Breast feeding new born babies
Breastfeeding FAQs: How Much and How Often (for Parents)
Breastfeeding is a natural thing to do, but it still comes with its fair share of questions. Here's what you need to know about how often and how long to breastfeed your baby.
How Often Should I Breastfeed?
Newborn babies should breastfeed 8–12 times per day for about the first month. Breast milk is easily digested, so newborns are hungry often. Frequent feedings helps stimulate your milk production during the first few weeks.
By the time your baby is 1–2 months old, he or she probably will nurse 7–9 times a day.
In the first few weeks of life, breastfeeding should be "on demand" (when your baby is hungry), which is about every 1-1/2 to 3 hours. As newborns get older, they'll nurse less often, and may have a more predictable schedule. Some might feed every 90 minutes, whereas others might go 2–3 hours between feedings.
Newborns should not go more than about 4 hours without feeding, even overnight.
How Do I Count the Time Between Feedings?
Count the length of time between feedings from the time your baby begins to nurse (rather than at the end) to when your little one starts nursing again. In other words, when your doctor asks how often your baby is feeding, you can say "about every 2 hours" if your first feeding started at 6 a.m., the next feeding was around 8 a.m., then 10 a.m., and so on.
Especially at first, you might feel like you're nursing around the clock, which is normal. Soon enough, your baby will go longer between feedings.
How Long Does Nursing Take?
Newborns may nurse for up to 20 minutes or longer on one or both breasts. As babies get older and more skilled at breastfeeding, they may take about 5–10 minutes on each side.
How long it takes to breastfeed depends on you, your baby, and other things, such as whether:
- your milk supply has come in (this usually happens 2–5 days after birth)
- your let-down reflex (which causes milk to flow from the nipple) happens right away or after a few minutes into a feeding
- your milk flow is slow or fast
- the baby has a good latch, taking in as much as possible of your areola (the dark circle of skin around your nipple)
- your baby begins gulping right away or takes it slow
- your baby is sleepy or distracted
Call your doctor if you're worried that your baby's feedings seem too short or too long.
When Should I Alternate Breasts?
Alternate breasts and try to give each one the same amount of nursing time throughout the day. This helps to keep up your milk supply in both breasts and prevents painful engorgement (when your breasts overfill with milk).
You may switch breasts in the middle of each feeding and then alternate which breast you offer first for each feeding. Can't remember where your baby last nursed? It can help to attach a reminder — like a safety pin or small ribbon — to your bra strap so you'll know which breast your baby last nursed on. Then, start with that breast at the next feeding. Or, keep a notebook handy or use a breastfeeding app to keep track of how your baby feeds.
Your baby may like switching breasts at each feeding or prefer to nurse just on one side. If so, then offer the other breast at the next feeding. Do whatever works best and is the most comfortable for you and your baby.
How Often Should I Burp My Baby During Feedings?
After your baby finishes on one side, try burping before switching breasts. Sometimes, the movement alone can be enough to cause a baby to burp.
Sometimes, the movement alone can be enough to cause a baby to burp.
Some infants need more burping, others less, and it can vary from feeding to feeding.
If your baby spits up a lot, try burping more often. While it's normal for infants to "spit up" a small amount after eating or during burping, a baby should not vomit after feeding. If your baby throws up all or most of a feeding, there could be a problem that needs medical care. If you're worried that your baby is spitting up too much, call your doctor.
Why Is My Baby Hungrier Than Usual?
When babies go through a period of rapid growth (called a growth spurt), they want to eat more than usual. These can happen at any time. But in the early months, growth spurts often happen when a baby is:
- 7–14 days old
- 2 months old
- 4 months old
- 6 months old
During these times and whenever your baby seems extra hungry, follow your little one's hunger cues. You may need to breastfeed more often for a while.
How Long Should I Breastfeed My Baby?
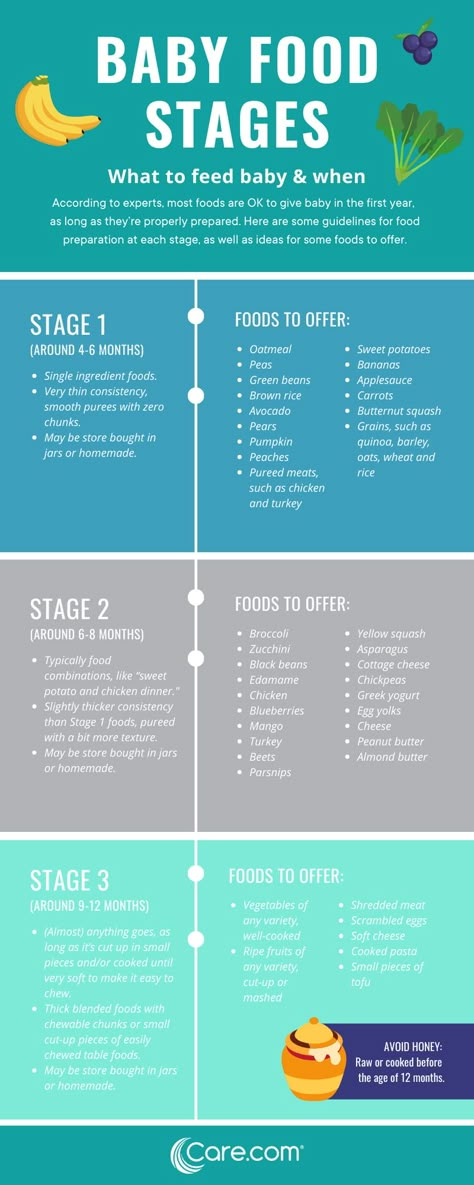
That's a personal choice. Experts recommend that babies be breastfed exclusively (without formula, water, juice, non–breast milk, or food) for the first 6 months. Then, breastfeeding can continue until 12 months (and beyond) if it's working for you and your baby.
