Best way to bottle feed newborn baby
How to Bottle-Feed a Baby
Whether you’re breastfeeding, formula-feeding or doing a combination of both, chances are you’ll eventually use a bottle with your infant. No big deal, right? But while images of a parent blissfully holding a bottle make the process look easy, there’s a learning curve when it comes to proper bottle-feeding. Here, everything you need to know about how to bottle-feed a baby safely and happily.
In this article:
How to choose the right bottle and nipple
How to make a baby bottle
Best bottle-feeding positions
What is pace feeding?
How to get baby to take a bottle
When to wean baby off the bottle
How to Choose the Right Bottle and Nipple
When it comes to figuring out how to bottle-feed a baby, selecting an appropriate bottle and nipple is step one. If people gifted you a bunch of bottles at your baby shower, you may want to hold off before opening and sterilizing them until baby is born, or at least take out just a few to try in the early days of feeding. Why? Because you won’t know what kind of bottle is best until you figure out what baby’s feeding needs are.
“Certain bottles work better for certain babies,” explains Jamie O’Day, BSN, RN, CLC, a registered nurse, certified lactation consultant and cofounder of Boston NAPS, a pre- and postnatal resource center in the Boston area. “For example, some babies who have issues with gas may do better with a bottle that has a filtration system, like a Doctor Brown’s style bottle, while babies who are used to being breastfed may have more success drinking from a bottle that aims to mimic the shape and feel of a mother’s breast, like the Comotomo.”
That said, O’Day has a universal tip for all parents: Look for a bottle that’s easy to take apart and clean. That generally means a nice wide neck and the fewest parts possible. “Proper cleaning is so important, so I always tell parents to choose the simplest bottle, which may just have a nipple, bottle and collar,” she says. If your child seems happy and easily takes the bottle, then there’s no need to switch.
Of course, it’s not just the bottle that you have to consider. It’s also important to pay attention to the flow of the nipple, which varies based on infant age. Generally speaking, young babies need a slower flow, while older babies who’ve mastered the art of bottle-feeding can handle a faster flow. The nipple may be called “slow flow,” “medium flow” or “fast flow” or may be numbered from one to three, with one being the slowest flow. There is no standard of flow between different brands, but most newborns should begin on level one or slow flow.
So how can you tell when it’s time to change the nipple size? That depends. Some infants happily use the same flow nipple throughout their infancy, while others may need a faster flow nipple. “If you notice your child taking a long time to finish a bottle, or losing interest midway through feedings, a faster flow nipple may be needed,” O’Day says, adding that this might happen at around 3 or 4 months of age, with another potential upgrade around 6 or 7 months.
If your infant finishes a bottle quickly (say, under five minutes), seems gassy or cranky, or spits up a lot of milk right after feedings, it may be time to go back to a slower-flow nipple. Your pediatrician can also help determine if it may be time to switch the flow of the nipple.
How to Make a Baby Bottle
If you’re wondering how to bottle-feed a baby, you’re probably new to prepping baby bottles. Take a new skill, add in sleep deprivation and sprinkle in some very real safety concerns and you’ve got the somewhat daunting process of making a baby bottle (at least at first). Don’t despair. By reading directions, following the advice of a pediatrician and making sure to err on the side of caution, you’ll get the hang of it in no time.
How to make a baby bottle with formula
Baby formula comes in three different forms: ready-to-feed, concentrate and powder. The Centers for Disease Control and Prevention (CDC) recommends that babies under 3 months start off with ready-to-feed formula because of the small but real risk of cronobacter, a bacteria that can live in powdered infant formula.
• Preparing ready-to-feed formula: These require very little prep, since they come ready to be poured into a bottle and fed to an infant. Some ready-to-feed formulas come in bottles that can accomodate disposable nipples—all you need to do is screw a nipple on, feed and discard.
• Preparing concentrate formula: To prepare a baby body with this liquid formula, you’ll need to add water. It’s important to read the directions to learn the right ratio of water to concentrate. As for what type of water should you use, that depends on where you live, your pediatrician’s recommendation and your own wishes. If your tap water is safe, feel free to use it—just run it for several minutes before you fill the bottle to remove any trace contaminants in the water. You can also use filtered water, bottled water or boiled (and cooled) tap water.
• Preparing powdered formula: Just like concentrate, it’s important to follow directions on the right ratio of scoops of powder to ounces of water, says Carmen Baker-Clark, an International Board Certified Lactation Consultant (IBCLC) in Hoboken, New Jersey. When using powdered formula, make sure to shake well so the liquid isn’t clumpy. “Some parents notice powdered formulas may make their infant more gassy, more prone to spit-up or more constipated. A lot of this is due to the bottle preparation. For example, not shaking enough can create uneven consistency that may be harder for baby to digest,” Baker-Clark explains.
When using powdered formula, make sure to shake well so the liquid isn’t clumpy. “Some parents notice powdered formulas may make their infant more gassy, more prone to spit-up or more constipated. A lot of this is due to the bottle preparation. For example, not shaking enough can create uneven consistency that may be harder for baby to digest,” Baker-Clark explains.
Regardless of what kind of formula you choose, Baker-Clark recommends sticking with the same brand or being deliberate as you try new ones, instead of just using whatever formula is on sale. While all infant formulas are regulated by the FDA and must pass the same nutrient tests, babies may react differently to various brands of formula. If an infant has frequent reflux, crying episodes or seems uncomfortable after a feeding, speak with your pediatrician. Your child may have an allergy or intolerance and may need a special formula.
Whether you warm the bottle up is up to you. “Many infants have no problem taking a cold bottle and the advantage is that you then don’t need to warm a bottle when you’re on the go,” Baker-Clark says. Once a formula bottle has been made and the nipple has touched baby’s lips, the bottle is good for an hour. But if the bottle isn’t used, a bottle may be refrigerated for a day, O’Day says. Some parents like to prepare and refrigerate a bottle in advance to make middle-of-the-night feedings easier, while others may prepare a pitcher to use during the day.
Once a formula bottle has been made and the nipple has touched baby’s lips, the bottle is good for an hour. But if the bottle isn’t used, a bottle may be refrigerated for a day, O’Day says. Some parents like to prepare and refrigerate a bottle in advance to make middle-of-the-night feedings easier, while others may prepare a pitcher to use during the day.
