Feeding a baby with acid reflux
Reflux And Bottle Feeding | Feeding Your Baby
There may be times when feeding your baby is challenging. Never ignore any issues you may have – talk to your health visitor, midwife or GP if you have any concerns about bottle feeding. Here are some common feeding issues, and tips on what to do.
- Colic and bottle feeding
- Constipation and bottle feeding
- COVID-19 and bottle feeding
- Reflux and bottle feeding
- Tongue-tie and bottle feeding
Reflux and bottle feeding
When your baby brings up milk, or is sick during or after feeding, this is known as reflux. Reflux, also referred to as posseting or spitting up, is quite common and babies usually grow out of it by the age of 1.
What is baby reflux?
The muscle at the bottom of the food pipe (oesophagus) acts as a kind of door into the stomach – so when food or milk travels down, the muscle opens allowing the food into the stomach.
However, while this muscle is still developing in the first year, it can open when it should not (usually when your baby's tummy is full) allowing some food and stomach acid to travel back up again. Acid in the stomach is a normal part of the digestion process – it helps break down food.
In most babies, reflux is nothing to worry about, as long as they are healthy and gaining weight as expected.
What are baby reflux symptoms?
- constant or sudden crying when feeding
- bringing up milk during or after feeds (regularly)
- frequent ear infections
- lots of hiccups or coughing
- refusing, gagging, or choking during feeds
- poor weight gain
- waking at night a lot
GORD
When reflux becomes painful and happens frequently, this is known as ”gastro-oesophageal reflux disease” (GORD). GORD is more serious than mild, everyday reflux. The strong stomach acid can irritate and make the food pipe sore and inflamed, which is painful for your baby and may result in them needing medication.
The main signs and symptoms of GORD in your baby are:
- spitting up frequently
- tummy (abdominal) pain
- feeding difficulties
- seeming unsettled and grizzly after a feed
These symptoms can lead to your baby not gaining weight, or even losing weight.
Silent reflux
Silent reflux can be confusing as there are no obvious signs or clues (such as spitting up). It's when the food travels back up the food pipe – but it's swallowed rather than spat out so is harder to identify. But your baby may display similar symptoms to those of regular reflux.
Bottle feeding tips for babies with reflux
You can help your baby's reflux by:
- feeding little and often, smaller feeds stop their tummy getting too full
- burping your baby frequently during feeds – have a look at our Guide to burping your baby for techniques
- try to keep your baby upright, for at least an hour, after feeding - this should help keep the milk down
If you are using formula, your GP or health visitor may advise you to use a thicker formula (that's less likely to be brought up), or one that does not contain cows' milk if your baby is allergic to it. If the thickening powder does not help, your GP may recommend medicines that stop your baby's tummy producing as much acid.
If the thickening powder does not help, your GP may recommend medicines that stop your baby's tummy producing as much acid.
If you are mixed feeding (combining breastmilk and formula feeds), have a look at our advice on breastfeeding and reflux.
When to seek medical advice
If your baby has difficulty feeding or refuses to feed, keeps vomiting during or after feeding, talk to your pharmacist, GP, or health visitor. They will be able to give you practical advice on how to ease the symptoms and manage it – they may need to rule out other causes such as an intolerance to cows' milk or allergies.
It might be helpful to keep a record of when your baby feeds, with details of how often and how much your baby brings the food back up, and how often your baby cries or seems distressed. This will help your health visitor or GP decide if your baby needs treatment.
How to Feed a Baby With Reflux – bökee
We know spit up down the front of your shirt isn’t your best look, but for many new moms, it’s a rite of passage.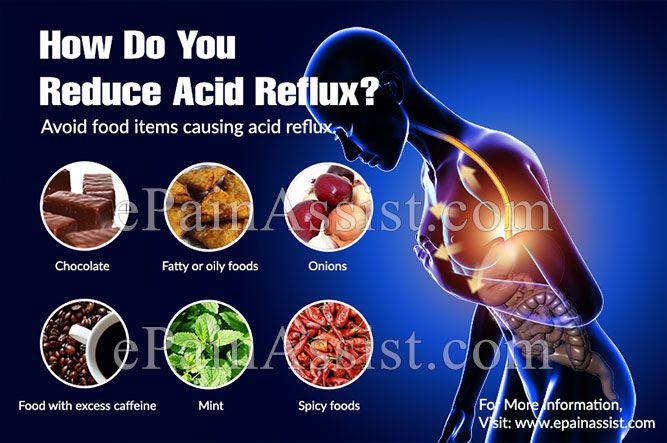 You finally just go with it because changing would mean even more laundry added to the ever-growing pile of burp cloths. But the truth is that changing the way you feed your baby can actually reduce or eliminate their uncomfortable reflux that’s causing all that spit-up.