Breastfeeding has many benefits for mom and baby both. Studies show that breastfeeding can lessen a baby's chances of diarrhea, ear infections, and bacterial meningitis, or make symptoms less severe. Breastfeeding also may protect children from sudden infant death syndrome (SIDS), diabetes, obesity, and asthma.
For moms, breastfeeding burns calories and helps shrink the uterus. In fact, breastfeeding moms might return to their pre–pregnancy shape and weight quicker. Breastfeeding also helps lower a woman's risk of diseases like:
- breast cancer
- high blood pressure
- diabetes
- heart disease
It also might help protect moms from uterine cancer and ovarian cancer.
Feeding Your Newborn (for Parents)
How you feed your newborn is the first nutrition decision you make for your child. These guidelines on breastfeeding and bottle feeding can help you know what's right for you and your baby.
Breast or Bottle?
The American Academy of Pediatrics (AAP) recommends that babies be breastfed exclusively for about the first 6 months. After they start on solid foods, babies should breastfeed through the first year of life and even beyond, if desired.
But breastfeeding isn't possible or preferable for all new moms. Deciding to breastfeed or bottle feed a baby is usually based on the mother's comfort level with breastfeeding and her lifestyle. In some cases, breastfeeding may not be recommended for a mom and her baby. If you have any questions about whether to breastfeed or formula feed, talk to your pediatrician.
Remember, your baby's nutritional and emotional needs will be met whether you choose to breastfeed or formula feed.
Benefits of Breastfeeding
Breastfeeding your newborn has many benefits. Perhaps most important, breast milk is the perfect food for a baby's digestive system. It has the nutrients that a newborn needs, and it’s easily digested. Commercial formulas try to imitate breast milk, and come close, but can't match it exactly.
Breast milk has
antibodiesthat help protect babies from many infections, including diarrhea and ear and lung infections. Breastfed babies are less likely to develop medical problems such as diabetes, high cholesterol, asthma, and allergies. Breastfeeding also might make a child less likely to become overweight.
Breastfeeding is great for moms too. It burns calories, so can help nursing moms lose the weight gained during pregnancy. Breastfeeding also may offer protection from breast cancer and ovarian cancer.
Some moms find breastfeeding easier and quicker than formula feeding — it needs no preparation, and you don't run out of breast milk in the middle of the night. Also, breastfeeding costs little. Nursing mothers do need to eat more and may want to buy nursing bras and pads, a breast pump, or other equipment. But these expenses are generally less than the cost of formula.
Also, breastfeeding costs little. Nursing mothers do need to eat more and may want to buy nursing bras and pads, a breast pump, or other equipment. But these expenses are generally less than the cost of formula.
Breastfeeding meets a variety of emotional needs for both moms and babies. The skin-to-skin contact can enhance the emotional connection, and providing complete nourishment can help new moms feel confident in their ability to care for their newborn.
Limitations of Breastfeeding
With all the good things known about breastfeeding, why doesn't every mother choose to breastfeed?
Breastfeeding requires a big commitment from a mother. Some new moms feel tied down by the demands of a nursing newborn. Because breast milk is easily digested, breastfed babies tend to eat more often than babies who are fed formula. This means moms can be in demand as often as every 2 or 3 hours in the first few weeks. This can be tiring, but it's not long before babies feed less often and sleep longer at night.
Some new mothers need to get back to work outside the home or separate from their babies from time to time for other reasons. Some opt for formula feeding so other caregivers can give the baby a bottle. Mothers who want to continue breastfeeding can use a breast pump to collect breast milk to be given in a bottle, so their babies still get its benefits even when mom isn't there to breastfeed.
Fathers and other family members may want to share in feeding the baby. When mom is breastfeeding, dad or siblings may want to stay close by. Helping mom get comfortable, or providing a burp cloth when needed, will let them be part of the experience.
When breastfeeding is going well, other family members can help by giving the baby pumped breast milk in a bottle when mom needs a break.
Some moms may feel embarrassed or worried about breastfeeding. These feelings usually end after a successful breastfeeding process is set. It can help to get advice from those who've gone through the experience. Most hospitals and birthing centers offer in-depth instruction on breastfeeding to new moms. Your pediatrician, nurse practitioner, or nurse can answer questions or put you in touch with a lactation consultant or a breastfeeding support group.
Most hospitals and birthing centers offer in-depth instruction on breastfeeding to new moms. Your pediatrician, nurse practitioner, or nurse can answer questions or put you in touch with a lactation consultant or a breastfeeding support group.
In some cases, a mother's health may affect her ability to breastfeed. Moms getting chemotherapy for cancer and those who have HIV should not breastfeed, for example.
If you have a medical condition or take any medicines regularly, talk with your doctor about whether it's OK to breastfeed. If you have to stop nursing temporarily, continue to pump breast milk to maintain milk production. If you or your baby are sick, continue to breastfeed if you can. Talk to the doctor if you have any concerns.
In some situations, it may not possible to breastfeed, such as when a baby is very sick or born early. Mothers should talk with their baby's doctor about expressing and storing milk. Often, a baby who can't breastfeed can get breast milk through a feeding tube or bottle.
Some moms who have inverted nipples may have trouble breastfeeding, but a lactation consultant usually can help them overcome this. Likewise, women who have had plastic surgery on their breasts should be able to successfully breastfeed. Talk with your doctor if you have any concerns.
Hold off on pacifiers or bottles until your baby has gotten used to and is good at breastfeeding. Lactation professionals recommend waiting until a baby is about 3–4 weeks old before offering artificial nipples of any kind (including pacifiers).
