Feeding your baby breastmilk and formula
How to combine breast and bottle feeding
It can take several weeks for you and your baby to feel happy and confident with breastfeeding.
Once you've both got the hang of it, it's usually possible to offer your baby bottles of expressed milk or formula alongside breastfeeding.
This is sometimes called mixed or combination feeding.
Why combine breast and bottle?
You may want to combine breastfeeding with bottle feeding if you:
- are breastfeeding and want to use a bottle to offer your baby some expressed breast milk
- want to breastfeed for some of your baby's feeds, but give bottles of formula for 1 or more feeds
- are bottle feeding your baby and want to start breastfeeding
- need to leave your baby and want to make sure they have some milk while you're away
Introducing formula feeds can affect the amount of breast milk you produce. There is also a small amount of evidence to show babies may not breastfeed as well because they learn to use a different kind of sucking action at the bottle than at the breast.
These things can make breastfeeding more difficult, especially in the first few weeks when you and your baby are still getting comfortable with breastfeeding.
Your breastmilk supply will usually not be affected if you start bottle feeding your baby when they are a bit older, you are both comfortable with breastbeeding, and you breastfeed every day.
Introducing formula feeds
If you're combining breastfeeding with formula feeds both you and your baby can carry on enjoying the benefits of breastfeeding.
If you choose to introduce infant formula:
- it's best to do it gradually to give your body time to reduce the amount of milk it makes – this helps lower your chance of getting uncomfortable, swollen breasts, or mastitis
- if you're going back to work, start a few weeks beforehand to give both of you time to readjust
- if your baby is 6 months old or more and can drink milk from a cup, you may not need to introduce a bottle at all
For more information, see drinks and cups for babies.
Giving your baby their first bottle
It may take a while for a breastfed baby to get the hang of bottle feeding, because they need to use a different sucking action.
- it usually helps to give the first few bottles when your baby is happy and relaxed – not when they're very hungry
- it may help if someone else gives the first bottle feeds, so that your baby is not near you and smelling your breast milk
- you might want to try using a different position for bottle and breastfeeding
See more advice on how to bottle feed.
Restarting breastfeeding
If you want to start breastfeeding more and give your baby fewer bottles, it's a good idea to ask your midwife, health visitor or breastfeeding supporter for support.
These tips may help too:
- Hold and cuddle your baby as much as possible, ideally skin to skin. This will encourage your body to make milk and your baby to feed.

- Express your breast milk regularly. Expressing releases the hormone prolactin, which stimulates your breasts to make milk. About 8 times a day, including once at night is ideal. It may be easier to express by hand to begin with – your midwife, health visitor or breastfeeding supporter can show you how.
- Try bottlefeeding while holding your baby skin to skin and close to your breasts.
- If your baby is latching on, feed little and often. Do not worry if your baby does not feed for long to begin with. See tips on how to get your baby properly positioned and attached.
- Choose times when your baby is relaxed, alert and not too hungry, and do not force your baby to stay at the breast.
- Decrease the number of bottles gradually, as your milk supply increases.
- Consider using a lactation aid (supplementer). A tiny tube is taped next to your nipple and passes into your baby's mouth so your baby can get milk via the tube as well as from your breast.
 This helps to support your baby as they get used to attaching to the breast. Your midwife, health visitor or breastfeeding supporter can give you more information.
This helps to support your baby as they get used to attaching to the breast. Your midwife, health visitor or breastfeeding supporter can give you more information.
See more tips on boosting your milk supply.
Help and support with mixed feeding
If you have any questions or concerns about combining breast and bottle feeding:
- talk to your midwife, health visitor or breastfeeding supporter
- call the National Breastfeeding Helpline on 0300 100 0212 (9.30am to 9.30pm, every day)
- find breastfeeding support near you
Video: why combine breast and bottle feeding?
In this video, 3 mothers discuss ways to combine breast and bottle feeding.
Media last reviewed: 22 March 2020
Media review due: 22 March 2023
Page last reviewed: 8 October 2019
Next review due: 8 October 2022
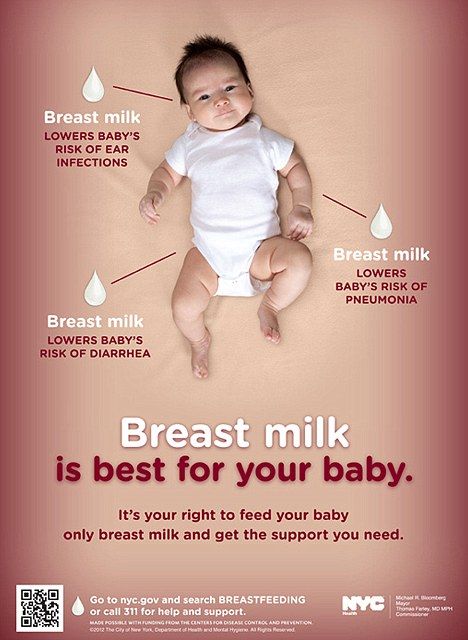
How to Supplement Breastmilk with Formula – Happiest Baby
Exclusive breastfeeding may be the ultimate goal for some, but the reality is, for many parents, combo feeding with breastmilk and baby formula becomes necessary at some point. In fact, almost 36% of breastfed babies receive supplemental formula before they’re 6 months old, according to the Centers for Disease Control and Prevention. And there’s nothing wrong with that! There’s no rule that says you have to choose between breastfeeding and formula. It’s not an all-or-nothing approach…and you can most certainly do both! Fed is best, after all. If you’re considering combo feeding, read on to learn why others choose this route—and how to best approach this feeding strategy.
In fact, almost 36% of breastfed babies receive supplemental formula before they’re 6 months old, according to the Centers for Disease Control and Prevention. And there’s nothing wrong with that! There’s no rule that says you have to choose between breastfeeding and formula. It’s not an all-or-nothing approach…and you can most certainly do both! Fed is best, after all. If you’re considering combo feeding, read on to learn why others choose this route—and how to best approach this feeding strategy.
There’s not one overriding reason why families choose to supplement breastfeeding with formula. Instead, there are many. Here are some of the most common reasons parents add baby formula to the mix.
Your Pediatrician Recommended Supplementing with FormulaIf your baby was born premature or is having difficulties growing and gaining weight, your pediatrician may recommend supplementing with infant formula for additional calories and nutrition. Your doctor may also suggest supplementing with baby formula if your little one develops jaundice, which occurs when a chemical called bilirubin builds up in your baby’s blood. Supplementing breast milk with formula can lower bilirubin levels—and help sidestep the need for further treatment.