You finally just go with it because changing would mean even more laundry added to the ever-growing pile of burp cloths. But the truth is that changing the way you feed your baby can actually reduce or eliminate their uncomfortable reflux that’s causing all that spit-up.
Even though young babies’ immature digestive systems make them prime candidates for reflux, there are several feeding strategies we suggest to improve it. Not only does reflux cause spit-up, but it can also cause your baby a lot of discomfort, and we know more than anything you want your baby to feel good.
You’ll first want to identify if your baby is experiencing reflux and what might be causing it. Then we’ll give you our top tips to get your baby’s tummy back on track (and your shirts back to pristine condition.)
What is acid reflux in babies?When a baby drinks breast milk or formula, it has a tendency to back up from her stomach. This is referred to as reflux, or gastroesophageal reflux (GER). Reflux is most common during the newborn stage (0-4 months) and improves as time goes on.
Reflux is most common during the newborn stage (0-4 months) and improves as time goes on.
According to the Mayo Clinic, this is because an infant’s ring of muscle between the esophagus and the stomach is not fully mature, allowing the contents of the stomach to flow backward.
So how do you know if your baby has reflux?
How to Identify Acid Reflux or GER in Your BabyMild reflux in young babies is common. According to Medline Plus, “About half of all babies spit up many times a day in the first 3 months of their lives.”
And even more will spit up about once or twice per day. In other words, it’s generally not a condition to be concerned about (and it’s temporary.)
Usually most parents just take the spitting up in stride if their baby seems comfortable and happy. In these cases, it’s mostly a nuisance to you while they could care less!
But there are also babies who may experience gas along with their reflux making them pretty uncomfortable or they might have what is called “silent reflux. ”
”
Whereas a baby who spits up will usually feel instantly better, a baby experiencing silent reflux will likely be in pain. This is because the acid will come up the throat, but then they swallow it back down.
If you have a baby showing the following symptoms, they’re likely suffering from one of the types of reflux:
- Frequent spit-ups
- Arching body during or after feeding
- Crying when laid on their back
- Inconsolable crying after feeding (but could also be hours later)
- Pulling legs up
- Trouble sleeping
If your baby is under 4 months and growing well, you don’t need to be concerned about your baby’s reflux. But even though you don’t need to be “concerned,” it's still stressful when you feel like your baby isn't feeling their best but you can't help them.
Identifying your baby’s symptoms as reflux is the first step to fixing it. Knowing what causes it helps, too. That's when you’ll be able to utilize our tips to help your baby feel their best (while keeping the spit up to a minimum. )
)
The cause of reflux in a young baby is pretty straightforward. It’s really not about anything you’re doing wrong, instead, you just have a tiny little human on your hands whose digestive system is still maturing.
Other than that, the fact that babies lie on their backs so often and are on a completely liquid diet make them susceptible to reflux symptoms. Premature babies, especially, have a hard time.
This all sounds pretty standard, right? And the fact that your baby is on a 100% liquid diet is out of your control. Luckily, there are some easy strategies that you can start implementing today that will improve your baby’s reflux or even eliminate it altogether.
Feeding a Baby with Reflux: Top TipsWe at bökee are all parents. Though we can’t say necessarily that we’ve experienced it all, we’ve certainly experienced a lot raising babies. What we do know is that no two are alike and what works perfectly for your first baby will surely be the one thing that doesn’t work with the next. With that said, we suggest giving these different strategies a shot in order to help your baby through their reflux.
With that said, we suggest giving these different strategies a shot in order to help your baby through their reflux.
1.) Try Paced Bottle Feeding
If you bottle feed, implementing paced bottle feeding is a good place to start.
In a nutshell, paced bottle feeding utilizes the following:
- A slow-flow nipple
- An upright feeding position
- Only 20-30 seconds of continuous feeding and then pull the bottle back to give your baby a break
With paced bottle feeding, you slow down a bottle-feed in order to better mimic typical breastfeeding patterns. “Paced feeding reduces the risk of overfeeding that may result in discomfort to the baby,” writes the Minnesota Department of Health.
In our article, “How Paced Bottle Feeding Will Benefit Your Baby,” we discuss this feeding strategy further and give you the steps on how to put it into practice.
2.) Feed in Smaller Quantities, but More FrequentlyJust as paced bottle feeding reduces the likelihood that your baby will overeat and get reflux, feeding your baby in smaller quantities but more often can have the same effect.
When babies take in a large meal at one time, it can be difficult to digest all at once. It also makes it more likely that some will come right back up through your baby’s immature ring muscle between the esophagus and stomach.
With this strategy, your baby will still drink the same amount of breast milk or formula in a 24-hour period, but could be given in 10 feeds instead of 7 (as an example.)
3.) Keep Baby in an Upright Position During Feeding and AfterBabies sleep a lot and that means a lot of laying down. But reducing this amount of time is one of the easiest ways to prevent reflux symptoms.