Benefits of Formula Feeding
Commercially prepared infant formula is a nutritious alternative to breast milk. Bottle feeding can offer more freedom and flexibility for moms, and make it easier to know how much the baby is getting.
Because babies digest formula more slowly than breast milk, a baby who is getting formula may need fewer feedings than one who breastfeeds. Formula feeding also can make it easier to feed the baby in public, and lets the father and other family members help feed the baby, which can enhance bonding.
Limitations of Formula Feeding
Just as breastfeeding has its unique demands, so does bottle feeding. Bottle feeding takes organization and preparation, especially if you want to take your baby out. Store-bought formula can be pretty expensive, but do not try to make your own formula at home.
It's important to make sure that you have enough formula on hand, and bottles that are clean and ready to be used.
Here are a few guidelines for formula feeding:
- Carefully follow directions on the label when preparing formula. Do not add more water than directed.
- Bottles left out of the refrigerator longer than 1 hour and any formula left in the bottle that a baby doesn't finish should be discarded.
- Prepared bottles of formula can be stored in the refrigerator up to 24 hours and carefully warmed just before feeding. You don't have to warm formula, but most babies prefer it.
- A bottle of formula can be warmed by holding it in running warm water or setting it in a pan of warm water.
 A bottle of formula (or breast milk) should never be warmed in a microwave. The bottle can heat unevenly and leave "hot spots" that can burn a baby's mouth.
A bottle of formula (or breast milk) should never be warmed in a microwave. The bottle can heat unevenly and leave "hot spots" that can burn a baby's mouth.
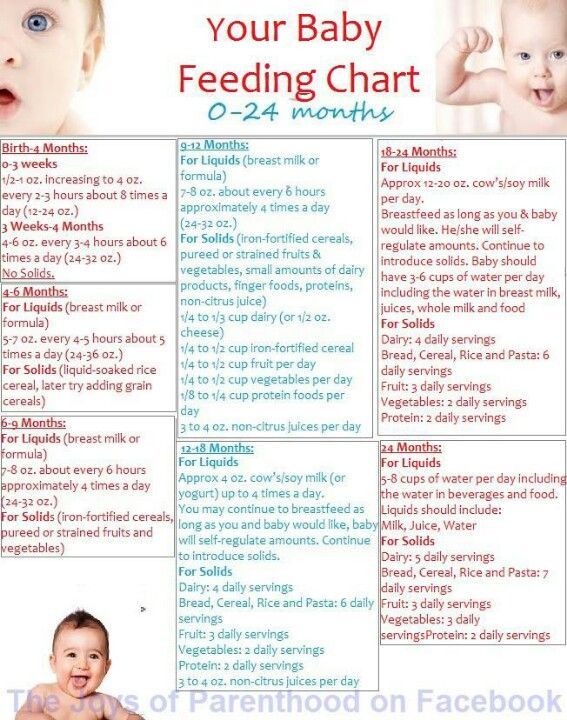
How Often Do Newborns Eat?
Your newborn will nurse about 8 to 12 times per day during the first weeks of life. In the beginning, mothers may want to try nursing 10–15 minutes on each breast, then adjust the time as needed.
Breastfeeding should be on demand (when your baby is hungry), which is generally every 1–3 hours. As newborns get older, they'll nurse less often and have longer stretches between feedings. Newborn babies who are getting formula will likely take about 2–3 ounces every 2–4 hours. Newborns should not go more than about 4–5 hours without feeding.
Signs that babies are hungry include:
- moving their heads from side to side
- opening their mouths
- sticking out their tongues
- placing their hands and fists to their mouths
- puckering their lips as if to suck
- nuzzling against their mothers' breasts
- crying
A feeding schedule is not necessary — you and your baby will get into a routine. Babies know (and will let their parents know) when they're hungry and when they've had enough. Watch for signs that your baby is full (slowing down, spitting out the bottle or unlatching from breast, closing the mouth, turning away from the breast or bottle) and stop the feeding when these signs appear.
Babies know (and will let their parents know) when they're hungry and when they've had enough. Watch for signs that your baby is full (slowing down, spitting out the bottle or unlatching from breast, closing the mouth, turning away from the breast or bottle) and stop the feeding when these signs appear.
As babies grow, they begin to eat more at each feeding and can go longer between feedings. There may be other times when your infant seems hungrier than usual. Continue to nurse or feed on demand. Nursing mothers need not worry — breastfeeding stimulates milk production, and your supply of breast milk will adjust to your baby's demand for it.
Is My Newborn Getting Enough to Eat?
New parents often worry about whether their babies are getting enough to eat.
Babies are getting enough to eat if they:
- seem satisfied
- have about 6–8 wet diapers a day
- have regular bowel movements (poops)
- sleep well
- are alert when awake
- are gaining weight
A baby who is fussing, crying, seems hungry, does not appear satisfied after feeding, and has fewer wet diapers may not be getting enough to eat. If you're concerned that your baby isn't getting enough to eat, call your doctor.
If you're concerned that your baby isn't getting enough to eat, call your doctor.
Most infants "spit up" a small amount after eating or during burping, but a baby should not vomit after feeding. Vomiting after every feeding might be a sign of an allergy, digestive problem, or other problem that needs medical care. If you have concerns that your baby is spitting up too much, call your doctor.
Should Newborns Get Nutritional Supplements?
Breast milk has the right combination of vitamins and easily absorbed iron for newborns. A healthy infant being nursed by a healthy mother doesn't need extra vitamins or nutritional supplements, with the exception of vitamin D. Breastfed babies should begin vitamin D supplements within the first few days of life, continuing until they get enough vitamin D-fortified formula or milk (after 1 year of age).