Your doctor may also suggest supplementing with baby formula if your little one develops jaundice, which occurs when a chemical called bilirubin builds up in your baby’s blood. Supplementing breast milk with formula can lower bilirubin levels—and help sidestep the need for further treatment.
Pumping is a lot of work…and, truth is, there still isn’t a ton of support to continue pumping once a nursing mom heads back to work or school. In fact, a Mamava survey found that only 40% of employed moms have access to a designated lactation room at work. (Forty-three percent pumped in a borrowed or repurposed space, like a closet, and 13% had to resort to pumping breastmilk in their car). If you can relate, consider speaking with an international board certified lactation consultant (IBCLC) for advice on how to best make pumping work…and you may just find that supplementing with formula helps keep pumping and nursing going.
Your Milk Supply Is LowThinking you’re not producing enough breastmilk is one of the biggest reasons parents stop nursing, notes a report in Maternal & Child Nutrition. But the reality is, physically not being able to produce enough breastmilk is only an issue for about 5% of breastfeeding moms. If you feel your milk supply is low, don’t hesitate to get some guidance from an IBCLC, your baby’s pediatrician, or a local breastfeeding support group.
But the reality is, physically not being able to produce enough breastmilk is only an issue for about 5% of breastfeeding moms. If you feel your milk supply is low, don’t hesitate to get some guidance from an IBCLC, your baby’s pediatrician, or a local breastfeeding support group.
Breastfeeding is a beautiful way to bond with your baby—and it’s recommended that new parents exclusively breastfeed for about the first six months. But usually only one parent can offer this service, perhaps leaving your partner with a little FOMO. The solution for many: Tag team Baby’s feedings. While you get some much needed rest, your partner feeds the baby pumped breastmilk or prepared formula.
You Prefer Supplementing With FormulaAnd, guess what? If breastfeeding and supplementing with formula works best for you, that’s totally okay! When it comes to feeding your baby, the most important factors are 1) your little one gets the nutrition they need, and 2) you’re feeding your baby in a way that works for you and your family.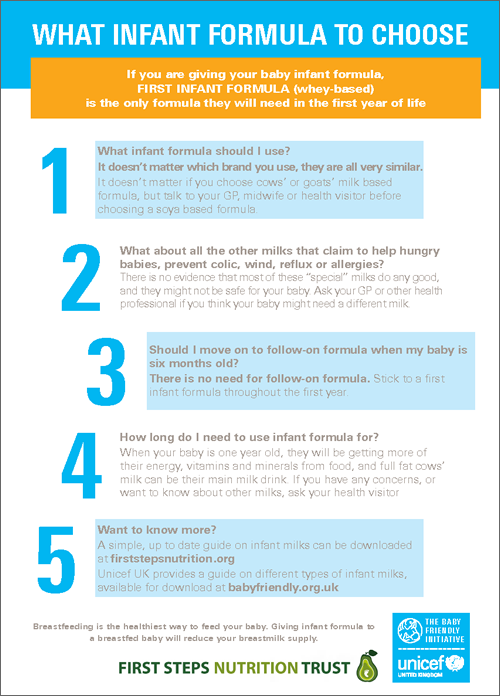 While everyone’s feeding situation is different, in the end, all parents simply want a thriving, healthy, and happy baby.
While everyone’s feeding situation is different, in the end, all parents simply want a thriving, healthy, and happy baby.
If you’ve decided to go the formula route from the get-go, that’s one thing. But planning to breastfeed and offer baby formula requires planning and troubleshooting to ensure your milk supply remains intact. Here’s help.
