Baby feeding but not gaining weight
Why Isn’t Your Baby Gaining Weight? And When Should You Worry?
AddictionAllergies & AsthmaAmbulatoryAudiologyAutismAwardsBC4TeensBehavioral HealthBehind the ScenesBurn CenterCancerCardiologyCenter for Healthy Weight and NutritionCenter for Injury Research and PolicyChild BehaviorChild DevelopmentColorectal and Pelvic ReconstructionCommunity EducationCommunity ResourcesCoronavirusDentistryDermatologyDiseases & ConditionsDiversity and InclusionEndocrinologyENTEpilepsyEverything MattersFertility and Reproductive Health ProgramFundraising EventsGastroenterologyGeneticsGynecologyHematologyHomecareHospiceHospital NewsInfants & NewbornsInfectious DiseaseKids & TeensLaboratory ServicesMake Safe HappenMarathonNeonatologyNephrologyNeurologyNeurosurgeryNew HospitalNICUNutrition & FitnessOccupational TherapyOphthalmologyOrthopedicsOur PatientsOur staffPalliative CareParentingPediatric NewsPharmacyPhysical Therapy - Sports and OrthopedicPlastic SurgeryPopulation HealthPregnancyPrimary CarePsychologyPulmonaryRadiologyReach Out and ReadRehabilitationResearchRheumatologySafety & PreventionSports MedicineSurgical ServicesThe Center for Family Safety and HealingTherapeutic RecreationTherapyTHRIVE ProgramToddlers & PreschoolersUrgent CareUrology
Aaron Barber, AT, ATC, PESAbbie Roth, MWCAbby Orkis, MSW, LSWAdam Ostendorf, MDAdriane Baylis, PhD, CCC-SLPAdrienne M. Flood, CPNP-ACAdvanced Healthcare Provider CouncilAila Co, MDAlaina White, AT, ATCAlana Milton, MDAlana Milton, MDAlecia Jayne, AuDAlena SchuckmannAlessandra Gasior, DOAlex Kemper, MDAlexandra Funk, PharmD, DABATAlexandra Sankovic, MDAlexis Klenke, RD, LDAlice Bass, CPNP-PCAlison PeggAllie DePoyAllison Rowland, AT, ATCAllison Strouse, MS, AT, ATCAmanda E. Graf, MDAmanda GoetzAmanda Smith, RN, BSN, CPNAmanda Sonk, LMTAmanda Whitaker, MDAmber Patterson, MDAmberle Prater, PhD, LPCCAmy Brown Schlegel, MDAmy Coleman, LISWAmy Dunn, MDAmy E. Valasek, MD, MScAmy Fanning, PT, DPTAmy Garee, CPNP-PCAmy Hahn, PhDAmy HessAmy Leber, PhDAmy LeRoy, CCLSAmy Moffett, CPNP-PCAmy Randall-McSorley, MMC, EdD CandidateAmy Thomas, BSN, RN, IBCLCAmy Wahl, APNAnastasia Fischer, MD, FACSMAndala HardyAndrea Brun, CPNP-PCAndrea M. Boerger, MEd, CCC-SLPAndrea Sattler, MDAndrea ShellowAndrew AxelsonAndrew Kroger, MD, MPHAndrew SchwadererAndria Haynes, RNAngela AbenaimAngela Billingslea, LISW-SAnn Pakalnis, MDAnna Lillis, MD, PhDAnnette Haban-BartzAnnie Drapeau, MDAnnie Temple, MS, CCC-SLP, CLCAnnie Truelove, MPHAnthony Audino, MDAnup D.
 Patel, MDAri Rabkin, PhDAriana Hoet, PhDArielle Sheftall, PhDArleen KarczewskiAshlee HallAshleigh Kussman, MDAshley Debeljack, PsyDAshley Ebersole, MDAshley EcksteinAshley Kroon Van DiestAshley M. Davidson, AT, ATC, MSAshley Minnick, MSAH, AT, ATCAshley Overall, FNPAshley Parikh, CPNP-PCAshley Parker MSW, LISW-SAshley Parker, LISW-SAshley Tuisku, CTRSAsuncion Mejias, MD, PhDAurelia Wood, MDBailey Young, DOBecky Corbitt, RNBelinda Mills, MDBenjamin Fields, PhD, MEdBenjamin Kopp, MDBernadette Burke, AT, ATC, MSBeth Martin, RNBeth Villanueva, OTD, OTR/LBethany Uhl, MDBethany Walker, PhDBhuvana Setty, MDBill Kulju, MS, ATBlake SkinnerBonnie Gourley, MSW, LSWBrad Childers, RRT, BSBrandi Cogdill, RN, BSN, CFRN, EMT-PBrandon MorganBreanne L. Bowers, PT, DPT, CHT, CFSTBrendan Boyle, MD, MPHBrian Boe, MDBrian K. Kaspar, PhDBrian Kellogg, MDBriana Crowe, PT, DPT, OCSBrigid Pargeon, MS, MT-BCBrittney Hardin, MOT, OTR/LBrooke Sims, LPCC, ATRCagri Toruner, MDCaitlin Bauer, RD, LDCaitlin TullyCaleb MosleyCallista DammannCallista PoppCami Winkelspecht, PhDCamille Wilson, PhDCanice Crerand, PhDCara Inglis, PsyDCarl H.
Patel, MDAri Rabkin, PhDAriana Hoet, PhDArielle Sheftall, PhDArleen KarczewskiAshlee HallAshleigh Kussman, MDAshley Debeljack, PsyDAshley Ebersole, MDAshley EcksteinAshley Kroon Van DiestAshley M. Davidson, AT, ATC, MSAshley Minnick, MSAH, AT, ATCAshley Overall, FNPAshley Parikh, CPNP-PCAshley Parker MSW, LISW-SAshley Parker, LISW-SAshley Tuisku, CTRSAsuncion Mejias, MD, PhDAurelia Wood, MDBailey Young, DOBecky Corbitt, RNBelinda Mills, MDBenjamin Fields, PhD, MEdBenjamin Kopp, MDBernadette Burke, AT, ATC, MSBeth Martin, RNBeth Villanueva, OTD, OTR/LBethany Uhl, MDBethany Walker, PhDBhuvana Setty, MDBill Kulju, MS, ATBlake SkinnerBonnie Gourley, MSW, LSWBrad Childers, RRT, BSBrandi Cogdill, RN, BSN, CFRN, EMT-PBrandon MorganBreanne L. Bowers, PT, DPT, CHT, CFSTBrendan Boyle, MD, MPHBrian Boe, MDBrian K. Kaspar, PhDBrian Kellogg, MDBriana Crowe, PT, DPT, OCSBrigid Pargeon, MS, MT-BCBrittney Hardin, MOT, OTR/LBrooke Sims, LPCC, ATRCagri Toruner, MDCaitlin Bauer, RD, LDCaitlin TullyCaleb MosleyCallista DammannCallista PoppCami Winkelspecht, PhDCamille Wilson, PhDCanice Crerand, PhDCara Inglis, PsyDCarl H. Backes, MDCarlo Di Lorenzo, MDCarly FawcettCarol Baumhardt, LMTCarolyn FigiCarrie Rhodes, CPST-I, MTSA, CHESCasey Cottrill, MD, MPHCasey TrimbleCassandra McNabb, RN-BSNCatherine Earlenbaugh, RNCatherine Sinclair, MDCatherine Trimble, FNPCatrina Litzenburg, PhDCharae Keys, MSW, LISW-SCharles Elmaraghy, MDChelsea Britton, MS, RD, LD, CLC Chelsea Kebodeaux, MDChelsie Doster, BSCheryl Boop, MS, OTR/LCheryl G. Baxter, CPNPCheryl Gariepy, MDChet Kaczor, PharmD, MBAChris MarreroChris Smith, RNChristina Ching, MDChristina DayChristine Johnson, MA, CCC-SLPChristine Koterba, PhDChristine Mansfield, PT, DPT, OCS, ATCChristine PrusaChristopher Goettee, PT, DPT, OCSChristopher Iobst, MDChristopher Ouellette, MDChristy Lumpkins, LISW-SCindy IskeClaire Kopko PT, DPT, OCS, NASM-PESCody Hostutler, PhDConnor McDanel, MSW, LSWCorey Rood, MDCorinne Syfers, CCLSCourtney Bishop. PA-CCourtney Brown, MDCourtney Hall, CPNP-PCCourtney Porter, RN, MSCristina Tomatis Souverbielle, MDCrystal MilnerCurt Daniels, MDCynthia Holland-Hall, MD, MPHDana Lenobel, FNPDana Noffsinger, CPNP-ACDane Snyder, MDDaniel Coury, MDDaniel DaJusta, MDDanielle Peifer, PT, DPTDavid A Wessells, PT, MHADavid Axelson, MDDavid Stukus, MDDean Lee, MD, PhDDebbie Terry, NPDeborah Hill, LSWDeborah Zerkle, LMTDeena Chisolm, PhDDeipanjan Nandi, MD MScDenis King, MDDenise EllDennis Cunningham, MDDennis McTigue, DDSDiane LangDominique R.
