Baby ounces per feeding
Formula Feeding FAQs: How Much and How Often (for Parents)
Whether you plan to formula feed your baby from the start, want to supplement your breast milk with formula, or are switching from breast milk to formula, you probably have questions.
Here are answers to some common questions about formula feeding.
How Often Should I Feed My Baby?
Newborns and young babies should be fed whenever they seem hungry. This is called on-demand feeding.
After the first few days of life, most healthy formula-fed newborns feed about every 2–3 hours. As they get bigger and their tummies can hold more milk, they usually eat about every 3–4 hours. As babies get older, they’ll settle into a more predictable feeding routine and go longer stretches at night without needing a bottle.
Talk to your doctor if you have concerns about feeding your baby, especially if your baby is very small, is not gaining weight, or was born early (prematurely).
How Can I Tell When My Baby Is Hungry?
Signs that babies are hungry include:
- moving their heads from side to side
- opening their mouths
- sticking out their tongues
- placing their hands, fingers, and fists to their mouths
- puckering their lips as if to suck
- nuzzling again their mothers' breasts
- showing the rooting reflex (when a baby moves its mouth in the direction of something that's stroking or touching its cheek)
Babies should be fed before they get upset and cry. Crying is a late sign of hunger. But every time your baby cries is not because of hunger. Sometimes babies just need to be cuddled or changed. Or they could be sick, tired, too hot or too cold, in pain, or have colic.
How Much Should My Baby Drink?
In the first few weeks, give 2- to 3-ounce (60- to 90-milliliter) bottles to your newborn. Give more or less depending on your baby’s hunger cues.
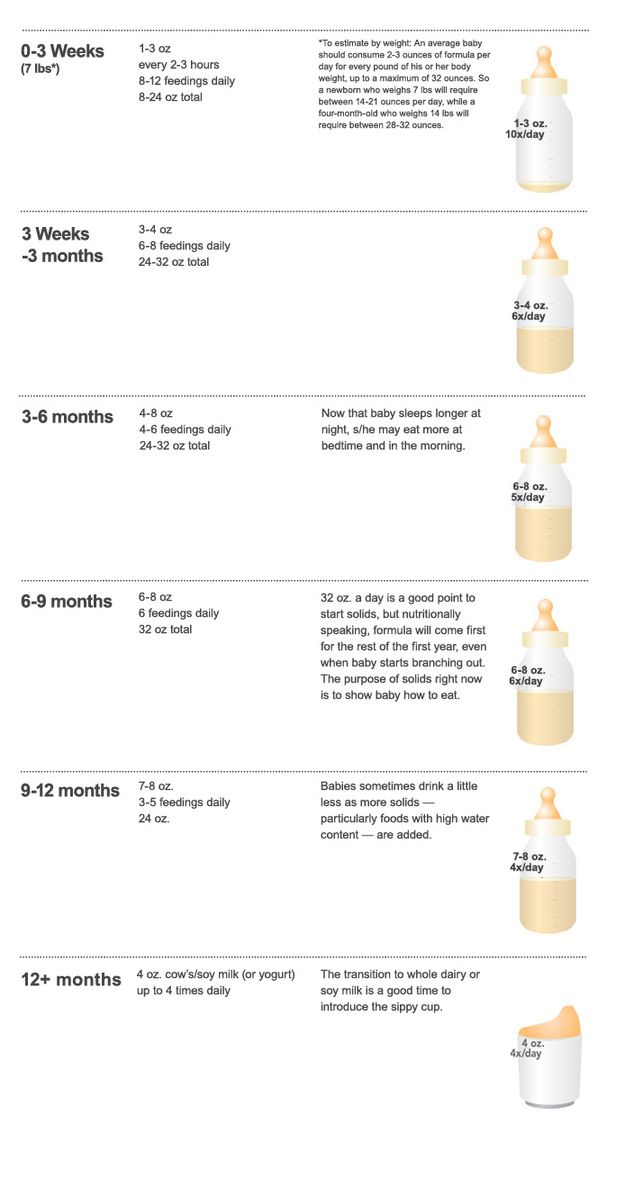
Here's a general look at how much your baby may be eating at different ages:
- On average, a newborn drinks about 1.5–3 ounces (45–90 milliliters) every 2–3 hours. This amount increases as your baby grows and can take more at each feeding.
- At about 2 months, your baby may drink about 4–5 ounces (120–150 milliliters) every 3–4 hours.
- At 4 months, your baby may drink about 4–6 ounces (120-180 milliliters) at each feeding, depending on how often they eat.
- By 6 months, your baby may drink 6–8 ounces (180–230 milliliters) about 4–5 times a day.

Watch for signs that your baby is hungry or full. Respond to these cues and let your baby stop when full. A baby who is full may suck with less enthusiasm, stop, or turn away from the bottle.
Why Does My Baby Seem Hungrier Than Usual?
As babies grow, they begin to eat more at each feeding and can go longer between feedings. Still, there may be times when your little one seems hungrier than usual.
Your baby may be going through a period of rapid growth (called a growth spurt). These can happen at any time, but in the early months are common at around:
- 7–14 days old
- between 3–6 weeks
- 4 months
- 6 months
During these times and whenever your baby seems especially hungry, follow their hunger cues and continue to feed on demand, increasing the amount of formula you give as needed.
Is My Baby Eating Enough?
At times, you may wonder whether your baby is getting enough nutrients for healthy growth and development. Babies who get enough to eat seem satisfied after eating and are regularly peeing and pooping.
Babies who get enough to eat seem satisfied after eating and are regularly peeing and pooping.
At your baby’s checkups, the doctor will review your baby’s growth chart, track your little one’s development, and answer any questions. Talk to your doctor if you have any concerns about your baby’s feeding and nutrition.
Reviewed by: Mary L. Gavin, MD
Date reviewed: November 2021
How Often and How Much Should Your Baby Eat?
By: Sanjeev Jain, MD, FAAP
One of the most common questions new parents have is how often their baby should eat. The best answer is surprisingly simple: in general, babies should be fed whenever they seem hungry.
How do I know when my baby is hungry?
For babies born
prematurely or with certain medical conditions, scheduled feedings advised by your pediatrician are best. But for most healthy, full-term infants, parents can look to their baby rather than the clock for hunger cues. This is called feeding on demand, or
responsive feeding.
This is called feeding on demand, or
responsive feeding.
Hunger cues
A hungry baby often will cry. But it's best to watch for hunger cues before the baby starts crying, which is a late sign of hunger and can make it hard for them to settle down and eat.
Some other typical hunger cues in babies:
Licking lips
Sticking tongue out
Rooting (moving jaw and mouth or head in search of breast)
Putting his/her hand to mouth repeatedly
Opening her mouth
Fussiness
Sucking on everything around
It is important to realize, however, that every time your baby cries or sucks it is not necessarily because he or she is hungry. Babies suck not only for hunger, but also for comfort; it can be hard at first for parents to tell the difference. Sometimes, your baby just needs to be cuddled or changed.
General guidelines for baby feeding
It is important to remember all babies are different―some like to snack more often, and others drink more at one time and go longer between feedings. However, most babies will drink more and go longer between feedings as they get bigger and their tummies can hold more milk:
However, most babies will drink more and go longer between feedings as they get bigger and their tummies can hold more milk:
Most newborns eat every 2 to 3 hours, or 8 to 12 times every 24 hours. Babies might only take in half ounce per feeding for the first day or two of life, but after that will usually drink 1 to 2 ounces at each feeding. This amount increases to 2 to 3 ounces by 2 weeks of age.
At about 2 months of age, babies usually take 4 to 5 ounces per feeding every 3 to 4 hours.
At 4 months, babies usually take 4 to 6 ounces per feeding.
At 6 months, babies may be taking up to 8 ounces every 4 to 5 hours.
Most babies will increase the amount of formula they drink by an average of 1 ounce each month before leveling off at about 7 to 8 ounces per feeding.
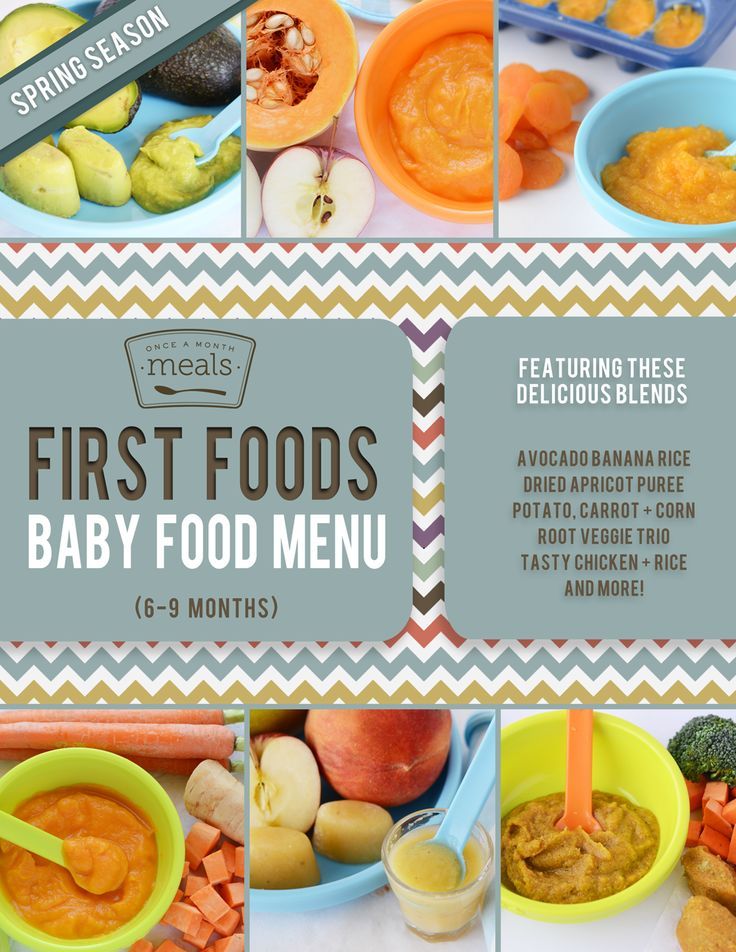
Solid foods should be started at about 6 months old.
Concerns about overfeeding or underfeeding your baby
Too full?
Babies are usually pretty good at eating the right amount, but they can sometimes take in more than they need. Infants who are bottle feeding may be more likely to overfeed, because drinking from a bottle may take less effort than breastfeeding.
Overfed babies can have stomach pains, gas, spit up or vomit and be at higher risk for obesity later in life. It's better to offer less, since you can always give more if your baby wants it. This also gives babies time to realize when they're full.
If you are concerned your baby wants to eat
all the time―even when he or she is full―talk with your pediatrician.
Pacifiers may be used after feeding to help sooth healthy-weight babies who like to suck for comfort, rather than nutrition. For babies who are breastfed, it's best to wait to offer pacifiers until around 3 to 4 weeks of age, when breastfeeding is well-established.
Trouble gaining weight?
Most babies will double their birth weight by 5 months of age and triple their birth weight by their first birthday. If your baby is having trouble gaining weight, don't wait too long between feeding―even if it means waking your baby. Be sure to talk with your pediatrician about how often and how much to feed your baby.
How do I know if my baby is getting enough to eat?
Daily diapers
A newborn's diaper is a good indicator of whether he or she is getting enough to eat. In the first few days after birth, a baby should have 2 to 3 wet diapers each day. After the first 4 to 5 days, a baby should have at least 5 to 6 wet diapers a day. Stool frequency is more variable and depends whether your baby is breastfed or formula fed.
Growth charts
During regular health check-ups, your pediatrician will check your baby's weight and plot it on a
growth chart. Your baby's progress on the growth chart is one way to tell whether or not they are getting enough food. Babies who stay in healthy growth percentile ranges are
probably getting a healthy amount of food during feedings.