We recommend the following:
- Keep baby upright during feeds
- Hold your baby upright for the 20 - 30 minutes following a feed
- Wear your baby in a baby carrier so you can get a break while being able to keep your baby upright more often
With this said, we want to caution you against usually sleep positioners. You may be tempted to try these due to their promises of reducing a baby’s reflux, but the AAP advises against their use due to SIDS concerns. Even babies with reflux should be placed on their back on a flat mattress to sleep.
You may be tempted to try these due to their promises of reducing a baby’s reflux, but the AAP advises against their use due to SIDS concerns. Even babies with reflux should be placed on their back on a flat mattress to sleep.
This works great with a paced bottle feeding approach. Every 20-30 seconds try burping your baby. At a minimum, you should burp your baby after every 1-2 ounces of milk ingested.
The best way to burp a baby experiencing reflux is by holding them with their tummy side against your chest and burping them over your shoulder.
This will allow for removal of trapped gas and acid from your baby’s system before giving them further milk to drink. They may still have “wet burps” but that's a whole lot better than a full-blown spit-up at the end of a feed!
The tips we just covered are the easiest to implement right away. And for many babies, it will be all you need to do! If your baby is still spitting up or is experiencing irritability related to gas or silent reflux, we recommend trying these last two suggestions:
5. ) Consider “Drops” Prior to or After Feeding
) Consider “Drops” Prior to or After FeedingGripe Water is a natural remedy that helps to relieve reflux and other infant stomach aches. The herbs can help ease digestion. Utilizing these drops in combination with the above recommendations will likely work for many babies.
If you think your baby’s discomfort is related to gas, Mylicon is an over-the-counter remedy that many parents swear by. It’s common for babies to have both reflux and gas, so it’s worth a shot if what you’ve done hasn’t shown a lot of improvement.
We love using these two options with the bökee. Because a baby experiencing silent reflux or gas is often crying and inconsolable, this leaves you having to open these bottles one-handed while you carry your baby in the other. The last thing you want to do is put your baby down in these moments. The bökee may have originally been designed for easier bottle prep, but it works great to stabilize medicine bottles to get the tops off so you can get the medicine to your baby more quickly.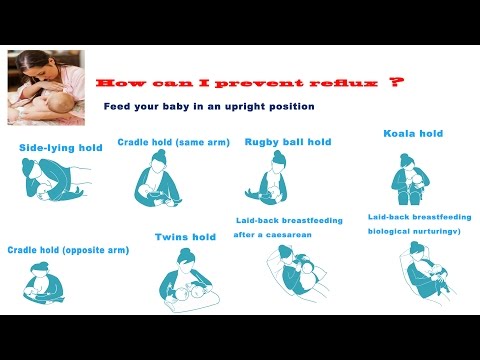
Though it can be annoying to have to go out and buy a brand new set of bottles, getting the right bottle can often be the solution you’re looking for to eliminate your baby’s reflux. You'll want to look for bottles with a type of vent system that eliminates air bubbles in your baby's breast milk or formula.
You can find some great anti-reflux bottle options here.
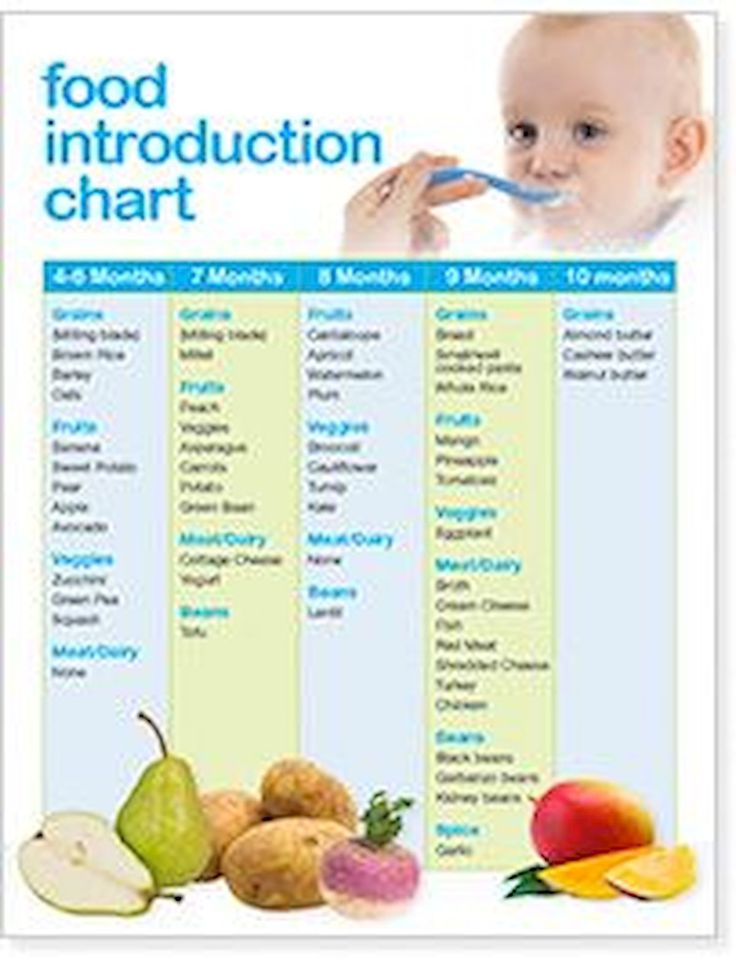
You may also see recommendations to use a special formula designed for reflux relief or to put rice cereal in your baby’s bottle to thicken your baby’s milk (making it more difficult for them to bring it back up). But these two options should be done at the direction of your doctor. So, how do you know when it’s time to contact your pediatrician?
