper seal to maintain vacuum pressure to transfer milk effectively and efficiently.
Many times parents are told that clicking is typical, or that there are no issues with their baby’s noisy eating, even though they sound similar to the baby below.
The baby in this clip is NOT feeding efficiently at all. Continued poor feeding is often very stressful for babies (and parents) and can lead to long term feeding aversions. Clicking may be the only noticeable sign of dysfunctional feeding, especially when babies are gaining weight or having appropriate diaper output.
If your baby is making clicking noises that persists or if they leak, gulp, gasp, pant, pop off or grimace and fuss while feeding (bottle or breast), please download this DIY Oral Assessment worksheet.
Once completed, you will have a better understanding of your baby’s oral strengths and weaknesses. The sooner we find solutions to make feeding easier for your baby, the better. You can book an appointment here.
The sooner we find solutions to make feeding easier for your baby, the better. You can book an appointment here.
You may also like:
Shondra MattosComment
0 LikesBaby Clicking While Bottle Feeding? Reasons & How to Fix It
Babies make a wide range of noises which they use to communicate with their caregivers long before they produce their first word. Aside from the typical sounds such as crying, cooing, and gurgling, babies are also capable of making sounds while they feed, to indicate contentment, discomfort, and even difficulty feeding.
A clicking sound while bottle feeding usually indicates a loss of suction and/or repeated attempts to get a good latch on the bottle nipple. If you notice your baby making clicking sounds while drinking from a bottle, the quickest fix is just to take the bottle out of their mouth, reposition it, and try again.
There are a few reasons why your baby might make a clicking sound while feeding, such as an improper or shallow latch, incorrect nipple size, teething, and even an ear infection. Once you figure out the underlying reason for the clicking, you can work on fixing the problem and getting a good experience out of bottle-feeding your baby.
What Makes the Clicking Sound?
Just like with breastfeeding, bottle-fed babies need to get a good latch on the silicone nipple to feed properly. A clicking sound might occur when your baby isn’t able to suck on the bottle nipple properly, and ends up sucking on their tongue or cheeks instead.
The clicking is produced similarly to the “tsk tsk” sound you might make to express distaste, although it might not be as loud or clear as an adult would make it.
While hearing your baby clicking while feeding can be concerning, it is not always a bad sound to hear.
While consistent clicking with every feed is a concern that suggests a feeding issue that needs to be addressed quickly, the odd click here and there while feeding isn’t necessarily something to worry about, provided that your baby is otherwise healthy, feeding well, and gaining weight.
Reasons Why You Hear A Clicking Sound While Bottle Feeding
Poor Latching
A good latch on the bottle nipple is just as important as a good latch on a human nipple. The techniques for getting a good latch on a bottle nipple are fairly simple and similar to the techniques used for a breastfeeding latch.
Use the tip of the bottle nipple to tickle your baby’s lip and nose. This will stimulate their rooting reflex and get them to open their mouth wide. Insert the nipple with the bottle angled up towards their hard palate.
Check to see that the nipple is positioned over and not under the tongue. The protruding tip should be entirely inside their mouth. Gently push their lower lip upwards to help them seal their lips around the nipple until they latch on completely.
Body and Bottle Position
The wrong body posture can make it hard for your baby to maintain a proper latch on a bottle nipple. Hold your baby to your chest at a 45-degree angle and hold the bottle horizontally with a very slight tilt. An angled baby bottle may also be more ergonomic and allow for a better latch with upright feeding.
An angled baby bottle may also be more ergonomic and allow for a better latch with upright feeding.
It is also important that you keep a comfortable position while holding the bottle for your baby. You can use a nursing pillow to prop your baby up and reduce the amount of work your arms need to do to support them.
Nipple Flow Rate
As you may know, bottle nipples come with different sizes or numbers of holes, to allow for different levels of milk flow. Using a nipple with too high or low of a flow rate can make it difficult for your baby to feed properly and cause them to click.
Signs of a nipple flow rate being too high include milk leaking out from the sides of your baby’s mouth, gulping, coughing, gasping, or sputtering while feeding, and finishing bottles very quickly (in less than five minutes). Your baby may also struggle to swallow in between sucks when milk is coming into their mouth too quickly.
Signs of a nipple flow rate being too low include flattened or collapsed nipples from your baby sucking too hard, taking more than half an hour to finish feeding, and eating less and getting hungry quickly after feeding. A too slow flow rate may also cause your baby show signs of frustration by crying, squirming, or pulling away from the bottle.