Breastfeeding mothers who follow vegetarian diets that do not include animal products need vitamin B12 supplements.
Iron-fortified formula has the right blend of vitamins and minerals for a baby, so supplements usually aren't needed. Infants drinking less than 1 liter, or about a quart, of formula a day may need a vitamin D supplement.
Infants drinking less than 1 liter, or about a quart, of formula a day may need a vitamin D supplement.
Water, juice, and other foods usually aren't necessary during a baby's first 6 months. Breast milk and formula provide everything babies need nutritionally until they start eating solid foods. Talk to your doctor if you have any questions about feeding your newborn.
Reviewed by: Mary L. Gavin, MD
Date reviewed: February 2021
Breastfeeding a newborn | What to Expect in the First Week
The first week of a baby's life is a wonderful but hectic time, especially if you haven't breastfed before. Our breastfeeding tips will help you settle in as quickly as possible
Share this information
The first time after childbirth, mothers are often confused. The body is still recovering, and you are already starting to get to know your newborn baby. The emotional state during this period can be unstable, especially between the second and fifth day, when many women have milk 1 and at the same time postpartum depression begins 2 . In addition, people around often expect (and demand) that a woman come to her senses as soon as possible and become a “super mom”. But the best thing to do this first week is just to be with your baby and get breastfeeding going.
In addition, people around often expect (and demand) that a woman come to her senses as soon as possible and become a “super mom”. But the best thing to do this first week is just to be with your baby and get breastfeeding going.
When should I start breastfeeding my newborn?
Try to breastfeed your baby within the first hour after birth. When the baby latch onto the breast and begins sucking rhythmically, it stimulates the mammary gland cells and starts milk production. 1 It is not for nothing that this time is called the “magic hour”!
“Ideally, the baby should be placed on the mother's stomach immediately after birth so that it can immediately attach to the breast. He won't necessarily eat, but he should be able to,” explains Cathy Garbin, an internationally recognized expert on breastfeeding.
“Hold your baby and let him find the breast on his own and put the nipple in his mouth. This is called the breast-seeking reflex. On the Internet you can watch videos that show what this process looks like. If the baby does not latch onto the nipple on its own, the midwife will help to properly attach it to the breast. But for starters, it’s good to give the baby the opportunity to do it on their own. In this case, the optimal position for the mother is reclining. ”
If the baby does not latch onto the nipple on its own, the midwife will help to properly attach it to the breast. But for starters, it’s good to give the baby the opportunity to do it on their own. In this case, the optimal position for the mother is reclining. ”
Don't spend that special first hour of your baby's life weighing and swaddling—or at least wait until he's suckling for the first time. Enjoy hugs and close skin-to-skin contact. This promotes the production of oxytocin, the hormone of love, in you and your baby, and oxytocin plays a key role in the supply of the first breast milk - colostrum. 3
“As soon as the obstetricians were convinced that our son was healthy, the three of us — me, my husband and our baby — were left to give us the opportunity to get to know each other. It was a very special hour - an hour of awkwardness, turbulent emotions and bliss. During this time, I breastfed my son twice, ”recalls Ellie, a mother of two from the UK.
Did you know that breastfeeding helps to recover after childbirth? This is because oxytocin stimulates uterine contractions.![]() In the first hours after childbirth, this contributes to the natural release of the placenta and reduces blood loss. 4
In the first hours after childbirth, this contributes to the natural release of the placenta and reduces blood loss. 4
What if the birth did not go according to plan?
If you had a cesarean section or other complications during childbirth,
You can still make skin-to-skin contact with your baby and breastfeed him in the first hours after birth.
“If you can't hold your baby, have your partner do it for you and make skin-to-skin contact with the baby. This will give the baby a sense of security, care and warmth so that he can hold on until you recover, ”Katie advises.
If the baby is unable to breastfeed, it is advisable to start expressing milk as early as possible and do so as often as possible until the baby is able to feed on its own. “While breastfeeding in the first hours after birth lays an excellent foundation for the future, it is not so important,” Cathy reassures. “It is much more important to start lactation so that in the future, if necessary, you can start breastfeeding. ”
”
To start milk production, you can express milk manually or use a breast pump that can be given to you at the hospital. 5 And with expressed precious colostrum, it will be possible to feed the child. This is especially important if the baby was born premature or weak, since breast milk is extremely healthy.
If a baby was born prematurely or has a medical condition and cannot be breastfed immediately, this is no reason not to continue breastfeeding. “I have worked with many new mothers who were unable to breastfeed their baby for the first six weeks due to preterm labor or other reasons. Nevertheless, all of them later successfully switched to breastfeeding,” says Kathy.
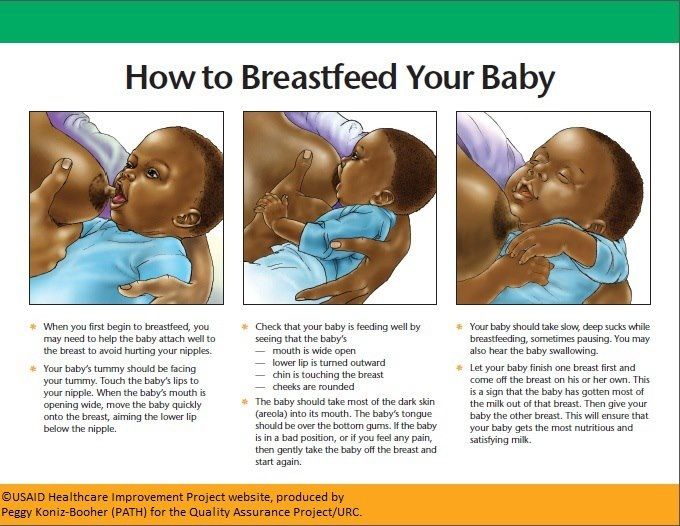
Does the baby latch on correctly?