Backes, MDCarlo Di Lorenzo, MDCarly FawcettCarol Baumhardt, LMTCarolyn FigiCarrie Rhodes, CPST-I, MTSA, CHESCasey Cottrill, MD, MPHCasey TrimbleCassandra McNabb, RN-BSNCatherine Earlenbaugh, RNCatherine Sinclair, MDCatherine Trimble, FNPCatrina Litzenburg, PhDCharae Keys, MSW, LISW-SCharles Elmaraghy, MDChelsea Britton, MS, RD, LD, CLC Chelsea Kebodeaux, MDChelsie Doster, BSCheryl Boop, MS, OTR/LCheryl G. Baxter, CPNPCheryl Gariepy, MDChet Kaczor, PharmD, MBAChris MarreroChris Smith, RNChristina Ching, MDChristina DayChristine Johnson, MA, CCC-SLPChristine Koterba, PhDChristine Mansfield, PT, DPT, OCS, ATCChristine PrusaChristopher Goettee, PT, DPT, OCSChristopher Iobst, MDChristopher Ouellette, MDChristy Lumpkins, LISW-SCindy IskeClaire Kopko PT, DPT, OCS, NASM-PESCody Hostutler, PhDConnor McDanel, MSW, LSWCorey Rood, MDCorinne Syfers, CCLSCourtney Bishop. PA-CCourtney Brown, MDCourtney Hall, CPNP-PCCourtney Porter, RN, MSCristina Tomatis Souverbielle, MDCrystal MilnerCurt Daniels, MDCynthia Holland-Hall, MD, MPHDana Lenobel, FNPDana Noffsinger, CPNP-ACDane Snyder, MDDaniel Coury, MDDaniel DaJusta, MDDanielle Peifer, PT, DPTDavid A Wessells, PT, MHADavid Axelson, MDDavid Stukus, MDDean Lee, MD, PhDDebbie Terry, NPDeborah Hill, LSWDeborah Zerkle, LMTDeena Chisolm, PhDDeipanjan Nandi, MD MScDenis King, MDDenise EllDennis Cunningham, MDDennis McTigue, DDSDiane LangDominique R. Williams, MD, MPH, FAAP, Dipl ABOMDonna M. Trentel, MSA, CCLSDonna Ruch, PhDDonna TeachDoug WolfDouglas McLaughlin, MDDrew Duerson, MDEd MinerEdward Oberle, MD, RhMSUSEdward Shepherd, MDEileen Chaves, PhDElena CamachoElise Berlan, MDElise DawkinsElizabeth A. Cannon, LPCCElizabeth Cipollone, LPCC-SElizabeth Zmuda, DOEllyn Hamm, MM, MT-BCEmily A. Stuart, MDEmily Decker, MDEmily GetschmanEmma Wysocki, PharmD, RDNEric Butter, PhDEric Leighton, AT, ATCEric Sribnick, MD, PhDErica Domrose, RD, LDEricca L Lovegrove, RD, LDErika RobertsErin Gates, PT, DPTErin Johnson, M.Ed., C.S.C.S.Erin Shann, BSN, RNErin TebbenFarah W. Brink, MDFatimah MasoodFrances Fei, MDGail Bagwell, DNP, APRN, CNSGail Besner, MDGail Swisher, ATGarey Noritz, MDGary A. Smith, MD, DrPHGeri Hewitt, MDGina Hounam, PhDGina McDowellGina MinotGrace Paul, MDGregory D. Pearson, MDGriffin Stout, MDGuliz Erdem, MDHailey Blosser, MA, CCC-SLPHanna MathessHeather Battles, MDHeather ClarkHeather L. Terry, MSN, RN, FNP-C, CUNPHeather Yardley, PhDHenry SpillerHenry Xiang, MD, MPH, PhDHerman Hundley, MS, AT, ATC, CSCSHilary Michel, MDHiren Patel, MDHolly Deckling, MSWHoma Amini, DDS, MPH, MSHoward Jacobs, MDHunter Wernick, DOIbrahim Khansa, MDIhuoma Eneli, MDIlana Moss, PhDIlene Crabtree, PTIrene Mikhail, MDIrina Buhimschi, MDIvor Hill, MDJackie Cronau, RN, CWOCNJacqueline Wynn, PhD, BCBA-DJacquelyn Doxie King, PhDJaime-Dawn Twanow, MDJaimie D.