When to Consult a Doctor for Your Baby’s RefluxThough mild cases of reflux can usually be improved by using the above strategies, some babies may need further intervention if those don’t help.
Babies who experience further distress may be experiencing a more severe form of reflux called GERD. Consulting a doctor at this time is necessary.
This may be noted by the following symptoms:
- Large volumes of spit-up
- Vomiting
- Difficulty eating
- low/no weight gain
If you notice any of these in your baby, getting direction from your doctor is imperative.
Final Word on Feeding a Baby With RefluxLuckily for most families, dealing with reflux and spit-up is a challenge that’s easy enough to work through. Taking the time to implement a few of the simple strategies above will help you avoid the milk stain while keeping a smile on your sweet baby’s face.
Infant Reflux: Symptoms and Treatment
Search Support IconSearch Keywords
Home ›› What is Reflux in Infants?
Home ›› What is reflux in babies?
↑ Top
Signs and what to do
Post-feed regurgitation is a common occurrence in the first few months of life. This is usually harmless and completely normal, but parents should read about gastroesophageal reflux (GER) and laryngopharyngeal reflux (LPR) in infants and how long it lasts to give them peace of mind. nine0019
This is usually harmless and completely normal, but parents should read about gastroesophageal reflux (GER) and laryngopharyngeal reflux (LPR) in infants and how long it lasts to give them peace of mind. nine0019
We look at signs of reflux in babies, symptoms of different types of reflux, and how to help a child with signs of reflux. If you require further information, always contact your healthcare provider.
What is reflux in babies?
So we know reflux is common, but what causes reflux in babies? Because young children have not yet fully developed the lower esophageal sphincter (LES), that is, the muscle at the bottom of the esophagus that opens and closes to let food into the stomach and keep it there, food can easily pass back up the esophagus. nine0003
Acid reflux, also known as gastroesophageal reflux (GER), is a normal reflux that occurs in babies. This type of reflux is considered normal and occurs in 40-65% of babies.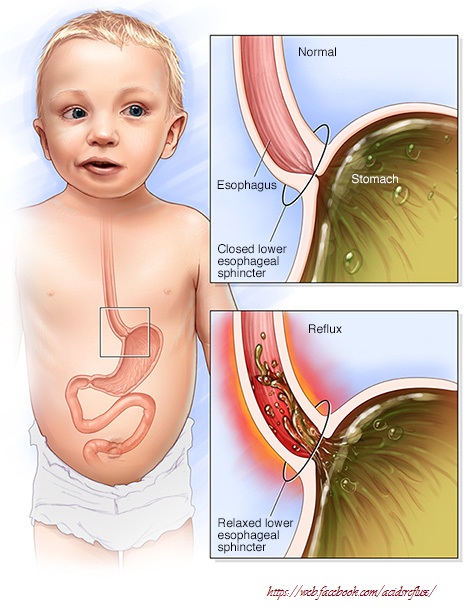
How do I know if my child has acid (gastroesophageal) reflux?
If a baby is spitting up milk after a feed, it is most likely acid reflux. As babies get older, GER usually goes away on its own without any intervention. If a baby has complications beyond just spitting up a small amount of milk (such as feeding difficulties and discomfort), they may have gastroesophageal reflux disease (GERD). nine0019
Symptoms of GERD include:
- baby arching during or after feeding;
- crying more than three hours a day for no apparent reason;
- cough;
- gag reflex or difficulty swallowing;
- irritability, restlessness after eating;
- eating little or not eating;
- poor weight gain or loss;
- difficult breathing;
- severe or frequent vomiting. nine0019
GERD usually occurs when LES muscles are not toned in time, causing stomach contents to back up into the esophagus.
How do I know if my child has Laryngopharyngeal Reflux?
Another type of reflux, laryngopharyngeal reflux (LPR), also called silent reflux, is when the contents of the baby's stomach leak back into the larynx, the back of the nasopharynx. This type of reflux does not always cause external symptoms, which is why it is called "silent". Babies can have GERD and silent reflux at the same time, but their symptoms are somewhat different. nine0019
The following are some of the symptoms of laryngopharyngeal reflux:
- breathing problems;
- gag reflex;
- chronic cough;
- swallowing problems;
- hoarseness;
- regurgitation;
- poor weight gain or weight loss.