A too slow flow rate may also cause your baby show signs of frustration by crying, squirming, or pulling away from the bottle.
Generally, you’ll want to start with the slowest flow rate available for that particular nipple and move up as needed. There are also recommendations for nipple flow rates by age, as can be seen here.
Incorrect Nipple Shape
If the nipple tip is too long or too large, your baby may gag on it or push it out of their mouth to avoid gagging. Gagging, grimacing, shallow latching, and clicking may mean that the nipple is too long for them and you may need to switch to a shorter or smaller nipple.
The shape of the bottle nipple matters too. With a breastfed baby, you want to choose a bottle nipple with a gradual slope and narrower base that will allow your baby to take all of or most of the silicone portion of the nipple into their mouth and seal their lips close to the O-ring collar, much like they would with a deep breastfeeding latch.
With bottle nipples with a narrow tip and a suddenly wide base, your baby may end up sucking on the tip like a straw. Dimpled or hollow cheeks are usually a sign of straw drinking. They may also try to take the base into their mouth, creating an air pocket that will prevent a proper seal from forming and cause them to swallow more air while feeding.
Dimpled or hollow cheeks are usually a sign of straw drinking. They may also try to take the base into their mouth, creating an air pocket that will prevent a proper seal from forming and cause them to swallow more air while feeding.
Nipple Tip Shapes
Generally speaking, bottle nipples that bear a similar rounded bulb shape to a human nipple are best for breastfed or combination-fed babies. You want your baby to maintain the same oral posture at the bottle as they do at the breast. This helps prevent nipple confusion and potential pain or damage to your nipple later on.
Orthodontic nipples that are flat on one side and rounded on the other (like lipstick) are designed to prevent teeth misalignment and malocclusion. The rounded side rests against your baby’s palate, while the flatter bottom and tapered sides put less pressure on your baby’s teeth and jaw.
Orthodontic nipples may also be easier on a teething baby’s gums and a pediatric dentist may recommend switching to one once your baby begins teething. If you think your baby’s clicking is related to teething soreness, ask a pediatrician or a dentist about using an orthodontic nipple.
If you think your baby’s clicking is related to teething soreness, ask a pediatrician or a dentist about using an orthodontic nipple.
Teething
Your baby may be using the bottle nipple like a teether, chewing on it to massage their gums instead of sucking on it to draw milk out. Help relieve the soreness in their gums before a feed by offering a cold teether for a few minutes before you bring out the bottle.
Tongue and Lip Ties
Tongue ties are caused by a shortened lingual frenulum, aka the bit of tissue that anchors your tongue to the floor of your mouth. Lip ties are similar – the labial frenulum, which connects the underside of your upper lip to your gumline is abnormally shortened.
Tongue ties and lip ties limit the range of motion of the oral structures that would normally assist in sucking and swallowing. Clicking sounds while feeding is a common symptom of tongue and lip ties.
A frenectomy is usually done to release tongue ties and lip ties. Using scissors or a laser, a surgeon cuts and modifies the tissue to allow the affected structure, in this case, the tongue or the lip, to move normally. The procedure is typically performed under local anesthesia and causes little to no pain or discomfort. Babies can feed immediately following the procedure.
Using scissors or a laser, a surgeon cuts and modifies the tissue to allow the affected structure, in this case, the tongue or the lip, to move normally. The procedure is typically performed under local anesthesia and causes little to no pain or discomfort. Babies can feed immediately following the procedure.
Temporary Illness
Some mild illnesses and infections can cause your baby to change the way they feed, causing them to click. Clicking that occurs while your baby is sick will most likely resolve once they get better.
Congestion
If your baby has a cold and is congested, they will need to break the seal to breathe through their mouth every few sucks.
Using a rubber bulb syringe or nasal aspirator can help clear the mucus from their nasal passages and allow them to breathe through their nose while feeding. Saline nasal drops can also help loosen the mucus and make it easier for them to breathe through their nose.
Ear Infections
Sucking and swallowing can cause pressure changes in the middle ear that may exacerbate ear infection pain. When a baby has an ear infection, they may change the way they latch on to a bottle to make themselves more comfortable. They may also repeatedly break the seal as a way to relieve pressure.
When a baby has an ear infection, they may change the way they latch on to a bottle to make themselves more comfortable. They may also repeatedly break the seal as a way to relieve pressure.