Williams, MD, MPH, FAAP, Dipl ABOMDonna M. Trentel, MSA, CCLSDonna Ruch, PhDDonna TeachDoug WolfDouglas McLaughlin, MDDrew Duerson, MDEd MinerEdward Oberle, MD, RhMSUSEdward Shepherd, MDEileen Chaves, PhDElena CamachoElise Berlan, MDElise DawkinsElizabeth A. Cannon, LPCCElizabeth Cipollone, LPCC-SElizabeth Zmuda, DOEllyn Hamm, MM, MT-BCEmily A. Stuart, MDEmily Decker, MDEmily GetschmanEmma Wysocki, PharmD, RDNEric Butter, PhDEric Leighton, AT, ATCEric Sribnick, MD, PhDErica Domrose, RD, LDEricca L Lovegrove, RD, LDErika RobertsErin Gates, PT, DPTErin Johnson, M.Ed., C.S.C.S.Erin Shann, BSN, RNErin TebbenFarah W. Brink, MDFatimah MasoodFrances Fei, MDGail Bagwell, DNP, APRN, CNSGail Besner, MDGail Swisher, ATGarey Noritz, MDGary A. Smith, MD, DrPHGeri Hewitt, MDGina Hounam, PhDGina McDowellGina MinotGrace Paul, MDGregory D. Pearson, MDGriffin Stout, MDGuliz Erdem, MDHailey Blosser, MA, CCC-SLPHanna MathessHeather Battles, MDHeather ClarkHeather L. Terry, MSN, RN, FNP-C, CUNPHeather Yardley, PhDHenry SpillerHenry Xiang, MD, MPH, PhDHerman Hundley, MS, AT, ATC, CSCSHilary Michel, MDHiren Patel, MDHolly Deckling, MSWHoma Amini, DDS, MPH, MSHoward Jacobs, MDHunter Wernick, DOIbrahim Khansa, MDIhuoma Eneli, MDIlana Moss, PhDIlene Crabtree, PTIrene Mikhail, MDIrina Buhimschi, MDIvor Hill, MDJackie Cronau, RN, CWOCNJacqueline Wynn, PhD, BCBA-DJacquelyn Doxie King, PhDJaime-Dawn Twanow, MDJaimie D. Nathan, MD, FACSJames Murakami, MDJames Popp, MDJames Ruda, MDJameson Mattingly, MDJamie Macklin, MDJamie ReedyJane AbelJanelle Huefner, MA, CCC-SLPJanice M. Moreland, CPNP-PC, DNPJanice Townsend, DDS, MSJared SylvesterJason JacksonJason P. Garee, PhDJaysson EicholtzJean Hruschak, MA, CCC/SLPJeff Sydes, CSCSJeffery Auletta, MDJeffrey Bennett, MD, PhDJeffrey Hoffman, MDJeffrey Leonard, MDJen Campbell, PT, MSPTJena HeckJenn Gonya, PhDJennie Aldrink, MDJennifer Borda, PT, DPTJennifer HofherrJennifer LockerJennifer PrinzJennifer Reese, PsyDJennifer Smith, MS, RD, CSP, LD, LMTJennifer Walton, MD, MPH, FAAPJenny Worthington, PT, DPTJerry R. Mendell, MDJessalyn Mayer, MSOT, OTR/LJessica Bailey, PsyDJessica Bogacik, MS, MT-BCJessica Bowman, MDJessica BrockJessica Bullock, MA/CCC-SLPJessica Buschmann, RDJessica Scherr, PhDJim O’Shea OT, MOT, CHTJoan Fraser, MSW, LISW-SJohn Ackerman, PhDJohn Caballero, PT, DPT, CSCSJohn Kovalchin, MDJonathan D. Thackeray, MDJonathan Finlay, MB, ChB, FRCPJonathan M.
Nathan, MD, FACSJames Murakami, MDJames Popp, MDJames Ruda, MDJameson Mattingly, MDJamie Macklin, MDJamie ReedyJane AbelJanelle Huefner, MA, CCC-SLPJanice M. Moreland, CPNP-PC, DNPJanice Townsend, DDS, MSJared SylvesterJason JacksonJason P. Garee, PhDJaysson EicholtzJean Hruschak, MA, CCC/SLPJeff Sydes, CSCSJeffery Auletta, MDJeffrey Bennett, MD, PhDJeffrey Hoffman, MDJeffrey Leonard, MDJen Campbell, PT, MSPTJena HeckJenn Gonya, PhDJennie Aldrink, MDJennifer Borda, PT, DPTJennifer HofherrJennifer LockerJennifer PrinzJennifer Reese, PsyDJennifer Smith, MS, RD, CSP, LD, LMTJennifer Walton, MD, MPH, FAAPJenny Worthington, PT, DPTJerry R. Mendell, MDJessalyn Mayer, MSOT, OTR/LJessica Bailey, PsyDJessica Bogacik, MS, MT-BCJessica Bowman, MDJessica BrockJessica Bullock, MA/CCC-SLPJessica Buschmann, RDJessica Scherr, PhDJim O’Shea OT, MOT, CHTJoan Fraser, MSW, LISW-SJohn Ackerman, PhDJohn Caballero, PT, DPT, CSCSJohn Kovalchin, MDJonathan D. Thackeray, MDJonathan Finlay, MB, ChB, FRCPJonathan M. Grischkan, MDJonathan Napolitano, MDJoshua Prudent, MDJoshua Watson, MDJulee Eing, CRA, RT(R)Julia Colman, MOT, OTR/LJulie ApthorpeJulie Lange, MDJulie Leonard, MD, MPHJulie Racine, PhDJulie Samora, MDJustin Indyk, MD, PhDKady LacyKaitrin Kramer, DDS, MS, PhDKaleigh Hague, MA, MT-BCKaleigh MatesickKamilah Twymon, LPCC-SKara Malone, MDKara Miller, OTR/LKaren A. Diefenbach, MDKaren Allen, MDKaren Days, MBAKaren Rachuba, RD, LD, CLCKari A. Meeks, OTKari Cardiff, ODKari Dubro, MS, RD, LD, CWWSKari Phang, MDKarla Vaz, MDKaryn L. Kassis, MD, MPHKasey Strothman, MDKatherine Deans, MDKatherine McCracken, MD FACOGKathleen (Katie) RoushKathryn Blocher, CPNP-PCKathryn J. Junge, RN, BSNKathryn Obrynba, MDKatia Camille Halabi, MDKatie Brind'Amour, MSKatie DonovanKatie Thomas, APRKatrina Hall, MA, CCLSKatrina Ruege, LPCC-SKatya Harfmann, MDKayla Zimpfer, PCCKaylan Guzman Schauer, LPCC-SKeli YoungKelley SwopeKelli Dilver, PT, DPTKelly AbramsKelly BooneKelly HustonKelly J. Kelleher, MDKelly McNally, PhDKelly N.
Grischkan, MDJonathan Napolitano, MDJoshua Prudent, MDJoshua Watson, MDJulee Eing, CRA, RT(R)Julia Colman, MOT, OTR/LJulie ApthorpeJulie Lange, MDJulie Leonard, MD, MPHJulie Racine, PhDJulie Samora, MDJustin Indyk, MD, PhDKady LacyKaitrin Kramer, DDS, MS, PhDKaleigh Hague, MA, MT-BCKaleigh MatesickKamilah Twymon, LPCC-SKara Malone, MDKara Miller, OTR/LKaren A. Diefenbach, MDKaren Allen, MDKaren Days, MBAKaren Rachuba, RD, LD, CLCKari A. Meeks, OTKari Cardiff, ODKari Dubro, MS, RD, LD, CWWSKari Phang, MDKarla Vaz, MDKaryn L. Kassis, MD, MPHKasey Strothman, MDKatherine Deans, MDKatherine McCracken, MD FACOGKathleen (Katie) RoushKathryn Blocher, CPNP-PCKathryn J. Junge, RN, BSNKathryn Obrynba, MDKatia Camille Halabi, MDKatie Brind'Amour, MSKatie DonovanKatie Thomas, APRKatrina Hall, MA, CCLSKatrina Ruege, LPCC-SKatya Harfmann, MDKayla Zimpfer, PCCKaylan Guzman Schauer, LPCC-SKeli YoungKelley SwopeKelli Dilver, PT, DPTKelly AbramsKelly BooneKelly HustonKelly J. Kelleher, MDKelly McNally, PhDKelly N. Day, CPNP-PCKelly Pack, LISW-SKelly Tanner,PhD, OTR/L, BCPKelly Wesolowski, PsyDKelly Wise, PharmDKent Williams, MDKevin Bosse, PhDKevin Klingele, MDKim Bjorklund, MDKim Hammersmith, DDS, MPH, MSKimberly Bates, MDKimberly Sisto, PT, DPT, SCSKimberly Van Camp, PT, DPT, SCSKirk SabalkaKris Jatana, MD, FAAPKrista Winner, AuD, CCC-AKristen Armbrust, LISW-SKristen Cannon, MDKristen E. Beck, MDKristen Martin, OTR/LKristi Roberts, MS MPHKristina Booth, MSN, CFNPKristina Reber, MDKristol Das, MDKyle DavisLance Governale, MDLara McKenzie, PhD, MALaura Brubaker, BSN, RNLaura Dattner, MALaura Martin, MDLaurel Biever, LPCLauren Durinka, AuDLauren Garbacz, PhDLauren Justice, OTR/L, MOTLauren Madhoun, MS, CCC-SLPLauryn Rozum, MS, CCLSLeah Middelberg, MDLee Hlad, DPMLeena Nahata, MDLelia Emery, MT-BCLeslie Appiah, MDLinda Stoverock, DNP, RN NEA-BCLindsay Kneen, MDLindsay Pietruszewski, PT, DPTLindsay SchwartzLindsey Vater, PsyDLisa GoldenLisa Halloran, CNPLisa M. Humphrey, MDLogan Blankemeyer, MA, CCC-SLPLori Grisez PT, DPTLorraine Kelley-QuonLouis Bezold, MDLourdes Hill, LPCC-S Lubna Mazin, PharmDLuke Tipple, MS, CSCSLynda Wolfe, PhDLyndsey MillerLynn RosenthalLynne Ruess, MDMaggy Rule, MS, AT, ATCMahmoud Kallash, MDManmohan K Kamboj, MDMarc P.