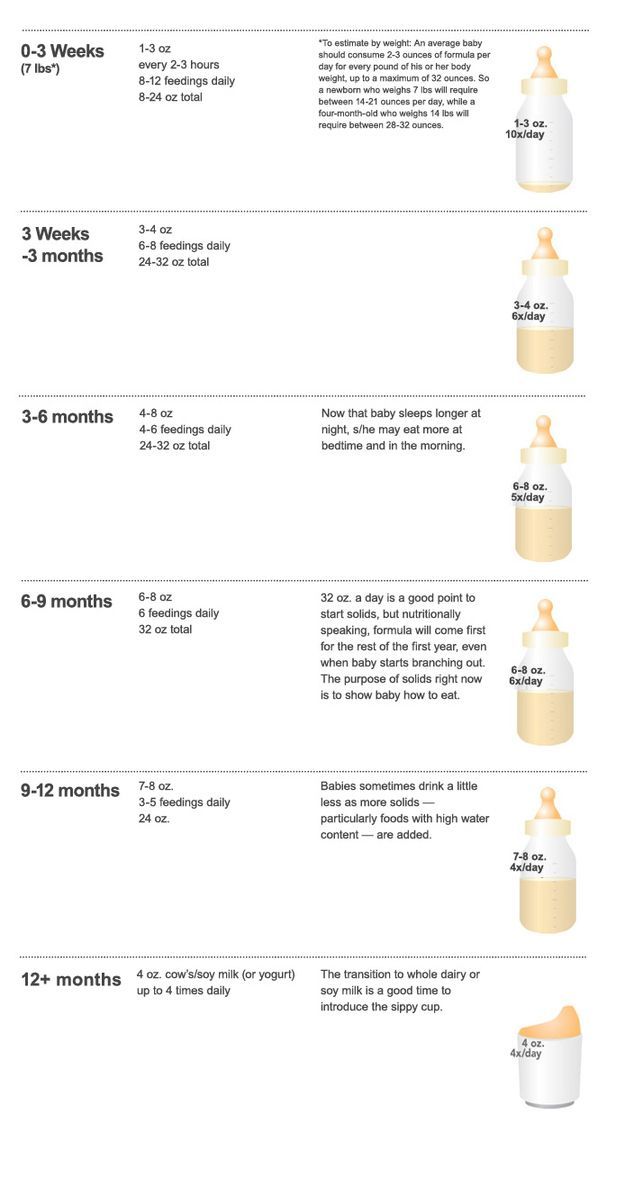
Introduce formula at the right time.Research shows that the more formula given to a baby in the hospital after birth, the less likely Mom will continue to breastfeed. You see, when a newborn gets filled up on formula, they’re less inclined to wake and nurse well for their next feed…which can set you on the path to producing less milk and Baby preferring the ease of the bottle. (With breastfeeding, Baby needs to establish a deep latch, suckle quickly to get the milk flowing, then slow the suck to a rhythmic pattern to empty your breast. With bottles, there’s a steady flow from the start, making eating a breeze.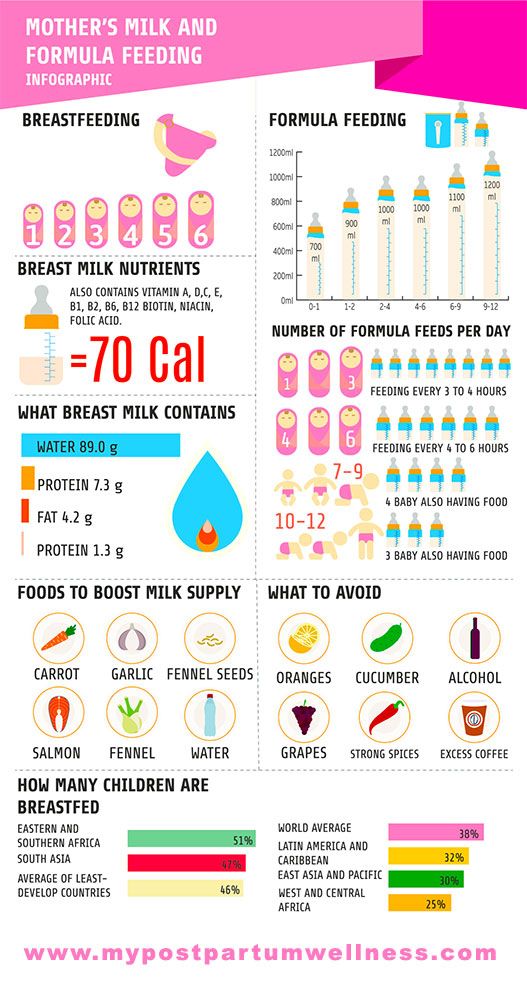 )
)
If you’re planning on (even partially) breastfeeding, it’s best to wait until your little one is about 3 to 4 weeks old before offering a bottle of formula or breastmilk. Alternatively, if you wait till, say 2, 3, or 4 months to introduce a bottle, your precious bub may say No Thanks. To sidestep that, try offering your baby one bottle a day—of breastmilk or formula—around 6 weeks.
Choose a safe infant formula.Truth: All commercial formulas sold in the United States are perfectly safe for babies thanks to some very specific and stringent manufacturing regulations put forth by the Food and Drug Administration. (PS: Homemade infant formula can lead to serious health problems for your baby. Do not use!) To choose the very best baby formula for your baby, make sure the container is sealed, unexpired—and is labeled iron-fortified. While most commercial infant formulas sold in America contain iron, it’s not universal, so be sure to check. Iron-fortified infant formulas are the recommended choice, according to the Centers for Disease Control and Prevention (CDC).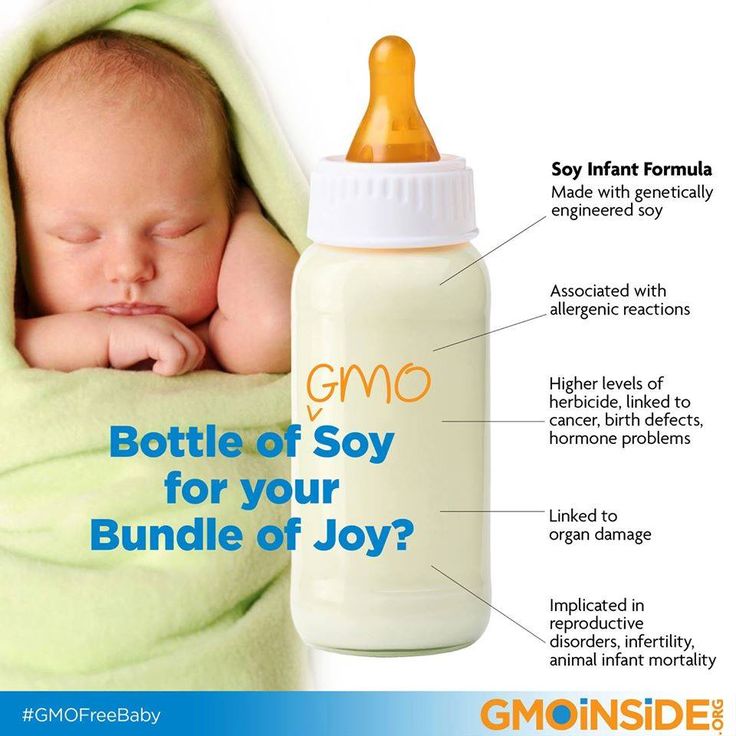 Also, double check the label to ensure the baby formula in question is, in fact, for babies! (Toddler formulas can look very similar.) And feel free to ask your baby’s pediatrician or registered pediatric dietitian for advice on selecting the right formula for your baby.
Also, double check the label to ensure the baby formula in question is, in fact, for babies! (Toddler formulas can look very similar.) And feel free to ask your baby’s pediatrician or registered pediatric dietitian for advice on selecting the right formula for your baby.
Formula feeding can be so very helpful…but it can also threaten your milk supply. To ensure your breasts continue to fill with milk, try introducing just two ounces of formula after one breastfeeding session each day to start. (Again, try to wait till your baby is about 6 weeks old.) If after a week of one-bottle-a-day is working, you can try add a second two-ounce bottle to your day while you continue to breastfeed. And when starting out, always offer breastmilk before the bottle.
