Baby forgets to breathe when feeding
Breath-holding in babies and children
Breath-holding is when a baby or child stops breathing for up to 1 minute and may faint. It can happen when a child is frightened, upset, angry, or has a sudden shock or pain. It's usually harmless but can be scary for parents, particularly when it happens for the first time.
Immediate action required: Call 999 for an ambulance if your child:
- faints and cannot be woken up
- is shaking or jerking because of a fit
- is blue or grey
These could be symptoms of breath-holding, but could also be related to other, more serious conditions. If a doctor has not previously told you it's breath-holding, it's important to get it checked immediately.
What happens during breath-holding
During breath-holding, your child may:
- cry and then be silent while holding their breath
- open their mouth as if going to cry but make no sound
- turn blue or grey
- be floppy or stiff, or their body may jerk
- faint for 1 or 2 minutes
Your child may be sleepy or confused for a while afterwards.
Breath-holding is usually harmless
Although breath-holding can be scary for parents, it's usually harmless and your child should grow out of it by the age of 4 or 5.
Breath-holding episodes:
- usually last for less than 1 minute (if the child faints, they'll usually regain consciousness within 1 or 2 minutes)
- are not epileptic seizures
Your child is not doing it on purpose and cannot control what happens when they have a breath-holding episode.
What to do when a child has a breath-holding episode
Do
-
stay calm – it should pass in less than 1 minute
-
lie the child on their side – do not pick them up
-
stay with them until the episode ends
-
make sure they cannot hit their head, arms or legs on anything
-
reassure them and ensure they get plenty of rest afterwards
Don’t
-
do not shake your child or splash them with water
-
do not put anything in their mouth (including your fingers)
-
do not give them mouth-to-mouth or CPR
-
do not tell them off (they're not doing it deliberately)
Non-urgent advice: See a GP if:
your child has already been diagnosed with breath-holding and:
- has breath-holding episodes more often than before or the episodes seem worse
- is stiff or shakes for longer than a minute and takes a while to recover
- has breath-holding episodes that are affecting everyday life
The GP will try to find out if there's a more serious underlying condition. They may suggest an ECG to check your child's heart rhythm.
They may suggest an ECG to check your child's heart rhythm.
Treatments for breath-holding
There's no specific treatment for breath-holding. It should eventually stop by the time your child is 4 or 5 years old.
Medicines are rarely used to treat breath-holding.
Breath-holding is sometimes related to iron deficiency anaemia.
Your child's blood iron levels may be checked. They may need iron supplements if their iron levels are low.
Causes of breath-holding
Breath-holding is usually triggered by a sudden shock or pain, or strong emotions like fear, upset or anger.
There are 2 types of breath-holding:
Blue breath-holding spells
This is the most common type of breath-holding and happens when a child's breathing pattern changes.
Reflex anoxic seizures
This type of breath-holding happens when a child's heart rate slows down.
Information:
Find out more
- The Syncope Trust And Reflex anoxic Seizures (STARS) – reflex anoxic seizures
Page last reviewed: 26 November 2019
Next review due: 26 November 2022
Brief resolved unexplained event - BRUE: MedlinePlus Medical Encyclopedia
A brief resolved unexplained event (BRUE) is when an infant younger than one year stops breathing, has a change in muscle tone, turns pale or blue in color, or is unresponsive. The event occurs suddenly, lasts less than 30 to 60 seconds, and is frightening to the person caring for the infant.
BRUE is present only when there is no explanation for the event after a thorough history and exam.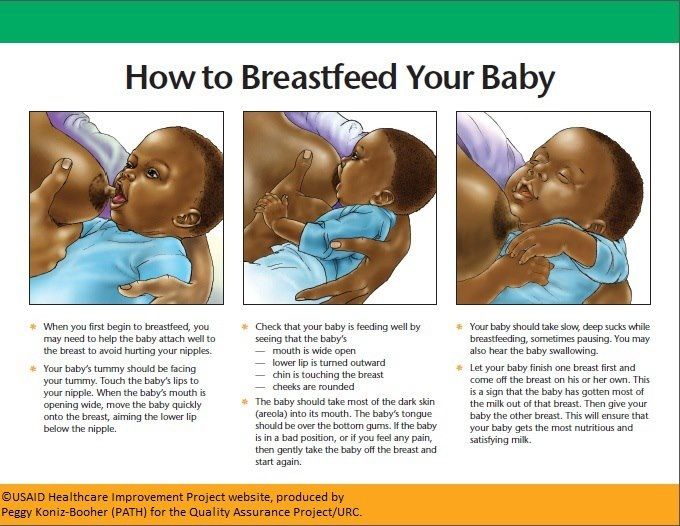 An older name used for these types of events is an apparent life-threatening event (ALTE).