Babies who stay in healthy growth percentile ranges are
probably getting a healthy amount of food during feedings.
Remember
Talk with your pediatrician if you have any questions or concerns about your baby getting the right amount to eat.
More information:
- Making Sure Your Baby is Getting Enough Milk
- Amount and Schedule of Formula Feedings
- Is Your Baby Hungry or Full? Responsive Feeding Explained (Video)
- Remedies for Spitty Babies
- Ask the Pediatrician: With the baby formula shortage, what should I do if I can't find any?
- Ask the Pediatrician: How should we feed our baby if we're running low on money?
-
Airplane Choo Choo: A Feeding Guide for Children (National Dairy Council)
About Dr. Jain:
Sanjeev Jain, MD, FAAP, is a Clinical Associate Professor of General Pediatrics and Adolescent Medicine at the University of Wisconsin School of Medicine and Public Health. Within the American Academy of Pediatrics, he is a member of the Section on International Child Health and the Wisconsin State Chapter.
Within the American Academy of Pediatrics, he is a member of the Section on International Child Health and the Wisconsin State Chapter.
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
Baby formula cake
One of the best solutions is mastic. It allows you to unfold your imagination and realize the most daring ideas! And we have collected 16 recipes for you, choose to your liking! Well, then - create! For inspiration, you can use our selection of amazing cakes
How to make fondant for cake
1. SUGAR PASTE
20 g gelatine
9 tbsp. l. cold water
juice of 0.5 lemon
powdered sugar (as much as you need to get an elastic mass)
Rinse gelatin and soak in cold water for 2-3 hours (it should swell). Then heat it up to 55 degrees to melt it. Strain the hot melted gelatin, then cool to 25-30 degrees and combine with the sifted powdered sugar, stirring constantly, until a homogeneous mass is obtained. It should be elastic, not stick to your hands and not crumble. Then add lemon juice.
Then heat it up to 55 degrees to melt it. Strain the hot melted gelatin, then cool to 25-30 degrees and combine with the sifted powdered sugar, stirring constantly, until a homogeneous mass is obtained. It should be elastic, not stick to your hands and not crumble. Then add lemon juice.
2. MARSHLINE MASTIC
per 1000 g:
470 g sugar, 12.5 g gelatin, 2 egg whites, 1 g citric acid, 150 g water, 500 g powdered sugar.
Soak gelatine in cold water. Beat the egg whites until 5 times the volume. Make syrup from sugar and water. In the finished syrup, put the swollen gelatin, citric acid and mix everything. Pour into beaten egg whites. Then add powdered sugar and mix.
This mastic has a delicate texture and should be stored in a container covered with a damp cloth.
3. SUGAR GELATIN MASTIC
1 kg. powdered sugar
1.5 tbsp. l. gelatin
0.25 cups of water
Gelatin is soaked in water (1:2) for 1 hour, put on a slow fire and heated with stirring until completely dissolved (I diluted it as indicated on the package) . . Then the mixture is filtered (if need?), add powdered sugar and mix. This mask dries VERY quickly. It’s even more likely not mastic, but pastilage.”
. Then the mixture is filtered (if need?), add powdered sugar and mix. This mask dries VERY quickly. It’s even more likely not mastic, but pastilage.”
4. COATING MASTIC
powdered sugar 500g
gelatine 12g
cold water 35g
corn syrup 80g (or any other without color)
protein 1 pc
coconut fat a little (1-2 teaspoons)
lemon juice 1 teaspoon
1. sift sugar Powder
2. Pour COLD WATER into a separate bowl, add gelatine and mix until pureed
3. put a cup of gelatin in a steam bath, add a little coconut fat, stir constantly until the gelatin melts
4. add the syrup and also stir constantly until it “melts”, the syrup should “mix” well with gelatin
5. add the mixture with gelatin to the sugar powder, mix a little and add protein hands are not sticky, grease your hands well with coconut fat) put in a container or bag. leave for a day.
Do not add powdered sugar, even if the mastic seems soft during kneading.
5. CHOCOLATE GASTE
CHOCOLATE GASTE
100 g dark chocolate
90 g marshmallows (color does not matter)
40 ml cream (30)
1/2-1 tbsp butter
90-120 g icing sugar
1-2 tbsp cognac
Method of preparation
First make the mastic :
Put the broken chocolate into a saucepan and place over low heat
Melt completely
Without removing the saucepan from the heat, add the marshmallows to the melted chocolate and stir constantly with a spoon. and cognac
Stir without ceasing until a homogeneous thick liquid mass is obtained.
Remove from fire.
While constantly stirring with a spoon, gradually pour in the sifted powdered sugar.
When the mass turns out to be too thick and elastic and it will no longer be convenient to interfere with a spoon - do it with your hands.
Pour in powdered sugar until the mass feels like a warm, tight, elastic dough.
It absolutely does not stick to hands - on the contrary, hands remain clean, but greasy.
Roll the mixture into a ball and place on baking paper.
Cover with another sheet of paper on top.
And roll out to the desired thickness.
Remove the top sheet of paper.
Mastic is ready.
It turns out to be barely warm, very soft and tender.
You can store it in a tightly closed form in the refrigerator, and slightly warm it up in the micro before the next use.
6. CHOCOLATE AND MARSHMELLA MASTIC
150 gr. sugar powder
200 gr. dark chocolate
180 gr. marshmallow (any color)
1 tbsp. l. butter or margarine or vegetable fat
3 Art. l. cream
1 st. l. liqueur or orange juice (optional)
1. Melt the chocolate in the steam bath.
2. Add marshmallows, mix with chocolate and continue melting.
3. Add cream and margarine. Interfere.
4. Into the mixer (guitar attachment, i.e. dough attachment), prepare the sugar. powder and add the liquid mixture.
5. Mix until a homogeneous dough.. the mastic is ready. Transfer to a bag and chill for a day. After getting it, let it warm up and knead again. It is better to roll out on a film.
Transfer to a bag and chill for a day. After getting it, let it warm up and knead again. It is better to roll out on a film.
6. Store in the same way as other mastics.
With white chocolate: instead of cream, I took milk and butter 1 tsp. Then it can be mixed even with marzipan, even with ordinary mastic, even with gelatin.
7. SUGAR PASTE
Ingredients:
powdered sugar 200 g
vegetable margarine 50 g
honey 1 tbsp. spoon
food coloring
Sift powdered sugar and mix it with margarine and honey. Add dye (optional). Roll the prepared mass into a ball. If needed, add more powdered sugar. Balls, flowers, etc. are molded from such a paste (you can use molds). If you're not going to use the paste right away, put it in the freezer and keep it there until you need it.
8. GELATIN MASTIC
The recipe is very simple from freely available products, without any CMC and glycerin:
Gelatin -12 gr.
water - 50 ml
egg white - 1 pc.
lemon juice - 1 tsp.
sugar powder - 1kg.
Add the starch to the powder, then the egg yolk. Soak gelatin, add lemon juice, heat to dissolve, pour into powder, water and knead an elastic dough, let it rest in the refrigerator.
9. How to make marshmallows at home
450g. sugar
15ml. glucose
8 drops van. aromas
25g. gelatin powder
2 egg whites
3-4 tbsp. l. starch
3-4 tbsp. l. sugar powder
pods. oil for form
- Sugar, glucose and 200 ml. Heat water and stir until sugar melts. Cook with the lid closed for about 3 minutes. Add van. aromas.
- Pour 100 ml of gelatin into a metal bowl. water, melt in a water bath.
- Whisk the whites to peaks.
- Pour the syrup into the egg whites in a thin stream, while stirring. Also gelatin. Beat 10 min. until the mass is stable.
- Mix starch and powder in a deep bowl (needed later)
- Lubricate a square mold with oil and sprinkle with a mixture (starch powder)
- Pour marshmallow cream into a mold, smooth and refrigerate for 4 hours.
- Sprinkle the table with the mixture, put the marshmallow on the table. Can be extruded into a round shape or cut into 3 by 3cm squares.
- Put squeezed or cut out marshmallows into a bowl with the mixture and mix everything well so that they do not stick to each other.
- You can melt the chocolate and dip the finished marshmallows halfway into the chocolate, cool.
10. Recipe for marshmallows
500 gr. sugar
350 ml. water
1 c. spoonful of glucose
30 gr. gelatin
2 proteins
powdered sugar
starch.
pour 200 ml. Bring sugar and glucose water to a boil. Dissolve
gelatin in the remaining water.
and start whipping the whites (turning the bowl does not fall).
mix gelatin with syrup and stir strongly and pour in while beating egg whites without stopping (the mass will become thick). Line
with parchment or sprinkle with powdered sugar mixed with starch in equal parts.
transfer everything into a syringe and squeeze out balls or spread evenly
11. SUGAR MASTIC on molasses.
SUGAR MASTIC on molasses.
You will need: gelatin - 10 g, water - 150 g, powdered sugar - 930 g, molasses - 50 g, fruit essence - 0.5 g.
You should get about a kilogram of mastic. Gelatin is washed by pouring it with cold water, then the water is drained, and the gelatin is again filled with water (its temperature should not exceed 20-25 degrees C). Let it swell (about 2 hours), put on low heat and heat until it is completely dissolved. The sifted icing sugar is poured in a pile on a wooden or marble table (the powder darkens from aluminum), a recess is made in it, into which molasses, dissolved gelatin and fruit essence are poured. Mix quickly to obtain a homogeneous white or slightly grayish mass. From this disgrace, they recommend sculpting flowers.
12. MASTIC ON GELATIN
You will need: 2 tbsp. l. cold water, 1.5 tsp. gelatin, 1.5 tbsp. l. liquid glucose, 2 tsp. glycerin, 450 gr of powdered sugar.
Pour gelatine with water and allow to swell. Then heat the gelatin on the stove until it dissolves, but DO NOT boil, add glucose and glycerin. Stir and gradually add the sifted icing sugar, knead the mastic first in a bowl, then on the table.
Stir and gradually add the sifted icing sugar, knead the mastic first in a bowl, then on the table.
Bird's milk mastic
Cut frozen "Bird's milk" coffees into 2 by 2 squares, roll them in powdered sugar. Warm up in the microwave, add powdered sugar and knead a tight mastic. It is better to sculpt if it lies down for 2-3 hours. Keeps for a long time. If it becomes harsh, warm up in a microwave oven for about 10 seconds. and you can sculpt further.
13. SUGAR AND STARCH MASTIC
800 g sugar. powder, 200 g of corn starch, citric acid at the tip of a teaspoon, 1 cup of water.
Dissolve a pinch of citric acid in a glass of water and bring to a boil. In 4 tbsp. l. cold water dissolve starch and brew it in boiling water with acid. Pour powdered sugar in small portions and stir until a homogeneous plasticine-like mass is obtained. At the end, dye is added.
Elastic sugar mastic (for 1200 g of finished mastic)
Water 80 ml
Gelatin 7 g
Glucose (sold in pharmacies) - 2 tbsp. spoons
spoons
Soft margarine - 1 tbsp. spoon
Powdered sugar 1 kg
Pour gelatine with water and leave to swell for 40 minutes.
Heat the gelatin in a water bath, when it dissolves, add margarine and glucose to the gelatin.
Mix well.
Pour into another container and leave to cool.
Add some powdered sugar to the chilled mass, start mixing, and continue to add a little powdered sugar.
When the mass is thick enough to be kneaded. Lay out on a cutting table.
Preliminary, on the cutting table, pour a hill of powdered sugar,
make a depression in the center of the hill, into which put the mastic.
Knead the mastic in powdered sugar until it has an elastic consistency.
Sugar elastic mastic can be prepared in advance, it is well preserved in hermetically sealed plastic bags.