How to make a baby bottle with breast milk
Preparing a bottle of breast milk is of course much more straightforward, since the milk itself is ready to go. But when grabbing a bag of breast milk to use, it’s important to keep an eye on when it was pumped and how it’s been stored since. According to breast milk storage guidelines, it’s safe to use freshly pumped milk that’s been stored at room temperature for up to four hours, in the fridge for up to four days or in the freezer for up to 12 months. Always use the oldest milk first. If baby doesn’t finish a bottle, you can offer it again within two hours of the last feeding.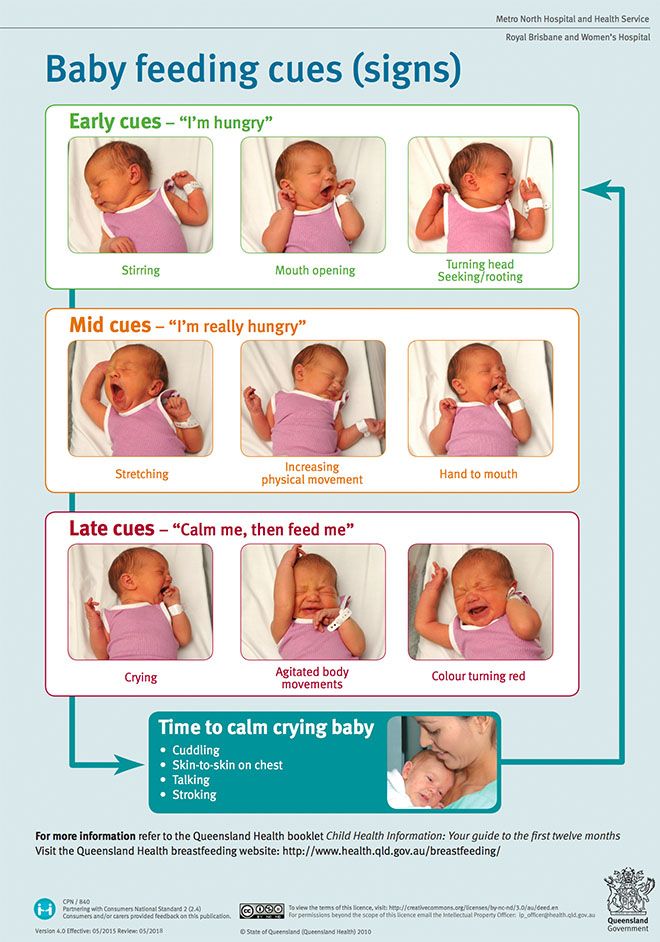
Before giving baby the bottle, you can warm the milk up by placing the bottle (or milk storage bag) in a cup of warm water for a few minutes, or pop the bottle into a bottle warmer. Whatever you do, steer clear of the microwave, which can cause dangerous hot spots.
Best Bottle-Feeding Positions
How you hold your little one during a feeding is a crucial part of knowing how to bottle-feed a baby properly. Chances are, you’ve come across loads of images of parents bottle-feeding babies—but the positions you sometimes see in photos or on TV may not actually be the best for baby. For one, forget about laying baby across your lap. “Have you ever easily drank something while you lay on your back?” O’Day asks. (Answer: no.) “It’s the same for baby.” Not only can a back position lead to reflux, but it may also cause ear infections. Try these bottle-feeding positions instead:
• Cradle baby in your arms. This is the classic position you probably think of when you imagine giving baby a bottle. In this bottle-feeding position, baby’s head rests in the crook of your arm as you hold her head and chest at a slight incline—close to your chest is great.
In this bottle-feeding position, baby’s head rests in the crook of your arm as you hold her head and chest at a slight incline—close to your chest is great.
• Hold baby upright. Instead of lying down, baby should be almost in a seated position, with his head on your chest or in the crook of your arm. “This position can work especially well for infants who have reflux,” Baker-Clark says. Tilt the bottle so the milk completely fills the nipple, since a nipple filled only halfway with milk may lead to baby gulping some air, which can lead to gassiness or reflux.
• Use a pillow. A nursing pillow can be helpful in keeping baby’s chest and head propped up at an angle. Bonus: It can give your arms a break too as you cradle baby in your lap.
• Switch sides. Regardless of whether you’re breastfeeding or bottle-feeding exclusively, switching baby from one side to another can help prevent your little one from developing a side preference and can give your arms a break. Switching sides can also naturally pace a feeding session and can give baby a chance to decide whether or not he’s full before the bottle is finished.
Switching sides can also naturally pace a feeding session and can give baby a chance to decide whether or not he’s full before the bottle is finished.
As baby gets older, she may toy with holding the bottle. That’s fine, if she wants to, but it’s not a developmental milestone. “She may want to hold the bottle at 6 months, so you can let her, but you should still be close by, holding her and supervising her,” O’Day says. And if baby doesn’t show any interest in holding her bottle? As long as she’s reached other developmental milestones, like reaching or grasping for toys, it’s totally normal if your older infant wants his bottle served to him.
What is Pace Feeding?
You may have heard of “pace feeding” and wondered how to bottle-feed a baby using this method. “Paced bottle-feeding is where you follow baby’s cues and allow for breaks,” Baker-Clark says. “Taking the bottle away and re-offering it benefits both breastfed and exclusively bottle-fed babies.”
Pace feeding helps babies learn to regulate their hunger and allows ample time for digestion. It can also cue you into baby’s biorhythm, O’Day says. You may find baby doesn’t uniformly eat the same size bottle at each time of day. For example, maybe he’s extra hungry in the morning and drinks 8 ounces, but prefers 4-ounce bottles post-nap. Paying attention to baby’s cues can help you clue into her unique needs and natural schedule.
It can also cue you into baby’s biorhythm, O’Day says. You may find baby doesn’t uniformly eat the same size bottle at each time of day. For example, maybe he’s extra hungry in the morning and drinks 8 ounces, but prefers 4-ounce bottles post-nap. Paying attention to baby’s cues can help you clue into her unique needs and natural schedule.
Plus, paced bottle-feeding makes a feeding session—which can last about 15 to 20 minutes—a great time for baby and his caregiver to bond. Here, some tips for how to pace feed:
• Hold the bottle at a horizontal angle. When the bottle is held horizontally, baby has to work to pull milk from the bottle, instead of the milk dripping into her mouth.
• Give baby some breaks. Instead of pulling the bottle away from baby’s mouth, lean the bottle back so the milk leaves the nipple. That way, baby has a chance to catch his breath. If he seems like he’s still rooting for milk, offer him more.
• Burp mid-feed. “If baby is pulling away, seems fussy or seems to be playing with the nipple with her mouth, give her a burp,” O’Day says. Then offer the bottle again.