Day, CPNP-PCKelly Pack, LISW-SKelly Tanner,PhD, OTR/L, BCPKelly Wesolowski, PsyDKelly Wise, PharmDKent Williams, MDKevin Bosse, PhDKevin Klingele, MDKim Bjorklund, MDKim Hammersmith, DDS, MPH, MSKimberly Bates, MDKimberly Sisto, PT, DPT, SCSKimberly Van Camp, PT, DPT, SCSKirk SabalkaKris Jatana, MD, FAAPKrista Winner, AuD, CCC-AKristen Armbrust, LISW-SKristen Cannon, MDKristen E. Beck, MDKristen Martin, OTR/LKristi Roberts, MS MPHKristina Booth, MSN, CFNPKristina Reber, MDKristol Das, MDKyle DavisLance Governale, MDLara McKenzie, PhD, MALaura Brubaker, BSN, RNLaura Dattner, MALaura Martin, MDLaurel Biever, LPCLauren Durinka, AuDLauren Garbacz, PhDLauren Justice, OTR/L, MOTLauren Madhoun, MS, CCC-SLPLauryn Rozum, MS, CCLSLeah Middelberg, MDLee Hlad, DPMLeena Nahata, MDLelia Emery, MT-BCLeslie Appiah, MDLinda Stoverock, DNP, RN NEA-BCLindsay Kneen, MDLindsay Pietruszewski, PT, DPTLindsay SchwartzLindsey Vater, PsyDLisa GoldenLisa Halloran, CNPLisa M. Humphrey, MDLogan Blankemeyer, MA, CCC-SLPLori Grisez PT, DPTLorraine Kelley-QuonLouis Bezold, MDLourdes Hill, LPCC-S Lubna Mazin, PharmDLuke Tipple, MS, CSCSLynda Wolfe, PhDLyndsey MillerLynn RosenthalLynne Ruess, MDMaggy Rule, MS, AT, ATCMahmoud Kallash, MDManmohan K Kamboj, MDMarc P. Michalsky, MDMarcel J. Casavant, MDMarci Johnson, LISW-SMarcie RehmarMarco Corridore, MDMargaret Bassi, OTR/LMaria HaghnazariMaria Vegh, MSN, RN, CPNMarissa Condon, BSN, RNMarissa E. Larouere, MBA, BSN, RNMark E. Galantowicz, MDMark Smith, MS RT R (MR), ABMP PhysicistMarnie Wagner, MDMary Ann Abrams, MD, MPHMary Fristad, PhD, ABPPMary Kay SharrettMary Shull, MDMatthew Washam, MD, MPHMeagan Horn, MAMegan Brundrett, MDMegan Dominik, OTR/LMegan FrancisMegan Letson, MD, M.EdMeghan Cass, PT, DPTMeghan Fisher, BSN, RNMeika Eby, MDMelanie Fluellen, LPCCMelanie Luken, LISW-SMelissa and Mikael McLarenMelissa McMillen, CTRSMelissa Winterhalter, MDMeredith Merz Lind, MDMichael Flores, PhDMichael T. Brady, MDMichelle Ross, MHA, RD, LD, ALCMike Patrick, MDMindy Deno, PT, DPTMitch Ellinger, CPNP-PCMolly Dienhart, MDMolly Gardner, PhDMonica Ardura, DOMonica EllisMonique Goldschmidt, MDMotao Zhu, MD, MS, PhDMurugu Manickam, MDNancy AuerNancy Cunningham, PsyDNancy Wright, BS, RRT, RCP, AE-C Naomi Kertesz, MDNatalie DeBaccoNatalie I.
Michalsky, MDMarcel J. Casavant, MDMarci Johnson, LISW-SMarcie RehmarMarco Corridore, MDMargaret Bassi, OTR/LMaria HaghnazariMaria Vegh, MSN, RN, CPNMarissa Condon, BSN, RNMarissa E. Larouere, MBA, BSN, RNMark E. Galantowicz, MDMark Smith, MS RT R (MR), ABMP PhysicistMarnie Wagner, MDMary Ann Abrams, MD, MPHMary Fristad, PhD, ABPPMary Kay SharrettMary Shull, MDMatthew Washam, MD, MPHMeagan Horn, MAMegan Brundrett, MDMegan Dominik, OTR/LMegan FrancisMegan Letson, MD, M.EdMeghan Cass, PT, DPTMeghan Fisher, BSN, RNMeika Eby, MDMelanie Fluellen, LPCCMelanie Luken, LISW-SMelissa and Mikael McLarenMelissa McMillen, CTRSMelissa Winterhalter, MDMeredith Merz Lind, MDMichael Flores, PhDMichael T. Brady, MDMichelle Ross, MHA, RD, LD, ALCMike Patrick, MDMindy Deno, PT, DPTMitch Ellinger, CPNP-PCMolly Dienhart, MDMolly Gardner, PhDMonica Ardura, DOMonica EllisMonique Goldschmidt, MDMotao Zhu, MD, MS, PhDMurugu Manickam, MDNancy AuerNancy Cunningham, PsyDNancy Wright, BS, RRT, RCP, AE-C Naomi Kertesz, MDNatalie DeBaccoNatalie I. Rine, PharmD, BCPS, BCCCPNatalie Powell, LPCC-S, LICDC-CSNatalie Rose, BSN, RNNathalie Maitre, MD, PhDNationwide Children's HospitalNationwide Children's Hospital Behavioral Health ExpertsNeetu Bali, MD, MPHNehal Parikh, DO, MSNichole Mayer, OTR/L, MOTNicole Caldwell, MDNicole Dempster, PhDNicole Greenwood, MDNicole Parente, LSWNicole Powell, PsyD, BCBA-DNina WestNkeiruka Orajiaka, MBBSOctavio Ramilo, MDOliver Adunka, MD, FACSOlivia Stranges, CPNP-PCOlivia Thomas, MDOmar Khalid, MD, FAAP, FACCOnnalisa Nash, CPNP-PCOula KhouryPaige Duly, CTRSParker Huston, PhDPatrick C. Walz, MDPatrick Queen, BSN, RNPedro Weisleder, MDPeter Minneci, MDPeter White, PhDPitty JenningsPreeti Jaggi, MDRachael Morocco-Zanotti, DORachel D’Amico, MDRachel Schrader, CPNP-PCRachel Tyson, LSWRajan Thakkar, MDRaymond Troy, MDRebecca Fisher, PTRebecca Hicks, CCLSRebecca Lewis, AuD, CCC-ARebecca M. Romero, RD, LD, CLC Reggie Ash Jr.Reno Ravindran, MDRichard Kirschner, MDRichard Wood, MDRobert A. Kowatch, MD, Ph.D.Robert Hoffman, MDRochelle Krouse, CTRSRohan Henry, MD, MSRose Ayoob, MDRose Schroedl, PhDRosemary Martoma, MDRoss Maltz, MDRyan Ingley AT, ATCSamanta Boddapati, PhDSamantha MaloneSammy CygnorSandra C.