Gauge your baby’s mood.The best time to introduce formula to your baby is when your sweet pea is content and calm—not super-hungry and flailing. When it’s time to eat, nurse your tot enough to fill their tummy.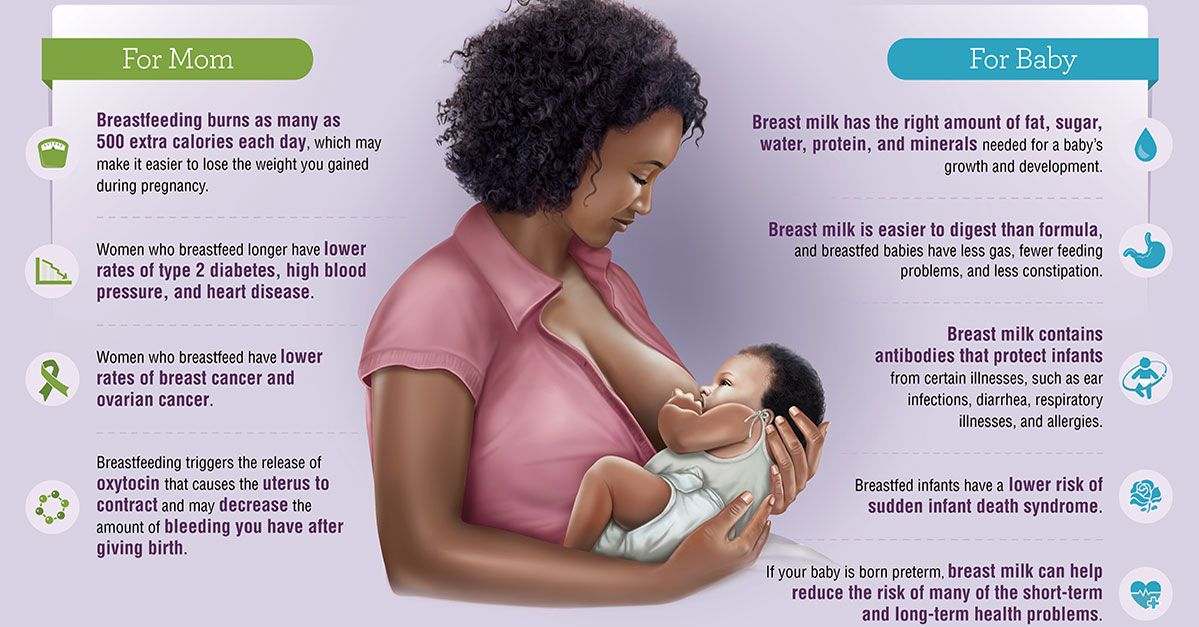 Then, if Baby still shows some signs of hunger after that breastfeeding session, offer a small bottle with formula. If your babe is totally satisfied post-nursing, you might wait 30 minutes to an hour later to offer formula. The key: Don’t wait until your baby is overly hungry to try baby formula!
Then, if Baby still shows some signs of hunger after that breastfeeding session, offer a small bottle with formula. If your babe is totally satisfied post-nursing, you might wait 30 minutes to an hour later to offer formula. The key: Don’t wait until your baby is overly hungry to try baby formula!
Before preparing your baby’s formula, wash your hands and wash and sanitize the bottle and bottle accessories. If you’re using a powder baby formula, make sure the water you use to mix in is safe, notes the American Academy of Pediatrics. Unsure? Check your local health department to find out. And while parents often assume they need to use warm water to mix infant formula, the CDC attests that that’s not true. Cool or warm, it’s really up to you. That said, if your baby prefers warm milk, you can safely heat Baby’s full bottle by placing it into a warm water bath for several minutes. It’s best to avoid the microwave here, since it can create hidden hot spots that can burn Baby’s mouth.
And if you’re hoping to create some bottles that are a mix of breastmilk and formula, know that that’s A-okay! Breastmilk and formula can be combined as long as the baby formula is safely mixed first. (Avoid adding formula powder to your breastmilk unless under the direction of your baby’s pediatrician.)
Seek help and support.Feeding a baby is no easy feat! If you’re thinking of supplementing with formula, it’s good to get some extra help to ease your worries. Consider reaching out to the La Leche League, a local lactation consultant, and/or another group that can support parents who breastfeed and supplement.
Troubleshooting Formula Feeding ProblemsBecause baby formula tastes different from your breastmilk and the act of sucking from a bottle is not like suckling from a breast, some resistance or confusion can arise when introducing supplemental formula to your baby.
Formula Feeding Problem: My baby chokes on formula.
Since breastmilk flows slower than formula from a bottle, that faster flow can catch your baby off-guard—and may cause coughing and spitting up. To help, try switching the nipple on your bottle to one with a slower flow. At the same time, use what’s called the “paced bottle feeding method” to better mimic breastfeeding. To do this, hold your little one as upright as possible and keep the bottle parallel to the floor during the feeding. Doing it this way keeps your baby from guzzling formula too quickly. Depending on your bub, it may take 10 to 15 minutes to finish a bottle, which is similar to breastfeeding.
Formula Feeding Problem: My baby refuses formula bottles.
Babies may refuse bottles filled with formula because breastmilk is sweeter than formula…and thus, more taste-bud friendly. While you can’t do anything about that, you can enlist another person to offer early bottles, so your little one is less likely to expect that comforting sweet treat associated with you.
Because breastmilk is easy to digest, you may notice an increase in baby toots when supplementing with formula. Plus, babies can be sensitive to lactose or milk proteins in formula, which may cause gassiness. While some toots can be totally normal, if your baby seems very fussy and very gassy, speak with your pediatrician about the possibility of switching to a different baby formula. There are specially-designed sensitive infant formulas that may help settle your wee one’s bloated belly and reduce gas.
Formula Feeding Problem: Baby is now refusing the breast.Some babies prefer the faster flow of milk from a bottle, causing them to shun the harder work of drinking from the breast. To help, try the nurse-first method where you breastfeed before offering formula. Also, you might try pumping your breastmilk and offering it in a bottle with a quicker-flow nipple.
Formula Feeding Problem: Infant formula is expensive.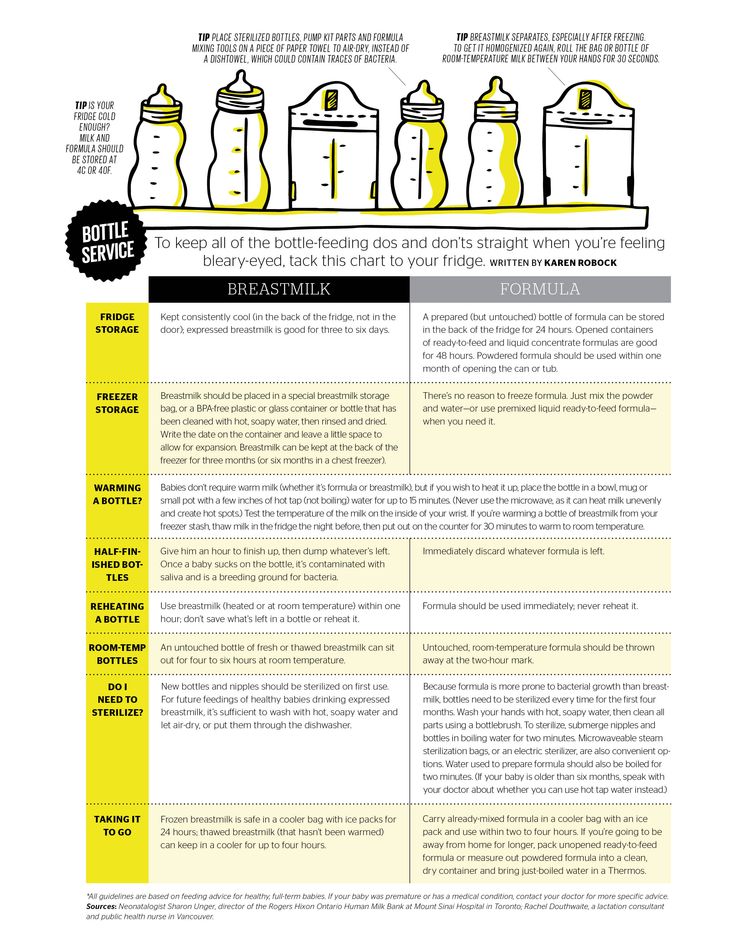
Baby formula is pricey! In fact, baby formula can cost anywhere between $1,200 and $1,500 throughout your baby’s first year. Here are a few things you can do to work around the hefty expense of purchasing baby formula.