“If baby is pulling away, seems fussy or seems to be playing with the nipple with her mouth, give her a burp,” O’Day says. Then offer the bottle again.
How to Get Baby to Take a Bottle
Even if you’re planning to exclusively breastfeed, at some point you’ll likely need some pointers on how to get baby to take a bottle. “I tell my clients to introduce baby to a bottle once breastfeeding has been established, which depends on each mother-baby dyad, but on average, it’s around one month,” O’Day says. “Even if they’re not planning to regularly bottle-feed, doing so can give peace of mind if an emergency comes up, and can also be a way for mom to get a break.”
Some babies take a bottle no problem—after all, sucking is an instinctive reflex, which is why bottle-fed babies tend to get the hang of it in the first few days of life. But other breastfed babies may initially be reluctant to take a bottle. And sometimes breastfed babies have no issue taking a bottle when they’re one month old, but if a bottle hasn’t been regularly offered, by 3 or 4 months of age, they’re less happy to accept a bottle. Bottle resistance is pretty common, but luckily there are some tried-and-true tips for what to do when baby is refusing a bottle.
Bottle resistance is pretty common, but luckily there are some tried-and-true tips for what to do when baby is refusing a bottle.
• Offer often. Even if you’re breastfeeding, O’Day recommends giving baby at least one bottle a week, once breastfeeding has been established. “That way it’s part of their routine, so they’re less likely to resist it,” she says.
• Don’t offer it when baby is starving. If you’re regularly nursing your infant, O’Day suggests offering a bottle in between nursing sessions. “If they’re too hungry, they may be too worked up to take a bottle. If they’re calm and not super hungry, they may take it,” she explains.
• Let others try bottle-feeding. Some moms have success leaving the house and allowing their partner to try feeding baby a bottle. Again, try it at a time that’s not baby’s “must-feed” time.
• Don’t get frustrated. If baby isn’t taking the bottle, O’Day suggests putting it down and trying again later rather than forcing it, which can make both you and baby upset.
• Ask for help. A lactation consultant can suggest some techniques to help get even the most resistant bottle-feeders to accept a bottle. They may check your infant’s mouth and tongue for any latch problems that could contribute to the difficulty, suggest the best bottle for your infant, troubleshoot any behavioral issues or offer alternate nutritive methods, such as cup- or syringe-feeding.
When to Wean Baby Off the Bottle
The American Academy of Pediatrics recommends parents stop offering bottles by 18 months due to tooth decay concern, but it’s smart to talk with your pediatrician about exactly when baby should wean from the bottle around the 9-month mark, O’Day says. “How and when to wean depends on how much table food baby is eating, any developmental concerns and your pediatrician’s assessment,” she says. Note, though, that cow’s milk shouldn’t be introduced until baby is 12 months old.
When baby is around 6 months old, offer a sippy cup or straw cup for water, O’Day says, since learning to drink from cups can help make the transition from bottles seamless. Some babies have no problem giving up the bottle, while others may require more time to make the transition, but looping in your pediatrician or lactation consultant can help make sure you’re all on the right track.
Some babies have no problem giving up the bottle, while others may require more time to make the transition, but looping in your pediatrician or lactation consultant can help make sure you’re all on the right track.
Whether you’re breastfeeding and offering the occasional bottle, combo-feeding or exclusively bottle-feeding, you might hit some bumps along your bottle-feeding journey. But there are ways to navigate through any problems that arise. If you’re struggling to find the best baby bottle for your child, need some pointers on how to bottle-feed a baby in an optimal position or encounter a full-on bottle strike, reach out to your pediatrician or lactation consultants for guidance.
Published August 2018
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances.
Plus, more from The Bump:
14 Best Bottles for Every Feeding Need
Pumping 101: How to Pump Breast Milk
The Best Baby Formulas for Your Child’s Needs
How to Bottle-Feed a Baby
Whether you’re breastfeeding, formula-feeding or doing a combination of both, chances are you’ll eventually use a bottle with your infant. No big deal, right? But while images of a parent blissfully holding a bottle make the process look easy, there’s a learning curve when it comes to proper bottle-feeding. Here, everything you need to know about how to bottle-feed a baby safely and happily.
In this article:
How to choose the right bottle and nipple
How to make a baby bottle
Best bottle-feeding positions
What is pace feeding?
How to get baby to take a bottle
When to wean baby off the bottle
How to Choose the Right Bottle and Nipple
When it comes to figuring out how to bottle-feed a baby, selecting an appropriate bottle and nipple is step one. If people gifted you a bunch of bottles at your baby shower, you may want to hold off before opening and sterilizing them until baby is born, or at least take out just a few to try in the early days of feeding. Why? Because you won’t know what kind of bottle is best until you figure out what baby’s feeding needs are.
If people gifted you a bunch of bottles at your baby shower, you may want to hold off before opening and sterilizing them until baby is born, or at least take out just a few to try in the early days of feeding. Why? Because you won’t know what kind of bottle is best until you figure out what baby’s feeding needs are.
“Certain bottles work better for certain babies,” explains Jamie O’Day, BSN, RN, CLC, a registered nurse, certified lactation consultant and cofounder of Boston NAPS, a pre- and postnatal resource center in the Boston area. “For example, some babies who have issues with gas may do better with a bottle that has a filtration system, like a Doctor Brown’s style bottle, while babies who are used to being breastfed may have more success drinking from a bottle that aims to mimic the shape and feel of a mother’s breast, like the Comotomo.”
That said, O’Day has a universal tip for all parents: Look for a bottle that’s easy to take apart and clean. That generally means a nice wide neck and the fewest parts possible. “Proper cleaning is so important, so I always tell parents to choose the simplest bottle, which may just have a nipple, bottle and collar,” she says. If your child seems happy and easily takes the bottle, then there’s no need to switch.
“Proper cleaning is so important, so I always tell parents to choose the simplest bottle, which may just have a nipple, bottle and collar,” she says. If your child seems happy and easily takes the bottle, then there’s no need to switch.
Of course, it’s not just the bottle that you have to consider. It’s also important to pay attention to the flow of the nipple, which varies based on infant age. Generally speaking, young babies need a slower flow, while older babies who’ve mastered the art of bottle-feeding can handle a faster flow. The nipple may be called “slow flow,” “medium flow” or “fast flow” or may be numbered from one to three, with one being the slowest flow. There is no standard of flow between different brands, but most newborns should begin on level one or slow flow.