Thrush
While oral thrush is easily treatable and rarely serious, it does cause itching and soreness in your baby’s mouth, which may cause your baby to click and break the seal around the nipple.
Cleft Lip or Palate
Often, babies with a cleft lip only (no palate involvement) can feed well enough with normal breastfeeding or bottle-feeding. There are also bottle nipples shaped to help babies with clefts eat properly.
A cleft palate, on the other hand, opens up the division between the oral and nasal cavity, making it difficult for babies to create the pressure vacuum that allows them to suck. It can also interfere with the normal function of the muscles that facilitate swallowing at the back of the mouth.
Some types of cleft palate are not always visible. Submucosal cleft palates are covered by a layer of mucosa (tissue) and may be missed during a newborn oral exam. There are, however, common signs of submucosal clefts, such as a bifid (split) uvula, and a pale bluish tint along the roof of the mouth.
There are, however, common signs of submucosal clefts, such as a bifid (split) uvula, and a pale bluish tint along the roof of the mouth.
A speech-language pathologist that specializes in pediatric feeding may be able to help you find techniques that can help your baby feed well. Clefts that are diagnosed at birth are usually repaired through surgery within the first 18 months of life.
Baby won't take the bottle | Philips Avent
search support iconSearch Keywords
Home ›› What to do when your baby refuses a bottle
↑ top
any problems. If your breastfed baby refuses a bottle, don't worry. This is a common occurrence in many babies who are used to breastfeeding. Obviously, this can create certain difficulties for moms, especially if you need to return to work in the near future.
3 Philips Avent products to help you bottle feed:
So why is your baby refusing to bottle and crying? There are many ways to quickly and easily teach a breastfed baby to a bottle. Here are important tips on what to do when your baby refuses a bottle.
Here are important tips on what to do when your baby refuses a bottle.
Is the baby refusing the bottle? Take a step back
If your baby cries while bottle feeding, the first thing to do is to start over and rethink your feeding approach and technique. Try the following steps when bottle feeding your baby: [1]
- Lift and tilt your baby's head forward. Before inserting the pacifier into the baby's mouth, make sure that the baby's head is raised and tilted over his body to avoid choking: so that the baby does not choke and have the opportunity to burp during bottle feeding.
- Insert the pacifier. Bring the pacifier to the baby's lips and gently guide it into the baby's mouth. In no case do not try to press the nipple on the baby's lips and try to push it into his mouth. After touching the pacifier to the baby's lips, wait for the baby to open his mouth and take the pacifier.
- Hold the bottle at an angle. Tilt the bottle at an angle so that the nipple is only half full.
 So the child can eat at his own pace.
So the child can eat at his own pace. - Let the baby burp during and after feeding. It can be useful for a child to burp not only after feeding, but also approximately in the middle of the process. This will help reduce gas or tummy discomfort that your baby may experience from swallowing too much air.
- Stop in time, do not overfeed the baby. If the baby begins to turn his head away from the bottle or closes his mouth, then he is full and you need to stop feeding.
- Perhaps the flow of milk from the nipple to the baby is weak or, on the contrary, too fast, so he is naughty and refuses the bottle. Try changing the nipple to a nipple with a different flow.
Other tips if your baby refuses the bottle
If you've followed the steps above and your baby still refuses the bottle, don't worry. There are other ways to help bottle feed your baby. Here are some simple tricks you can add to your bottle feeding process. [2]
1. Remind your child about mom.
Remind your child about mom.
Sometimes a child can be fed by someone other than his mother - dad, grandmother or, for example, a nanny. If your baby fusses while bottle feeding, try wrapping the bottle in something that smells like mommy, like a piece of clothing or some fabric. This will make it easier to feed the baby when the mother is not around.
2. Try to maintain skin contact while bottle feeding.
Some babies need contact with their mother, so try bottle feeding while leaning against you. However, some babies are better at bottle feeding when they are in the exact opposite position than when they are breastfed. For example, there is a position with bent legs. Lay the child on your bent knees, facing you, pointing the child's legs towards your stomach. During feeding, the baby will be able to look at you and contact you in this way. If your baby refuses a bottle, experiment to see which works best.
3.![]() Move while feeding.
Move while feeding.
Sometimes all it takes to get your baby to take the bottle is a little wiggle or walk. The next time your baby starts crying while bottle feeding, try moving around a little rhythmically to calm him down.