14. SUGAR AND MASTIC
Ingredients:
molasses 83 g
corn starch 101 g
icing sugar 775 g
water 202 g
Bring the molasses and water to a boil and, stirring, pour in the starch so that there are no lumps. Then powdered sugar is added and kneaded until a homogeneous mass resembling plasticine. Custard sugar mastic is more plastic; decorations made from this mastic are first dried and then used for decoration.
Then powdered sugar is added and kneaded until a homogeneous mass resembling plasticine. Custard sugar mastic is more plastic; decorations made from this mastic are first dried and then used for decoration.
15. MASTIC RECIPE FROM MARSHMALLOW
marshmallows - 100 g
- butter - 1 tbsp. l.
- icing sugar - 200-300 g
- food coloring
Put marshmallows in a mold, add butter
Microwave for 15-20 seconds. The mass should increase in volume. Put on the table, add dye, mix. Then add 100 g of powdered sugar, mix. Add powdered sugar until you get a mass similar in consistency to plasticine.
Knead the mass until it comes off hands.
Put the finished mass in the refrigerator for a couple of hours. Remove from refrigerator and thaw again to room temperature. When working with mastic, sprinkle the table and hands with starch.
16. HONEY MASTIC.
Ingredients for honey mastic
For 500 grams of powdered sugar
2 tbsp. spoons of honey
10 grams of gelatin
2 tbsp. tablespoons vegetable margarine or cream spread
tablespoons vegetable margarine or cream spread
6 tbsp. spoons of water
Preparation
As is customary when working with gelatin: soak the gelatin in water for 30-40 minutes.
When the gelatin has swollen well, heat it in a water bath until dissolved and cool.
In a bowl, stir together honey, melted margarine or spread and chilled dissolved gelatine.
Slowly start adding powdered sugar to the mixture, mixing gently with a wooden spatula or spatula. When the mass becomes thick enough and it can be kneaded, put it on a table sprinkled with powdered sugar and knead the elastic dough.
The honey fondant for the cake should be elastic so that it can be easily rolled out. If the honey mastic turns out to be soft, it will be impossible to work with it, it will stretch and tear a lot when covering the cake. Therefore, if your mastic is too soft, mix powdered sugar into the mastic to make the mastic more abruptly.
I hope that you will be able to choose from the proposed recipes for cake fondant that is right for you.
Milk mastic
Milk mastic is very convenient and versatile to use. It is convenient for her to cover the cake and sculpt figures. Due to its sticky and oily structure, the details of the figurines can be glued together even without special confectionery glue. You just need to do it right away, without waiting for drying. After drying, the figures become hard and durable. But they remain edible.
In my opinion, this mastic has only one drawback - it is not white, because condensed milk and infant formula have a yellowish tint. Therefore, the color is not what we would like. It is impossible to get a pure white and soft blue color from milk.
There are many milk mastic recipes on the net. I bring, in my opinion, the most successful version of milk mastic, which has served me faithfully for a long time.
Milk mastic recipe
Ingredients:
- Baby formula - 1 pack. (350 gr.)
These mixtures are #1 and #2, there is no difference. Haven't tried other blends. Although, logically, any formula should work. Pay attention to weight. You can also use powdered milk or powdered cream instead of milk formula.
Haven't tried other blends. Although, logically, any formula should work. Pay attention to weight. You can also use powdered milk or powdered cream instead of milk formula.
- Condensed milk - 1 can
It is necessary that the composition contains only milk and sugar. Quality matters. There have never been any problems with Rogachev's condensed milk.
- Powdered sugar - 350 gr.
Powder must be very fine. Such powder is sold in stores, but you can grind sugar at home in a coffee grinder. The main thing is that the quality of the powder should be high, there should not be grains in it, otherwise the mastic will not be of a homogeneous structure, it will tear and the figures will not turn out neat.
Preparation
1. Add all ingredients to the pot and stir. Loose powder and milk mixture can be mixed together first.
2. After two minutes, during the kneading process, the mastic is loose, not homogeneous, sticky.
3. After another 5 minutes, it becomes homogeneous, well mixed. We wash our hands, wipe them, sprinkle with powder and form a ball from the mastic.
4. To make it easier to work with mastic, wrap it in cellophane and leave it on the table for half an hour to strengthen the structure. After that, you can separate the necessary piece from it, add dye and roll it out for tightness. But even immediately after kneading, you can already work with it, it is soft, but it rolls out beautifully with powder, it does not stick. The thickness of the mastic for covering is about 3-4 millimeters. For a cake with a diameter of 24, a height of 8-10, it takes about 300-400 gr. mastics.
I rolled it out for you with a specially textured rolling pin, so that it can be seen that the relief is perfectly visible on it. It does not spring, keeps its shape perfectly, does not tear. Wrapping a cake is a real pleasure.
5. Here is a flower. I made it using a special cutting. He is with fringes, he did not specially make beauty. As it is. If the mastic is allowed to lie down a little, it will be better for modeling, of course. It won't be as soft.
As it is. If the mastic is allowed to lie down a little, it will be better for modeling, of course. It won't be as soft.
And here is an example of a cake with this fondant. The cover and figures are made of milk. Inscription, eyes and small flowers from purchased (Satin ice)
Store leftover milk mastic in the refrigerator. It will be firm when taken out of the refrigerator, but will quickly become usable if heated in the microwave while stirring. Those. put on 5 seconds, pull out, knead. If not soft enough, then put on for another 5 seconds and knead again. And so on until the mastic becomes plastic.
Work with mastic with powdered hands. Just like you need to roll out the mastic on a table sprinkled with powder. Otherwise it will stick.
Baby formula cake: step by step recipe with photo
When I found out that a cake can be made from baby formula, I was pleasantly surprised. If suddenly there is a mixture that is no longer needed, then why not try to make a cake that I call Baby.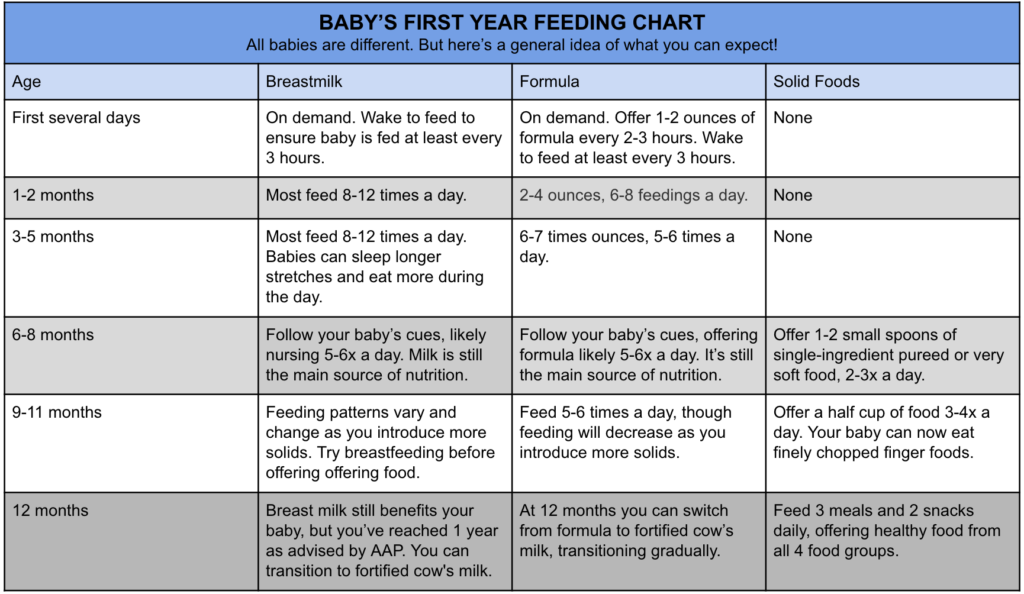
Ingredients
For the dough
3 eggs
200 g sugar
1 cup flour
200 g milk mixture
l. water
For cream
1 cup sour cream
6 tbsp infant formula
Step-by-step preparation
Mix all ingredients for the dough, beat. Pour the dough into a cake mold, bake for 40 minutes at 160 degrees. We take out the finished cake and let it cool. After cooling, divide into 3 parts.
For the cream, beat the sour cream with the mixture. Gradually grease each cake and collect the cake in this way. We leave the cake in the refrigerator for 2-3 hours for impregnation and you can taste an unusual cake from infant formula.
( 1 estimate, average 5 out of 5 )
Baby formula cake on the Internet (I think I stole it along with the link) Well, okay, I wasn’t there for a long time ... In general, I couldn’t sell the mixture, so I opened 1 jar (I left one, I’ll give it for 1000 tenge if anything) I had Nutrilon, and so any will do))))
Baby formula cake
Chicken eggs 3 pcs
Sugar 1 cup . l (quenched with lemon)
l (quenched with lemon)
Water (3 tbsp each in dough and cream)
Butter 200 gr (I took 100 gr)
Cream:
1/2 cup sugar 1 cup sour cream
(yogurt added)
1 glass of mixture
The cake was cut in half, smeared with cream and sprinkled with nuts!
The biscuit turned out tender and airy! but the cream for my taste should be made without a mixture !!
In general, you can cook porridge, and pancakes, and a cake without baking, but I have already written a proven recipe))))
Baby cake recipe
Delicious and easy-to-prepare cake from baby milk formula
Cake "Baby" contains infant milk formula, which is added to both the dough and the cream. The cake got its name from the name of the mixture that is used to make it, but you can replace it with any other. This recipe appeared in Soviet times, many have pleasant childhood memories associated with this taste.
For the test:
- Eggs - 3 pcs.
- Sugar - 1 cup
- Sour cream - 1 cup
- Infant formula - 1 cup
- Flour - 1 cup
- Baking powder - 1 tsp.
- Walnuts - 50 g
For cream:
- Sour cream - 1 cup
- Infant milk formula - 6 tbsp.
To decorate:
Cake "Baby" turns out to be very tasty, both adults and children love it. This dessert is perfect for a birthday party. Cake "Baby" is light and does not contain harmful ingredients; even kids can be treated with such a dessert. And the cake is prepared simply and quickly. If you have little time, but you want to treat your loved ones with a delicious and healthy dessert, the sweet and fragrant Baby Cake is a godsend for you. Be sure to try!
Baby formula cake, recipe with photo step by step
Soft, porous cakes with a milky taste! Any cream, even a simple apple jam, is perfect here.
Any mother with a small child knows the problem of choosing infant formula. Even those who are lucky enough to breastfeed a baby still have powdered milk formula in stock, just in case. And if you can’t find the right brand for a long time, there are a lot of such jars. And everything would be fine, but the shelf life of an open box is no more than three weeks. But a good hostess will never lose anything. And so mothers got the hang of cooking a lot of delicious desserts from infant formula. These are pancakes, and cookies, and even a cake. Today we will try to make a cake from baby formula. Cakes are tender, porous, with a pleasant milky taste. Well, as a cream we will use apple jam. It will be a very tasty dessert, try it.