We have looked at the signs of reflux in infants, now we will move on to the treatment and duration of silent reflux in children, as well as the treatment of GERD. nine0003
How to deal with laryngopharyngeal reflux in babies while breastfeeding?
Breastfeeding mothers may need to review their diet if their babies show signs of reflux.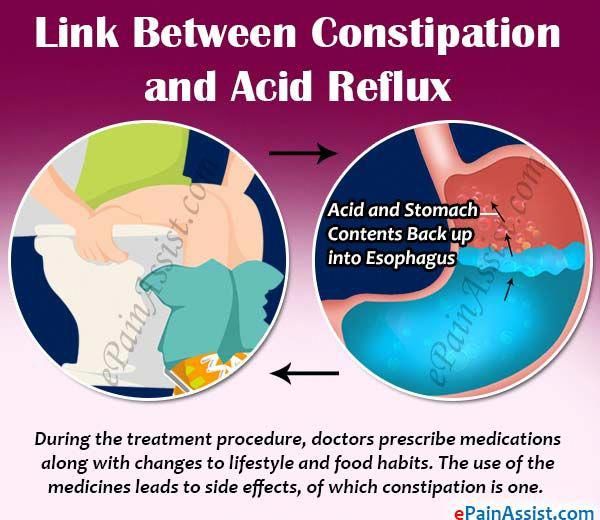 The American Academy of Pediatrics (AAP) recommends breastfeeding mothers cut eggs and milk from their diet for two to four weeks to see if their baby's reflux symptoms improve or disappear. It may be worth eliminating acidic foods from your diet. nine0019
The American Academy of Pediatrics (AAP) recommends breastfeeding mothers cut eggs and milk from their diet for two to four weeks to see if their baby's reflux symptoms improve or disappear. It may be worth eliminating acidic foods from your diet. nine0019
In most cases, GER and laryngopharyngeal reflux go away on their own. Typically, children outgrow reflux in the first year of life. If a child has persistent symptoms of laryngopharyngeal reflux, parents should consult a doctor. If your baby has severe vomiting, blood in the stool, or any of the symptoms of GERD listed above, parents should contact their pediatrician as soon as possible.
How can I help my child with reflux or GERD? nine0008
Reflux symptoms in babies usually go away on their own, but the following tips can help relieve symptoms:
- Thicken food with rice or a special milk thickener.
- Hold the bottle at an angle that fills the nipple completely with milk to reduce the amount of air your baby swallows.
 This can help prevent colic, gas, and reflux.
This can help prevent colic, gas, and reflux. - Try the AirFree anti-colic bottle, designed to reduce air swallowing during feeding. nine0047
4. Let the baby burp during and after feeding. If the baby is bottle fed, parents can let him burp after every 30-60 ml. If the mother is breastfeeding, she may let the baby burp when changing breasts.
5. Hold baby upright after feeding. As a rule, in order for the milk to remain in the stomach, after feeding the baby, it is necessary to hold it in an upright position for 10-15 minutes. But, if the child has reflux, parents should keep him upright a little longer. nine0003
These tips may help relieve symptoms, but they do not replace a doctor's advice.
Parents should not change their infant formula formula without first talking to their healthcare provider.
Don't panic! Reflux is very common in babies during the first three months of life, and most babies outgrow it without any consequences. Although GERD is a slightly more serious condition, there are many treatments, ways to manage it, and help newborns. Feel free to contact your doctor with any questions or concerns you may have. nine0003
Although GERD is a slightly more serious condition, there are many treatments, ways to manage it, and help newborns. Feel free to contact your doctor with any questions or concerns you may have. nine0003
4 Seattle Children’s Hospital
5 The National Institute of Diabetes and Digestive and Kidney Diseases - Treatment for GER & GERD in Infants
Any links to third party websites that may be included on this site are provided solely as a convenience to you. Philips makes no warranties regarding any third party websites or the information they contain. nine0003
I understand
You are about to visit a Philips global content page
Continue
You are about to visit the Philips USA website.
I understand
Gastroesophageal reflux disease in infants. Information for patients.
Gastroesophageal reflux (GER) is the medical term for regurgitation (backward reflux) of stomach contents into the esophagus and (sometimes) the mouth. Since certain acids are normally found in the lumen of the stomach, GER is sometimes (especially abroad) called acid reflux. nine0003
Since certain acids are normally found in the lumen of the stomach, GER is sometimes (especially abroad) called acid reflux. nine0003
Reflux is normal and occurs in healthy infants, children and adults. Most babies have brief episodes during which they spit up milk or breastfeeding formula through their mouth and/or nose. Uncomplicated reflux usually does not bother the child, has a low risk of developing chronic complications, and usually does not require treatment.