4. Try changing the milk temperature.
If the baby still does not want to take the bottle, check if the milk in the bottle is too hot or too cold. Before feeding, put some warm breast milk on the inside of your wrist to check the temperature. Milk should be warm, but if it seemed hot to you, just place the bottle for a short while under a stream of cold water.
Choosing the right bottle for your baby If you plan to combine bottle feeding with breastfeeding, it is advisable to choose bottles with a nipple that will have a wide base as the bottle will grip closer to the breast. Also pay attention to the fact that the nipple is firm and flexible, the child must make an effort to drink from the bottle, as well as from the breast.
 Give preference to nipples with an anti-colic valve that vents air out of the bottle.
Give preference to nipples with an anti-colic valve that vents air out of the bottle. Natural bottle allows you to combine breast and bottle feeding. 83.3% of babies switch from a Natural bottle to breastfeeding and back.*
If you choose a bottle for artificial feeding, traditional bottles are fine, but it is desirable that the nipple is made of a hypoallergenic material, such as silicone, has an anti-colic valve and did not stick together when bottle fed. In case your baby spit up often, then use special bottles with anti-colic and anti-reflux valve, which reduces the risk of spitting up and colic.
Bottle with unique AirFree valve reduces the risk of colic, gas and spitting up. With this bottle, you can feed your baby in an upright or semi-upright position to reduce spitting up. Due to the fact that the nipple is filled with milk and not air during feeding, the baby does not swallow air, which means that feeding will be more comfortable.
Both bottles are indispensable if you want to breastfeed, bottle feed or just bottle feed your baby.
“My baby refuses to breastfeed but bottle feeds – help!”
Sometimes a baby gets used to bottle feeding and refuses to breastfeed. Therefore, it is important to use bottles that are suitable for combining breastfeeding with bottle feeding. If, nevertheless, you are faced with the fact that the child refuses to take the breast, try using silicone nipple covers to make the transition from the bottle to the breast and back more imperceptible.
Remember that if you want to combine breastfeeding and bottle feeding, it is worth waiting at least a month before offering a bottle, so that you are lactating and have time to get used to each other and develop a breastfeeding regimen.
Breastfeed and bottle feed your baby with pleasure
Remember that it takes a while for your baby to get used to bottle feeding. This is completely normal. If you have to go to work, be sure to set aside enough time to bottle train your baby beforehand.
Remember that every child is different, so what works for one may not work for another. With a little time and patience, you will find out what works best for your baby when he refuses a bottle.
You will identify your child's unique needs. However, if your baby still refuses the bottle after all the steps above, check with your pediatrician.
Articles and tips from Philips Avent
References:
*O.L. Lukoyanova, T.E. Borovik, I.A. Belyaeva, G.V. Yatsyk; NTsZD RAMS; 1st Moscow State Medical University THEM. Sechenova, "The use of modern technological methods to maintain successful breastfeeding", RF, 10/02/2012 3 llli.org - The Baby Who Doesn't Nurse
llli.org - Introducing a Bottle to a Breastfed Baby
Baby+ app
Download the app and track your child's development and growth with trackers and save those special moments forever.
Download app:
You are leaving the Philips Healthcare (“Philips”) official website. Any links to third party websites that may be included on this site are provided solely as a convenience to you. Philips makes no warranties regarding any third party websites or the information they contain.
Any links to third party websites that may be included on this site are provided solely as a convenience to you. Philips makes no warranties regarding any third party websites or the information they contain.
I understand
You are about to visit a Philips global content page
Continue
You are about to visit the Philips USA website.
I understand
Separation in the maternity hospital: what to do if the baby is taken from a mother with covid after childbirth
History fourth of October in Moscow. The day before, upon admission to the maternity hospital, I passed a rapid test for COVID-19- this is now a mandatory order for all incoming women in labor. There were no antibody tests in the hospital.
Childbirth was paid, under a special contract with the maternity hospital. Everything went well, the day after the birth, the mother and child were in the same room. The next morning, a team of Rospotrebnadzor in protective suits entered the ward with the words:
The next morning, a team of Rospotrebnadzor in protective suits entered the ward with the words:
- Bad news: you have a positive test. The child is a contact child, we pick him up. We are transferring you to the isolation ward for now, then to the infectious disease ward. And the child - in the children's infectious, in the covid department.