Baby formula cake recipe with photo step by step
Ingredients:
egg 3 pcs.
sugar 1 tbsp. l.
infant milk formula 3 tbsp. l.
wheat flour 3 tbsp. l.
baking powder 1 tsp.
apple jam 1 glass.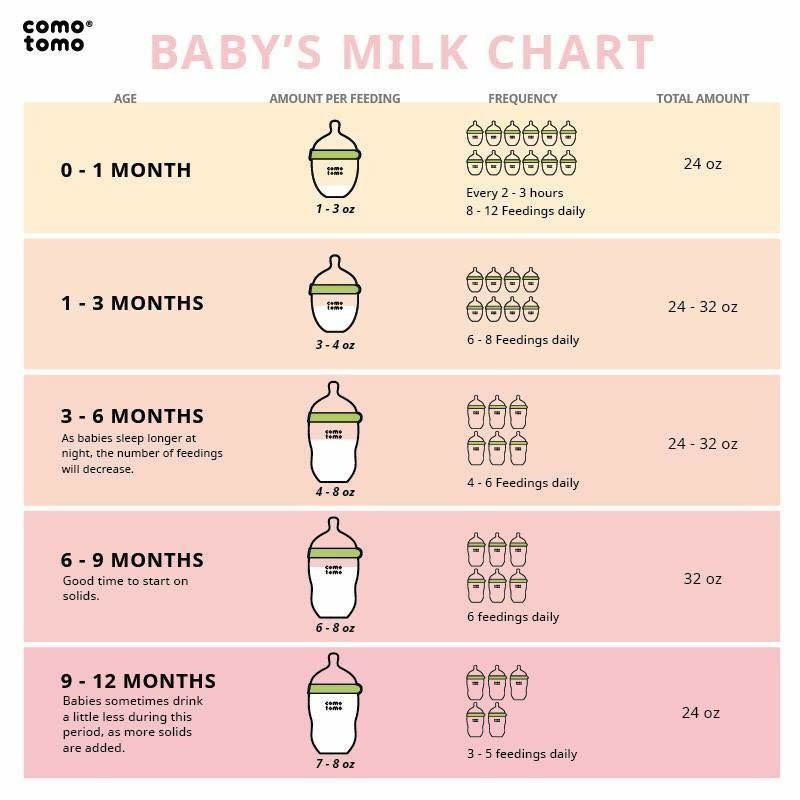
How to make an infant formula cake
Prepare everything you need. The infant formula is used milk, the brand does not really matter, they are all approximately the same in composition.
Break the eggs into a clean, dry bowl and add the sugar. Adjust the amount of sugar depending on the sweetness of the jam.
Beat with a mixer at high speed until a stable foam and increase in volume. Add sifted flour with baking powder and baby formula.
Stir gently with a spoon or spatula. It is better not to use a mixer, so the mass will be airy and porous. In this case, there should not be any unmixed areas with lumps of flour or mixture. The consistency of the dough will turn out to be more liquid than biscuit, as it should be.
Line a baking sheet (size 30x30 cm) with parchment, grease it with butter and place in the preheated oven for 2-3 minutes. Pour in the batter, smooth it out. It is necessary to try so that the layer is more or less the same thickness, about 4-6 millimeters. The crust will rise while baking.
The crust will rise while baking.
Place in the oven on the top rack at 180 degrees for 7 minutes. As soon as the layer began to brown around the edges, everything is ready. The cake is soft and elastic, easily separated from the parchment.
Cut into 10x15 cm rectangular pieces. There are four of them. You can even divide it into two parts and the cake will come out large, but low. Lay the crust out on a flat surface.
Spread generously with apple jam or any cream. The dough is porous and absorbs moisture well, so you should put more jams.
Collect the entire baby formula cake in this way.
For decoration, you can use cake cuts, which must be dried in the oven and crushed into crumbs. Any shortbread cookies, waffles, nuts will do.
Top and sides of the cake also grease with jam and sprinkle with prepared crumbs.
Be sure to chill in the refrigerator for at least a couple of hours before serving. Soaked in jam, the cakes will increase slightly and become even more tender.
Say thanks for the article 0
Subscribe to our channel in Yandex.Zen! Click "Subscribe to the channel" to read Lady-day.ru in the Yandex feed
ways to make dessert: Labuda.blog
Baby formula cakes were very popular among the inhabitants of the Soviet Union. In conditions of food shortages, this component was used not only for feeding babies, but also as an ingredient in confectionery. Today, such desserts have not lost their relevance. Moms make these cakes from the leftover mixture they buy for their kids. Several baking recipes are presented in the article.
Simple buttercream dessert
For it you will need:
- Three eggs.
- 200 g of granulated sugar.
- Flour (one glass).
- Soda (half a teaspoon).
- Milk formula "Baby" in the amount of 400 g.
- Butter - about 200 g.
- Six large spoons of water.
Baby formula cake is prepared like this.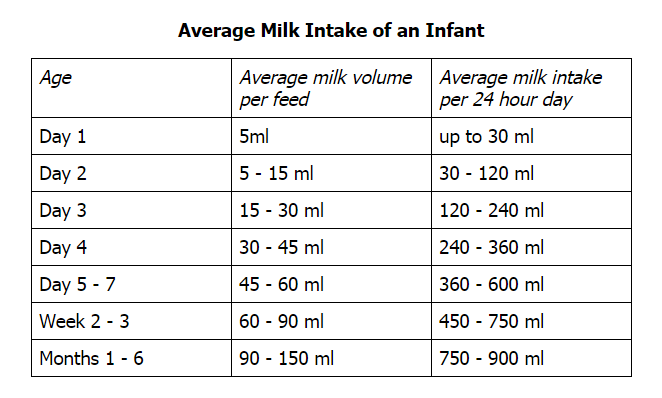
Eggs are combined with granulated sugar. They rub well. Add a mixture of 200 g, soda, flour, pour in water - three tablespoons. The resulting dough is divided into three fragments, each of which must be cooked in the oven at a temperature of about 200 degrees for 15 minutes. Then the layers of dessert should be cooled.
For the cream, beat the butter with a mixer. Add three large spoons of water and the remaining mixture. Whisk the ingredients thoroughly. The layers of dessert are smeared with the resulting mass, connected to each other.
Sour cream pastry
The base for the treat includes:
- Half a glass of baby formula.
- The same amount of flour.
- 100 g granulated sugar.
- Sour cream (the same).
- Two eggs.
- Baking powder - half a teaspoon.
For cream you will need:
- Sour cream (half a glass).
- Milk mixture (3 tablespoons).
- Sugar - to taste.

Four walnut kernels are used to decorate the dessert. How to make a baby formula cake with sour cream?
The recipe is described in the next chapter.
Preparation
Combine the ingredients needed for the biscuit in a deep dish. Grind until a homogeneous mass is formed. The mixture should be placed in a baking dish. Sprinkle with a layer of chopped walnut kernels. The biscuit is cooked in the oven at 160 degrees for 30 minutes.
To prepare the cream, sour cream is combined with a portion of the mixture. You can put sugar in the mass (about 1 tablespoon). Then the products are rubbed well.
The biscuit is cooled and cut lengthwise into three identical pieces. Cakes are covered with sour cream, put in a cold place. When the cream becomes thick, layers of dessert are stacked on top of each other. The baby formula cake is sprinkled with chopped walnut kernels.
Condensed milk treat
To prepare the dough you need:
- Flour (about 200 grams).

- A glass of infant formula.
- The same amount of granulated sugar.
- Three eggs.
- Three tablespoons of water.
- Seven grams of baking powder.
The cream contains:
- Butter in the amount of 200 grams.
- A glass of infant formula.
- Three tablespoons of water.
- Condensed milk (to taste)
. For the impregnation of the dessert is used:
- 75 g of granulated sugar.
- 150 ml water.
Nut kernels, biscuit crumbs, waffles are used to decorate the dish.
How to make a baby formula cake? The recipe with a photo is discussed in this chapter. To prepare a biscuit, you need to grind the eggs with sugar. Add water, baking powder and flour. Whisk the ingredients well. Pour into the milk mixture. Thoroughly mix the products with a mixer.
Place the dough in a bowl lined with parchment paper. Cook in the oven for about a quarter of an hour. Then the biscuit should be cooled. Divide into two or three fragments of the same size.
Then the biscuit should be cooled. Divide into two or three fragments of the same size.
To make cream, beat warm butter with a mixer. Combine it with milk mixture and water. Add condensed milk and mix well.
Syrup is made from granulated sugar and water, which is used to cover the surface of the cakes. Layers of dessert are stacked on top of each other. Each tier of the baby formula cake is smeared with cream. The surface of the treat is covered with wafers, nuts, and cookie crumbs crushed in a blender.
Recipe for dessert with apple marmalade
For baking you will need:
- Three eggs.
- Sugar (1 tablespoon).
- 7 grams baking powder.
- Apple jam - 1 cup.
- Three tablespoons of formula milk.
- Wheat flour (the same).
- Wafers, nut kernels.
To make dessert, grind eggs with sugar. The components are whipped with a mixer until foam is formed. Add sifted flour, milk mixture and baking powder. The ingredients are rubbed with a spatula or spoon.
The ingredients are rubbed with a spatula or spoon.
The resulting mass is placed in a bowl lined with baking paper and greased with butter. Cook in the oven for seven minutes.
Remove the cake from the mold and let it cool. Cut lengthwise into several pieces of the same size. Cover with a layer of jam. Place the dessert tiers on top of each other.
Walnut kernels and waffles should be ground with a blender. A cake from a baby formula according to a recipe with the addition of jam is sprinkled with the resulting crumbs.
Dessert with the addition of cocoa powder without baking
It consists of the following components:
- Softened butter in the amount of 250 grams.
- Water (one glass).
- Half a kilo of infant formula.
- Cocoa powder - five tablespoons.
- The same amount of granulated sugar.
- Cookies (about four packs).
How to make a cake with infant formula? The recipe for the dish is presented in the next chapter.
Preparation
The mixture is combined with cocoa powder and butter. Rub until a lump appears. Water and granulated sugar are heated on the stove. Cool the syrup and combine with the chocolate mixture. Cream for dessert should be soft, without lumps.
Baking utensils covered with foil. Cookies are placed on its surface, covered with cream. Repeat these steps until the products run out.
The infant formula cake is then placed in a cold place.
Infant Formula - American Family Physician
2. Gartner LM, Morton J. Lawrence RA, et al., for the Breastfeeding Section of the American Academy of Pediatrics. Breastfeeding and drinking breast milk. Pediatrics . 2005. 115(2): 496–506.
3. Enrichment of infant formulas with iron. American Academy of Pediatrics. Nutrition Committee. Pediatrics . 1999; 104 (1 p.1): 119–123.
4. Hopkins D, Emmett P, Rule C, Rogers I, Noble S, Emond A. Infant feeding during the second 6 months of life is associated with iron status: an observational study. Arch Dis Child . 2007. 92(10): 850–854.
Arch Dis Child . 2007. 92(10): 850–854.
5. Simmer K, Patole SC, Rao SC. Long-chain polyunsaturated fatty acid supplementation in term infants. Cochrane Database Syst Rev . 2008; (1): CD000376.
6. Simmer K, Schulzke SM, Patole S. Supplementation of long-chain polyunsaturated fatty acids in preterm infants. Cochrane Database Syst Rev . 2008; (1): CD000375.
7. RT Hall, Carroll RE. Infant feeding. Pediatrician Rev. . 2000. 21(6): 191–199.
8. Henderson G, Fahey T, McGuire W. Nutrient-enriched formula versus standard preterm formula after hospital discharge. Cochrane Database Syst Rev . 2007; (4): CD004696.
9. Hayman MB. Nutrition Committee. Lactose intolerance in infants, children and adolescents. Pediatrics . 2006. 118(3): 1279–1286.
10. American Academy of Pediatrics. Nutrition Committee. Hypoallergenic formulas for babies. Pediatrics . 2000; 106 (2 p. 1): 346–349.
11. Bhatia J, Greer F, for the Committee on Nutrition of the American Academy of Pediatrics. The use of soy protein formulas in infant feeding. Pediatrics . 2008. 121(5): 1062–1068.
Bhatia J, Greer F, for the Committee on Nutrition of the American Academy of Pediatrics. The use of soy protein formulas in infant feeding. Pediatrics . 2008. 121(5): 1062–1068.
12. Craig VR, Hanlon-Dirman A, Sinclair C, Tobacco S, Moffatt M. Metoclopramide, thickened feedings and positioning in gastroesophageal reflux in children under two years of age. Cochrane Syst Rev 9 Database0261 . 2004; (4): CD003502.