-
Stick to powder formula. It’s always going to be cheaper than liquid and concentrate versions.
-
Consider calling your local WIC office. If you’re eligible, you can get free breastfeeding help, access to breast pumps, and a monthly formula allotment, all for free.
-
Accumulate samples. Baby formula reps often drop samples for patients at pediatrician offices, so never hesitate to ask for some.
-
Get on lists! Sign up for the email list of commercial formula companies for samples, coupons, and special deals.
-
Buy store brand. Since all commercial infant formula is safe, consider purchasing store brand formula...that contains iron, of course.
About Gabrielle McPherson
Gabrielle McPherson, MS, RDN, LDN is registered dietitian in Missouri who specializes in community and pediatric nutrition.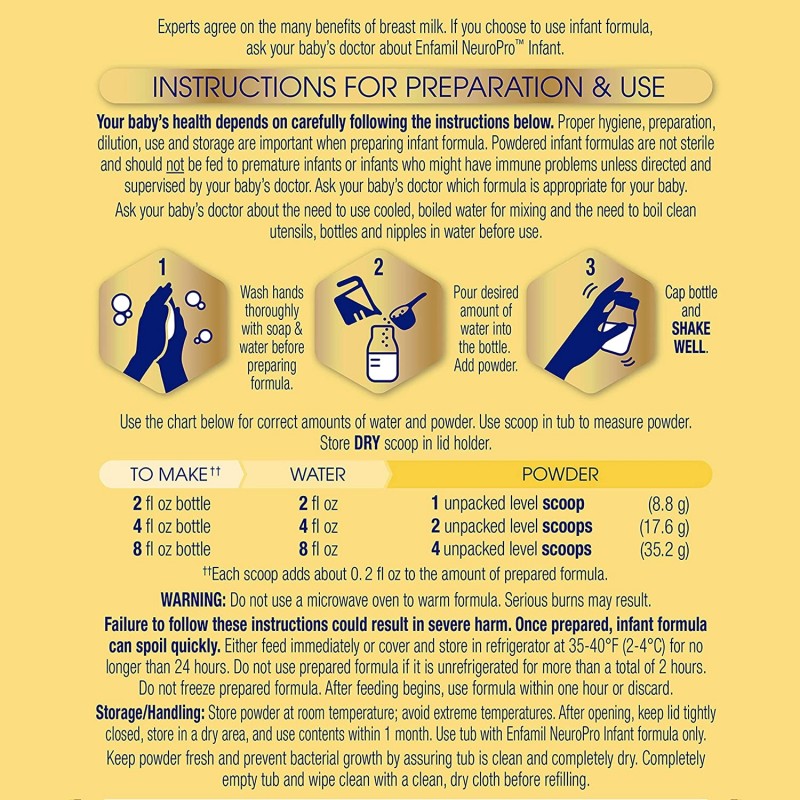 Gaby is passionate about encouraging families to eat well in simple, practical ways that are realistic...and delicious! When not working, Gaby loves cooking, baking, and making messes and memories with her sous-chef/preschooler Charlotte.
Gaby is passionate about encouraging families to eat well in simple, practical ways that are realistic...and delicious! When not working, Gaby loves cooking, baking, and making messes and memories with her sous-chef/preschooler Charlotte.
View more posts tagged, feeding
Have questions about a Happiest Baby product? Our consultants would be happy to help! Connect with us at [email protected].
Disclaimer: The information on our site is NOT medical advice for any specific person or condition. It is only meant as general information. If you have any medical questions and concerns about your child or yourself, please contact your health provider.
Breast milk and formula: what do they have in common?
1 Cribb VL et al. Contribution of inappropriate complementary foods to the salt intake of 8-month-old infants. Eur J Clin Nutr . 2012;66(1):104. - Cribb V.L. et al., "Effects of inappropriate complementary foods on salt intake in 8-month-old infants". Yur J Clean Nutr. 2012;66(1):104.
2012;66(1):104. - Cribb V.L. et al., "Effects of inappropriate complementary foods on salt intake in 8-month-old infants". Yur J Clean Nutr. 2012;66(1):104.
2 Lönnerdal B. Nutritional and physiologic significance of human milk proteins. Am J Clin Nutr . 2003;77(6):1537 S -1543 S - Lönnerdahl B., "Biologically active proteins of breast milk". F Pediatrician Child Health. 2013;49 Suppl 1:1-7.
3 Savino F et al. Breast milk hormones and their protective effect on obesity. Int J Pediatric Endocrinol. 2009;2009:327505. - Savino F. et al., "What role do breast milk hormones play in protecting against obesity." Int J Pediatrician Endocrinol. 2009;2009:327505.
4 Hassiotou F, Hartmann PE. At the Dawn of a New Discovery: The Potential of Breast Milk Stem Cells. Adv Nutr . 2014;5(6):770-778. - Hassiot F, Hartmann PI, "On the threshold of a new discovery: the potential of breast milk stem cells." Adv Nutr. 2014;5(6):770-778.
Adv Nutr . 2014;5(6):770-778. - Hassiot F, Hartmann PI, "On the threshold of a new discovery: the potential of breast milk stem cells." Adv Nutr. 2014;5(6):770-778.