An older name used for these types of events is an apparent life-threatening event (ALTE).
It is unclear how often these events occur.
BRUE is NOT the same as sudden infant death syndrome (SIDS). It is also NOT the same as older terms such as "near-miss SIDS" or "aborted crib deaths," which are no longer used.
Events that involve a change in an infant's breathing, color, muscle tone, or behavior may be caused by an underlying medical problem. But these events would then NOT be considered a BRUE. Some of the causes for events that are not a BRUE include:
- Reflux after eating
- Severe infections (such as bronchiolitis, whooping cough)
- Birth defects that involve the face, throat, or neck
- Birth defects of the heart or lungs
- Allergic reactions
- A brain, nerve, or muscle disorder
- Child abuse
- Certain uncommon genetic disorders
A specific cause of the event is found about half the time. In healthy children who only have one event, the cause is rarely identified.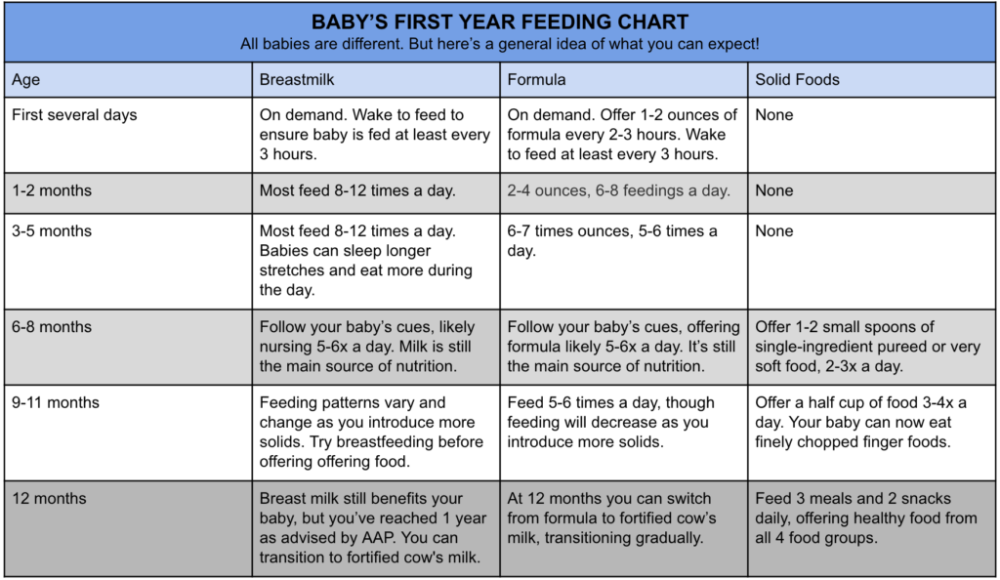
The main risk factors for BRUE are:
- A prior episode when the child stopped breathing, turned pale, or had blue coloring
- Feeding problems
- Recent head cold or bronchitis
- Age younger than 10 weeks
Low birth weight, being born early, or secondhand smoke exposure also may be risk factors.
These events are more likely to occur during the first two months of life and between 8 a.m. and 8 p.m.
A BRUE includes one or more of the following:
- Breathing changes -- either no effort at breathing, breathing with great difficulty, or decreased breathing
- Color change -- most often blue or pale (many infants turn red, when crying for example, so this does not indicate a BRUE)
- Change in muscle tone -- most often they are limp, but they may become rigid
- Change in level of responsiveness
Choking or gagging means the event was likely not a BRUE. These symptoms are more likely caused by reflux.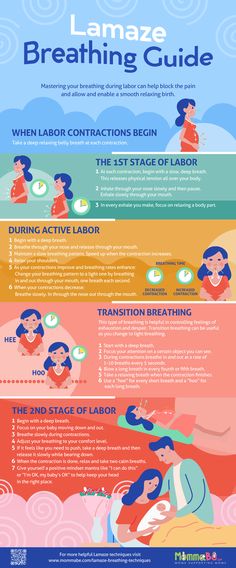
The health care provider will ask you to describe what occurred during the event. The provider will also ask about:
- Other events like this one in the past
- Other known medical problems
- Medicines, herbs, or extra vitamins the infant may be taking
- Other medicines at home the child could have taken
- Complications during pregnancy and labor, or at birth, or being born early
- Siblings or children in the household who also had this type of event
- Illegal drugs or heavy alcohol use in the house
- Prior reports of abuse
When deciding if more testing is needed, the provider will consider:
- The type of event that occurred
- How severe the symptoms were
- What was going on right before the event
- Other health problems that are present or that are found on physical exam
A thorough physical exam will be done, checking for:
- Signs of infection, trauma, or abuse
- Low oxygen level
- Abnormal heart sounds
- Signs of birth defects that involve the face, throat, or neck that may cause breathing problems
- Signs of abnormal brain function
If there are no findings to suggest a high-risk BRUE, lab tests and imaging tests are often not needed. If choking or gasping occurred during feeding and the infant recovered quickly, more testing will often not be needed.