13. Garrison MM, Christakis D.A. Systematic review of methods of treatment of infantile colic. Pediatrics . 2000; 106 (1 pt 2): 184–190.
14. Absence G, Fox D, Northstone C, Golding J, for the Avon Parent-Child Longitudinal Study Group. Factors associated with the development of peanut allergy in childhood. N Engl J Med . 2003. 348(11): 977–985.
15. Klemola T, Kalimo K, Pussa T, and others. Feeding soy formula to children with cow's milk allergy: development of immunoglobulin E-mediated allergy to soy and peanuts. Pediatr Allergy Immunol . 2005. 16(8): 641–646.
2005. 16(8): 641–646.
16. Osborne DA, Sinn J. Hydrolyzed protein formulas for the prevention of allergies and food intolerances in infants. Cochrane Database Syst Rev . 2006; (4): CD003664.
17. Allen UD, McLeod K, Van E. Cow's milk versus soy-based formulas for mild to moderate diarrhea: a randomized controlled trial. Acta Paediatr . 1994. 83(2): 183–187.
18. Strom BL, Shinnar R, Ziegler E. et al. Exposure to soy-based formula in infancy, and endocrinological and reproductive outcomes in young adulthood. JAMA . 2001. 286(7): 807–814.
19. Essex K. Phytoestrogens and soy-based infant formulas. BMJ . 1996. 313 (7056): 507–508.
20. Hall RT, Kallenbach JC, Sheehan MB, and others. Comparison of a mixture of soy isolates containing calcium and phosphorus with whey-dominated preterm infant formula for very low birth weight infants. J Pediatrician Gastroenterol Nutr . 1984. 3(4): 571–576.
21. Callenbach JC, Sheehan MB, Abramson SJ, Hall RT. Etiological factors of rickets in children with very low birth weight. J Pediatrician . 1981. 98(5): 800–805.
Etiological factors of rickets in children with very low birth weight. J Pediatrician . 1981. 98(5): 800–805.
22. Sandhu BK, Isolauri E, Walker-Smith JA, et al. Multicenter study on behalf of the Acute Diarrhea Working Group of the European Society of Pediatric Gastroenterology and Nutrition. Early feeding in pediatric gastroenteritis. J Pediatrician Gastroenterol Nutr . 1997. 24(5): 522–527.
23. Agostoni C, Fiocchi A, Riva E, and others. Growth of infants with IgE-mediated cow's milk allergy fed various formulas during the complementary feeding period. Pediatr Allergy Immunol . 2007. 18(7): 599–606.
24. Hill DJ, March S., Rafferty K, Wallis P., Green CJ. Efficacy of amino acid formulas in alleviating symptoms of cow's milk allergy: a systematic review. Clin Exp Allergy . 2007. 37(6): 808–822.
25. Greer FR, Shicherer S, Burks AV, for the Committee on Nutrition of the American Academy of Pediatrics, Section of Allergy and Immunology of the American Academy of Pediatrics. The impact of early dietary intervention on the development of atopic disease in infants and children: the role of maternal dietary restriction, breastfeeding, timing of complementary foods, and hydrolyzed formulas. Pediatrics . 2008. 121(1): 183–191.
The impact of early dietary intervention on the development of atopic disease in infants and children: the role of maternal dietary restriction, breastfeeding, timing of complementary foods, and hydrolyzed formulas. Pediatrics . 2008. 121(1): 183–191.
26. Mukarzel AA, Abdelnur Kh, Akacheyan K. Effect of pre-thickened formula on esophageal pH and gastric emptying in infants with GER. J Clean Gastroenterol . 2007. 41(9): 823–829.
27. Lothe L, Lindberg T, Jakobsson I. Cow's milk formula as a cause of infantile colic: a double-blind study. Pediatrics . 1982; 70(1): 7–10.
28.Campbell JP. Dietary treatment of infantile colic: a double-blind study. J R Coll Gen Pract . 1989. 39 (318): 11–14.
29. Lucassen PL, Assendelft WJ, Gabbels JW, van Eyck JT, van Geldrop WJ, Neven AK. Efficacy in the treatment of infantile colic: a systematic review [published amendments published in BMJ. 1998, 317 (7152): 171]. BMJ . 1998. 316 (7144): 1563–1569.
30. Taubman B. Parental counseling versus avoiding cow's milk or soy milk protein for treatment of infantile colic syndrome: a randomized trial. Pediatrics . 1988. 81(6): 756–761.
.
How much formula should you feed your baby?
How much formula to feed your baby: where to start
Babies generally eat when hungry and stop when full, so it's important to pay attention to your baby's hunger signals and resist the temptation to encourage your baby to finish every bottle. The key recommendations below describe how much a formula-fed baby typically eats based on weight and age. The healthy growth curve will show that your baby's diet is being followed.
A few notes:
- This guide is for infants who are exclusively formula fed for the first 4-6 months and then formula and solid foods until 1 year of age.
- If your baby is receiving formula and breast milk, talk to your doctor for specific advice.

- Your child's doctor can tell you where your child is on the growth charts and help make sure he is growing steadily and getting a healthy amount of formula. If you ever worry that your child is getting too little or too much formula, talk to their doctor.
How Much Hunger Signal Formula
Although the sections below give recommendations on how much formula to feed your baby based on weight and age, it is always important to also pay attention to behaviors called hunger signals.
Crying: Crying is a late sign of hunger. Early signals that your baby is hungry include:
- Snacking or sucking
- Rooting (turning head towards hand when you stroke his cheek)
- Bringing hands to mouth
- Opening mouth
Look around: You will know that your baby wants more when he quickly finishes feeding and looks around for more. If after the first bottle he seems unhappy, try making another couple ounces at a time. If you make a large amount, he may not finish it and you will have to throw it away.
If you make a large amount, he may not finish it and you will have to throw it away.
Growth spurts: Your child may be hungrier than usual during growth spurts. This usually occurs 10–14 days after birth and around 3, 6, 3, and 6 months of age. Your child may be less hungry than usual if they are not feeling well.
It's not always hunger: Resist the urge to respond to your baby's every whimper with a bottle. Consider the possibility - especially if you've fed him recently - that he's crying because his diaper is wet, he's cold or hot, he needs to burp, or he just wants to be near you. For more help, read this article on 12 Reasons Babies Cry and How to Soothe Them.
How Much Formula By Weight
For the first 4-6 months when your baby is not eating solids, here's a simple rule of thumb: Offer 2.5 ounces of formula per pound of body weight each day, up to a maximum of about 32 ounces per day.
For example, if your child weighs 6 pounds, you will give him about 15 ounces of formula in 24 hours. If she weighs 10 pounds, you will give her about 25 ounces in 24 hours.
If she weighs 10 pounds, you will give her about 25 ounces in 24 hours.
These numbers are not hard and fast rules. They offer a rough estimate of what your child may need. Some children will grow well if they take less than the recommended amount, while others constantly need more. Your baby's daily feeding will also vary based on his individual needs - in other words, he may want a little more on some days and a little less on others.
How much formula by age
As your baby gets older and his tummy gets bigger, he will drink fewer bottles per day with more formula in each. It is important not to overfeed your baby to keep him healthy. Your child should drink no more than 32 ounces of formula in 24 hours.
Here are typical amounts per day by age:
- First week: Formula feed on demand. Most newborns want to eat every two to three hours. For the first day or two, they can only drink half an ounce per feeding. After that, offer 1 to 2 ounces at each feeding for the rest of the week.

- After 2 weeks: 2-3 ounces at each feed
- Weeks 2-4: 2-4 ounces every three to four hours
- C 1 month or more 4 ounces: at least three up to four hours
- C 2 months : 4 to 5 ounces every three to four hours
- C 4 months : 4 to 6 ounces every three to four hours, with longer breaks time
- C 6 months : 6 to 8 ounces every four to five hours, with longer breaks at night, especially if he sleeps all night
He will probably level off when he reaches about 7-8 ounces per feeding.
After reaching his first birthday, he can switch to whole cow's milk in a bottle or drinking glass, as well as three solid meals and two snacks between meals per day.
Signs your baby is getting the right amount of formula
Here are the signs that your baby is getting all the formula he needs:
- Steady weight gain.
 She continues to gain weight after the first 10 days and follows a healthy growth curve during the first year. (Most babies lose up to 10 percent of their birth weight in the first few days and then gain it back by the time they are about 10 days old .)
She continues to gain weight after the first 10 days and follows a healthy growth curve during the first year. (Most babies lose up to 10 percent of their birth weight in the first few days and then gain it back by the time they are about 10 days old .) - Happy baby. After feeding, she seems relaxed and satisfied.
- Wet diapers. She wets two to three diapers (disposable or cloth) a day for the first few days after birth. Over the next few days, the number of diapers should increase to at least five to six diapers a day if you use disposable diapers, or six to eight if you use cloth diapers. (Disposable products contain more fluid.)
Signs that your child is getting too much formula
- Vomiting after feeding may be a sign that your child has eaten too much. (Spitting up is normal, vomiting is not. Find out how to tell the difference.)
- Abdominal pain after feeding can also be a sign of overeating.
 If your child pulls up his legs or his stomach feels tight, he may be in pain. (See Other Possible Causes of Abdominal Pain in Babies.)
If your child pulls up his legs or his stomach feels tight, he may be in pain. (See Other Possible Causes of Abdominal Pain in Babies.)
How Your Doctor Can Help
If you are worried that your child is getting too little or too much formula, talk to their doctor. The doctor can:
- Check your child's weight and height
- Tell you if his intake is appropriate for his size and age
- Tell us to you about any adjustments you may need
For other formula feeding questions, visit our Formula Feeding Problem Solver section.
.
Infant formula selection | Nutrition
No brand of infant formula is suitable for all babies. You should choose an infant formula that is made specifically for babies. The US Food and Drug Administration (FDA) regulates commercial infant formula to ensure that it meets minimum nutritional and safety requirements. Pediatricians generally recommend iron-fortified infant formulas, and most commercial infant formulas sold in the US contain iron. Commercial infant formulas come in liquid and powder forms.
Commercial infant formulas come in liquid and powder forms.
If infant formula is selected:
- Check that it has not expired.
- Make sure the container is sealed and in good condition. If there are leaks, swollen tips, or rust spots, do not feed this to your baby.
Talk to your child's doctor or nurse if you have questions about choosing infant formula for your baby or if you are thinking about changing brands or types of infant formula.
Homemade baby food
The FDA and the American Academy of Pediatrics warn against using prescriptions for homemade infant formula. Using homemade infant formula can cause serious health problems for your baby. Your baby's nutritional needs are very specific, especially in the first year of life. Homemade infant formula may contain too little or too much of certain ingredients, such as vitamins and minerals (such as iron).
Homemade infant formula may also have an increased risk of contamination, which can cause the baby to become ill or develop an infection. Commercial powder mixes are also not guaranteed to be sterile. However, these products and manufacturing facilities are regularly reviewed by the FDA to ensure that these products are safe.
Commercial powder mixes are also not guaranteed to be sterile. However, these products and manufacturing facilities are regularly reviewed by the FDA to ensure that these products are safe.
Imported infant formula
There are some public claims that infant formula sold in other countries and advertised as "natural" or "organic" is better for babies. However, there is no scientific evidence that these infant formulas are better for babies than commercial infant formulas sold in the United States. All infant formula legally sold in the United States, whether manufactured in the United States or imported from other countries, must be reviewed by the FDA. The American Academy of Pediatrics warns against using illegally imported formulas, such as products ordered online from third-party distributors . The FDA may not review these products. Illegally imported mixtures may also have been mishandled and stored.