Correct breastfeeding is essential for successful breastfeeding 6 , as it determines how effectively the baby will suckle milk and hence grow and develop. Latching on the breast incorrectly can cause sore or damaged nipples, so don't hesitate to ask your doctor to check that your baby is properly attached to the breast, even if you are told that everything is fine and you do not see obvious problems - especially while you are in the hospital.
“While I was in the hospital, I called the doctor at every feed and asked me to check if I was breastfeeding correctly,” says Emma, mother of two from Australia. - There were several cases when it seemed to me that everything seemed to be right, but it was painful to feed, and the doctor helped me take the baby off the breast and attach it correctly. By the time I was discharged, I had already learned to do it confidently.”
When applying to the breast, point the nipple towards the palate. This will allow the baby to take the nipple and part of the areola under it into their mouth. It will be easier for him to suck if he has both the nipple and part of the areola around in his mouth. 6
“When a baby latch on properly, it doesn't cause discomfort and it causes a pulling sensation, not pain,” Cathy explains. - The baby's mouth is wide open, the lower lip may be slightly turned outward, and the upper one lies comfortably on the chest. The body language of the child indicates that he is comfortable.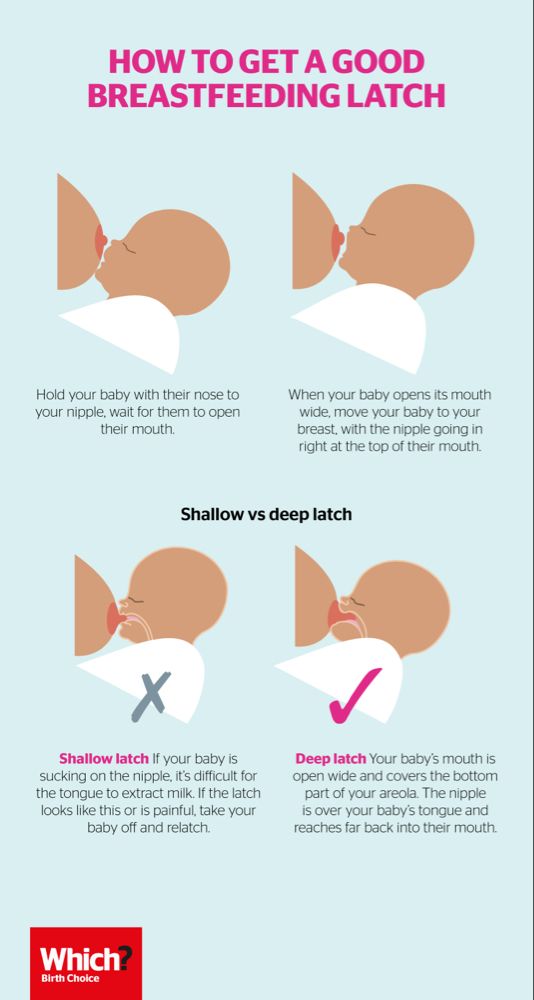 There isn't much milk at this early stage, so you probably won't notice your baby swallowing, but he will suckle a lot and nurse frequently."
There isn't much milk at this early stage, so you probably won't notice your baby swallowing, but he will suckle a lot and nurse frequently."
How often should a newborn be fed?
The frequency and duration of breastfeeding in the first week can vary greatly. “The first 24 hours of life are completely different for different children. Someone sleeps a lot (after all, childbirth is tiring!), And someone often eats, says Katie. - Such a variety greatly confuses young mothers. Everyone gives different advice, so it's important to remember that every mother and child is different."
“Colostrum is thicker than mature breast milk and is produced in smaller amounts, but has many benefits. When the baby eats colostrum, he learns to suck, swallow and breathe until milk begins to flow in more volume, ”explains Cathy.
Milk usually arrives on the second or fourth day after delivery. Until this time, the baby is applied to the breast 8-12 times a day (and sometimes more often!), including at night. 7 Feeding may last 10-15 minutes at this stage, or 45 minutes or even an hour, as the baby is just beginning to develop the muscles and coordination needed to suckle effectively.
7 Feeding may last 10-15 minutes at this stage, or 45 minutes or even an hour, as the baby is just beginning to develop the muscles and coordination needed to suckle effectively.
“At first, the intensity of feeding is very high, often higher than many people realize, and this is shocking to most new mothers,” says Cathy. - Sometimes mom has no time to go to the toilet, take a shower and have a snack. It usually comes as a surprise."
Camille, a mother from Australia, experienced this. “The first week, Frankie ate every two hours, day and night, and each time it took half an hour to an hour to feed,” she recalls. “My husband and I were completely exhausted!”
Do I need to feed my newborn on a schedule?
The good news is that frequent feeding promotes lactation and stimulates milk production. 7 The more your baby eats, the more milk you will have. Therefore, forget about feeding your newborn on a schedule - this way he will have less chance of feeding. Try to feed your baby when he signals that he is hungry 8 :
Try to feed your baby when he signals that he is hungry 8 :
- tossing and turning in her sleep;
- opens eyes;
- turns his head if he feels a touch on his cheek;
- sticks out tongue;
- groans;
- licks lips;
- sucks fingers;
- is naughty;
- whimpers;
- is crying.
Crying is the last sign of hunger, so when in doubt, just offer your baby the breast. If he bursts into tears, it will be more difficult to feed him, especially at first, when both of you are just learning how to do it. As your baby grows, he will likely eat less frequently and take less time to feed, so breastfeeding will seem more predictable.
Does breastfeeding hurt?