Olga was not asked to sign any informed consent. It was difficult to argue with a group of people in special suits, and there was no time for disputes: now the main thing is the daughter's health.
Olga felt quite healthy, she had no symptoms of SARS. When she offered to retake the test, in response she heard the phrase: "There are no false positive tests."
Olga spent the hour allotted for getting ready to call the Ministry of Health, Rospotrebnadzor, the Moscow COVID-19 hotline. The calls did not bring results - the operators, at best, resent to each other.
Olga, as requested, vacated the ward, the child lay there alone and started screaming - the mother was no longer allowed to feed the girl in the morning, and, as the doctor said later, the daughter did not eat the mixture from the bottle.
Olga went to the isolation ward, continuing to call the Ministry of Health and Rospotrebnadzor, and then one of the doctors whispered that, while waiting for the test, her daughter could not be sent to the hospital, after all, she had an infectious disease, but give it to her husband if he ... brought a freshly taken PCR test.
“Yes, he was in labor yesterday, but he needs a fresh, today's test,” the manager confirmed. – No, you cannot retake the test in a commercial laboratory. We don’t know who makes them there and from what material.”
“So my husband can bring a test from a third-party organization, but I can't? Olga was surprised. “It seems to be some sort of double standard.”
It took about an hour to find a laboratory where the test results would be reported immediately. He was negative and the "contact" child was given to dad.
After making sure that the child was safe, Olga, crying, remained in the isolation ward to wait for the transfer. The wait dragged on until the evening, Olga still did not feel any manifestations of the disease. After examining her again, the doctors of the detention center said that Olga was “sick asymptomatically” and allowed her to continue to get sick at home, but on the condition that the child should be at a different address.
The wait dragged on until the evening, Olga still did not feel any manifestations of the disease. After examining her again, the doctors of the detention center said that Olga was “sick asymptomatically” and allowed her to continue to get sick at home, but on the condition that the child should be at a different address.
At the same time, the patient was not allowed to drive home in her car, in the evening she was taken by a special carriage with a driver, but without a medical team. By this time, the husband and children had already moved in with their parents.
The next day, Olga called two independent laboratories to her house and again passed the PCR test, as well as, on the advice of a lawyer, tests for two types of antibodies. A day later, all tests came back negative - Olga was healthy and did not have a coronavirus infection in the past.
At the same time, the whole family, together with grandparents, and even, once again, a newborn daughter, did the tests - and everyone was healthy. By that time, the result of the text from the maternity hospital had arrived, once again confirming that the newborn was healthy.
By that time, the result of the text from the maternity hospital had arrived, once again confirming that the newborn was healthy.
Only now the baby refused mixtures and constantly screamed. “In this whole situation, we were very helped out by the fact that my husband is an experienced dad, our eldest son is already three years old.
Immediately after the birth, the husband held his daughter in his arms for a long time, then we specially covered her with his T-shirt, so that she knew his smell, - says Olga. - If there were no such experience, the situation would be even sadder.
I myself was constantly pumping milk for these three days and anyway, in the end, I just climbed the wall from pain. Neither cream, nor cabbage, nor other folk remedies helped - the chest was stone, mastitis began.
At this time, there were endless calls home from all sorts of control organizations. Olga answered the calls, but refused to come and examine the infectious ambulance with a fight.
“I have several tests confirming that I am healthy, so it is you who have been in contact with the infected who are a danger to me, not me to you,” she said. The doctors stopped insisting only when they heard that the alleged patient simply would not open the door for them.
On the fourth day, the local pediatrician came to register the newborn and decide with which of the adults and where to isolate her, since the child was “listed as a contact”. But, looking at a pile of negative tests, the doctor ordered not to torture the baby and give it to his mother. After that, Olga and her daughter, just in case, honestly stayed at home for two weeks.
“When my husband brought the baby to me, she finally stopped screaming. The chest took eagerly, in the first days she could not let me go and overeat. Now the daughter is completely healthy, she gained 1100 grams in the first month
If the mother has covid: Rospotrebnadzor protocols
If the woman in labor has confirmed COVID-19, the child who was with her is considered “contact”. PCR tests should be taken from him, there are cases when analyzes of other media were also done (not only a smear from the mucous membrane, but also a fecal analysis).
PCR tests should be taken from him, there are cases when analyzes of other media were also done (not only a smear from the mucous membrane, but also a fecal analysis).