So how can you tell when it’s time to change the nipple size? That depends. Some infants happily use the same flow nipple throughout their infancy, while others may need a faster flow nipple. “If you notice your child taking a long time to finish a bottle, or losing interest midway through feedings, a faster flow nipple may be needed,” O’Day says, adding that this might happen at around 3 or 4 months of age, with another potential upgrade around 6 or 7 months.
If your infant finishes a bottle quickly (say, under five minutes), seems gassy or cranky, or spits up a lot of milk right after feedings, it may be time to go back to a slower-flow nipple. Your pediatrician can also help determine if it may be time to switch the flow of the nipple.
How to Make a Baby Bottle
If you’re wondering how to bottle-feed a baby, you’re probably new to prepping baby bottles. Take a new skill, add in sleep deprivation and sprinkle in some very real safety concerns and you’ve got the somewhat daunting process of making a baby bottle (at least at first). Don’t despair. By reading directions, following the advice of a pediatrician and making sure to err on the side of caution, you’ll get the hang of it in no time.
How to make a baby bottle with formula
Baby formula comes in three different forms: ready-to-feed, concentrate and powder. The Centers for Disease Control and Prevention (CDC) recommends that babies under 3 months start off with ready-to-feed formula because of the small but real risk of cronobacter, a bacteria that can live in powdered infant formula.
• Preparing ready-to-feed formula: These require very little prep, since they come ready to be poured into a bottle and fed to an infant. Some ready-to-feed formulas come in bottles that can accomodate disposable nipples—all you need to do is screw a nipple on, feed and discard.
• Preparing concentrate formula: To prepare a baby body with this liquid formula, you’ll need to add water. It’s important to read the directions to learn the right ratio of water to concentrate. As for what type of water should you use, that depends on where you live, your pediatrician’s recommendation and your own wishes. If your tap water is safe, feel free to use it—just run it for several minutes before you fill the bottle to remove any trace contaminants in the water. You can also use filtered water, bottled water or boiled (and cooled) tap water.
• Preparing powdered formula: Just like concentrate, it’s important to follow directions on the right ratio of scoops of powder to ounces of water, says Carmen Baker-Clark, an International Board Certified Lactation Consultant (IBCLC) in Hoboken, New Jersey. When using powdered formula, make sure to shake well so the liquid isn’t clumpy. “Some parents notice powdered formulas may make their infant more gassy, more prone to spit-up or more constipated. A lot of this is due to the bottle preparation. For example, not shaking enough can create uneven consistency that may be harder for baby to digest,” Baker-Clark explains.
When using powdered formula, make sure to shake well so the liquid isn’t clumpy. “Some parents notice powdered formulas may make their infant more gassy, more prone to spit-up or more constipated. A lot of this is due to the bottle preparation. For example, not shaking enough can create uneven consistency that may be harder for baby to digest,” Baker-Clark explains.
Regardless of what kind of formula you choose, Baker-Clark recommends sticking with the same brand or being deliberate as you try new ones, instead of just using whatever formula is on sale. While all infant formulas are regulated by the FDA and must pass the same nutrient tests, babies may react differently to various brands of formula. If an infant has frequent reflux, crying episodes or seems uncomfortable after a feeding, speak with your pediatrician. Your child may have an allergy or intolerance and may need a special formula.
Whether you warm the bottle up is up to you. “Many infants have no problem taking a cold bottle and the advantage is that you then don’t need to warm a bottle when you’re on the go,” Baker-Clark says. Once a formula bottle has been made and the nipple has touched baby’s lips, the bottle is good for an hour. But if the bottle isn’t used, a bottle may be refrigerated for a day, O’Day says. Some parents like to prepare and refrigerate a bottle in advance to make middle-of-the-night feedings easier, while others may prepare a pitcher to use during the day.
Once a formula bottle has been made and the nipple has touched baby’s lips, the bottle is good for an hour. But if the bottle isn’t used, a bottle may be refrigerated for a day, O’Day says. Some parents like to prepare and refrigerate a bottle in advance to make middle-of-the-night feedings easier, while others may prepare a pitcher to use during the day.
How to make a baby bottle with breast milk
Preparing a bottle of breast milk is of course much more straightforward, since the milk itself is ready to go. But when grabbing a bag of breast milk to use, it’s important to keep an eye on when it was pumped and how it’s been stored since. According to breast milk storage guidelines, it’s safe to use freshly pumped milk that’s been stored at room temperature for up to four hours, in the fridge for up to four days or in the freezer for up to 12 months. Always use the oldest milk first. If baby doesn’t finish a bottle, you can offer it again within two hours of the last feeding.
Before giving baby the bottle, you can warm the milk up by placing the bottle (or milk storage bag) in a cup of warm water for a few minutes, or pop the bottle into a bottle warmer. Whatever you do, steer clear of the microwave, which can cause dangerous hot spots.
Best Bottle-Feeding Positions
How you hold your little one during a feeding is a crucial part of knowing how to bottle-feed a baby properly. Chances are, you’ve come across loads of images of parents bottle-feeding babies—but the positions you sometimes see in photos or on TV may not actually be the best for baby. For one, forget about laying baby across your lap. “Have you ever easily drank something while you lay on your back?” O’Day asks. (Answer: no.) “It’s the same for baby.” Not only can a back position lead to reflux, but it may also cause ear infections. Try these bottle-feeding positions instead:
• Cradle baby in your arms. This is the classic position you probably think of when you imagine giving baby a bottle. In this bottle-feeding position, baby’s head rests in the crook of your arm as you hold her head and chest at a slight incline—close to your chest is great.
In this bottle-feeding position, baby’s head rests in the crook of your arm as you hold her head and chest at a slight incline—close to your chest is great.
• Hold baby upright. Instead of lying down, baby should be almost in a seated position, with his head on your chest or in the crook of your arm. “This position can work especially well for infants who have reflux,” Baker-Clark says. Tilt the bottle so the milk completely fills the nipple, since a nipple filled only halfway with milk may lead to baby gulping some air, which can lead to gassiness or reflux.
• Use a pillow. A nursing pillow can be helpful in keeping baby’s chest and head propped up at an angle. Bonus: It can give your arms a break too as you cradle baby in your lap.
• Switch sides. Regardless of whether you’re breastfeeding or bottle-feeding exclusively, switching baby from one side to another can help prevent your little one from developing a side preference and can give your arms a break.![]() Switching sides can also naturally pace a feeding session and can give baby a chance to decide whether or not he’s full before the bottle is finished.
Switching sides can also naturally pace a feeding session and can give baby a chance to decide whether or not he’s full before the bottle is finished.