5 Hassiotou F et al. Maternal and infant infections stimulate a rapid leukocyte response in breastmilk. Clin Transl Immunology . - Hassiot F. et al., "Infectious diseases of the mother and child stimulate a rapid leukocyte reaction in breast milk." Clean Transl Immunology. 2013;2(4):e3.
6 Pannaraj PS et al. Association Between Breast Milk Bacterial Communities and Establishment and Development of the Infant Gut Microbiome. JAMA Pediatr. 2017;171(7):647-654. - Pannaraj P.S. et al., "Bacterial communities in breast milk and their association with the emergence and development of the neonatal gut microbiome". JAMA pediatric. 2017;171(7):647-654.
7 Bode L. Human milk oligosaccharides: every baby needs a sugar mama.Glycobiology. 2012;22(9):1147-1162. - Bode L., "Oligosaccharides in breast milk: a sweet mother for every baby." Glycobiology (Glycobiology). 2012;22(9):1147-1162.
8 Deoni SC et al. Breastfeeding and early white matter development: A cross-sectional study. neuroimage. 2013;82:77-86. - Deoni S.S. et al., Breastfeeding and early white matter development: a cross-sectional study. Neuroimaging. 2013;82:77-86.
9 Birch E et al. Breast-feeding and optimal visual development. J Pediatr Ophthalmol Strabismus. 1993;30(1):33-38. - Birch, I. et al., "Breastfeeding and Optimum Vision Development." J Pediatrician Ophthalmol Strabismus. 1993;30(1):33-38.
10 Sánchez CL et al. The possible role of human milk nucleotides as sleep inducers. Nutr Neurosci . 2009;12(1):2-8. - Sanchez S.L. et al., "Nucleotides in breast milk may help the baby fall asleep." Nutr Neurosai. 2009;12(1):2-8.
2009;12(1):2-8. - Sanchez S.L. et al., "Nucleotides in breast milk may help the baby fall asleep." Nutr Neurosai. 2009;12(1):2-8.
11 Moukarzel S, Bode L. Human Milk Oligosaccharides and the Preterm Infant: A Journey in Sickness and in Health. Clin Perinatol. 2017;44(1):193-207. - Mukarzel S., Bode L., "Breast milk oligosaccharides and the full-term baby: a path to illness and health." Klin Perinatol (Clinical perinatology). 2017;44(1):193-207.
12 Beck KL et al. Comparative Proteomics of Human and Macaque Milk Reveals Species-Specific Nutrition during Postnatal Development. J Proteome Res . 2015;14(5):2143-2157. - Beck K.L. et al., "Comparative proteomics of human and macaque milk demonstrates species-specific nutrition during postnatal development." G Proteome Res. 2015;14(5):2143-2157.
13 Michaelsen KF, Greer FR.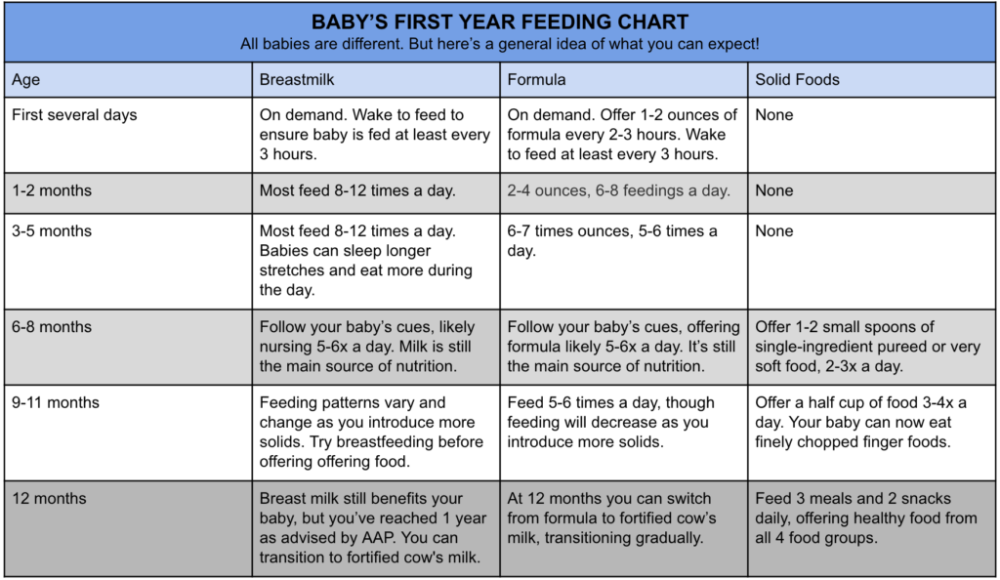 Protein needs early in life and long-term health. Am J Clin Nutr . 2014;99(3):718 S -722 S . - Mikaelsen KF, Greer FR, Protein requirements early in life and long-term health. Am J Clean Nutr. 2014;99(3):718S-722S.
Protein needs early in life and long-term health. Am J Clin Nutr . 2014;99(3):718 S -722 S . - Mikaelsen KF, Greer FR, Protein requirements early in life and long-term health. Am J Clean Nutr. 2014;99(3):718S-722S.
14 Howie PW et al. Positive effect of breastfeeding against infection. BMJ .1990;300(6716):11-16. — Howie PW, "Breastfeeding as a defense against infectious diseases." BMJ. 1990;300(6716):11-16.
15 Duijts L et al. Prolonged and exclusive breastfeeding reduces the risk of infectious diseases in infancy. Pediatrics , 2010;126(1): e 18-25. - Duitz L. et al., "Prolonged exclusive breastfeeding reduces the risk of infectious diseases in the first year of life." Pediatrix (Pediatrics). 2010;126(1):e18-25.
16 Ladomenou F et al. Protective effect of exclusive breastfeeding against infections during infancy: a prospective study. Arch Dis Child . 2010;95(12):1004-1008. - Ladomenu, F. et al., "The effect of exclusive breastfeeding on infection protection in infancy: a prospective study." Arch Dis Child. 2010;95(12):1004-1008.
Protective effect of exclusive breastfeeding against infections during infancy: a prospective study. Arch Dis Child . 2010;95(12):1004-1008. - Ladomenu, F. et al., "The effect of exclusive breastfeeding on infection protection in infancy: a prospective study." Arch Dis Child. 2010;95(12):1004-1008.
17 Vennemann MM et al. Does breastfeeding reduce the risk of sudden infant death syndrome?. Pediatrics . 2009;123(3): e 406- e 410. - Wennemann M.M. et al., "Does Breastfeeding Reduce the Risk of Sudden Infant Death?" Pediatrix (Pediatrics). 2009;123(3):e406-e410.
