Feeding your baby formula
Amount and Schedule of Baby Formula Feedings
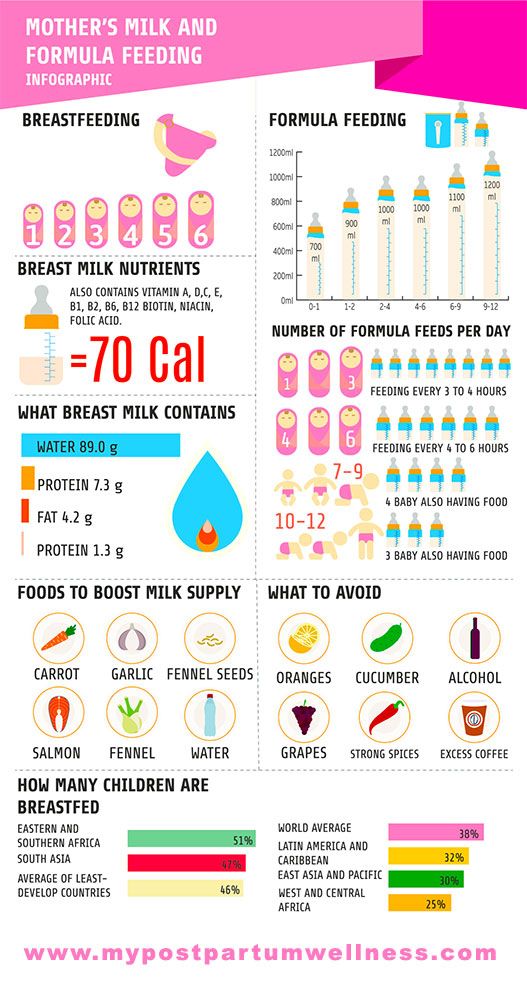
- In the first week after birth, babies should be eating no more than about 1 to 2 ounces (30 to 60 ml) per feed.
- During the first month, babies gradually eat more until they take 3 to 4 ounces (90 to 120 ml) per feed, amounting to 32 ounces per day. Formula-fed babies typically feed on a more regular schedule, such as every 3 or 4 hours. Breastfed babies usually take smaller, more frequent feedings than formula-fed infants.
If your baby sleeps longer than 4 to 5 hours during the first few weeks after birth and starts missing feedings, wake them up and offer a bottle.
By the end of the first month: Your baby will be up to at least 3 to 4 ounces (120 mL) per feeding, with a fairly predictable schedule of feedings about every 3 to 4 hours.
By 6 months: Your baby will consume 6 to 8 ounces (180–240 mL) at each of 4 or 5 feedings in 24 hours.
Formula feeding based on body weight
On average, your baby should take in about 2½ ounces (75 mL) of infant formula a day for every pound (453 g) of body weight. But they probably will regulate their intake from day to day to meet their own specific needs, so let them tell you when they've had enough. If they become fidgety or easily distracted during a feeding, they're probably finished. If they drain the bottle and continues smacking their lips, they might still be hungry.
There are high and low limits, however. If your baby consistently seems to want more or less than this, discuss it with your pediatrician. Your baby should usually drink no more than an average of about 32 ounces (960 mL) of formula in 24 hours. Some babies have higher needs for sucking and may just want to suck on a pacifier after feeding.