Rine, PharmD, BCPS, BCCCPNatalie Powell, LPCC-S, LICDC-CSNatalie Rose, BSN, RNNathalie Maitre, MD, PhDNationwide Children's HospitalNationwide Children's Hospital Behavioral Health ExpertsNeetu Bali, MD, MPHNehal Parikh, DO, MSNichole Mayer, OTR/L, MOTNicole Caldwell, MDNicole Dempster, PhDNicole Greenwood, MDNicole Parente, LSWNicole Powell, PsyD, BCBA-DNina WestNkeiruka Orajiaka, MBBSOctavio Ramilo, MDOliver Adunka, MD, FACSOlivia Stranges, CPNP-PCOlivia Thomas, MDOmar Khalid, MD, FAAP, FACCOnnalisa Nash, CPNP-PCOula KhouryPaige Duly, CTRSParker Huston, PhDPatrick C. Walz, MDPatrick Queen, BSN, RNPedro Weisleder, MDPeter Minneci, MDPeter White, PhDPitty JenningsPreeti Jaggi, MDRachael Morocco-Zanotti, DORachel D’Amico, MDRachel Schrader, CPNP-PCRachel Tyson, LSWRajan Thakkar, MDRaymond Troy, MDRebecca Fisher, PTRebecca Hicks, CCLSRebecca Lewis, AuD, CCC-ARebecca M. Romero, RD, LD, CLC Reggie Ash Jr.Reno Ravindran, MDRichard Kirschner, MDRichard Wood, MDRobert A. Kowatch, MD, Ph.D.Robert Hoffman, MDRochelle Krouse, CTRSRohan Henry, MD, MSRose Ayoob, MDRose Schroedl, PhDRosemary Martoma, MDRoss Maltz, MDRyan Ingley AT, ATCSamanta Boddapati, PhDSamantha MaloneSammy CygnorSandra C. Kim, MDSara Bentley, MT-BCSara Bode, MDSara Breidigan, MS, AT, ATCSara N. Smith, MSN, APRNSara O'Rourke, MOT, OTR/L, Clinical LeadSara Schroder, MDSarah A. Denny, MDSarah Cline, CRA, RT(R)Sarah Driesbach, CPN, APNSarah GreenbergSarah Hastie, BSN, RNC-NIC Sarah Keim, PhDSarah MyersSarah O'Brien, MDSarah SaxbeSarah Schmidt, LISW-SSarah ScottSarah TraceySarah VerLee, PhDSasigarn Bowden, MDSatya Gedela, MD, MRCP(UK)Scott Coven, DO, MPHScott Hickey, MDSean EingSean Rose, MDSeth Alpert, MDShalini C. Reshmi, PhD, FACMGShana Moore, MA, CCC-AShannon Reinhart, LISW-SShari UncapherSharon Wrona, DNP, PNP, PMHSShaun Coffman PT, DPT, OCSShawn Pitcher, BS, RD, USAWShawNaye Scott-MillerShea SmoskeSheena PaceSheila GilesShelly BrackmanSimon Lee, MDSini James, MDStacy Ardoin, MDStacy Whiteside APRN, MS, CPNP-AC/PC, CPONStefanie Bester, MDStefanie Hirota, OTR/LStephanie Burkhardt, MPH, CCRCStephanie CannonStephanie Santoro, MDStephanie Vyrostek BSN, RNStephen Hersey, MDSteve Allen, MDSteven C. Matson, MDSteven Ciciora, MDSteven CuffSuellen Sharp, OTR/L, MOTSurlina AsamoaSusan Colace, MDSusan Creary, MDSwaroop Pinto, MDTabatha BallardTabbetha GrecoTabi Evans, PsyDTabitha Jones-McKnight, DOTahagod Mohamed, MDTamara MappTammi Young-Saleme, PhDTaylor Hartlaub, MD, MPHTerry Barber, MDTerry Bravender, MD, MPHTerry Laurila, MS, RPhTheresa Miller, BA, RRT, RCP, AE-C, CPFTThomas Pommering, DOTiasha Letostak, PhDTiffanie Ryan, BCBA Tim RobinsonTim Smith, MDTimothy Cripe, MD, PhDTimothy Landers PhD RN APRN-CNP CIC FAANTracey L.
Kim, MDSara Bentley, MT-BCSara Bode, MDSara Breidigan, MS, AT, ATCSara N. Smith, MSN, APRNSara O'Rourke, MOT, OTR/L, Clinical LeadSara Schroder, MDSarah A. Denny, MDSarah Cline, CRA, RT(R)Sarah Driesbach, CPN, APNSarah GreenbergSarah Hastie, BSN, RNC-NIC Sarah Keim, PhDSarah MyersSarah O'Brien, MDSarah SaxbeSarah Schmidt, LISW-SSarah ScottSarah TraceySarah VerLee, PhDSasigarn Bowden, MDSatya Gedela, MD, MRCP(UK)Scott Coven, DO, MPHScott Hickey, MDSean EingSean Rose, MDSeth Alpert, MDShalini C. Reshmi, PhD, FACMGShana Moore, MA, CCC-AShannon Reinhart, LISW-SShari UncapherSharon Wrona, DNP, PNP, PMHSShaun Coffman PT, DPT, OCSShawn Pitcher, BS, RD, USAWShawNaye Scott-MillerShea SmoskeSheena PaceSheila GilesShelly BrackmanSimon Lee, MDSini James, MDStacy Ardoin, MDStacy Whiteside APRN, MS, CPNP-AC/PC, CPONStefanie Bester, MDStefanie Hirota, OTR/LStephanie Burkhardt, MPH, CCRCStephanie CannonStephanie Santoro, MDStephanie Vyrostek BSN, RNStephen Hersey, MDSteve Allen, MDSteven C. Matson, MDSteven Ciciora, MDSteven CuffSuellen Sharp, OTR/L, MOTSurlina AsamoaSusan Colace, MDSusan Creary, MDSwaroop Pinto, MDTabatha BallardTabbetha GrecoTabi Evans, PsyDTabitha Jones-McKnight, DOTahagod Mohamed, MDTamara MappTammi Young-Saleme, PhDTaylor Hartlaub, MD, MPHTerry Barber, MDTerry Bravender, MD, MPHTerry Laurila, MS, RPhTheresa Miller, BA, RRT, RCP, AE-C, CPFTThomas Pommering, DOTiasha Letostak, PhDTiffanie Ryan, BCBA Tim RobinsonTim Smith, MDTimothy Cripe, MD, PhDTimothy Landers PhD RN APRN-CNP CIC FAANTracey L. Sisk, RN, BSN, MHATracie Steinke RD, LD, CDETracy Mehan, MATravis Gallagher, ATTrevor MillerTria Shadeed, NNPTyanna Snider, PsyDTyler Congrove, ATValencia Walker, MD, MPH, FAAPVanessa Shanks, MD, FAAPVenkata Rama Jayanthi, MDVidu Garg, MDVidya Raman, MDW. Garrett Hunt, MDWalter Samora, MDWarren D. Lo, MDWendy Anderson, MDWendy Cleveland, MA, LPCC-SWhitney McCormick, CTRSWhitney Raglin Bignall, PhDWilliam Cotton, MDWilliam J. Barson, MDWilliam Ray, PhDWilliam W. Long, MD
Sisk, RN, BSN, MHATracie Steinke RD, LD, CDETracy Mehan, MATravis Gallagher, ATTrevor MillerTria Shadeed, NNPTyanna Snider, PsyDTyler Congrove, ATValencia Walker, MD, MPH, FAAPVanessa Shanks, MD, FAAPVenkata Rama Jayanthi, MDVidu Garg, MDVidya Raman, MDW. Garrett Hunt, MDWalter Samora, MDWarren D. Lo, MDWendy Anderson, MDWendy Cleveland, MA, LPCC-SWhitney McCormick, CTRSWhitney Raglin Bignall, PhDWilliam Cotton, MDWilliam J. Barson, MDWilliam Ray, PhDWilliam W. Long, MD
Managing Poor Weight Gain in Your Breastfed Infant
Managing Poor Weight Gain in Your Breastfed Infant | Johns Hopkins MedicineSometimes, a breastfed baby will gain weight more slowly than he or she should. This could be because the mother isn't making enough milk, the baby can't get enough milk out of the breast, or the baby has a medical problem. Your baby's healthcare provider should evaluate any instance of poor weight gain. Often, a certified lactation consultant can help. Below are some general tips for addressing poor weight gain in a breastfed baby.