As baby gets older, she may toy with holding the bottle. That’s fine, if she wants to, but it’s not a developmental milestone. “She may want to hold the bottle at 6 months, so you can let her, but you should still be close by, holding her and supervising her,” O’Day says. And if baby doesn’t show any interest in holding her bottle? As long as she’s reached other developmental milestones, like reaching or grasping for toys, it’s totally normal if your older infant wants his bottle served to him.
What is Pace Feeding?
You may have heard of “pace feeding” and wondered how to bottle-feed a baby using this method. “Paced bottle-feeding is where you follow baby’s cues and allow for breaks,” Baker-Clark says. “Taking the bottle away and re-offering it benefits both breastfed and exclusively bottle-fed babies.”
Pace feeding helps babies learn to regulate their hunger and allows ample time for digestion. It can also cue you into baby’s biorhythm, O’Day says. You may find baby doesn’t uniformly eat the same size bottle at each time of day. For example, maybe he’s extra hungry in the morning and drinks 8 ounces, but prefers 4-ounce bottles post-nap. Paying attention to baby’s cues can help you clue into her unique needs and natural schedule.
It can also cue you into baby’s biorhythm, O’Day says. You may find baby doesn’t uniformly eat the same size bottle at each time of day. For example, maybe he’s extra hungry in the morning and drinks 8 ounces, but prefers 4-ounce bottles post-nap. Paying attention to baby’s cues can help you clue into her unique needs and natural schedule.
Plus, paced bottle-feeding makes a feeding session—which can last about 15 to 20 minutes—a great time for baby and his caregiver to bond. Here, some tips for how to pace feed:
• Hold the bottle at a horizontal angle. When the bottle is held horizontally, baby has to work to pull milk from the bottle, instead of the milk dripping into her mouth.
• Give baby some breaks. Instead of pulling the bottle away from baby’s mouth, lean the bottle back so the milk leaves the nipple. That way, baby has a chance to catch his breath. If he seems like he’s still rooting for milk, offer him more.
• Burp mid-feed. “If baby is pulling away, seems fussy or seems to be playing with the nipple with her mouth, give her a burp,” O’Day says. Then offer the bottle again.
“If baby is pulling away, seems fussy or seems to be playing with the nipple with her mouth, give her a burp,” O’Day says. Then offer the bottle again.
How to Get Baby to Take a Bottle
Even if you’re planning to exclusively breastfeed, at some point you’ll likely need some pointers on how to get baby to take a bottle. “I tell my clients to introduce baby to a bottle once breastfeeding has been established, which depends on each mother-baby dyad, but on average, it’s around one month,” O’Day says. “Even if they’re not planning to regularly bottle-feed, doing so can give peace of mind if an emergency comes up, and can also be a way for mom to get a break.”
Some babies take a bottle no problem—after all, sucking is an instinctive reflex, which is why bottle-fed babies tend to get the hang of it in the first few days of life. But other breastfed babies may initially be reluctant to take a bottle. And sometimes breastfed babies have no issue taking a bottle when they’re one month old, but if a bottle hasn’t been regularly offered, by 3 or 4 months of age, they’re less happy to accept a bottle. Bottle resistance is pretty common, but luckily there are some tried-and-true tips for what to do when baby is refusing a bottle.
Bottle resistance is pretty common, but luckily there are some tried-and-true tips for what to do when baby is refusing a bottle.
• Offer often. Even if you’re breastfeeding, O’Day recommends giving baby at least one bottle a week, once breastfeeding has been established. “That way it’s part of their routine, so they’re less likely to resist it,” she says.
• Don’t offer it when baby is starving. If you’re regularly nursing your infant, O’Day suggests offering a bottle in between nursing sessions. “If they’re too hungry, they may be too worked up to take a bottle. If they’re calm and not super hungry, they may take it,” she explains.
• Let others try bottle-feeding. Some moms have success leaving the house and allowing their partner to try feeding baby a bottle. Again, try it at a time that’s not baby’s “must-feed” time.
• Don’t get frustrated. If baby isn’t taking the bottle, O’Day suggests putting it down and trying again later rather than forcing it, which can make both you and baby upset.
• Ask for help. A lactation consultant can suggest some techniques to help get even the most resistant bottle-feeders to accept a bottle. They may check your infant’s mouth and tongue for any latch problems that could contribute to the difficulty, suggest the best bottle for your infant, troubleshoot any behavioral issues or offer alternate nutritive methods, such as cup- or syringe-feeding.
When to Wean Baby Off the Bottle
The American Academy of Pediatrics recommends parents stop offering bottles by 18 months due to tooth decay concern, but it’s smart to talk with your pediatrician about exactly when baby should wean from the bottle around the 9-month mark, O’Day says. “How and when to wean depends on how much table food baby is eating, any developmental concerns and your pediatrician’s assessment,” she says. Note, though, that cow’s milk shouldn’t be introduced until baby is 12 months old.
When baby is around 6 months old, offer a sippy cup or straw cup for water, O’Day says, since learning to drink from cups can help make the transition from bottles seamless. Some babies have no problem giving up the bottle, while others may require more time to make the transition, but looping in your pediatrician or lactation consultant can help make sure you’re all on the right track.
Some babies have no problem giving up the bottle, while others may require more time to make the transition, but looping in your pediatrician or lactation consultant can help make sure you’re all on the right track.
Whether you’re breastfeeding and offering the occasional bottle, combo-feeding or exclusively bottle-feeding, you might hit some bumps along your bottle-feeding journey. But there are ways to navigate through any problems that arise. If you’re struggling to find the best baby bottle for your child, need some pointers on how to bottle-feed a baby in an optimal position or encounter a full-on bottle strike, reach out to your pediatrician or lactation consultants for guidance.
Published August 2018
Please note: The Bump and the materials and information it contains are not intended to, and do not constitute, medical or other health advice or diagnosis and should not be used as such. You should always consult with a qualified physician or health professional about your specific circumstances.
Plus, more from The Bump:
14 Best Bottles for Every Feeding Need
Pumping 101: How to Pump Breast Milk
The Best Baby Formulas for Your Child’s Needs
How to properly bottle feed
Feeding your baby is not only an important process for healthy growth and development, but also a way to establish close emotional contact with the baby and build trusting and loving relationships. The transition from breastfeeding to bottle feeding should be carried out after the mother and the child are fully prepared for this. We are talking about both the moral aspect, and about choosing the right bottle and getting adults the necessary skills so that eating brings only positive emotions and benefits to the baby. In this article, we will talk more about how to properly bottle feed your baby and where to start.