You may have heard that breastfeeding is not painful at all, but in fact, in the first days, many new mothers experience discomfort. And this is not at all surprising, given that the nipples are not used to such frequent and strong sucking.
“Breastfeeding can be uncomfortable for the first couple of days – your body and your baby are just getting used to it. If a baby eats for too long and does not latch well, the sensations are almost the same as from unworn new shoes, Cathy compares. Just as tight shoes can rub your feet, improper suckling can damage your nipples. Prevention is always better than cure, so if the pain persists after a few days of feeding, contact a lactation consultant or healthcare professional.”
Maria, a mother from Canada, agrees: “Although my son seemed to latch onto the breast well, he damaged his nipples while feeding, and I was in pain. As it turned out, the reason was a shortened frenulum of the tongue. The breastfeeding specialists at our city clinic have been of great help in diagnosis and treatment.”
In addition, you may experience period cramps during the first few days after breastfeeding, especially if this is not your first baby. This is the so-called postpartum pain. The fact is that oxytocin, which is released during breastfeeding, contributes to further contraction of the uterus to restore its normal size. 4
The fact is that oxytocin, which is released during breastfeeding, contributes to further contraction of the uterus to restore its normal size. 4
When milk arrives, the breasts usually become fuller, firmer and larger than before delivery. In some women, the breasts swell, harden and become very sensitive - swelling of the mammary glands occurs. 10 Frequent breastfeeding relieves these symptoms. For more breast care tips, read our article What is Breast Swelling?
How often does the newborn urinate and defecate?
What goes into the body must go back out. Colostrum
has a laxative effect, helping to eliminate meconium - the original feces. It looks a little scary - black and sticky, like tar. 11 But don't worry, it won't always be like this. Breastfed babies usually have a slightly sweet smell of stool.
How many times a day you will need to change diapers and how the contents should look like, see below.
Day one
- Frequency: once or more.

- Colour: greenish black.
- Texture: sticky like tar.
Day two
- Frequency: twice or more.
- Colour: dark greenish brown.
- Texture: less sticky.
Day three
- Frequency: twice or more.
- Colour: greenish brown to brownish yellow.
- Texture: non-sticky.
Fourth day and then the entire first month
- Frequency: twice or more.
- Color: yellow (feces should turn yellow no later than by the end of the fourth day).
- Texture: grainy (like mustard with grains interspersed). Leaky and watery.
The baby's urine should be light yellow. On average, babies urinate once a day for the first two days. Starting around the third day, the number of wet diapers increases to three, and from the fifth day onwards, diapers have to be changed five times a day or more often. In addition, during the first few days, the weight of wet diapers increases. 11
11
Is the baby getting enough breast milk?
Since very little milk is produced at first,
You may feel that this is not enough for your baby. But if you feed your baby on demand, you will produce exactly as much milk as he needs. If you want to keep the process under control, be guided by the frequency of diaper changes above. If your baby soils less diapers, check with your doctor.
“For the first three or four weeks, most babies just eat and sleep. If the child is worried and constantly asks for a breast, you should consult with your doctor, ”Katie recommends.
Sometimes the baby may vomit after feeding. If the vomit is the color of milk, this is not a cause for concern. But if there are orange, red, green, brown or black blotches in it, or the child vomits with a "fountain", consult a doctor. You should also consult a doctor if the baby has a high temperature, the fontanel (soft spot on the head) has sunk, blood is found in the stool, and also if the weight recorded at birth has not recovered within two weeks. 11
11
But if there are no frightening symptoms and the baby is growing at a normal pace, it means that he has enough milk. Soon you will both get used to breastfeeding and establish a more stable routine.
For the next step in breastfeeding, see Breastfeeding in the First Month: What to Expect.
Literature
1 Pang WW, Hartmann PE. Initiation of human lactation: secretory differentiation and secretory activation. J Mammary Gland Biol Neoplasia 2007;12(4):211-221. - Pang, W.W., Hartmann, P.I., "Lactation initiation in the lactating mother: secretory differentiation and secretory activation." G Mammary Gland Biol Neoplasia. 2007;12(4):211-221.
2 Shashi R et al. Postpartum psychiatric disorders: Early diagnosis and management. Indian J Psychiatry . 2015; 57( Suppl 2): S 216– S 221. - Shashi R. et al., Postnatal mental disorders: early diagnosis and treatment. Indian J Saikiatri. 2015; 57(App 2):S216-S221.
2015; 57( Suppl 2): S 216– S 221. - Shashi R. et al., Postnatal mental disorders: early diagnosis and treatment. Indian J Saikiatri. 2015; 57(App 2):S216-S221.
3 Moberg KU, Prime DK. Oxytocin effects in mothers and infants during breastfeeding. Infant . 2013;9(6):201-206. - Moberg K, Prime DK, "The effects of oxytocin on mother and child during breastfeeding." Infant. 2013;9(6):201-206.