The FDA reviews all infant formula legally sold in the United States to ensure that it meets minimum nutritional and safety requirements. The FDA also ensures that the water used to make formulas meets safety standards set by the US Environmental Protection Agency.
The FDA also ensures that the water used to make formulas meets safety standards set by the US Environmental Protection Agency.
Infant milk or formula
Infant milk, drinks or formula are not needed to meet the nutritional needs of older children. At 12 months old, your baby can be introduced to fortified cow's milk. Babies under 12 months of age should be fed formulas specially formulated to meet their nutritional needs. They must and not to feed babies drinks or formula intended for babies.
.
FORMULA FOR CHILDREN | Definition of
in the Cambridge English Dictionary Proposal relating to infant formula of formula and subsequent formula provisions. Trade advertising does not promote baby food to consumers, but it does serve to make retailers more aware of the baby food products they may wish to have in stock.
These examples are from the Cambridge English Corpus and online sources. Any opinions in the examples do not represent those of the editors of the Cambridge Dictionary, Cambridge University Press or its licensors.
Any opinions in the examples do not represent those of the editors of the Cambridge Dictionary, Cambridge University Press or its licensors.
More examples Fewer examples
In its anti-boycott ad, Nestl stated that it sells infant formula ethically and responsibly. From
Wikipedia
-SA. Yashili increasingly focuses on baby food baby food which currently accounts for 80% of the group's sales. From
Wikipedia
This example is taken from Wikipedia and may be reused under license from CC BY-SA. It was first used mainly in infant formulas.
Read online Companion to the breastfeeding mother.
 From Pregnancy to Weaning,” Kathleen Huggins – LitRes, page 2
From Pregnancy to Weaning,” Kathleen Huggins – LitRes, page 2 Breastfeeding isn’t always easy
If breastfeeding is natural, it should be easy, right? Well, sometimes it's not like that. Today, about half of mothers who start breastfeeding their babies stop within the first six weeks. The reason for failure most often lies not in the fact that the mother's body is not able to produce enough milk. Usually the point is that a woman trying to breastfeed was not helped in time. Too many new mothers know very little about breastfeeding and babies, receive little or no information and support while learning to feed.
Although breastfeeding is natural, people cannot breastfeed based on instinct alone - feeding must be learned. The later chapters of this book will tell you everything you need to know.
Many excellent books have already been written about the benefits of breastfeeding over formula. I have tried to provide mothers with a practical guide that they can refer to while breastfeeding. The first part of the book provides basic information about breastfeeding, breastfeeding preparation, and feeding during the first week postpartum; the rest of the book is meant to be read gradually as the baby grows and feeds continue. The book has chapters on each of the three further periods of breastfeeding - after the second week until the end of the second month, from two months to six and after six. At the end of each chapter is a "Survival Guide" - a short but powerful reference material for almost any problem that you and your child may encounter during the time discussed. Although you may not often need to refer to the Survival Guide, I have included them in the book so that, if the need arises, you can find material on your problem and solve it as quickly as possible.
The first part of the book provides basic information about breastfeeding, breastfeeding preparation, and feeding during the first week postpartum; the rest of the book is meant to be read gradually as the baby grows and feeds continue. The book has chapters on each of the three further periods of breastfeeding - after the second week until the end of the second month, from two months to six and after six. At the end of each chapter is a "Survival Guide" - a short but powerful reference material for almost any problem that you and your child may encounter during the time discussed. Although you may not often need to refer to the Survival Guide, I have included them in the book so that, if the need arises, you can find material on your problem and solve it as quickly as possible.
Because many breastfeeding mothers need some form of medication from time to time, Dr. Philip O. Anderson wrote an appendix on medications for this book that evaluates their safety for breastfeeding babies.
Mothers breastfeed not only because they want to give their children the best possible nutrition and protection, and not only because there are many benefits to them, but simply because they enjoy it. The loving bond between mother and infant that begins at the breast brings joy and emotional fulfillment to both of them. The most wonderful thing about motherhood is watching your body grow a child, first inside itself, and then at the breast.
You may have made the decision to breastfeed long before you got pregnant. Or you started to think about it just now, it also happens.
Although breastfeeding is natural, many new mothers are surprised to find that it is a skill that needs to be learned; It usually takes several weeks to fully master it.
Successful breastfeeding often depends on a woman's perseverance and self-confidence. You can help build self-confidence by learning about breastfeeding early. As for perseverance, it is useful to provide yourself with good support in advance.
Collecting information
Several generations ago, as a first mother, you would have turned to your own mother for help and support in feeding. Fortunately, many women still have this opportunity. But others don't.
If your mother didn't breastfeed or stopped breastfeeding quickly, there are several ways you can learn to feed early. Undoubtedly, it is useful to read books on relevant topics. In some cities you can find courses on breastfeeding. Pregnant women are also very welcome to the meetings of La Leche League [6] , which usually take place once a month. La Leche League is an organization for breastfeeding mothers whose goal is to support breastfeeding throughout the world. There are other support groups in some places, such as the Council for Nursing Moms; they run courses and provide telephone counseling for pregnant and lactating women. In addition, prenatal courses on breastfeeding can take place at maternity hospitals and other health care institutions.
Another great way to learn about breastfeeding is to spend time with breastfeeding mothers. Perhaps you have never seen a mother breastfeeding her baby up close. Most breastfeeding women will be very pleased that you are interested, and one of them may be a good source of information and support for you in the near future. Be sure to ask them about the first weeks of feeding. Chances are you'll hear many different stories and perhaps gradually get a sense of what early breastfeeding is like.
Your breasts
During pregnancy, your breasts undergo many changes to prepare them to feed your baby when he is born. In the first trimester, you may have noticed that your breasts are fuller and more sensitive than usual. These changes in size are due to the fact that glandular tissue develops inside the breast, which will serve to produce milk. Most women choose to wear a supportive bra during pregnancy, although some are just as comfortable without one. At the beginning or middle of pregnancy, your chest also expands.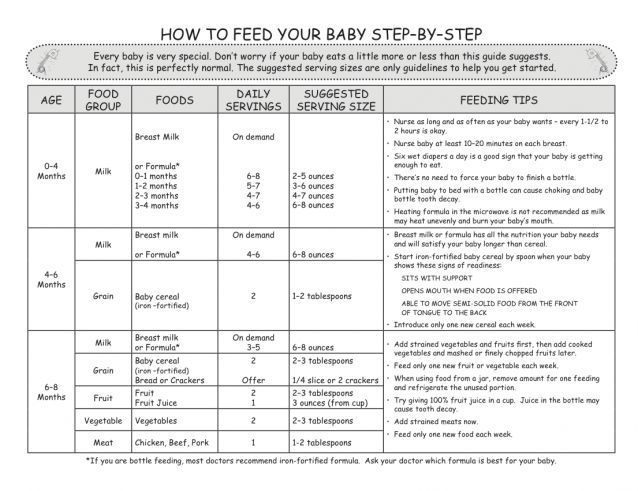
You will probably feel that the bra is pressing under your breasts, and because of this you may get new bras or a special insert to expand the old ones. Your breasts gradually increase in size, more blood is now circulating in them, and the veins on the chest can be clearly visible. Some women develop stretch marks on their breasts - the same as on the stomach.
The nipples and the area around them - the areola - may double in size and darken; the darker color seems to be to make it easier for the newborn to see the nipple [7] . At the same time, the bumps on the areola, the so-called Montgomery's glands, become more prominent. Their function is to produce an antibacterial lubricant that moisturizes and protects the nipple during pregnancy and breastfeeding. That is why soap and any creams are not needed now for your breasts and can even harm it: soap would remove natural lubrication, and cream could affect its antibacterial effect.
During pregnancy, the nipples often become especially sensitive. Some women find that it even hurts to touch them. Sensitivity decreases as the duration of pregnancy increases - it should not make breastfeeding something unpleasant! Other women, on the contrary, like this increased sensitivity, and during sex during this period they are especially pleased when a partner caresses their breasts.
Some women find that it even hurts to touch them. Sensitivity decreases as the duration of pregnancy increases - it should not make breastfeeding something unpleasant! Other women, on the contrary, like this increased sensitivity, and during sex during this period they are especially pleased when a partner caresses their breasts.
At the fifth or sixth month of pregnancy, the breasts are already fully capable of producing milk. Some women at this time notice drops of liquid on their nipples. This liquid, known as colostrum, is the food that your baby will receive in the first days after birth. Some women don't ooze colostrum from their breasts, but they still have it inside.
Breast care
In the last months of pregnancy, try not to wash your breasts with soap, just rinse them when you shower or bath. Soap can dry out your nipples and areolas. If dryness bothers you or if your breasts itch, a gentle cream or lotion can help, but avoid putting it on your nipples and areolas.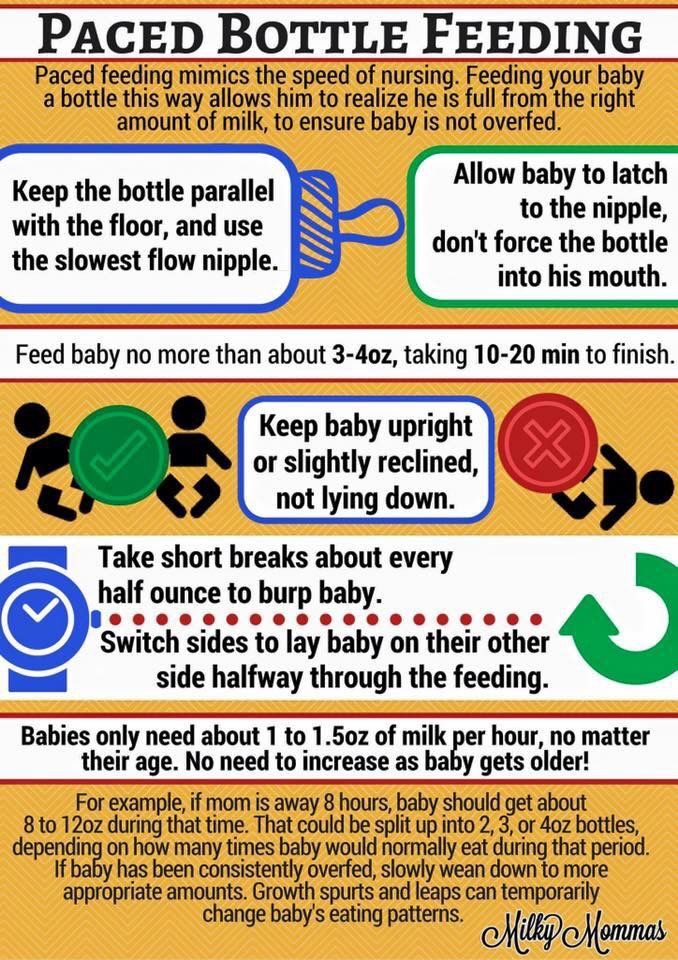
To all of us, women, the world around us constantly broadcasts our body assessments and tells us how it supposedly “should” look. This affects our self-esteem, including how we feel about our breasts in general and their appearance in particular. You probably remember how you perceived your breasts when they grew at the beginning of puberty. Maybe you were proud of the fact that it increases and you can already wear a bra. Or you were embarrassed that she began to grow earlier than other girls, or that she was bigger than theirs. You may have been worried if your breasts were slow to grow, or you may have felt more confident about being small.
You may still wish that your breasts were smaller or larger, that they looked fuller or drooped less. Maybe you don't look like the women with the "perfect" breasts in the photographs of the "perfect" breastfeeding mothers. Especially women with large breasts often feel insecure, imagining that the breasts will increase even more or that milk will leak heavily from it. In fact, large breasts rarely grow much after childbirth, and they usually leak less than small ones.
In fact, large breasts rarely grow much after childbirth, and they usually leak less than small ones.