How to prepare your baby for bottle feeding
If this method of feeding is a completely new experience for the baby, or if parents decide to bottle feed their baby from a very young age, slow flow nipples should be preferred. So you protect the child from the possibility of choking while eating. Over time, you can gradually switch to bottles with nipples, which would provide faster and more intense feeding.
So you protect the child from the possibility of choking while eating. Over time, you can gradually switch to bottles with nipples, which would provide faster and more intense feeding.
Feeding bottle selection and daily care
All baby accessories should be kept clean and sterilized regularly and thoroughly.
There are several ways to sterilize dishes:
- select the appropriate mode when using the dishwasher;
- or place the bottle and teat in a vessel of boiling water for 5 minutes.
Before using this method of cleaning the bottle, make sure that the material it is made of can be exposed to high temperatures. Since some types of plastic contain various chemicals in their composition, after sterilization they can become dangerous for their little user. For this reason, experts recommend choosing glass bottles.
The need for thorough cleansing of everything that the baby will touch is caused by the fact that in the first months of life, the child's immune system is just beginning to strengthen.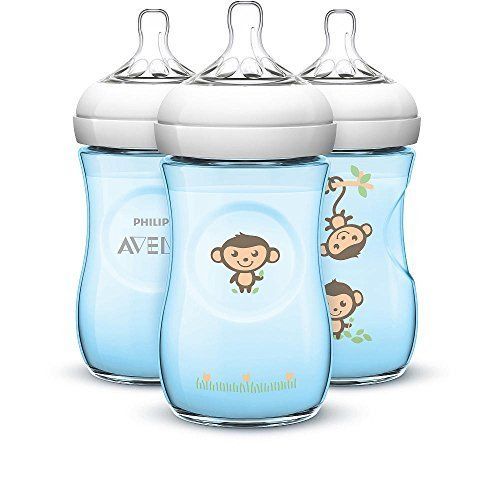 Before sterilizing the teat, it can be cleaned with dishwashing detergent. There are special products for washing children's dishes, without a strong odor and with a safe composition.
Before sterilizing the teat, it can be cleaned with dishwashing detergent. There are special products for washing children's dishes, without a strong odor and with a safe composition.
How to bottle feed your baby
Before starting a meal, mom or dad should wash their hands well with soap and warm running water. Particular attention should be paid to the area between the fingers and under the nails. The hand washing process should take at least 20 seconds. And after carrying out this hygienic procedure, hands should be wiped dry with a paper towel or clean towel.
The next step is to prepare for the meal. If you plan to fill the bottle with formula, then dilute it with water in accordance with the instructions in the instructions. Improper proportions can lead to dehydration or bloating. It should also be remembered that for the preparation of the mixture you need to use only clean drinking water.
Breast milk is the most beneficial for a newborn. Despite this, pediatricians advise breastfeeding babies for as long as possible. Even if the mother is ready to give up breastfeeding, milk can be expressed into a bottle and gradually accustom the baby to the nipple. If, for one reason or another, the mother does not have the opportunity to feed herself, then the only alternative is feeding with a special mixture.
Despite this, pediatricians advise breastfeeding babies for as long as possible. Even if the mother is ready to give up breastfeeding, milk can be expressed into a bottle and gradually accustom the baby to the nipple. If, for one reason or another, the mother does not have the opportunity to feed herself, then the only alternative is feeding with a special mixture.
In the first six months after birth, cow's or goat's milk or its substitute in the form of soy milk should not be included in the baby's diet. Valid options for supporting healthy development of a newborn are breast milk or formula milk only.
What temperature should the bottle filler be? Under no circumstances should the bottle be heated on the stove or in the microwave. If the temperature of the bottle and its filling exceed 37°C, the baby may be burned. It is recommended to use special bottle warmers. If this is not possible, then use the following method:
- put a saucepan on the stove with a little water;
- bring the water to a boil, then remove the pan from the heat;
- place a bottle of milk in a vessel and heat it up to 37◦С;
- check the temperature with a pre-cleaned thermometer or a special device for measuring the temperature of foodstuffs.

You can also check the temperature of the ready-to-use bottle as follows:
- turn the bottle over;
- drip several times into your wrist area.
In this way, you can check not only the temperature of the milk or formula, but also how well the liquid flows out of the bottle. If you have to shake or squeeze the bottle hard to drip, the nipple is blocked and needs to be cleaned out. If, on the contrary, the filler pours out when the bottle is turned over, this means that the nipple is damaged and another nipple should be used to feed the baby, having previously sterilized it.
How to bottle feed your baby lying down
There are several techniques for feeding your baby. However, it is the feeding of the child lying down from the bottle that young parents consider the most comfortable. It is worth noting that eating in this position will only be safe when the baby's head is slightly raised. Otherwise, the child may simply choke. In the prone position, the child should be placed on his arm bent at the elbow. After feeding, you should place the baby in an upright position, taking him in your arms and putting his stomach to your chest.
In the prone position, the child should be placed on his arm bent at the elbow. After feeding, you should place the baby in an upright position, taking him in your arms and putting his stomach to your chest.
Make sure that the feeding bottle is closed correctly: the ring at the connection of the nipple to the bottle must not be too tight. Air must enter the bottle, otherwise a vacuum will be created there, which, in turn, will complicate the consumption of food for the child.
How to bottle feed without spitting up
Since the newborn is not able to fully control the process of feeding, along with milk, he can also take in air. This may be the reason that at one meal the child could not master the planned portion. In view of this, it is recommended to take small breaks during feeding.
As soon as you notice that the baby has stopped sucking on the pacifier, is tired or thoughtful, pick him up and press his face to you, holding his head and back. To help burp excess air, you can make a light massage between the shoulder blades, pat on the back or pope.
To help burp excess air, you can make a light massage between the shoulder blades, pat on the back or pope.
The air will quickly rise up and the baby will burp it without any extra effort. However, you should be prepared for the fact that, along with the air, part of the consumed mixture or milk may also return. Therefore, before taking the baby in your arms, cover yourself with a diaper, because it will be easier to wash it than clothes.
Never leave your baby alone with the bottle or let him fall asleep while using it. After eating, mom or dad must help their child burp. This will help to avoid colic, bloating and other manifestations of stomach discomfort.
Where to buy baby accessories
It's safe to say that I Love Mommy online store is one of the best places to buy baby food. Our catalogs feature products from world-famous brands, the quality of which you will not have to doubt for a minute. Bottles, baby dishes, pacifiers, baby bibs - all this and much more you can buy for your son or daughter from us at affordable prices in just a few minutes.