4 Sobhy SI, Mohame NA. The effect of early initiation of breast feeding on the amount of vaginal blood loss during the fourth stage of labor. J Egypt Public Health Assoc . 2004;79(1-2):1-12. - Sobhi SI, Moham NA, "Early initiation of breastfeeding and its effect on vaginal bleeding in the fourth stage of labor." G Egypt Public Health Assoc.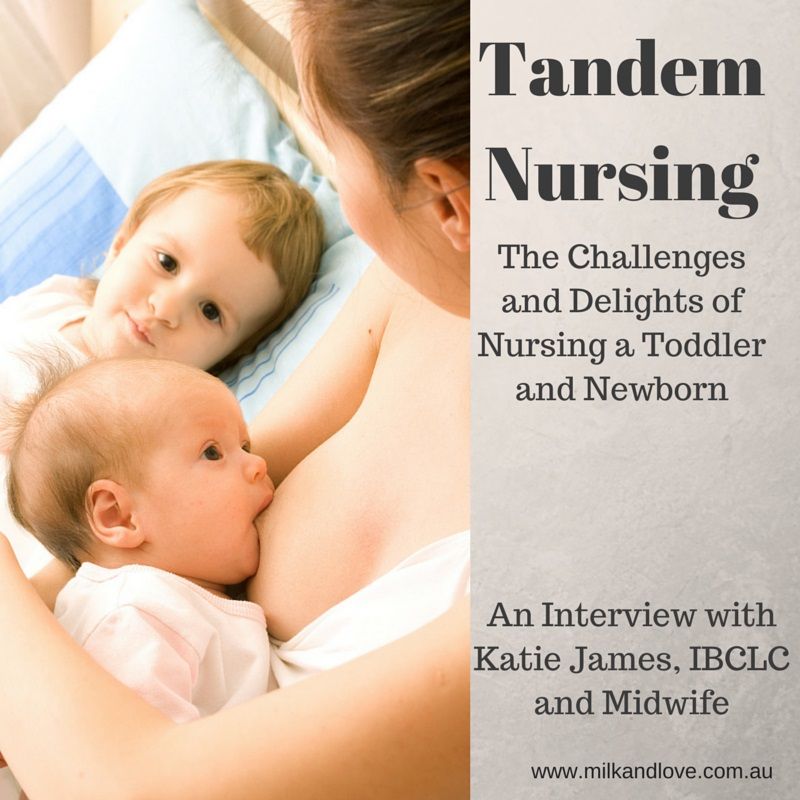 2004;79(1-2):1-2.
2004;79(1-2):1-2.
5 Meier PP et al. Which breast pump for which mother: an evidence-based approach to individualizing breast pump technology. J Perinatol . 2016;36(7):493. - Meyer P.P. et al., Breastpump Selection: A Scientific Approach to Customizing Pumping Technology. J Perinatol (Journal of Perinatology). 2016;36(7):493-499.
6 Cadwell K. Latching - On and Suckling of the Healthy Term Neonate: Breastfeeding Assessment. J Midwifery & Women ’ s 2007;52(6):638-642. — Cadwell, K., "Latching and sucking in healthy newborns: evaluation of breastfeeding." W Midwifery Women Health. 2007;52(6):638-642.
7 Kent JC et al. Principles for maintaining or increasing breast milk production. 2012;41(1):114-121. - Kent J.S. et al. , "Principles for Maintaining and Increasing Milk Production". J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
, "Principles for Maintaining and Increasing Milk Production". J Obstet Ginecol Neoneutal Nurs. 2012;41(1):114-121.
8 Australian Breastfeeding Association [ Internet ]. Feeding cues ; 2017 Sep [ cited 2018 Feb ]. - Australian Breastfeeding Association [Internet], Feed Ready Signals; September 2017 [cited February 2018]
9 Jacobs A et al. S3-guidelines for the treatment of inflammatory breast disease during the lactation period. Geburtshilfe Frauenheilkd . 2013;73(12):1202-1208. - Jacobs A. et al., "Guidelines S -3 for the management of inflammatory breast disease during breastfeeding." Geburtskhilfe und Frauenheilkünde. 2013;73(12):1202-1208.
10 Lawrence RA, Lawrence RM. Breastfeeding: A guide for the medical profession. 7th ed. Maryland Heights MO, USA: Elsevier Mosby; 2010. 1128 p . - Lawrence R.A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." Seventh edition. Publisher Maryland Heights , Missouri, USA: Elsevier Mosby; 2010. P. 1128.
Breastfeeding: A guide for the medical profession. 7th ed. Maryland Heights MO, USA: Elsevier Mosby; 2010. 1128 p . - Lawrence R.A., Lawrence R.M., "Breastfeeding: A guide for healthcare professionals." Seventh edition. Publisher Maryland Heights , Missouri, USA: Elsevier Mosby; 2010. P. 1128.
Breastfeeding newborns | Medela
Nommsen-Rivers, L.A., Chantry, C.J., Peerson, J.M., Cohen, R.J. & Dewey, K.G. Delayed onset of lactogenesis among first-time mothers is related to maternal obesity and factors associated with ineffective breastfeeding. Am J Clin . Nutr 92, 574–584 (2010). - Nommsen-Rivers L.A., Chantry S.J., Pearson J.M., Cohen R.J., Dewey C.J., "Delayed onset of lactogenesis in primiparous mothers is associated with obesity and factors associated with ineffective breastfeeding." Am J Klin Nutr 92, 574–584 (2010).
Berra, S. et al. Correlates of breastfeeding duration in an urban cohort from Argentina. Acta Paediatr . 92, 952–957 (2003). - Berra S. et al., Correlates of duration of breastfeeding among Argentine urban women. Akta Pediatr. 92, 952–957 (2003).
American Academy of Pediatrics and The American College of Obstetricians and Gynecologists. Breastfeeding Handbook for Physicians 2006). - American Academy of Pediatrics and American College of Obstetrics and Gynecology. The Doctor's Guide to Breastfeeding, 2006.