If choking or gasping occurred during feeding and the infant recovered quickly, more testing will often not be needed.
Factors that suggest a higher risk for recurrence or the presence of a serious cause include:
- Infants under 2 months of age
- Being born at 32 weeks or earlier
- More than 1 event
- Episodes lasting longer than 1 minute
- CPR by a trained provider was needed
- Signs of child abuse
If risk factors are present, testing that may be done includes:
- A complete blood count (CBC) to look for signs of infection or anemia.
- A metabolic profile to look for problems with how the kidneys and liver are working. Abnormal levels of calcium, protein, blood sugar, magnesium, sodium, and potassium may also be found.
- Urine or blood screen to look for drugs or toxins.
- Chest x-ray.
- Holter monitoring or echocardiogram for heart problems.
- CT or MRI of the brain.
- Laryngoscopy or bronchoscopy.
- Tests to evaluate the heart.
- Test for pertussis.
- Sleep study.
- X-rays of the bones looking for prior trauma.
- Screening for different genetic disorders.
If the event was brief, included no signs of breathing or heart problems, and corrected on its own, your child will likely not need to stay in the hospital.
Reasons your child may be admitted overnight include:
- The event included symptoms that indicate a more serious cause.
- Suspected trauma or neglect.
- Suspected poisoning.
- The child appears unwell or is not thriving well.
- Need to monitor or observe while feeding.
- Concern over ability of parents to care for child.
If admitted, your child's heart rate and breathing will be monitored.
The provider may recommend that you and other caregivers:
- Place your infant on his back when sleeping or napping. His face should be free.
- Avoid soft bedding materials.
 Babies should be placed on a firm, tight-fitting crib mattress without loose bedding. Use a light sheet to cover the baby. Do not use pillows, comforters, or quilts.
Babies should be placed on a firm, tight-fitting crib mattress without loose bedding. Use a light sheet to cover the baby. Do not use pillows, comforters, or quilts. - Avoid exposure to secondhand smoke.
- Consider saline nose drops or using a nasal bulb if the nose is congested.
- Learn proper techniques to respond to any future events. This includes NOT shaking the infant. Your provider can instruct you.
- Avoid overfeeding, perform frequent burping during feedings, and hold the infant upright after feeding.
- Talk to your provider before thickening your child's feedings or using medicines that reduce acid and reflux.
Although not common, home monitoring devices may be recommended.
Most often, these events are harmless and not a sign of more serious health problems or death.
BRUE is unlikely to be a risk for sudden infant death syndrome (SIDS). Most victims of SIDS do not have any types of events beforehand.
A child with risk factors for BRUE may have a higher risk for recurrence or the presence of a serious cause.
Call the provider right away if child abuse is suspected. Possible signs of abuse include:
- Poisoning or head injury that are not caused by an accident
- Bruising or other signs of a prior injury
- When events occur only in the presence of a single caretaker when no health problems are found as the cause for these events
Apparent life-threatening event; ALTE
Marcdante KJ, Kliegman RM. Control of breathing. In: Marcdante KJ, Kliegman RM, eds. Nelson Essentials of Pediatrics. 8th ed. Philadelphia, PA: Elsevier; 2019:chap 134.
Tieder JS, Bonkowsky JL, Etzel RA, et al; Subcommittee on Apparent Life Threatening Events. Brief resolved unexplained events (formerly apparent life-threatening events) and evaluation of lower-risk infants. Pediatrics. 2016;137(5). PMID: 27244835 pubmed.ncbi.nlm.nih.gov/27244835/.
Updated by: Amit M. Shelat, DO, FACP, FAAN, Attending Neurologist and Assistant Professor of Clinical Neurology, Renaissance School of Medicine at Stony Brook University, Stony Brook, NY. Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Review provided by VeriMed Healthcare Network. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
How to get rid of sleep apnea while feeding a baby?
Home→Articles → Patients→Topical topics→Apnea while feeding a baby: how to make the baby breathe normally?
Apnea is the most common breathing control problem in infants. There are many reasons for this state of affairs. Most often, the nervous system or pathological diseases are not sufficiently formed.