How to bottle feed: tips and tricks
Kiseleva Elena Sergeevna
Candidate of Medical Sciences, Scientific Advisor MAMAKO ®
Breast milk is the best food for your baby*. But breastfeeding is not possible for all women. For moms who can't breastfeed or keep breastfeeding for as long as they would like, quality infant formula is a healthy alternative.
The best thing is when the baby is in her arms, ideally in skin-to-skin contact: such a position when bottle-feeding, as well as during breastfeeding, creates close contact between mother and baby, helps them get closer, strengthen emotional connection.
Feeding time is a time to be together and communicate with the baby (and for dad too).
The first days of life are a period of adaptation of crumbs to the outside world. And the first thing he is looking for is protection and comfort . In the moments of application to the skin of the baby, it warms the warmth of the mother's body, soothes and comforts her smell and heartbeat, so familiar to him even before birth. Gentle touches and calm breathing, a smile and a soft voice of a mother, a mixture warm as breast milk give the baby everything he needs - safety, warmth and nutrition.
Gentle touches and calm breathing, a smile and a soft voice of a mother, a mixture warm as breast milk give the baby everything he needs - safety, warmth and nutrition.
Love and contact is the most important "ingredient" in any feeding process and infant formula is rich vitamins and nutrients that are good for your baby's health and development will help you feel confident in your ability to care for your baby.
In theory, feeding your baby formula is just a few simple steps. But if you've never made a bottle of baby food or the time is three in the morning, things seem complicated. Be patient to get into the rhythm.
For most mothers, bottle feeding becomes a part of baby food. And this does not depend on whether the bottle contains expressed breast milk or formula. The important thing is that sticking to breastfeeding exclusively can be difficult or impossible over time. Then the mother begins to supplement the baby with a mixture or transfer it to completely artificial feeding.
Below are answers to parents' questions about how to properly and safely bottle feed your baby.
1. How to make a formula bottle
We offer together step by step the process of preparing the first bottle for your baby.
- Hand hygiene : Wash hands thoroughly with soap and warm water before handling bottles and feeding the baby. We also check the cleanliness of the table and measuring spoon.
- Sterilization : bottles and teats should preferably be sterilized beforehand.
- Water preparation : boil bottled baby water and cool to 40 ˚C, determine the right amount of water, then pour it into the bottle up to the desired mark - according to the number of scoops of dry formula according to the weight and age of your child.
- Let's determine the volume of the mixture : on the jar, in the "Feeding table" block, it is indicated how many spoons are required for one feeding.
 The measuring spoon should be full and without a slide - we remove the excess on a special corner of the jar. Both day and night, it is best to look at the feeding chart (unless otherwise determined by your doctor) so as not to accidentally add too much or too little formula. An overly dilute formula or an excess of it can interfere with a child's proper nutrition.
The measuring spoon should be full and without a slide - we remove the excess on a special corner of the jar. Both day and night, it is best to look at the feeding chart (unless otherwise determined by your doctor) so as not to accidentally add too much or too little formula. An overly dilute formula or an excess of it can interfere with a child's proper nutrition. - Mixing according to instructions : Pour the required amount of product without a slide into a bottle of prepared water. Next, close the bottle with a lid and roll between the palms. If the bottle is shaken, a lot of foam may form.
- Checking the temperature of prepared meals : put a drop of the mixture on the inside of the wrist, where the skin is as sensitive as in a baby's mouth. Immediately after preparing the mixture, tightly close the jar of baby food and feed the baby.
- Let dad give a bottle of and be alone with the baby - they also need communication and time to make friends.
 The reality is that many dads feel left out while breastfeeding, but this can be avoided with formula feeding. Show how to hold your baby and bottle, support your partner during the first feedings . This help will be useful for you too. An extra pair of hands when bottle feeding gives mom a little more precious time.
The reality is that many dads feel left out while breastfeeding, but this can be avoided with formula feeding. Show how to hold your baby and bottle, support your partner during the first feedings . This help will be useful for you too. An extra pair of hands when bottle feeding gives mom a little more precious time.
2. What water to use for infant formula
Only boiled bottled baby water should be used in the bottle. This is a great way to make sure the water you use is safe for your baby.
All children's water is registered by Rospotrebnadzor in accordance with SanPiN 2.1.4.1116-02. Such water corresponds to the indicators of the highest category, is balanced in terms of mineral composition and is characterized by low total mineralization in the range of 200-500 mg / l (a baby’s body is simply not able to absorb higher concentrations of minerals and salts).
Packaged water may look the same. But some manufacturers divide baby water into two categories - for drinking and for preparing mixtures. The composition of drinking water contains a higher concentration of minerals that are beneficial for the child's body, but they can upset the balance of the nutrient mixture. Therefore, on the labels you can read about the different purposes of water: suitable for preparing baby food or for feeding babies and young children.
The composition of drinking water contains a higher concentration of minerals that are beneficial for the child's body, but they can upset the balance of the nutrient mixture. Therefore, on the labels you can read about the different purposes of water: suitable for preparing baby food or for feeding babies and young children.
It makes no sense to make large stocks of baby water - water in open bottles becomes unusable after 24-48 hours, depending on the manufacturer. Tap or spring water is also not suitable for feeding babies. Such water may contain various impurities, bacteria and microbes that are dangerous for babies. Boiling will “free” water from harmful microorganisms, but not from impurities of heavy metals and chemicals.
3. How to use the measuring spoon correctly
The measuring spoon helps you accurately measure the amount of the mixture and get the correct dosage. Fill a full spoon, but shoot a slide. You don't need a kitchen knife for this - each jar of mixture has a convenient wide corner for removing excess. And in economical jars with a volume of 800 g, for example, in MAMAKO ® Premium with goat milk, the spoon is conveniently attached to the lid - so you don’t have to look for it in a large package before each feeding. Fingers and knives are not absolutely clean, they always have a lot of bacteria that can spoil the mixture and harm the health of the baby. The antibacterial fastening of the spoon and the corner of the jar protect the mixture and the child from harmful bacteria from the external environment.
And in economical jars with a volume of 800 g, for example, in MAMAKO ® Premium with goat milk, the spoon is conveniently attached to the lid - so you don’t have to look for it in a large package before each feeding. Fingers and knives are not absolutely clean, they always have a lot of bacteria that can spoil the mixture and harm the health of the baby. The antibacterial fastening of the spoon and the corner of the jar protect the mixture and the child from harmful bacteria from the external environment.