Every woman's breasts are different from all other breasts in the world, but most breasts, regardless of size, are perfect for their primary mission of feeding our babies. The breast not only provides the baby with the most suitable food for his growth and development, but at the breast he acquires the warmth, comfort and sense of security so necessary for him in infancy. In this capacity, your breasts are the most beautiful thing in the world.
Milk production and separation
After giving birth, your baby will first have colostrum. It is an ideal food for the first days of life, both in terms of nutrition and protection against infections. Actually milk usually appears on the second or third day, but it happens that on the fourth, fifth or even later. This late appearance of milk, which is becoming more common, may be related to the way the birth has progressed (see Preparing for Birth, page 34).
When the placenta is born, the woman's body receives a signal to start producing milk. The hormone prolactin activates the corresponding cells in the breast. Initially, milk begins to be produced [8] whether the baby is breastfeeding or not. Here is the continuation of its development - this is another matter. It depends on frequent and regular stimulation of the breast and the outflow of milk. An infant suckling stimulates the nerve endings in the breast, which in turn trigger the release of two hormones needed for the production and flow of milk, prolactin and oxytocin.
Prolactin, as already mentioned, activates milk-producing cells in the breast. Oxytocin, on the other hand, is responsible for ensuring that milk flows out of those tiny sacs in which it is produced. This process is called the milk ejection reflex. When the baby suckles, the milk is pushed forward towards the nipple. The task of the child is to get milk by squeezing the areola with his lips and tongue during sucking.
In the first months of life, your baby will get enough milk if you feed him often (at least eight times [9] in 24 hours), if he attaches well and suckles effectively, and if you keep him at the chest long enough. The fact is that breastfeeding works on the principle of supply and demand. The more your breasts are stimulated and emptied by the suckling baby, the more milk will be produced in them.
Provide the purest milk
Mothers may sometimes wonder if their milk is completely safe for their baby. Most often, such doubts arise when the mother has to take medication. While many medications pass into breast milk, the vast majority pass only in very small amounts, which is considered safe for a breastfeeding baby. A comprehensive index of drug interactions with breast milk by Dr. Philip O. Anderson can be found in Appendix 3 (see page 365). Another source of such information is LactMed, a database developed by Dr. Anderson for the National Library of Medicine. You can find LactMed in the list of databases at www.toxnet.nlm.nih.gov.
You can find LactMed in the list of databases at www.toxnet.nlm.nih.gov.
More and more questions are being raised about the environmental pollution that affects us - insecticides, for example, or other toxic chemicals. Many of these substances accumulate in adipose tissue; as a result, small amounts can be found in breast milk. Experts, however, have been unable to identify any risks to the infant from so many potentially harmful substances, and most believe that the benefits of breast milk, both as nutrition and as an immune booster, far outweigh the possible risks from environmental pollutants. Unfortunately, our babies are much more exposed to some of these chemicals during fetal development than they are at the breast.
Fish and Seafood Safety
The US Food and Drug Administration (FDA) says that pregnant women should avoid eating shark, swordfish, king mackerel and cablefish, but that you can safely eat at 336 grams per week of any other thermally processed fish. The Environmental Working Group is even more conservative; this non-profit organization also suggests avoiding fresh tuna (including those found in Japanese restaurants), sea bass, Gulf of Mexico oysters, marlin, halibut, various types of walleye, white croaker, and largemouth bass, and advises eat no more than 168 grams (6 ounces) per month of canned tuna, dorado, mussels, oriental oysters, cod, pollock, Great Lakes salmon, Gulf of Mexico blue crab, wild catfish, yellowtail (also common in Japanese restaurants), mackerel , wild trout and lake white fish.
The Environmental Working Group is even more conservative; this non-profit organization also suggests avoiding fresh tuna (including those found in Japanese restaurants), sea bass, Gulf of Mexico oysters, marlin, halibut, various types of walleye, white croaker, and largemouth bass, and advises eat no more than 168 grams (6 ounces) per month of canned tuna, dorado, mussels, oriental oysters, cod, pollock, Great Lakes salmon, Gulf of Mexico blue crab, wild catfish, yellowtail (also common in Japanese restaurants), mackerel , wild trout and lake white fish.
Safe fish and seafood species with mercury levels below 0.2 ppm include farmed trout and catfish, fish fingers, shrimp, pollock, wild Pacific salmon, haddock, summer-caught flounder, croaker, Atlantic blue crab, freshwater game fish, scallop and various bivalves. Check with your local health authority for the safety of local fish species.
If you want to minimize your baby's exposure to toxic chemicals, observe the following restrictions while you are pregnant and throughout your breastfeeding period:
• Stop using pesticides in your home, garden, and pet care.
• Avoid contact with organic solvents found in paints, nail polish removers, gasoline fumes, non-water based adhesives, nail polish, and dry cleaners. All dry-cleaned clothing and clothing stored with moth repellants should be aired out before wearing, and avoid clothing that is already made to be moth repellent.
Tattoos
Some breastfeeding mothers would like to get a tattoo and wonder if it is safe. Many masters will not agree to work with a woman if they know that she is pregnant or nursing, as there is a recommendation to wait a year after giving birth before getting a tattoo. However, there is no evidence that tattoos have any effect on milk. When choosing a master, it is very important to check whether he observes adequate hygiene measures, otherwise you can pick up a local or even general infection. Some local health authorities may have specific guidelines for this, so you may want to start your search there. The tattoo artist must follow general precautions: sterilize instruments in an autoclave, use disposable needles, check the sterility of ink, and also work with gloves. If these precautions are not followed, infections such as hepatitis, tetanus, and even HIV can be contracted.
If these precautions are not followed, infections such as hepatitis, tetanus, and even HIV can be contracted.
If you decide to get a tattoo, be sure to wash the tattooed body part with mild soap and water to prevent local infection. Try not to scratch the tattoo site and keep it out of the sun.
Laser tattoo removal can be performed safely on breastfeeding women. The laser breaks the tattoo pigments into small pieces and allows the body to filter them out on its own. There is no bleeding and the whole procedure has minimal side effects.
• Avoid fish found to be highly contaminated with mercury and PCBs (polychlorinated biphenyls), such as shark, swordfish, king mackerel (found in Japanese restaurants), tilefish (also known as cabezon or malacant), and wild-caught fish. in contaminated waters, especially in the Great Lakes.
• Eat foods low in animal fats, choose lean meats and low fat dairy products.
• Don't smoke and avoid people who smoke around you.
• Thoroughly wash fresh vegetables and fruits and peel them. Avoid forced diets - they can increase the penetration of toxic substances into breast milk.
• If you work with chemicals, ask your doctor to refer you to a specialist who can advise you on their safety.
Preparing for a normal birth
In the past two decades, the number of women who received epidural anesthesia during childbirth, as well as those who gave birth by caesarean section, has increased many times over. Today we know that these high-tech interventions often affect breastfeeding.
Difficult births often end in the separation of mother and child. This can make it difficult to start breastfeeding. Often, difficult labor also results in a later delivery of milk. Causes can vary: prolonged contractions, epidural anesthesia, the use of artificial oxytocin (pitocin) to intensify or start contractions, and the administration of large volumes of intravenous fluids. If milk has not come in more than 72 hours after delivery, the newborn may develop jaundice and lose too much weight and need to be supplemented.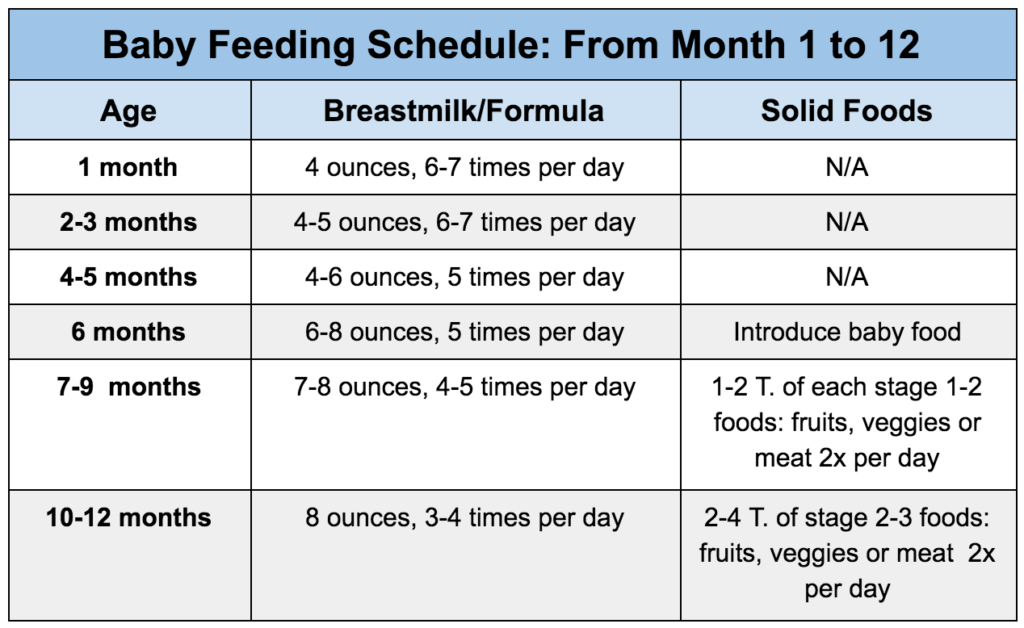 In such a situation, the likelihood that the mother will stop breastfeeding increases.
In such a situation, the likelihood that the mother will stop breastfeeding increases.
Difficult labor often does not start naturally, but is triggered by the doctor opening the amniotic sac. Your doctor may suggest this when your due date is approaching or past. Artificially induced contractions often lead to the need for other medical interventions. Opening the membranes may or may not cause contractions, but it certainly increases the risk of infection for both mother and child. As soon as the bubble is opened, the clock starts ticking. In most cases, it becomes necessary to have a baby within 24 hours to prevent infection.
Sometimes induced labor is justified because of a problematic pregnancy. It may be risky for a baby to remain in the uterus if the pregnancy has gone on for 42 weeks, if the mother has high blood pressure or an intrauterine infection, or if she has other health problems such as diabetes. Induction of labor may also be necessary if the baby stops growing or when there is very little amniotic fluid. However, many doctors induce labor in the name of the convenience of the mother, healthcare workers, and hospital staff. The doctor may advertise induced labor to the mother, describing it as a routine procedure to avoid an emergency trip to the hospital in the middle of the night, to ensure the presence of certain family members on the spot, or expressing concern about the size of the baby. Some mothers may demand that they go into labor just because they are tired of being pregnant.
However, many doctors induce labor in the name of the convenience of the mother, healthcare workers, and hospital staff. The doctor may advertise induced labor to the mother, describing it as a routine procedure to avoid an emergency trip to the hospital in the middle of the night, to ensure the presence of certain family members on the spot, or expressing concern about the size of the baby. Some mothers may demand that they go into labor just because they are tired of being pregnant.
None of the above is sufficient reason to initiate labor artificially. Large-scale studies confirm that induction of labor increases the likelihood of difficult labor and operative delivery without improving neonatal outcomes.
Nature begins to prepare for childbirth during the last weeks of pregnancy. The baby descends into the pelvis; the cervix moves forward and begins to soften. The lungs of the baby mature, he receives maternal antibodies that will protect him from infections in the first weeks of life, and acquires a fatty layer.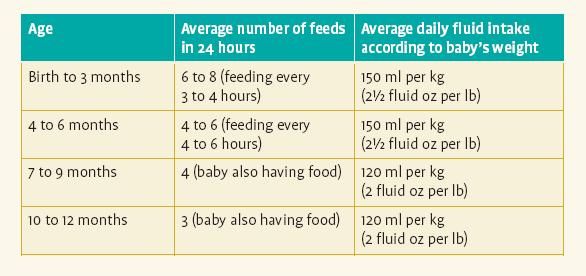 His body accumulates more iron, he develops the ability to coordinate sucking and swallowing. When the baby is ready to be born, it releases a small amount of the hormone, which in turn stimulates the mother's body to produce hormones that start labor. When the baby is ready, and the maternal hormones, and the uterus, and its cervix, and the placenta, then the contractions begin. If contractions begin spontaneously, labor is usually easier, and babies are more likely to be born ready to suckle.