Murray, E.K., Ricketts, S. & Dellaport, J. Hospital practices that increase breastfeeding duration: results from a population-based study. Birth 34, 202–211 (2007). - Murray, I.K., Ricketts, S., and Dellaport, J., "Hospital practices that increase breastfeeding duration: Findings from a population-based study.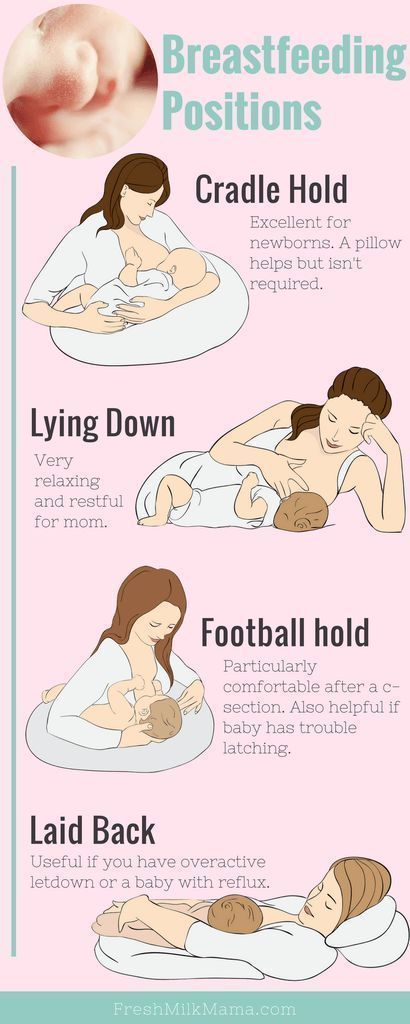 " Bers 34, 202-211 (2007).
" Bers 34, 202-211 (2007).
Chen, D.C., Nommsen-Rivers, L., Dewey, K.G. & Lonnerdal, B. Stress during labor and delivery and early lactation performance. Am . J . Clin . Nutr . 68, 335–344 (1998). — Chen D.S., Nommsen-Rivers L., Dewey K.G. and Lonnerdahl B., "Stress during childbirth and early onset of lactation." Am J Klin Nutr 68, 335–344 (1998).
Hill, P.D., Aldag, J.C., Chatterton, R.T., Zinaman, M. Comparison of Milk Output Between Mothers of Preterm and Term Infants: The First 6 Weeks After Birth. J Hum Lact 2005, 21(1): 22-30. - Hill P.D., Aldag J.S., Chatterton R.T., Zinaman M., "Comparison of the amount of milk in mothers of full-term and premature babies in the first 6 weeks after birth." J Hum Lakt (Journal of the International Association of Lactation Consultants) 2005, 21(1): 22-30.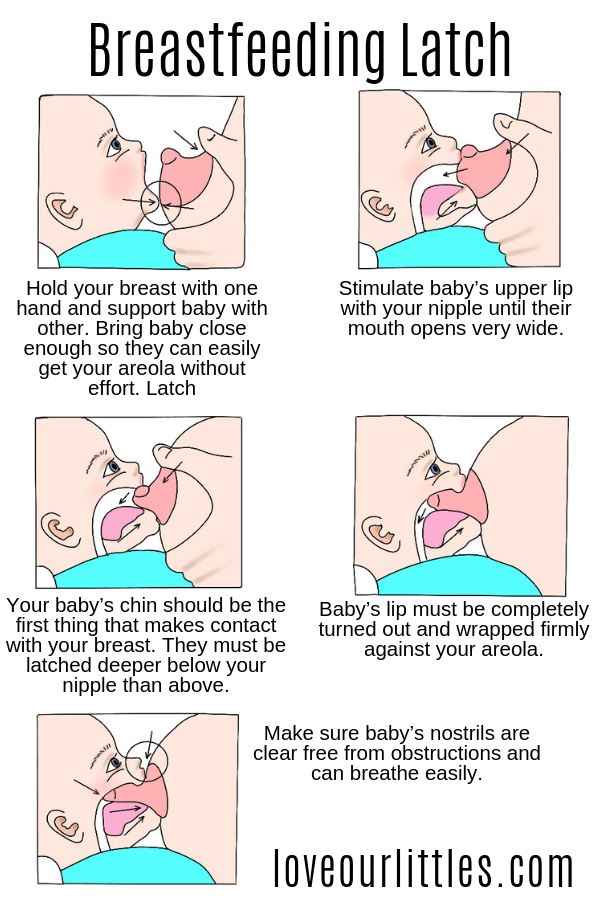
Hill, P.D., Aldag, J.C. & Chatterton, R.T. Initiation and frequency of pumping and milk production in mothers of non-nursing preterm infants. J Hum Lact 17, 9–13 (2001). - Hill P.D., Aldag J.S. and Chatterton, R.T., "Onset and frequency of expression and milk production in mothers who have given birth to premature babies and have not breastfed them." J Hum Lakt (Journal of the International Association of Lactation Consultants) 17, 9–13 (2001).
Hopkinson , J ., Schanler & Garza , C . MILK Production BY MOTHERS of PREMATURE 200 200 ANFANTS. Pediatrics 81, 815–820 (1988). - Hopkinson, J., Chanler, R., and Harza, S., "Milk production in mothers of preterm infants. " Pediatrix (Pediatrics) 81, 815–820 (1988).
" Pediatrix (Pediatrics) 81, 815–820 (1988).
Parker, L.A., Sullivan, S., Krueger, C., Kelechi, T. & Mueller, M. Effect of early breast milk expression on milk volume and timing of lactogenesis stage II among mothers of very low birth weight infants : a pilot study. J Perinatol 32, 205–209 (2012). - Parker L.A., Sullivan S., Kruger S., Kelechi T. and Muller M., "Effect of early pumping on milk supply and timing of second stage lactogenesis in mothers of extremely low birth weight infants: pilot study". J Perinatol (Journal of Perinatology) 32, 205–209 (2012).
Parker, L.A., Sullivan, S., Krueger, C., & Mueller, M. Association of timing of initiation of breastmilk expression on milk volume and timing of lactogenesis stage II among mothers of very low-birth-weight infants . Breastfeed Med (2015). - Parker L.A., Sullivan S., Kruger S., Kelechi T. and Muller M.