4. What temperature should the water and ready mix be?
Boiled water should be cooled to 40 °C. This temperature will retain all the benefits of baby food based on goat's milk. The easiest way to get water at the right temperature is to boil it in a kettle and let it cool for 20-30 minutes. A kettle for boiling water requires special care - it is covered with a mineral coating, which is easily removed by boiling citric acid. This is a troublesome procedure, since after cleaning it takes about 3-4 boils to remove traces of detergent. Create a rhythm for preparing dishes - at night or with a crying baby in your arms, there will be no time for this. The finished formula should be warm: 37 ˚C, as this is the temperature of breast milk and it is optimal for the baby's food. Before feeding, do not forget to check if the mixture is too hot by applying a couple of drops on the wrist. If it burns, you can hold the bottle under cold water for a while, after closing the nipple with a lid. If the mixture has cooled slightly, it is enough to heat it under a warm stream of water.
Create a rhythm for preparing dishes - at night or with a crying baby in your arms, there will be no time for this. The finished formula should be warm: 37 ˚C, as this is the temperature of breast milk and it is optimal for the baby's food. Before feeding, do not forget to check if the mixture is too hot by applying a couple of drops on the wrist. If it burns, you can hold the bottle under cold water for a while, after closing the nipple with a lid. If the mixture has cooled slightly, it is enough to heat it under a warm stream of water.
5. Mixed feeding: breast or bottle first
The best feeding schedule is when the mother supplements her baby with formula after breast milk. If the baby is given a bottle first, then he may begin to refuse the breast. This is due to the fact that it is easier to suck through the nipple, and with natural feeding, the baby has to “work” a lot to get mom's milk.
6. How many baby bottles do you need per day
It's all about how old you are on formula, how much formula you give, and how often your baby eats. It's best to keep six to ten bottles on hand so you always have clean dishes. In addition, the more bottles, the less often they will have to be sterilized. Buy 125 ml bottles for an infant, then upgrade to 150 ml and 240 ml as your baby's appetite and needs increase. Don't rush to part with smaller bottles, they are great for supplementing and watering.
It's best to keep six to ten bottles on hand so you always have clean dishes. In addition, the more bottles, the less often they will have to be sterilized. Buy 125 ml bottles for an infant, then upgrade to 150 ml and 240 ml as your baby's appetite and needs increase. Don't rush to part with smaller bottles, they are great for supplementing and watering.
7. Why can't the bottle be held horizontally during feeding
Mom tilts the bottle so that the nipple is always filled with formula. The angle of inclination increases as the bottle empties, so it is important to be close to the baby, not leaving him alone during feeding even for a minute. If you do not tilt the bottle, the child will begin to swallow air. Air bubbles can cause regurgitation during or immediately after feeding. In addition, when air enters the baby’s stomach, he feels full faster, which means he eats less and will be hungry after a short period of time.
8. Which nipple to choose for your baby bottle
Many wide and narrow neck bottles already come with a set of baby nipples. Almost all of them are made of silicone. Which shape of the nipple - anatomical or round - and what size of hole your child will like, can be understood by his reaction during feeding. If the mixture drips from the corners of the mouth, the flow may be too fast due to the large opening. If the baby is sucking hard, the mixture may drip too slowly. We recommend that you do not enlarge the opening of the nipple: it may tear, and the microparticles of the product may enter the child's body. Perhaps the hole is just clogged, this sometimes happens. If necessary, nipples can be replaced and bought separately from the bottles.
Almost all of them are made of silicone. Which shape of the nipple - anatomical or round - and what size of hole your child will like, can be understood by his reaction during feeding. If the mixture drips from the corners of the mouth, the flow may be too fast due to the large opening. If the baby is sucking hard, the mixture may drip too slowly. We recommend that you do not enlarge the opening of the nipple: it may tear, and the microparticles of the product may enter the child's body. Perhaps the hole is just clogged, this sometimes happens. If necessary, nipples can be replaced and bought separately from the bottles.
9. Should baby bottles be sterilized
Yes, to limit the spread of bacteria. Hard-to-reach places of the bottle must be washed from the mixture (a brush and warm water are enough) before sterilization. A sterilizer is ideal for this purpose - ultrasonic, electric or steam for a microwave oven. It can sterilize all baby accessories - bottles, nipples, caps, brushes. Of course, you can replace the sterilizer with a simple boil, but be careful that the water does not boil away, otherwise the bottles and nipples will be damaged and become dangerous.
Of course, you can replace the sterilizer with a simple boil, but be careful that the water does not boil away, otherwise the bottles and nipples will be damaged and become dangerous.
10. Can I use the microwave to heat formula
Resist the temptation to microwave the formula and save time. Microwave ovens heat liquids unevenly. Even if the bottle is not hot, the mixture can warm up quite strongly: there is a risk of burning the baby. In addition, heating in the microwave can break down the nutrients in the formula.
11. Can leftover formula be stored
If your child has not finished formula, discard any leftover formula. No need to heat up and reuse it. It's not safe for the baby. After a while, bacteria begin to multiply in the finished mixture. Dilute a fresh batch of formula every time the baby is hungry.
12. How to prepare a bottle while traveling
If you are away from home or on the road for several hours, you can take two bottles of warm boiled water in a thermal bag that keeps you warm. Before each feeding, it remains to pour the right amount of mixture into the bottle (it is convenient to measure portions in advance according to the number of feedings in the infant formula dispenser). If the water in the bottle is cold, it is enough to warm it under warm water (this will take a little time). Bottles and teats should last until the next opportunity to wash and sterilize them. Remember that a thermal bag is good for maintaining the temperature of boiled water, but it cannot be used to store the finished mixture - this is harmful to the baby's health.
Before each feeding, it remains to pour the right amount of mixture into the bottle (it is convenient to measure portions in advance according to the number of feedings in the infant formula dispenser). If the water in the bottle is cold, it is enough to warm it under warm water (this will take a little time). Bottles and teats should last until the next opportunity to wash and sterilize them. Remember that a thermal bag is good for maintaining the temperature of boiled water, but it cannot be used to store the finished mixture - this is harmful to the baby's health.
MAMAKO ® fully supports breastfeeding, but since this is not always possible, we have shown you how to bottle feed with love. In addition, the preparation of baby food will become a conscious and important matter. Very little time will pass, and you will fondly remember these precious moments of tender age, and feeding time will be the beginning of a warm, close connection with the baby.
* Breast milk is the best food for babies.