New mothers often complain that the baby stops breathing during feeding. Moreover, when breastfeeding, this happens much less often than when feeding from a bottle. When the baby eats with "greed", begins to choke, the breath disappears, then he turns blue, clears his throat in a moment and continues to eat.
The simplest thing pediatricians advise is bottle feeding in a position close to vertical. The head should be slightly tilted forward. In this position, the chances of choking are much less. Also:
In this position, the chances of choking are much less. Also:
- The bottle can be taken out periodically to let the baby catch his breath.
- To avoid problems with breathing, it is recommended to feed in a crib on the side.
What causes such apnea, the treatment of which also requires a serious approach? Doctors in most cases attribute this to prematurity. The shorter the gestation period, the more frequent the occurrence of apnea during feeding. In addition, more children with low weight suffer from this disease.
Apnea during feeding of a premature baby
There are many reasons for such apnea. Premature babies, as a rule, have an immature respiratory center, which means that the mechanism that regulates breathing is imperfect. As for the feeding reflexes, we are talking about swallowing, sucking, they are also not quite active. Their activities are poorly coordinated.
In addition, in premature babies, the work of the muscle fibers of the soft palate, as well as nearby tissues, is disrupted.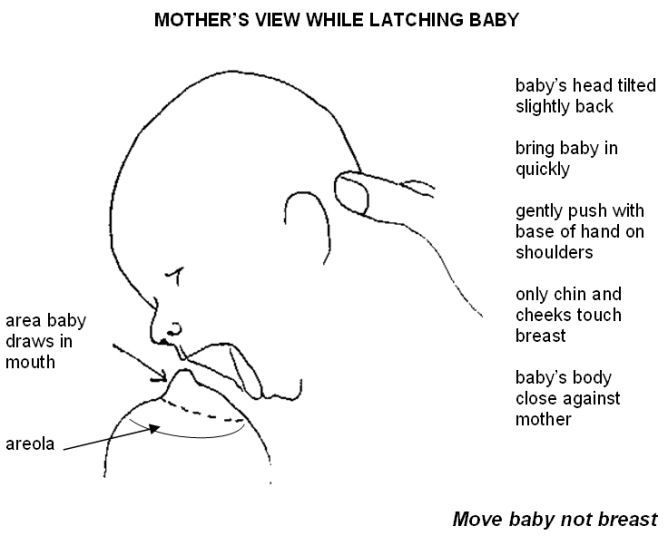 They sag when feeding on the back and apnea is clearly manifested. When feeding on the side, the baby suffers less from breathing problems, or there are no problems at all.
They sag when feeding on the back and apnea is clearly manifested. When feeding on the side, the baby suffers less from breathing problems, or there are no problems at all.
This is important!
Statistics show that babies born before 29 weeks can suffer from apnea during feeding in 80% of cases, half of babies born at 30-31 weeks and 10% of babies born after 32 weeks .
The baby may choke on milk with strong pressure. If the baby is breastfed, you can first express a little milk, and if he is bottle-fed, reducing the hole in the nipple helps.
What should a mother do if her baby has an apnea attack? First, stop feeding and try to "stir up" the child. If at the same time breathing is not restored, then you need to do artificial respiration.
In severe cases, go to chest compressions. For such young children, it is done by means of the thumbs, placing the rest of the fingers on the back of the child. Pushes should be carried out often, after every 5 pushes, mouth-to-mouth breathing should be done.
Remember that feeding apnea requires systematic medical prevention of seizures. To do this, oxygen is given to a premature baby before and after feeding. And, of course, in case of apnea in infants, it is always worth consulting a doctor once again.
You might be interested
Snoring in men: causes, effects and remedies
How to choose an oxygen concentrator supplier?
Apnea during pregnancy: causes, treatment, prevention
Discomfort in the chest (feeling full, muscle pain due to increased work of the respiratory muscles)
Breathe to eat?!
08/15/2016
The topic of breastfeeding is very relevant both for those who are just preparing to become a mother, and for those who are already clutching their first child to their breasts. Mother's milk is truly the best food that can only be offered to a child up to a year old. It helps the baby grow healthy and strengthens his immunity. That is why it is especially necessary for a child in the first six months of life. Breast milk contains all the necessary nutrients for the baby, and in the optimal ratio and form, adapted to the characteristics of the digestive system of the newborn. In addition, it is rich in vitamins, enzymes, minerals and contributes to the creation of the necessary conditions for the formation of the "correct" intestinal microbial biocenosis.