Often, a certified lactation consultant can help. Below are some general tips for addressing poor weight gain in a breastfed baby.
Check the schedule
-
Watch for signs from your baby that he or she wants to feed. Your baby should wake and "cue" to breastfeed about 8 to 12 times in 24 hours by rooting, making licking or sucking motions, bobbing his or her head or bringing his or her hand to the face or mouth. It is important for you to recognize these feeding cues and put your baby to your breast when he or she cues. Don't wait for your baby to cry. Crying is a late feeding cue. Usually a baby latches and breastfeeds better if he or she does not have to wait until he or she is crying, frustrated, or too tired to feed. Putting a baby off to try to get the baby to go longer between feedings and frequently offering a pacifier instead of the breast when a baby demonstrates feeding cues are often linked to poor weight gain.
-
Many mothers find milk production increases and babies' weight gains improve if they and their babies let chores and activities go for 2 or 3 days, so they can breastfeed, more or less, around the clock.
 When a baby is not breastfeeding, the mother holds him or her skin-to-skin on her chest, which often helps her become more sensitive to the baby's feeding cues.
When a baby is not breastfeeding, the mother holds him or her skin-to-skin on her chest, which often helps her become more sensitive to the baby's feeding cues. -
If your baby is a "sleepy" baby who does not cue to feed at least 8 times in 24 hours, you will have to wake the baby to feed frequently--about every 2 hours during the daytime and evening hours and at least every 3 to 4 hours at night until weight gain improves.
-
It can help to write down when your baby nurses, on which side, and for how long for a full 24 hours, if not longer. Take this record to your healthcare provider or lactation consultant to help find and fix the problem.
Latching and positioning
-
Be sure your baby is mainly uncovered during breastfeeding. A baby that is bundled papoose-style may get much too warm and comfy, and he or she is more likely to doze off too quickly during feedings. If there is a chill in the air, drape a sheet or light blanket over you and the baby, as needed.

-
If your baby falls asleep within minutes of latching on, massage your breast as he or she nurses. This can provide a burst of milk and re-trigger sucking. You can do this by stroking downward and inward on the breast.
-
Make sure your baby is latching on correctly. The latch should be comfortable to you. Your baby's lips should be flanged outward like "fish lips." The tongue should be under your breast. A large amount of your breast tissue should be in the baby's mouth.
-
In general, avoid "switch nursing." That is, breastfeeding at one breast for a few minutes, then the other, and then back again. This may interfere with your baby getting enough of the calorie-rich hindmilk, which your baby gets more of as a feeding continues on one breast. However, the "switch" strategy sometimes stimulates the "sleepy" baby so he or she wakes up and starts sucking again.
If your healthcare provider recommends supplementing
-
Use your own expressed milk first for any alternative feedings.

-
Use an alternative feeding method if it is recommended by your healthcare provider or a certified lactation consultant (IBCLC). There are many alternative feeding options, so let them know if a recommendation does not "feel right" for you. Alternative feeding methods include:
-
Several methods require assistance from a professional, such as a certified lactation consultant (IBCLC) so you can use them correctly. Depending on your baby and the cause of the problem, some methods may work better than others. Also, discuss bottle nipple type with the IBCLC if you bottle-feed any supplement. Some types of bottle nipples are less likely to interfere with breastfeeding than others.
Maintaining or increasing your milk supply
-
Pump your breasts after as many daily breastfeedings as possible, especially if you are uncertain whether your baby is effectively removing milk during breastfeeding. Many women find that trying for 8 times per day is manageable and helpful for their milk supply.

-
Pumping will remove milk effectively, so your breasts will know to make more milk. Pumping will also express supplemental milk for feeds. Milk can be removed from the breast by manual hand expression, a hand pump, a battery-powered pump, or an electric breast pump. If frequent and prolonged pumping is anticipated, a hospital-grade, electric pump can be very helpful.
Checking baby's weight
-
Your baby should be weighed on a frequent and regular basis until he or she is gaining weight at a satisfactory rate. Digital scales are available that allow a healthcare provider or a certified lactation consultant (IBCLC) to get precise pre- and post-feeding weights to measure how much milk a baby takes in during a particular breastfeeding. Although this can be helpful, babies take in different amounts at different feedings throughout a 24-hour period. Therefore, a professional may recommend that parents rent this type of scale so a baby can be weighed before and after different feedings.
 They also may suggest recording only a daily or weekly weight, depending on the situation.
They also may suggest recording only a daily or weekly weight, depending on the situation.
Call your baby's healthcare provider
If your baby ever shows signs of dehydration, call your baby's healthcare provider right away. Some signs of dehydration in a baby include:
-
Fewer stools and wet diapers than usual
-
Dry lips
-
Sunken fontanelle (soft spot)
-
Dark circles around the eyes
-
Appearing more tired than usual
If breastfeeding is properly managed, yet the baby still is not gaining enough weight, it is likely that some other factor is affecting milk production or the baby's ability to breastfeed effectively. Always consult your own, and your baby's healthcare provider.
Related
-
Pregnancy
What Really Helps You Bounce Back After Pregnancy
-
Breastfeeding Your Baby
Breastfeeding 101: Q&A with Lactation Expert Nadine Rosenblum
-
Breastfeeding Your Baby
Difficulty with Latching On or Sucking
Related Topics
A child under 1 year old does not gain weight
— Alla Anatolyevna, how much should a newborn gain weight and how should a child gain weight week by week in the first and second six months of life?
- When determining the weight gain of an infant, we all rely on the WHO centile tables. Weight gain is calculated not by weeks, but by months. In the first month of life, the child should add at least 600 g, then in the fifth month - 700-800 g each, starting from the sixth month - 650 g and then up to one year monthly - less than 50 g from the norm of the previous month.
Weight gain is calculated not by weeks, but by months. In the first month of life, the child should add at least 600 g, then in the fifth month - 700-800 g each, starting from the sixth month - 650 g and then up to one year monthly - less than 50 g from the norm of the previous month.
The first standard weight gain in the neonatal period takes into account the loss of birth weight associated with physiological conditions, so the baby grows less. In the future, as a rule, healthy children gain a little more than average - some even up to a kilogram per month.
Underweight below the first statistical corridor of the WHO centile scale is considered dangerous.
— Why is the baby not gaining weight on breastfeeding or artificial feeding?
— Low weight is often caused by malnutrition. The baby gains weight because he is fed and does not gain weight because he is not fed.