In contrast, children with gastroesophageal reflux disease (GERD) are whiny, gain weight more slowly, often have recurrent pneumonias, or hemoptysis. Children with these symptoms usually require further evaluation and treatment. Although most children with gastroesophageal reflux disease (GERD) symptoms resolve on their own as they grow older, some children have these symptoms as they age. nine0003
What is gastroesophageal reflux disease (GERD)?
When we eat, food passes into the esophagus and then into the stomach.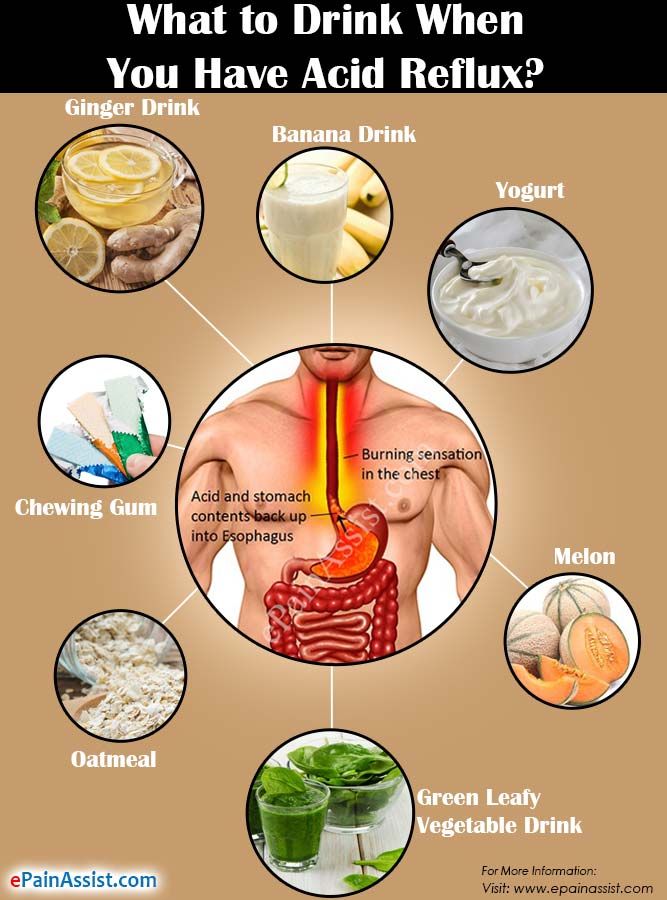 The esophagus is made up of, among other things, special layers of muscle that expand and contract to push food into the stomach in a series of undulating movements: this is called the peristaltic movement of the esophagus.
The esophagus is made up of, among other things, special layers of muscle that expand and contract to push food into the stomach in a series of undulating movements: this is called the peristaltic movement of the esophagus.
At the bottom of the esophagus, where it joins the stomach, there is a ring of muscle called the lower esophageal sphincter (LES). When food reaches the LES, it relaxes to allow it to enter the stomach, and when food passes into the stomach, it closes to prevent food and stomach acid from refluxing back into the esophagus. nine0003
Sometimes this ring of muscle (LE) does not close completely, allowing fluid from the stomach to back up into the esophagus, this can happen in anyone but is most common in infants. Most of these episodes go unnoticed because reflux only affects the lower esophagus.
As the child grows, the angle between the stomach and esophagus increases, which leads to a sharp decrease in the frequency of reflux. Spitting stops completely in more than half of children by 10 months of age, 80 percent of children by 18 months of age, and 98 percent of children under the age of two.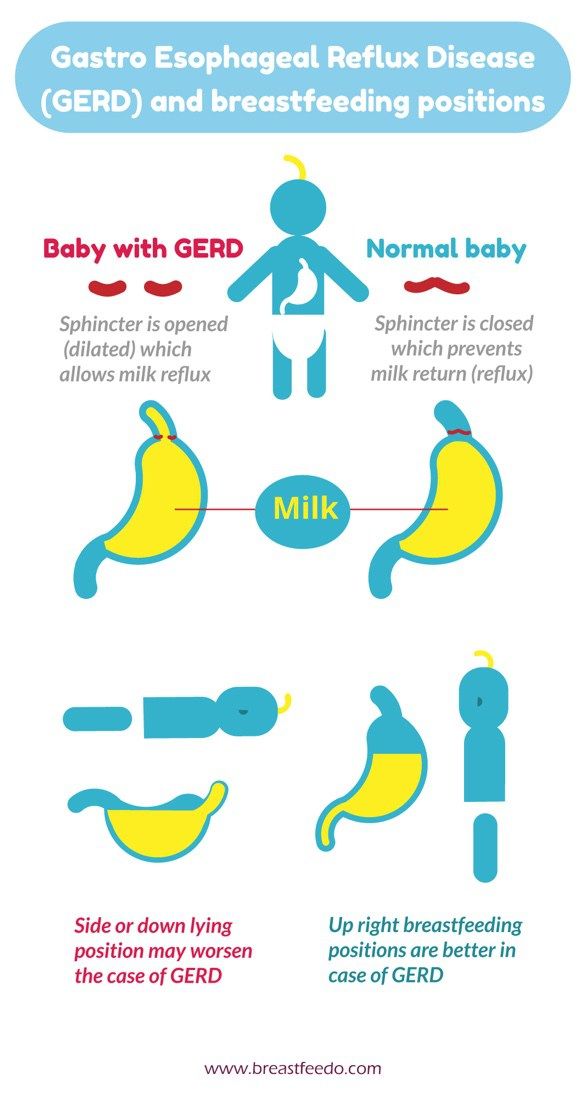
Uncomplicated gastroesophageal reflux Gastroesophageal reflux is very common in infants during the first months of life, approximately 50% of children aged 0-3 months have at least one regurgitation per day.