The contact child can wait for the results of the analysis either in the “yellow” department of the infectious diseases hospital (where children are suspected of covid), or at home with a healthy parent (if the child does not have signs of SARS). The second is safer, since the circle of contacts in this case is smaller.
A child with suspected COVID-19 at home must be registered with the local pediatrician. The child and caring parent must comply with the conditions of self-isolation until the diagnosis is clarified.
If the PCR test is positive, the child has COVID-19- the decision to hospitalize him is made depending on the condition of the child. With severe symptoms - fever, pneumonia - the child will be admitted to the children's infectious diseases hospital. With a mild (normal or subfebrile temperature, no pneumonia) or asymptomatic course, they will leave to get sick at home under the supervision of a local pediatrician.
At the same time, a parent who cared for a child diagnosed with covid is considered a contact parent and must comply with the rules of self-isolation.
There is a chance for a parent to become infected from a child, even if the child was asymptomatic.
“In utero, a child will not be infected with covid from a mother, but it is possible through airborne droplets” Lilia Kazakova. Photo: Evgeniy Globenko
Comments Lilia Kazakova, Pediatrician at the Center for Maternity, Natural Development and Child Health
– Is it possible that a woman in labor with COVID-19 gives birth to an uninfected child?
– Quite possible. We do not have data that there is intrauterine infection, so something is unlikely to happen to the child in this way. And I will add that a positive smear for COVID in the last weeks of pregnancy is not an indication for early delivery in any case.
So the child, when he was just born, will not be infected with the new virus, since the way of spread of this virus is mainly airborne, and the child himself in this world has hardly breathed yet.
Moreover, a sick mother's newborn may even have some kind of immunity, since part of her mother's antibodies got into her blood through the placenta. Here is such a protection system: antibodies pass through the placental barrier, but the virus does not. Unfortunately, it is still not very clear whether the child will have antibodies if the mother is an asymptomatic carrier of the virus. For children, such studies are still ongoing.
– The mother is sick, the child is healthy. Is separation inevitable?
- By Russian standards of assistance - yes. With the goal of “breaking the chain of infections”, although we don’t have any unequivocal information about the high risk of infection for healthy newborns.
The child will either be placed separately from the mother in the maternity hospital or discharged home. Mom will be transferred first to an observatory in the maternity hospital, then to the infectious diseases department of the hospital. A patient with a mild or asymptomatic course can be sent home to be ill, provided that a special transportation takes her there, and then she will be separated from the child. Today, this is exactly the procedure in Moscow and the Moscow region. Although, I repeat, there is no absolute certainty that such a separation of mother and baby is necessary in the world.
A patient with a mild or asymptomatic course can be sent home to be ill, provided that a special transportation takes her there, and then she will be separated from the child. Today, this is exactly the procedure in Moscow and the Moscow region. Although, I repeat, there is no absolute certainty that such a separation of mother and baby is necessary in the world.
Separated by Rospotrebnadzor
According to WHO recommendations, a mother with COVID-19 should continue breastfeeding if possible, subject to all precautions. That is, it is not necessary to separate the mother from the newborn. However, in Russia there is a system of measures prescribed by Rospotrebnadzor, according to which mother and child will be separated without fail.
As long as the mask is worn and hygiene is observed, such a mother can take care of the child and feed him, as there is evidence of the antiviral properties of breast milk.
At the same time, according to the law, for all manipulations, including the hospitalization of a mother or child, we sign a voluntary informed consent, here it is also needed.
As far as I know, from the current practice of mandatory isolation of the mother in case of a positive test, the employees of maternity hospitals themselves, who are forced to comply with the order of Rospotrebnadzor, are not at all enthusiastic.
True, there were also cases when a mother refuses isolation, and a month later the whole family falls ill. And it is impossible to say unequivocally how the infection occurred.
– To what extent can other relatives make up for the mother's absence?
- The same skin-to-skin contact may well be not only with mom, but with dad or grandma. For example, there is a method of nursing premature "kangaroos" when a child with all the tubes to which it is connected is not in an incubator, but in a special sling on the parent's body; He works great not only with mom, but also with dad.
Moreover, when using this method, which is not yet very popular in Russia, the child must be carried 24/7; One mother simply cannot cope with such a task.
But contact with a newborn doesn't have to be literally skin-to-skin. Contact "baby's clothes - dad's shirt" is also suitable, the main thing is that the child feels the warmth of the adult's body, his breathing, movement. Therefore, if, for example, a mother is in the hospital for COVID-19, and the child is at home, dad should hold him in his arms more.