Breast milk contains all the necessary nutrients for the baby, and in the optimal ratio and form, adapted to the characteristics of the digestive system of the newborn. In addition, it is rich in vitamins, enzymes, minerals and contributes to the creation of the necessary conditions for the formation of the "correct" intestinal microbial biocenosis.
In addition, during breastfeeding there is direct communication between mother and child, which contributes to the formation of a positive emotional bond between them. The very act of sucking is extremely important for the baby. Sucking for an infant is a need and a pleasure that is not directly related to the feeling of hunger. Thanks to sucking, the baby develops the jaw apparatus, muscles of the mouth and tongue, which is especially important in the future, for example, in the development of speech.
But sometimes the process of feeding may not go as smoothly as a mother would like. One of the most common reasons a baby refuses to breastfeed is difficulty in breathing through the nose. A significant role in the development of this condition is given to the physiological characteristics of the nasal mucosa of the newborn, as well as the anatomical features of the child's nose. In an infant, the nasal passages are much wider and shorter, the mucous lining the nasal cavity is thickened and rich in a dense network of blood vessels, while the number of glands that produce mucus is not yet large. Even a small swelling of the mucosa can block nasal breathing. During breastfeeding, the baby has to suck and breathe at the same time, and if the nose is clogged, it is simply impossible to combine these processes. If the baby does not breathe through the nose, feeding turns into torment - the baby cannot suckle without interruption, because he is suffocating.
A significant role in the development of this condition is given to the physiological characteristics of the nasal mucosa of the newborn, as well as the anatomical features of the child's nose. In an infant, the nasal passages are much wider and shorter, the mucous lining the nasal cavity is thickened and rich in a dense network of blood vessels, while the number of glands that produce mucus is not yet large. Even a small swelling of the mucosa can block nasal breathing. During breastfeeding, the baby has to suck and breathe at the same time, and if the nose is clogged, it is simply impossible to combine these processes. If the baby does not breathe through the nose, feeding turns into torment - the baby cannot suckle without interruption, because he is suffocating.
The child constantly has to let go of the chest in order to breathe in air through the mouth. This is repeated several times, and as a result, the baby drops the breast. In addition, swallowing air through the mouth contributes to its entry into the stomach, followed by regurgitation of its contents. Frequent regurgitation, in turn, contributes to irritation of the nasal mucosa and nasopharynx with gastric contents and the development of inflammation - rhinitis, which is manifested by prolonged difficulty in nasal breathing.
Frequent regurgitation, in turn, contributes to irritation of the nasal mucosa and nasopharynx with gastric contents and the development of inflammation - rhinitis, which is manifested by prolonged difficulty in nasal breathing.
That is why it is so important for newborns to pay close attention to nasal hygiene to ensure and maintain free nasal breathing. On the Internet, you can find recommendations advising mothers to instill vasoconstrictors for babies in the nose of babies before feeding. Such advice can be useful only if the child has a runny nose, in all other cases, one should be aware of side effects and the inadmissibility of long-term use of such drugs, as well as the need to consult a doctor.
For daily care and cleansing of the nasal mucosa, special products based on natural sea water have been developed. One of these products is the RINOSTOP® AQUA product line.
RINOSTOP® AQUA contains 100% natural sea water, widely known for its beneficial properties. No preservatives, stabilizers or other chemicals that can cause irritation of the nasal mucosa are used in the process of production and purification of water; preserved macro- and microelements of natural sea water (K, Mg, Na, Ca, Cl).
No preservatives, stabilizers or other chemicals that can cause irritation of the nasal mucosa are used in the process of production and purification of water; preserved macro- and microelements of natural sea water (K, Mg, Na, Ca, Cl).
The products of the line are available in bottles of different sizes; equipped with nozzles that take into account the anatomical structure of the nose and provide a continuous spray of water of different intensity - in the form of a jet, shower or soft shower.
The special design of the "BAG-ON-VALVE" bottles allows the use of funds in any position of the bottles with a full consumption of the contents without residue.
RINOSTOP® AQUA BABY is perfect for daily hygiene and moisturizing of little noses from birth. It contains sea water in an isotonic concentration close in its physiological characteristics to human plasma. Micro-diffusion water supply in the form of a soft shower provides:
- gentle care for the delicate nasal mucosa of babies;
- uniform irrigation of the entire surface of the mucosa by spraying sea water in the form of tiny particles mixed with air - "water vapor"; it is this spray that minimizes the risk of getting into the middle ear cavity;
- cleansing of mucus, crusts, dust and small foreign particles;
- maintaining the normal physiological state of the mucous membrane of the nasal cavity and facilitating nasal breathing of babies, contributing to the normalization of good sleep and optimizing the process of breastfeeding;
- moisturizing the nasal mucosa of infants, incl.