Food allergies can also lead to low weight. Milk protein is the most common cause of allergies in children. By eliminating the milk allergen, you can fight against insufficient weight gain, as well as problems from the gastrointestinal tract.
Milk protein is the most common cause of allergies in children. By eliminating the milk allergen, you can fight against insufficient weight gain, as well as problems from the gastrointestinal tract.
The child is not gaining weight: causes and solutions
What to do if the newborn is not gaining weight
- The child is malnourished - how to distinguish a simple unwillingness to eat from an illness?
— The health of the child should be assessed. A healthy baby will be calm, cheerful, smiling, he sleeps well. But if, during feeding, a child cries, throws a bottle or breast, tightens his legs, blushes, shrinks, burps, and rumbles in his stomach; if the baby has a fever, then perhaps he is sick and it is better to consult a doctor.
— How to feed a baby?
— The main responsibility of all parents is to make sure that their child is fed, receives all the nutrients necessary for his growth and development. Little tricks will help improve children's appetite. Each parent has their own approach. There are those who go to the doctor, but more often everything is decided at the family, household level.
Little tricks will help improve children's appetite. Each parent has their own approach. There are those who go to the doctor, but more often everything is decided at the family, household level.
- Improve diet. The quality and adequacy of the nutrition the child receives should be assessed. This is why it is important to keep a food diary.
- Feeding in a dream. A sleeping baby relaxes, breastfeeding takes place in a relaxed mode.
- Feed fractionally. First you need to feed the baby a little, after five minutes repeat the procedure. Some mothers feed from two breasts alternately, stimulating the production of hindmilk, which is rich in protein - a building material for physical development.
- Change the nipple on the bottle - some babies like anatomical nipples, others like cherry nipples.
— What mistakes are made by parents of babies who do not gain weight well?
- There are some common mistakes parents make.
- Breastfeeding mothers try to increase lactation on their own and start taking medications, lactagons, probiotics.
- Formula-fed parents try to change the formula as they see fit. Many believe that the more expensive the mixture, the better.
- Force feed a child when he has problems with his tummy, he cries. Negative emotions are fixed in the baby so that he starts crying only at the sight of the bottle.
- Cancel prescriptions and do not follow the doctor's advice, which can negatively affect the child's condition.
You need to consult a doctor in case of any trouble for the baby and when you cannot help him yourself. You may need an additional examination - ultrasound, medical tests.
— Does an insufficient amount of enzymes in a newborn affect the increase in body weight?
- Insufficient amount of enzymes in a child of the first trimester of life - the norm, no treatment is required. It is more often about transient (passing) lactase deficiency, which does not prevent the child from gaining weight well, eating with appetite and getting enough nutrients for growth and development.
It is more often about transient (passing) lactase deficiency, which does not prevent the child from gaining weight well, eating with appetite and getting enough nutrients for growth and development.
Parents often bring high-carbohydrate stool test results to appointments, which will not be a reason to administer enzymes - if the child is otherwise fine, no treatment is prescribed.
If the newborn does not gain weight, burps, worries, has abdominal pain, mucus and blood in the stool, then most likely this is not due to enzymes, but to food intolerance, which requires a visit to the doctor and the appointment of its own treatment.
- Alla Anatolyevna, how does complementary foods affect weight dynamics?
- Complementary foods are ideally introduced from 5.5-6 months, when the baby becomes interested in food, he begins to sit. They feed the baby with the aim of gradually transferring him to solid food in order to teach him to chew, to form taste preferences. But complementary foods do not affect weight gain.
But complementary foods do not affect weight gain.
— What should I feed my baby and how can he gain weight?
— The main nutritional value is in mother's milk or infant formula given to the baby. In force majeure circumstances, even an eight-month-old baby can consume only milk food all day and satisfy all his needs.
Vegetables are a low-calorie product. Receiving them with insufficient weight gain, the child will not gain it more. Milk porridges have more pronounced nutritional properties due to the nutritional value of milk and cereals. But if the milk formula is chosen incorrectly and the child has impaired intestinal absorption, the introduction of complementary foods in the form of porridge will also not help to gain weight. It is necessary to solve the problem of choosing a mixture and only then introduce complementary foods.
- Is it possible to accurately select milk formula and avoid weight problems?
— In my practice, most often nutritional deficiency is a problem of the initial period of life. Closer to six months, it has already been resolved, so by the period of complementary feeding, the baby comes with a mixture that is suitable for him.
Closer to six months, it has already been resolved, so by the period of complementary feeding, the baby comes with a mixture that is suitable for him.
In case of food allergies, the medicinal mixture is given to children only as a type of food approved by the doctor. If there is no allergy, a regular milk mixture is introduced, for example, based on goat milk MAMAKO ® Premium. It is important that complementary foods are not a treatment - they begin when the mixture is selected, there are no problems with digestion, the child is healthy.
Complementary foods should be introduced to a healthy toddler without digestive difficulties. Weight gain is adjusted by the selection of a special mixture or the diet of a nursing mother.
— Is it true that goat's milk formulas are better digested than cow's milk formulas, and this helps babies gain weight faster?
- "Goat" mixtures are designed to feed healthy babies. Goat protein is close to the protein of mother's milk and is absorbed by children better than cow's milk protein. But it should be remembered that normal weight helps to gain both the amount of food and the right mixture. Therefore, if the baby is healthy, then a mixture of goat's milk in sufficient quantities will provide the desired increase in weight. However, in case of problems with children's digestion, a therapeutic mixture is purchased on medical advice.
Goat protein is close to the protein of mother's milk and is absorbed by children better than cow's milk protein. But it should be remembered that normal weight helps to gain both the amount of food and the right mixture. Therefore, if the baby is healthy, then a mixture of goat's milk in sufficient quantities will provide the desired increase in weight. However, in case of problems with children's digestion, a therapeutic mixture is purchased on medical advice.
— Does protein saturation of baby food affect fatness?
- Low-protein breast milk contains only 0.9-1.1 g of proteins per 100 ml, but this allows the baby to develop normally physically.
It used to be thought that as children grow they need more protein, but this is not true. The increased content of protein leads to excessive development - paratrophy, obesity.
Nutrient mix MAMAKO ® Premium with a reduced protein index repeats the scheme and is created as close as possible to mother's milk, which is more physiological for children.
Protein content of goat milk infant formula:
- for children 0-6 months - 1.35 g/100 ml;
- for children 6-12 months - 1.5 g / 100 ml.
The dynamics of body weight depends on the age, nutrition, health of the baby and must be monitored by a doctor. If your baby is underweight, you should not self-medicate, since both overfeeding and underfeeding have a negative impact on health. It solves the problem at an early stage by correcting nutrition, the need for which can only be verified after a medical consultation. On natural feeding, the mother is offered to establish lactation or a dairy-free diet, on artificial nutrition - to introduce a therapeutic mixture. The pediatrician may also recommend increasing the volume of the milk formula or switching to goat milk formula to meet the needs of a healthy baby.