His body accumulates more iron, he develops the ability to coordinate sucking and swallowing. When the baby is ready to be born, it releases a small amount of the hormone, which in turn stimulates the mother's body to produce hormones that start labor. When the baby is ready, and the maternal hormones, and the uterus, and its cervix, and the placenta, then the contractions begin. If contractions begin spontaneously, labor is usually easier, and babies are more likely to be born ready to suckle.
If a mother has agreed to an induced labor, she usually arrives at the hospital before labor or even labor of any kind begins. If she was incorrectly determined the expected date of birth, the baby may be born a few weeks ahead of schedule. Functionally immature preterm infants have an increased risk of complications such as temperature instability, low blood sugar, breathing problems and jaundice. Babies born three or more weeks premature often do not suckle well until around the time they should have been born.
If the rupture of the amniotic sac does not lead to effective contractions, they can be enhanced with artificial oxytocin (pitocin). During normal contractions, the mother produces her own oxytocin, which causes the body to also produce endorphins, natural painkillers. Pitocin, administered intravenously, does not reach the brain and thus does not stimulate the release of natural endorphins. In addition to being more painful, pitocin-induced contractions often last longer, and the uterus cannot fully relax between contractions due to pitocin. Because pitocin increases stress on both the uterine muscles and the baby, the mother will need to be constantly connected to a fetal cardiotocography (CTG) machine. As a result, she may be confined to the bed instead of helping the contractions by moving freely, and may not be able to take a relaxing shower or bath to relieve the pain. A recent study looking at several thousand first births found that births that were artificially initiated—by bladder puncture, pitocin, or both—increased the chance of a caesarean section by at least four to a maximum of ten.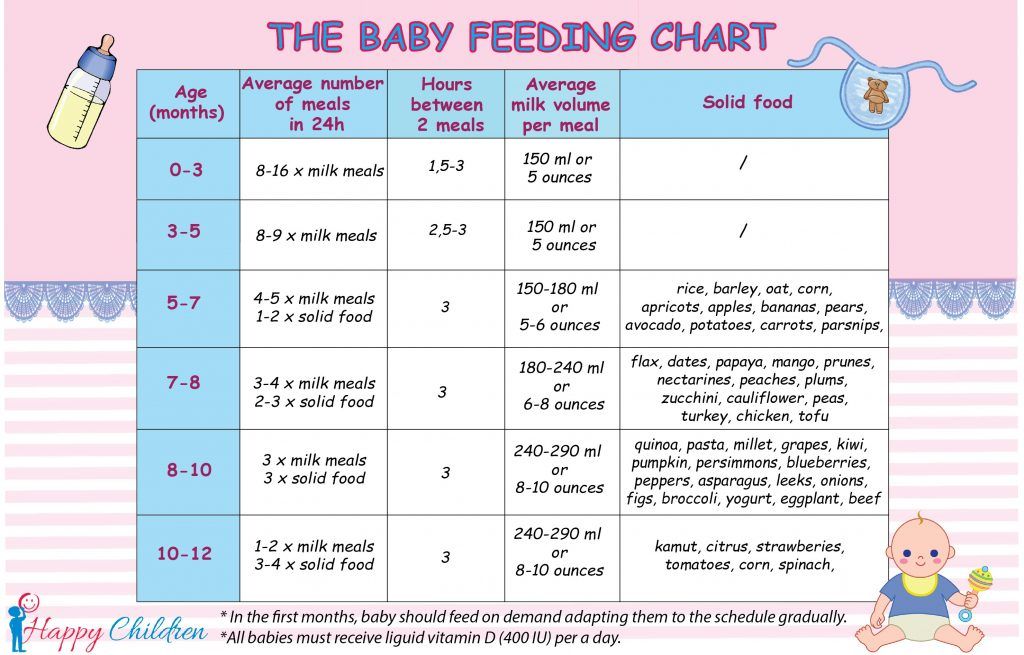 Many of these women and the rest of their children will be delivered by caesarean section.
Many of these women and the rest of their children will be delivered by caesarean section.
For induced or spontaneous labor, most women these days opt for epidural anesthesia, the injection of anesthesia and anesthetic into the space around the spinal cord. The drugs block nerve impulses from the lower spinal cord, and as a result, the patient feels less of the lower body.
80 percent of women are convinced that in their case, epidural anesthesia qualitatively relieves pain from contractions. However, undesirable complications can result from it. Childbirth usually lasts longer. The contractions themselves become weaker and less frequent as the epidural reduces the production of the mother's own oxytocin, which is the substance that causes the uterus to contract. This means that she is more likely to need artificial oxytocin. She won't be able to experience that burst of oxytocin that produces the strongest contractions at the end of labor, when the baby is born, and that helps a mother fall in love with her baby at first sight.
Epidural anesthesia has other side effects. Because the drug blocks the nerves that regulate blood pressure, one-third of women who receive an epidural experience a drop in blood pressure, and in 12 percent of the cases, the drop is severe enough to cause the infant to noticeably lack oxygen. To prevent a drop in blood pressure, mothers can give large amounts of fluid intravenously before the epidural is given. Because of this liquid, milk may come later.
If a mother receives both an epidural and pitocin, the baby's heartbeat may be affected. A study of primiparous mothers who received both interventions found that in half of the cases, births ended in caesarean section due to the pathological condition of the fetus.
Epidurals also often cause relaxation of the pelvic floor muscles, which can affect the ability of the infant's head to adjust and turn as it passes through the birth canal. This can lead to malposition (that is, the baby will fall facing the stomach or side of the mother), which makes childbirth difficult, or that he will not be able to lower himself at all, which becomes an indication for a caesarean section. An epidural also reduces a woman's ability to push (and some can't move her lower body at all), which may make it necessary to resort to forceps or a vacuum. The likelihood of a caesarean section increases three times if a woman was given an epidural. After epidural anesthesia, the risk of severe postpartum hemorrhage also increases.
An epidural also reduces a woman's ability to push (and some can't move her lower body at all), which may make it necessary to resort to forceps or a vacuum. The likelihood of a caesarean section increases three times if a woman was given an epidural. After epidural anesthesia, the risk of severe postpartum hemorrhage also increases.
Approximately 24 percent of women develop a fever after an epidural. Because any fever could mean an infection in the mother, the baby will need to be tested. If he also has a temperature, he will be subjected to new tests and will be treated with antibiotics. One large study found that mothers who had a fever during labor were more likely to have babies with low Apgar scores, low muscle tone, and seizures than mothers with normal temperatures. And a baby who is being tested and treated for a temperature is separated from her mother at the very hours when it is best to start breastfeeding.
Normal Birth Preparation
• Attend a Birth Preparation course, best taught by a certified Lamaze or Bradley instructor, to learn more about normal childbirth.
• Realize that EDD (estimated due date) is very approximate. Tell your doctor and midwife that you prefer to wait until labor begins on its own.
• If your doctor or midwife is concerned about your baby, ask for a CTG every two or three days to make sure your baby is doing well.
• Stay at home during the initial stages of labor until your water breaks or until you have contractions that are a minute every three to four minutes.
• Consider hiring a doula to help you through all the stages of labor
• Bathing or showering are good ways to reduce the intensity of your contractions.
• Try to avoid an epidural until the contractions are intense and the cervix dilates to 5 cm.
• Once the cervix is fully dilated, assume upright postures so that gravity works for you; in this position, the diameter of the pelvic opening increases, and it is easier for the baby to descend through the birth canal.
• When you start pushing, try to rest between pushing.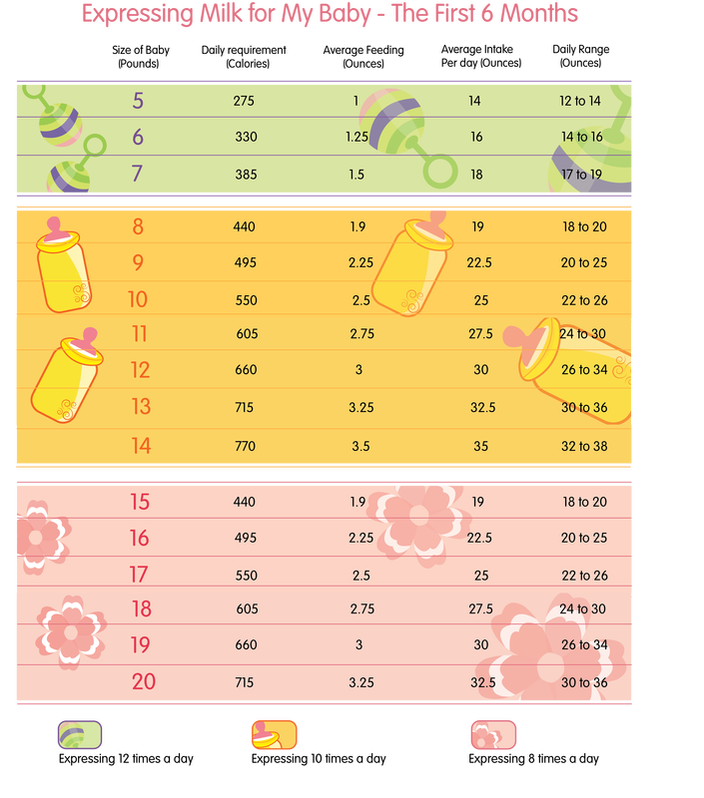 Push only when you are pushing or when your midwife advises you to do so. Push briefly, each time for 4-6 seconds - you need to conserve strength.
Push only when you are pushing or when your midwife advises you to do so. Push briefly, each time for 4-6 seconds - you need to conserve strength.
Not only are mothers whose labors are lengthened and complicated by medical interventions often come late, but their babies are often less active at the breast. A baby is usually most likely to suckle if it is born without both intravenous anesthesia and epidural anesthesia. Conversely, an infant suckles less actively if its mother was given intravenous or epidural medications during labor. Despite successful pain relief, many women after epidural anesthesia remain dissatisfied with their childbirth.
If you are sure that you want to relieve pain during childbirth, you can ask for an epidural, controlled by the patient herself. Such an opportunity is available in many maternity hospitals and birth centers. This allows the mother to add her dose of anesthesia and anesthesia when she feels the need. The dose is small, so it turns off pain receptors, but allows more movement in bed. Once the cervix is fully dilated, the epidural can be turned off so that the woman can respond to pushing. Mothers usually recover better from this anesthesia, walk earlier, which helps restore normal bladder function and may also prevent increased bleeding. Since the baby receives less anesthesia this way, the baby is more likely to show normal interest in and ability to latch on to the breast.
Once the cervix is fully dilated, the epidural can be turned off so that the woman can respond to pushing. Mothers usually recover better from this anesthesia, walk earlier, which helps restore normal bladder function and may also prevent increased bleeding. Since the baby receives less anesthesia this way, the baby is more likely to show normal interest in and ability to latch on to the breast.
If you are having a planned caesarean
There is a lot of evidence that a baby born more than seven days before due date may face some difficulties. Breathing problems, infections, low blood sugar, and the need for intensive care are especially common in babies born at 37 weeks or earlier. These problems usually result in mother-infant separation and delayed initiation of breastfeeding. In addition, babies born at 37 weeks or earlier often have poor suckling ability (see Severely Preterm or Sick Baby, page 151).
Despite these risks, one third of caesarean sections are performed before 39 weeks' gestation.