It is good for relatives to talk to the baby more often, stroke, hug, kiss. If a child at this moment does not hear his mother's voice, but hears his father's, grandmother's, grandfather's, dear person - this is wonderful!
– And there is another idea that the child should hear the beat of the mother's heart – he listened to it for nine months and now he recognizes it.
- A child really recognizes his mother from the very first days - by the beating of the heart, by the smell. But if during the mother's absence the child constantly smells and hears the heart of someone else, nothing terrible will happen.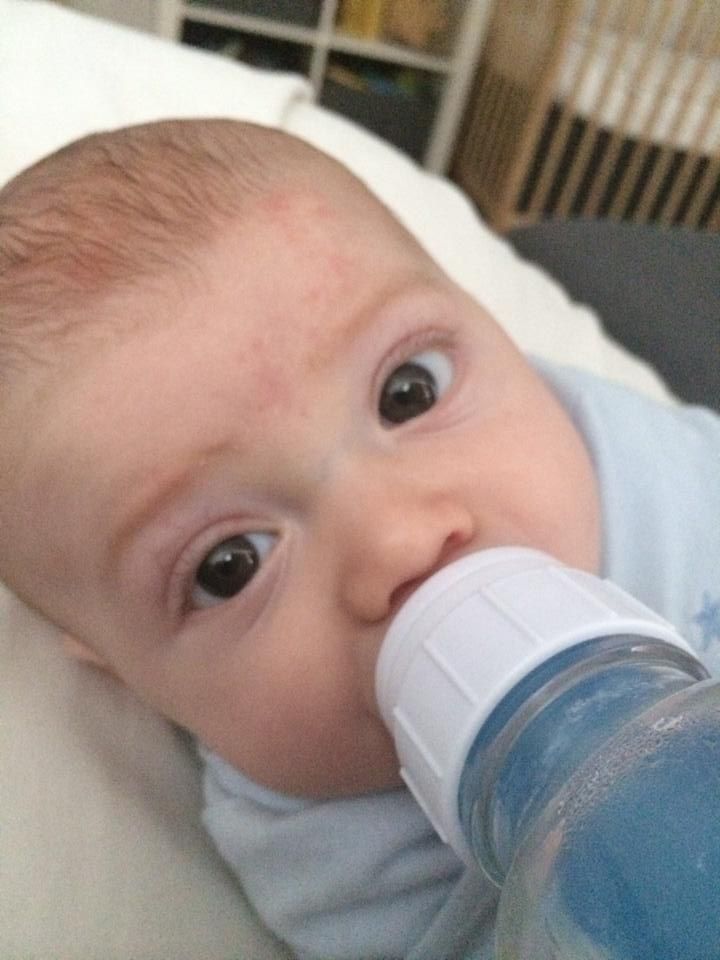
History 2
Let mother hear, let mother come!
Alla gave birth to a son on June 18, 2020 in Novosibirsk. The birth went well, then the son began to cough, the doctors reassured him: this is an allergy of the newborn to powder or diapers.
On the day of discharge, the relatives could not meet Alla from the maternity hospital, and she asked to stay for another day. I really wanted a beautiful statement - with flowers, balloons and a photographer. But, as expected, it didn't work out.
In the evening Alla had a fever. Right at the hospital, she underwent a CT scan, which showed pneumonia. They took a test from the woman and took her to the infectious diseases hospital - first to the “yellow” zone, where those whose diagnosis is in question lie, and when the test turned out to be positive, to the “red”. In the first three or four days, Alla had a temperature of forty.
The child stayed at the maternity hospital.
According to the law, only mom or dad can take him out of there, but Alla's husband was not in the country at the time of the birth. In order for the child to be given to the grandmother, it is necessary to write a notarized power of attorney - lying in the red zone, this is impossible to do.
A few days later, Alla's son was taken to a children's hospital. To the question: “Why is my child in the hospital if he is not sick?”, - in the help desk she was answered: “That's how it should be. Get out and take your son."
When the grandmother drove up to the hospital, begging the doctors on the phone to show her grandson at least from afar, they called the police.
By the tenth day, it turned out that the child also had COVID-19. CT showed pneumonia. Two weeks later, Alla was discharged and went to the hospital to her son.
“In the hospital, I saw that the child was dirty. Armpits are red under a heavy layer of powder.