On-demand feeding
Initially it is best to feed your formula-fed newborn a bottle on demand, or whenever they cry with hunger.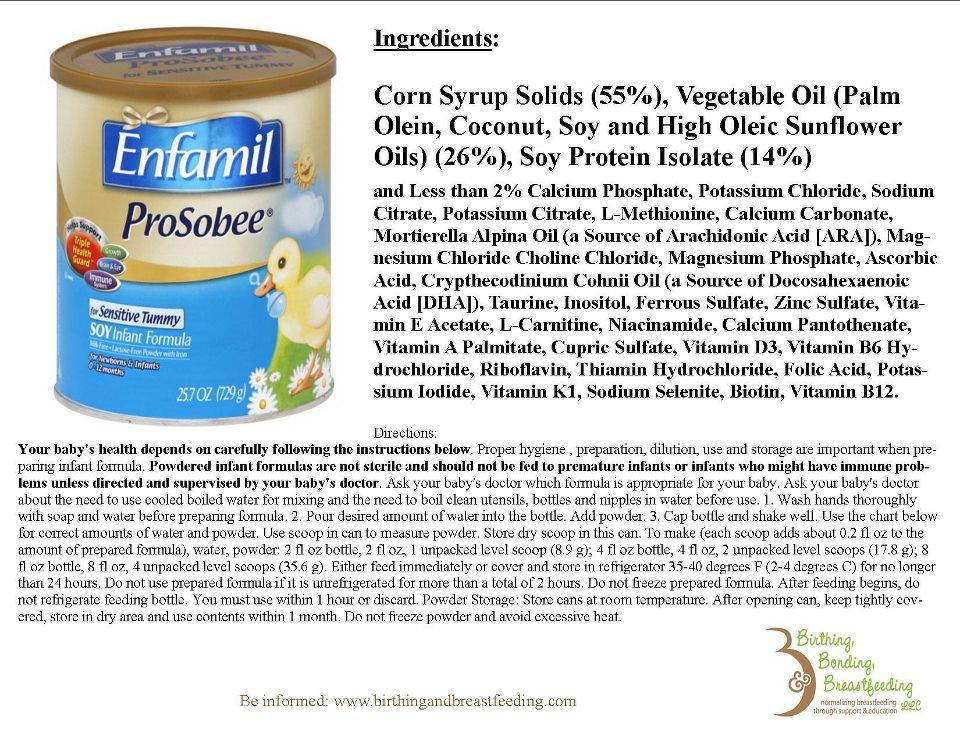 As time passes, your baby will begin to develop a fairly regular timetable of their own. As you become familiar with their signals and needs, you'll be able to schedule their feedings around their routine.
As time passes, your baby will begin to develop a fairly regular timetable of their own. As you become familiar with their signals and needs, you'll be able to schedule their feedings around their routine.
Eating & sleeping patterns
Between 2 and 4 months of age (or when the baby weighs more than 12 lb. [5.4 kg]), most formula-fed babies no longer need a middle-of-the-night feedings. They're consuming more during the day, and their sleeping patterns have become more regular (although this varies considerably from baby to baby). Their stomach capacity has increased, too, which means they may go longer between daytime feedings—occasionally up to 4 or 5 hours at a time.
If your baby still seems to feed very frequently or consume larger amounts, try distracting them with play or with a pacifier. Sometimes patterns of obesity begin during infancy, so it is important not to overfeed your baby.
Getting to know your baby's feeding needs
The most important thing to remember, whether you breastfeed or bottlefeed, is that your baby's feeding needs are unique. No book―or website―can tell you precisely how much or how often they need to be fed or exactly how you should handle them during feedings. You will discover these things for yourself as you and your baby get to know each other.
No book―or website―can tell you precisely how much or how often they need to be fed or exactly how you should handle them during feedings. You will discover these things for yourself as you and your baby get to know each other.
More information
- How Often and How Much Should Your Baby Eat?
- Making Sure Your Baby is Getting Enough Milk
- Is Your Baby Hungry or Full? Responsive Feeding Explained (Video)
- Remedies for Spitty Babies
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
Why Babies Spit Up - HealthyChildren.org
By: Alejandro Velez, MD, FAAP & Christine Waasdorp Hurtado, MD, FAAP
All babies spit up. Some babies spit up more than others, or at certain times.
Typically, babies spit up after they gulp down some air with breastmilk or formula. A baby's stomach is small and can't hold a lot, after all. Milk and air can fill it up quickly.
With a full stomach, any change in position such as bouncing or sitting up can force the flap between the esophagus (food pipe) and stomach to open. And when that flap (the esophageal sphincter) opens, that's when some of what your baby just ate can make a return appearance.
So, what can you do―if anything―to reduce the amount of your baby's spit up? How do you know if your baby's symptoms are part of a larger problem? Read on to learn more.
Common concerns parents have about spit up
My baby spits up a little after most feedings.
Possible cause: Gastroesophageal reflux (normal if mild)
Action to take: None. The spitting up will grow less frequent and stop as your baby's muscles mature—especially that flap we talked about earlier.
 It often just takes time.
It often just takes time.
My baby gulps their feedings and seems to have a lot of gas.
Possible cause: Aerophagia (swallowing more air than usual)
Action to take: Make sure your baby is positioned properly during feeds. Also be sure to burp the baby during and after feeds. Consider trying a different bottle to decrease your baby's ability to suck in air.