18 Straub N et al. Economic impact of breast-feeding-associated improvements of childhood cognitive development, based on data from the ALSPAC. Br J Nutr . 2016;1-6. - Straub N. et al., "Economic Impact of Breastfeeding-Associated Child Cognitive Development (ALSPAC)". Br J Nutr . 2016;1-6.
et al., "Economic Impact of Breastfeeding-Associated Child Cognitive Development (ALSPAC)". Br J Nutr . 2016;1-6.
19 Heikkilä K et al. Breast feeding and child behavior in the Millennium Cohort Study. Arch Dis Child . 2011;96(7):635-642 - Heikkila K. et al., Breastfeeding and Child Behavior in a Millennial Cohort Study. Arch Dis Child. 2011;96(7):635-642.
20 Singhal A et al. Infant nutrition and stereoacuity at age 4–6 y. Am J Clin Nutr , 2007;85(1):152-159. - Singhal A. et al., Nutrition in infancy and stereoscopic visual acuity at 4-6 years of age. Am F Clean Nutr. 2007;85(1):152-159.
21 Peres KG et al. Effect of breastfeeding on malocclusions: a systematic review and meta - analysis. Acta Paediatr . 2015;104(467):54-61. - Perez K.G. et al., "The impact of breastfeeding on malocclusion: a systematic review and meta-analysis". Akta Pediatr. 2015;104(S467):54-61.
Acta Paediatr . 2015;104(467):54-61. - Perez K.G. et al., "The impact of breastfeeding on malocclusion: a systematic review and meta-analysis". Akta Pediatr. 2015;104(S467):54-61.
22 Horta B et al. Long - term consequences of breastfeeding on cholesterol, obesity, systolic blood pressure and type 2 diabetes: a systematic review and meta - analysis. Acta Paediatr . 2015;104(467):30-37. - Horta B.L. et al., "Long-term effects of breastfeeding and their impact on cholesterol, obesity, systolic blood pressure, and type 2 diabetes: a systematic review and meta-analysis." Akta Pediatr. 2015;104(S467):30-37.
23 Lund-Blix NA. Infant feeding in relation to islet autoimmunity and type 1 diabetes in genetically susceptible children: the MIDIA Study. Diabetes Care . 2015;38(2):257-263. - Lund-Blix N.A. et al., "Breastfeeding in the context of isolated autoimmunity and type 1 diabetes in genetically predisposed children: the MIDIA study ". Diabitis Care. 2015;38(2):257-263.
- Lund-Blix N.A. et al., "Breastfeeding in the context of isolated autoimmunity and type 1 diabetes in genetically predisposed children: the MIDIA study ". Diabitis Care. 2015;38(2):257-263.
24 Amitay EL, Keinan-Boker L. Breastfeeding and Childhood Leukemia Incidence: A Meta-analysis and Systematic Review. JAMA Pediatr . 2015;169(6): e 151025. - Amitai I.L., Keinan-Boker L., "Breastfeeding and incidence of childhood leukemia: a meta-analysis and systematic review." JAMA Pediatrician. 2015;169(6):e151025.
25 Bener A et al. Does continued breastfeeding reduce the risk for childhood leukemia and lymphomas? Minerva Pediatr. 2008;60(2):155-161. - Bener A. et al., "Does long-term breastfeeding reduce the risk of leukemia and lymphoma in a child?". Minerva Pediatric. 2008;60(2):155-161.
26 Dewey KG. Energy and protein requirements during lactation. Annu Rev Nutr . 1997;17:19-36. - Dewey K. J., "Energy and Protein Requirements During Lactation". Anna Rev Nutr. 1997 Jul;17(1):19-36.
Energy and protein requirements during lactation. Annu Rev Nutr . 1997;17:19-36. - Dewey K. J., "Energy and Protein Requirements During Lactation". Anna Rev Nutr. 1997 Jul;17(1):19-36.
27 Victoria CG et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet. 2016;387(10017):475-490. - Victor S.J. et al., Breastfeeding in the 21st century: epidemiology, mechanisms and long-term effects. Lancet (Lancet). 2016;387(10017):475-490.
28 Jordan SJ et al. Breastfeeding and Endometrial Cancer Risk: An Analysis From the Epidemiology of Endometrial Cancer Consortium. Obstet Gynecol . 2017;129(6):1059-1067. — Jordan S.J. et al., "Breastfeeding and the risk of endometrial cancer: an analysis of epidemiological data from the Endometrial Cancer Consortium". Obstet Ginecol (Obstetrics and Gynecology). 2017;129(6):1059-1067.
2017;129(6):1059-1067.
29 Li DP et al. Breastfeeding and ovarian cancer risk: a systematic review and meta-analysis of 40 epidemiological studies. Asian Pac J Cancer Prev . 2014;15(12):4829-4837. - Lee D.P. et al., "Breastfeeding and the risk of ovarian cancer: a systematic review and meta-analysis of 40 epidemiological studies." Asia Pas G Cancer Prev. 2014;15(12):4829-4837.
30 Peters SAE et al. Breastfeeding and the Risk of Maternal Cardiovascular Disease: A Prospective Study of 300,000 Chinese Women. J Am Heart Assoc . 2017;6(6). - Peters S.A. et al., "Breastfeeding and Maternal Risk of Cardiovascular Disease: A Prospective Study of 300,000 Chinese Women". J Am Hart Assoc. 2017;6(6):e006081.
31 U.S. Department of Health & Human Services [Internet]. Surgeon General Breastfeeding factsheet ; 2011 Jan 20 — Department of Health and Human Services [Internet], Breastfeeding Facts from the Chief Medical Officer, January 20, 2011 [cited April 4, 2018]
Surgeon General Breastfeeding factsheet ; 2011 Jan 20 — Department of Health and Human Services [Internet], Breastfeeding Facts from the Chief Medical Officer, January 20, 2011 [cited April 4, 2018]
32 Doan T et al. Breast-feeding increases sleep duration of new parents. J Perinat Neonatal Nurs . 2007;21(3):200-206. - Dawn T. et al., "Breastfeeding increases parental sleep duration." G Perinat Neonatal Nurs. 2007;21(3):200-206.