Babies who burp infrequently, eat enough food, have normal weight gain for their age, and don't have excessive tearfulness - so-called "uncomplicated" reflux. Such regurgitation is a consequence of the anatomical features of a child of this age, since the short esophagus and the tiny volume of the stomach contribute to the reverse flow of fluid from it. Frequent emptying of air from the stomach and limiting physical activity after feeding can reduce the frequency and amount of spitting up. nine0003
Children with uncomplicated reflux usually do not need further testing. If the symptoms increase, appear for the first time after six months of life, or do not decrease by the age of 18 to 24 months, the child should be shown to the pediatrician, and most likely will require a consultation with a gastroenterologist.
Gastroesophageal reflux disease (GERD). Simple reflux becomes gastroesophageal reflux disease when stomach acid begins to irritate or damage the esophagus. It occurs in a very small percentage of children who have frequent regurgitation. The onset of the disease is due to: a high frequency of refluxes, a large amount of refluxes, or the inability of the esophagus to quickly neutralize the acid thrown into it. Treatment for gastroesophageal reflux disease (GERD) is directed at one or more of these factors. nine0003
Some of the signs or symptoms that may indicate GERD include: refusal to eat, frequent crying and arching of the neck and back (as if in pain), aspiration during regurgitation, severe (fountain) vomiting, frequent coughing, or small gains in weight. These symptoms are not normal and require further testing to confirm the diagnosis of GERD or identify another diagnosis.
It is often difficult to tell if an infant is in pain. Usually a baby who cries from "banal" reasons can be comforted by distracting him, or by detecting and eliminating the factor that irritates him (wet diapers, hunger, desire to sleep, etc.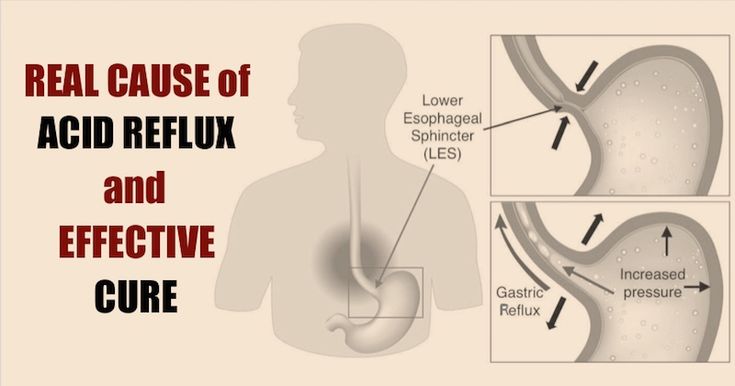 ). nine0003
). nine0003
Tearfulness and reflux. Many parents are concerned that reflux is the cause of their child's tearfulness or difficulty sleeping. However, clinical studies have shown that uncomplicated reflux does not usually cause pain, and lowering stomach acid does not reduce tearfulness.
Tearfulness and difficulty sleeping are not GERD-specific symptoms and may be due to a variety of causes. Children who have frequent regurgitation and severe tearfulness should be examined by a doctor. If there are no other problems, a milk-exclusion diet and food thickeners may be recommended for such an infant. nine0003
Diagnosis of GERD
If a child is suspected of having gastroesophageal reflux disease, the first step in the evaluation should be a history and physical examination. The need for further testing depends on what the doctor determines and may include the following tests:
- Laboratory testing (blood and/or urine)
- X-ray examination to assess the swallowing function of the infant and the anatomy of his stomach
- Endoscopy, to assess the condition of the esophagus
Treatment for GERD
Babies with uncomplicated reflux do not require any treatment, but some guidance can be given to parents to make lifestyle changes for these babies. Such recommendations usually include: avoiding overeating (eating more often and in smaller amounts), avoiding any exposure of the child to tobacco smoke, a diet with no milk, and food thickeners. We will call these measures conservative (as opposed to medical and surgical measures). nine0003
Such recommendations usually include: avoiding overeating (eating more often and in smaller amounts), avoiding any exposure of the child to tobacco smoke, a diet with no milk, and food thickeners. We will call these measures conservative (as opposed to medical and surgical measures). nine0003
Many children with reflux symptoms benefit from conservative measures. In one study, more than 80 percent of these children experienced complete or partial improvement in symptoms from conservative measures alone, such as food thickeners, avoidance of exposure to tobacco smoke, and reduced exposure to cow's milk protein (formulas based on partial protein hydrolysis, or complete exclusion of milk from the mother's diet if the child is breastfed).