My baby spits up when you bounce them or play with them after meals.
My baby's spitting up has changed to vomiting with muscle contractions that occur after every feeding. The vomit shoots out with force.
I found blood in my baby's spit-up or vomit.
Possible cause: Swelling of the esophagus or stomach (esophagitis or gastritis), or another health problem that requires diagnosis and treatment.
Action to take: Call you pediatrician right away so they can examine your baby.

Remedies for spitty babies
Regardless of whether or not your baby's spit up warrants watchful waiting or medical intervention, there are some simple feeding suggestions that can help you deal with the situation at hand.
5 tips to reduce your baby's spit up
Avoid overfeeding. Like a gas tank, fill baby's stomach it too full (or too fast) and it's going to spurt right back out at you. To help reduce the likelihood of overfeeding, feed your baby smaller amounts more frequently.
Burp your baby more frequently. Extra gas in your baby's stomach has a way of stirring up trouble. As gas bubbles escape, they have an annoying tendency to bring the rest of the stomach's contents up with them. To minimize the chances of this happening, burp not only after, but also during meals.
Limit active play after meals and hold your baby upright. Pressing on a baby's belly right after eating can up the odds that anything in their stomach will be forced into action.
 While
tummy time is important for babies, postponing it for a while after meals can serve as an easy and effective avoidance technique.
While
tummy time is important for babies, postponing it for a while after meals can serve as an easy and effective avoidance technique.Consider the formula. If your baby is formula feeding, there's a possibility that their formula could be contributing to their spitting up. While some babies simply seem to fare better with one formula over another without having a true allergy or intolerance, an estimated 5% of babies are genuinely unable to handle the proteins found in milk or soy formula―a condition called Cow Milk Protein Intolerance/Allery (CMPI and CMPA). In either case, spitting up may serve as one of several cues your baby may give you that it's time to discuss alternative formulas with your pediatrician. If your baby does have a true intolerance, a 1- or 2-week trial of hypoallergenic (hydrolyzed) formula designed to be better tolerated might be recommended by your baby's provider.
If breastfeeding, consider your diet.
 Cow's milk and soy in your diet can worsen spit up in infants with Cow Milk Protein Intolerance/Allergy (CMPI and CMPA). Removing these proteins can help to reduce or eliminate spit up.
Cow's milk and soy in your diet can worsen spit up in infants with Cow Milk Protein Intolerance/Allergy (CMPI and CMPA). Removing these proteins can help to reduce or eliminate spit up.Try a little oatmeal. Giving babies cereal before 6 months is generally not recommended—with one possible exception. Babies and children with dysphagia or reflux, for example, may need their food to be thicker in order to swallow safely or reduce reflux. In response to concerns over arsenic in rice, the American Academy of Pediatrics (AAP) now recommends parents of children with these conditions use of oatmeal instead of rice cereal. See Oatmeal: The Safer Alternative for Infants & Children Who Need Thicker Food for more information.
Vomit vs. spit up: what's the difference?
There is a big difference between vomiting and spitting up:
Vomiting is the forceful throwing up of stomach contents through the mouth.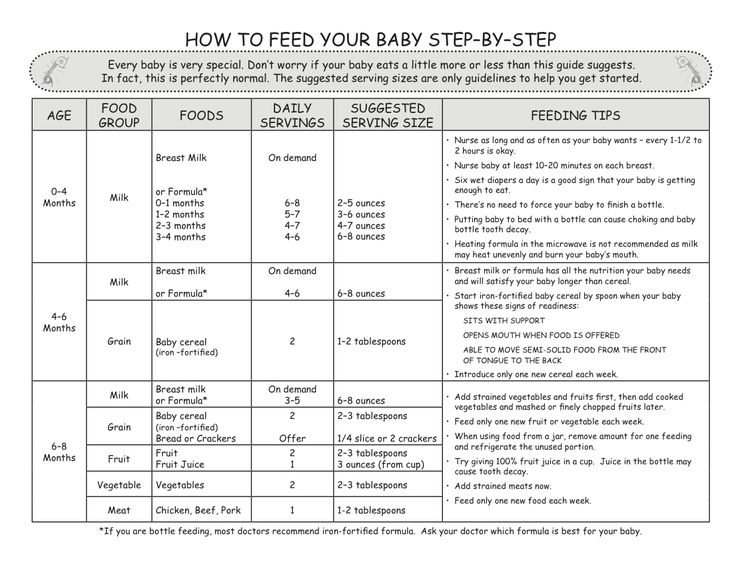 This typically involves using the abdominal muscles and is often uncomfortable, leaving you with a crying child.