Diarrhea. And also - an absolutely meaningless, somewhere inward, look. All sluggish, as if not in himself.
I cried for about an hour. I was afraid that he would stay like this. I had some milk left, but my son did not take the breast. He did not see me for more than two weeks and weaned!
But already three days after we ended up together, the look became completely different, as if the son recognized me, and then I guessed that the child most likely had not been picked up all this time, they had not spoken to him - nurses there was just no time.”
I was glad that, having found himself with his mother, the baby began to eat intensively. “It was impossible to take the bottle away from him. I realized that the baby was not eating enough and asked the nurses for more infant formula. In response, she heard: “The doctor calculates the mixture according to the norm. If tomorrow he recalculates the norm for you, we will add it.”
The question, “Will the child be hungry today?” The nurses weren't interested.
Then I poured a little boiled water into the bottle, rinsed the traces of the mixture on the walls with it. Only after drinking this slurry, the son calmed down.
Alla and her son stayed in the hospital for about two more weeks. At discharge, a one-month-old baby weighed exactly as much as he weighed at birth (!). At home, for some time he continued to shudder and cry when his mother straightened the blanket on him.
Now the four-month-old boy has caught up with his peers, his parents, grandparents are nearby, he is doing well.
Immediate and distant consequences of separation from mother Lilia Kazakova. Photo: Evgeniy Globenko
Comments Lilia Kazakova:
– How does at least a two-week separation from mother at such an early age threaten a child?
- Separation immediately after childbirth most often threatens with the loss of breastfeeding, a violation of psycho-emotional contact. Mom will suffer without a baby, the emotional development of the baby will be disrupted, because he will be all alone for many days. He will be cared for and, if necessary, treated by the medical staff and nothing more. The surrounding hospital microbial environment can affect the child in a negative way.
Mom will suffer without a baby, the emotional development of the baby will be disrupted, because he will be all alone for many days. He will be cared for and, if necessary, treated by the medical staff and nothing more. The surrounding hospital microbial environment can affect the child in a negative way.
Quite often the result of the separation of mother and baby is the loss of breastfeeding, even in cases where the woman has maintained lactation, regularly, at least 6-8 times a day, expressing milk during separation.
The baby, getting used to the bottle, may not take the breast later. The hard plastic bottle does not feel like warm, soft breasts to the touch, and the mechanics of the movements by which milk is extracted from the nipple are different than during breastfeeding. Having become accustomed to one, the child often cannot adapt to another.
With artificial feeding without skin-to-skin contact, the baby's microbiome will be formed differently. For a normal start to life, a child needs first colostrum, then mother's milk. A child with an improperly formed microbiome runs the risk of being more susceptible to infections in the future (SARS and, by the way, the same COVID-19).
A child with an improperly formed microbiome runs the risk of being more susceptible to infections in the future (SARS and, by the way, the same COVID-19).
– What are the consequences for the baby's nervous system? Why did the child, reunited with his mother in the hospital, show an absent look?
- These are all signs of sensory deprivation. When a child is in the hospital, there is no loving adult there to take care of him. The child does not see a constant, familiar person near him (and he distinguishes his mother by sensations and smell from birth, and by the age of two weeks he is already gradually learning to distinguish faces), no one responds to his needs in time. And the child "freezes", stops giving signals to the outside.
The consequences of this can be very different, but if soon the mother appears nearby and starts talking with the child, holding him in her arms a lot, reacting to his manifestations, the "frostiness" of the baby disappears. Of course, instead of a mother, there may be other relatives, as we said above, the main thing is that people should be constant and loving.
Of course, instead of a mother, there may be other relatives, as we said above, the main thing is that people should be constant and loving.
Here you can see a detailed analysis of the situation of separation of mother and child from the point of view of a lawyer.
How about in other countries?
The care of children born to mothers with suspected or confirmed COVID-19 varies around the world.
For example, the U.S. Centers for Disease Control and Prevention (a federal agency of the U.S. Department of Health) recommends that the placement of an infant born to such a mother be left to the discretion of the clinic.
At the same time, it is recommended to take into account that
1) an infant born from an infected mother is healthy, but further infection by airborne droplets during communication with the mother is possible;
2) breast-feeding is undoubtedly more useful than artificial feeding;
3) further keeping an infant who has been in contact with a sick mother with other children (including in intensive care units) may lead to their infection.