* Breast milk is the best food for babies. WHO recommends exclusive breastfeeding for the first 6 months of a child's life and continued breastfeeding after complementary foods are introduced until the age of 2 years.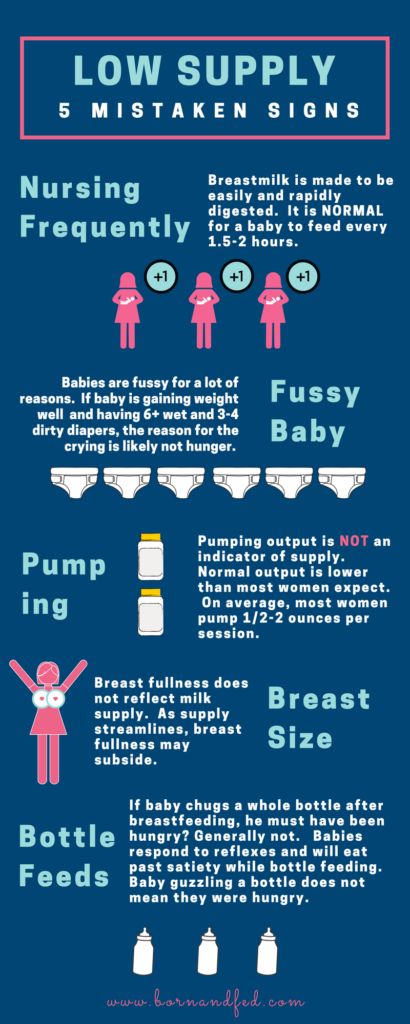 Before introducing new products into the baby's diet, you should consult with a specialist. The material is for informational purposes and cannot replace the advice of a healthcare professional. For feeding children from birth. The product is certified.
Before introducing new products into the baby's diet, you should consult with a specialist. The material is for informational purposes and cannot replace the advice of a healthcare professional. For feeding children from birth. The product is certified.
how to help them develop?
The birth of a small child is not uncommon today. Often, such babies are born on time or a little earlier, but due to a lack of weight, they can significantly lag behind their peers in development. Pediatricians and neuropathologists closely monitor the child's condition, because a child's body weight deficiency is a risk factor for changes in the neurological status, functional disorders of the cardiovascular and autonomic nervous systems. But because of their weakness, underweight children do not eat well, and the rate of weight gain in children born with low body weight determines their further physical and psychomotor development and the formation of the immune system.
How much weight should a newborn gain?
To assess the development of your child and the compliance with the norm of the main indicators (height, weight), you can contact a pediatrician or independently - according to existing tables. In the first months, the child is actively growing, adding up to 25-60 grams per day. Small children with adequate nutrition can increase body weight more intensively than their peers. For the first month of life, children should gain up to 1.3-1.7 kg. After 5-6 months of life, the intensity of weight gain decreases somewhat - in 30 days, the increase can be only 400-700 grams.
In the first months, the child is actively growing, adding up to 25-60 grams per day. Small children with adequate nutrition can increase body weight more intensively than their peers. For the first month of life, children should gain up to 1.3-1.7 kg. After 5-6 months of life, the intensity of weight gain decreases somewhat - in 30 days, the increase can be only 400-700 grams.
The length of the child's body during the first month increases by 4-7 cm, and after 5-6 months of life, growth is added less intensively - by 2-3 cm. But parents should understand that these figures are approximate. Each child is individual. Its weight and height depend on many factors: heredity, the quality of the mother's nutrition, the state of health of the newborn, the severity of childbirth.
Why is the child not gaining weight well?
The main cause of underweight in the neonatal period is the baby's refusal to breastfeed. Small children have poor appetite and spend most of the day sleeping. Often, parents have to wake up the child for a long time, and after a few minutes of sucking on the breast or a bottle of formula, the newborn falls asleep again. Children are especially sleepy, in whom pronounced physiological jaundice was observed in the first days of life.
Often, parents have to wake up the child for a long time, and after a few minutes of sucking on the breast or a bottle of formula, the newborn falls asleep again. Children are especially sleepy, in whom pronounced physiological jaundice was observed in the first days of life.
As a result, after the next weighing, the doctor can tell the mother that the newborn has not gained weight at all or the increase is insignificant. If the situation does not improve for several months, the mother and baby may be hospitalized for a comprehensive examination and tube feeding in a hospital setting.
Sometimes the cause of low weight gain lies in non-compliance with breastfeeding tactics. Pediatricians recommend applying the baby to only one breast during feeding so that it sucks out the "hind" milk, which is of particular energy value and rich in nutrients. Due to their inexperience, mothers offer both breasts to newborns. In this case, the child sucks the upper milk without making any effort and quickly falls asleep, slightly satisfying his hunger.
If the baby has had an infectious disease, been ill for a long time, suffered from a high fever or intestinal upset, then the monthly weight gain may be significantly less than usual. In this case, the timing of the introduction of complementary foods is also shifted, and during the period of illness, in general, many children practically refuse to eat, which is reflected in their weight. Parents should actively communicate with the pediatrician, if necessary, ask him questions of interest and adhere to all recommendations.
How to help a child gain weight and catch up with their peers in their development?
If you are breastfeeding, pay special attention to your diet. Drink as much liquid as possible: low-fat milk, compotes, hypoallergenic juices. Your diet must include boiled or baked meat. Take extra vitamins (as advised by the doctor). Breastfeed your baby immediately after waking up, when he is active, in a good mood and does not want to sleep.
But sometimes women's milk is produced in insufficient quantities or the baby does not have enough strength to suck it out.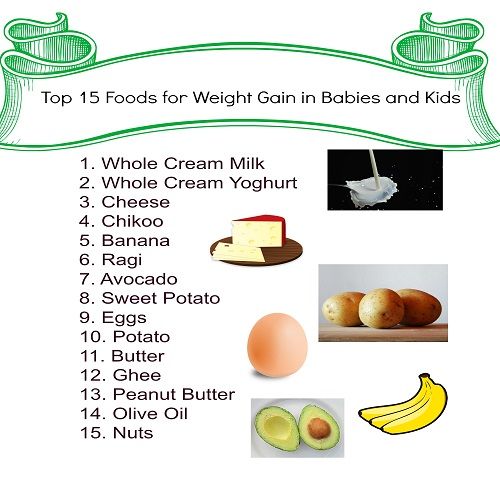 In this case, it is necessary to start supplementing with special infant formula as soon as possible. For children prone to allergic reactions, special hypoallergenic products are intended, which can be bought at a pharmacy, having previously discussed the mixture option with a pediatric nutritionist or pediatrician. Small babies are not adapted to intensive sucking, so the nipple on the bottle must be soft and pliable so that the child can fill up without problems.
In this case, it is necessary to start supplementing with special infant formula as soon as possible. For children prone to allergic reactions, special hypoallergenic products are intended, which can be bought at a pharmacy, having previously discussed the mixture option with a pediatric nutritionist or pediatrician. Small babies are not adapted to intensive sucking, so the nipple on the bottle must be soft and pliable so that the child can fill up without problems.
In addition, to increase the rate of weight gain and, accordingly, for the proper growth and development of the child, it is recommended to give courses of preparations containing L-carnitine (levorcarnitine), an essential vitamin-like substance that has anabolic properties and has proven itself to normalize body weight in case of its deficiency. In addition, by increasing the secretory and enzymatic activity of gastric and intestinal juices, appetite and digestion improve. One of these drugs is Elkar, containing an aqueous solution of L-carnitine. Elkar is included in the "National program for optimizing the feeding of children in the first year of life" as a means of correcting malnutrition of the II degree.
Elkar is included in the "National program for optimizing the feeding of children in the first year of life" as a means of correcting malnutrition of the II degree.
In children, in contrast to the adult body, where levocarnitine is among the substances produced, the synthesis of this compound covers only 1% of the required amount. Of course, the required amount of L-carnitine is found in breast milk, but if natural feeding is impaired or impossible, the drug must be added to the diet.
In underweight children, psychomotor development is often retarded, which can subsequently manifest itself in the form of speech defects, instability of the nervous system. Elcar improves the energy supply of brain activity, which will help to avoid or reduce the degree of development of functional failure in various areas of the child's neuropsychic response (motor, emotional-motivational, vegetative, cognitive spheres).
Another very important point: levocarnitine improves immunity, which is vital for small children, since almost all of them are predisposed to the development of infectious diseases.