Dairy-free diet. Studies show that 15 to 40 percent of children with gastroesophageal reflux disease have cow's milk protein intolerance, or "dietary, protein-induced gastroenteropathy." Diagnosis of this condition in most children is based on their symptoms, and the degree of positive response to changes in diet; laboratory studies are usually not necessary. nine0003
nine0003
Most children with dietary protein-induced gastroenteropathy are intolerant of cow's milk protein alone, although some are also intolerant of soy proteins. To eliminate these proteins from a baby's diet, breastfeeding mothers should completely eliminate all dairy and soy products from their diet. In rare cases, it may be necessary to exclude other proteins from the mother's diet, but all this should happen only on the recommendation of the attending physician.
If a child's GERD symptoms improve after two to three weeks of the diet, it is advisable to continue the diet until the child is one year old. After this age, many children get rid of intolerance to milk proteins. If, after the diet is canceled, the symptoms return, the mother should return to the restrictions in her diet and the nutrition of the baby. nine0003
If the baby is formula-fed, a formula that does not contain milk and soy protein (hydrolysates) may be offered. On this diet, the child is observed for 1-2 weeks to determine if the child's reflux symptoms are improving. If symptoms do not improve, the child may be advised to return to the original formula.
If symptoms do not improve, the child may be advised to return to the original formula.
Almost all children with protein intolerance recover from it by the age of 1 year.
Food thickeners. An adapted formula with a thickener, or expressed breast milk with a thickener added, can help reduce the frequency of spitting up and relieve symptoms in a baby who is gaining well. In children under the age of three months, or children with allergies, thickeners can only be prescribed by a doctor. However, thickeners are not recommended as monotherapy (the only treatment) in infants whose esophagus is already damaged by acid reflux (i.e., children with esophagitis). nine0003
In the United States of America, substances derived from rice are commonly used as food thickeners, in other countries rice starch, corn and potato starch, carob flour, or carob bean gluten are often used. To thicken your baby's nutrition, one tablespoon of rice starch per 1 ounce (about 30 ml) of formula or expressed breast milk is usually used. The hole on the nipple of the bottle should be slightly larger than usual to allow the passage of thickened formula or breast milk. However, it should not be too large, so that the child does not choke if the mixture flows too quickly. If the doctor recommended feeding the child with thickeners, then the usual formula for the child, or expressed milk, is mixed immediately before feeding with a special baby thickener, which are sold in pharmacies. In addition, there are ready-made artificial mixtures containing thickeners in their composition. nine0003
The hole on the nipple of the bottle should be slightly larger than usual to allow the passage of thickened formula or breast milk. However, it should not be too large, so that the child does not choke if the mixture flows too quickly. If the doctor recommended feeding the child with thickeners, then the usual formula for the child, or expressed milk, is mixed immediately before feeding with a special baby thickener, which are sold in pharmacies. In addition, there are ready-made artificial mixtures containing thickeners in their composition. nine0003
Women who are breastfeeding are generally advised not to replace breast milk with formula, but rather to express and add a thickener. Breast milk itself has properties that help babies recover from GERD.
Body position. Babies may have fewer episodes of spitting up if they are upright and physically and mentally calm each time after feeding for 20 to 30 minutes after feeding (i.e. the infant should be carried on an adult's shoulder rather than laid to bed after feeding). Parents should avoid large amounts of feeding, and should interrupt feeding as soon as the infant begins to lose interest in food and become distracted. nine0003
Parents should avoid large amounts of feeding, and should interrupt feeding as soon as the infant begins to lose interest in food and become distracted. nine0003
Drug therapy for GERD. If the child's symptoms do not improve after the conservative treatment described above, drugs that reduce the acidity of gastric contents may be recommended. There are a number of medications available to treat heartburn in adults. However, it should be remembered that the safety and efficacy of these drugs in children is completely different.
Children with uncomplicated gastroesophageal reflux (without esophagitis) should not be given drugs that reduce gastric acidity or gastric emptying rate. nine0003
Children with suspected GERD may have good symptomatic response with short courses of acid-blocking drugs. Omeprazole and lansoprazole have been best studied in infants. If after the appointment of these drugs there is no noticeable decrease in the manifestations of GERD, the course of treatment is most often interrupted.