33 Menella JA et al. Prenatal and postnatal flavor learning by human infants. Pediatrics . 2001;107(6): E 88. - Menella J.A. et al., Prenatal and Postnatal Taste and Smell Recognition in Children. Pediatrix (Pediatrics). 2001;107(6):e88.
34 Forestell CA, Mennella JA. Early determinants of fruit and vegetable acceptance. Pediatrics . 2007;120(6):1247-1254. - Forestell S.A., Mennella J.A., "The First Signs of Readiness to Taste Fruits and Vegetables." Pediatrix (Pediatrics). 2007;120(6):1247-1254.
Pediatrics . 2007;120(6):1247-1254. - Forestell S.A., Mennella J.A., "The First Signs of Readiness to Taste Fruits and Vegetables." Pediatrix (Pediatrics). 2007;120(6):1247-1254.
Mixed feeding of newborns: how to organize breastfeeding
No young mother is immune from the situation when a baby will need to be transferred from exclusive breastfeeding to a mixed one. When is it necessary and how to properly organize a new regime?
Dry initial milk formula adapted by Valio Baby 1 NutriValio for feeding children from birth to 6 months Read more
Follow-up dry milk formula adapted by Valio Baby 2 NutriValio for feeding children from 6 to 12 months More
Dry milk drink "Baby milk" Valio Baby 3 NutriValio for feeding children over 12 months Read more
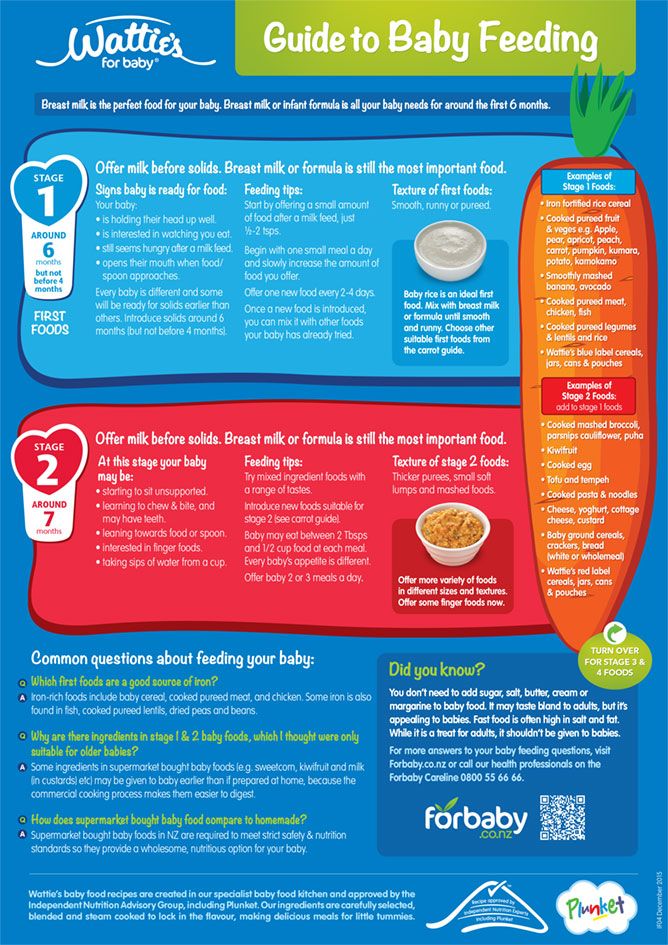
In our pediatric practice, the term "mixed feeding" refers to the combination of breast milk feeding (at least 250-200 ml) with its artificial substitutes (supplementary feeding, which is introduced if necessary up to 4 months).
First of all, it should be said that the decision to transfer the baby to mixed feeding (both breastfeeding and artificial mixture) must be made together with the pediatrician. If you decide to supplement the baby with a formula on your own, without good reason, you will only violate lactation.
As a rule, a woman is forced to introduce supplementary feeding with a mixture for one of two reasons - the baby does not have enough breast milk or the mother needs to go to work or study. And if everything is clear with the second situation without comment, then it is better to talk about the first in more detail.
Hypogalactia is a decrease in lactation. How to understand that the child does not have enough milk?
-
The infant rarely urinates (reduced daily urine volume is also called "dry diaper syndrome"). The liquid usually becomes concentrated, with a pungent odor.
-
Stool - rare or atypical (too liquid or thick, discolored).

-
The child is not gaining weight well. In the first 6 months, the baby should recover by 150-200 g per week, after six months - by 100-150 g. Of course, these are average figures, but you can focus on them.
If you notice these symptoms, then you need to take action. First of all, a woman is recommended to try all the ways to improve lactation (no matter how wonderful the mixture is, breast milk for a child is the most valuable food). If milk is still not enough, you need to introduce artificial nutrition.
There are two types of mixed feeding:
Remember that milk should remain the main food for the baby - offer the baby the breast as often as possible (this is a necessary condition for lactation to increase, because mixed feeding is often a temporary measure, and under favorable conditions, the mother can return to natural feeding).
You can feed your baby with a mixture not only from a bottle (the fact is that it is easier for a child to suck from a nipple and often babies refuse to breastfeed, realizing this). You can feed the baby from a special silicone spoon - in this case, put the mixture on the cheek, and not on the tongue. You can use a "syringe" (for example, a medicine dispenser) or a pipette. There are SNS systems - a bottle with a thin tube that is fixed on the mother's nipple. When a baby suckles, he receives both breast milk and formula. This is the ideal solution for hypogalactia as it helps to maintain close skin-to-skin contact between mother and baby, which has a beneficial effect on restoring lactation. If you are switching to mixed feeding due to the fact that you need to leave home, it is better for your assistant to accustom the child to the bottle - so the child will not smell you and reach for the breast.
You can feed the baby from a special silicone spoon - in this case, put the mixture on the cheek, and not on the tongue. You can use a "syringe" (for example, a medicine dispenser) or a pipette. There are SNS systems - a bottle with a thin tube that is fixed on the mother's nipple. When a baby suckles, he receives both breast milk and formula. This is the ideal solution for hypogalactia as it helps to maintain close skin-to-skin contact between mother and baby, which has a beneficial effect on restoring lactation. If you are switching to mixed feeding due to the fact that you need to leave home, it is better for your assistant to accustom the child to the bottle - so the child will not smell you and reach for the breast.
#PROMO_BLOCK#
For supplementary feeding, choose a high-quality, balanced mixture. Valio Baby baby food is made from the highest quality natural cow's milk and is as close as possible to the composition of breast milk. It will help the baby gain weight and strengthen the body.