This typically involves using the abdominal muscles and is often uncomfortable, leaving you with a crying child.
Spitting up is the easy flow of stomach contents out of the mouth, frequently with a burp. Spitting up doesn't involve forceful muscle contractions, brings up only small amounts of milk, and doesn't distress your baby or make them uncomfortable.
What causes vomiting?
Vomiting occurs when the abdominal muscles and diaphragm contract vigorously while the stomach is relaxed. This reflex action is triggered by the "vomiting center" in the brain after it has been stimulated by:
Nerves from the stomach and intestine when the gastrointestinal tract is either irritated or swollen by an infection or blockage (as in the stomach bug)
Chemicals in the blood such as drugs
Psychological stimuli from disturbing sights or smells
Stimuli from the middle ear (as in vomiting caused by motion sickness)
Always contact your pediatrician if your baby vomits forcefully after every feeding or if there is ever blood in your baby's vomit.
Remember
The best way to reduce spit up is to feed your baby before they get very hungry. Gently burp your baby when they take breaks during feedings. Limit active play after meals and hold your baby in an upright position for at least 20 minutes. Always closely supervise your baby during this time.
More information
- How to Keep Your Sleeping Baby Safe: AAP Policy Explained
- Gastroesophageal Reflux & Gastroesophageal Reflux Disease: Parent FAQs
-
How Much and How Often Should Your Baby Eat
About Dr. Velez
Alejandro Velez, MD, FAAP is a second-year gastroenterology fellow at Cincinnati Children’s Hospital who is interested in practicing general gastroenterology with a focus in motility and functional GI disorders, has a love for medical education at all levels, and harbors a passion for supporting and uplifting those that identify as unrepresented minorities in medicine. |
About Dr. Waasdorp
Christine Waasdorp Hurtado, MD, MSCS, FAAP is a member of the American Academy of Pediatrics and the North American Society of Pediatric Gastroenterology Hepatology and Nutrition. She is an Associate Professor of Pediatrics at the University of Colorado School of Medicine and practices in Colorado Springs. |
The information contained on this Web site should not be used as a substitute for the medical care and advice of your pediatrician. There may be variations in treatment that your pediatrician may recommend based on individual facts and circumstances.
Feeding baby formula
All parents dream that their child grows and develops correctly and harmoniously. However, the formation of a child's body largely depends on balanced nutrition that the baby receives from the first days of life.
Dry milk drink "Baby milk" Valio Baby 3 NutriValio for feeding children over 12 months Read more
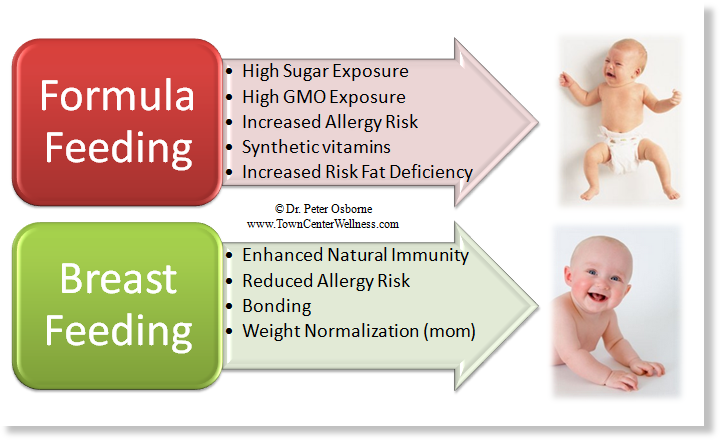
Of course, the best food for a baby is mother's milk, because it gives the child a lot of useful and necessary substances for growth and development. The quality of a child's nutrition in early childhood largely determines the state of his health in adulthood. In addition, nutrition is important in the development of the child's central nervous system and affects his intelligence and abilities. nine0003
The quality of a child's nutrition in early childhood largely determines the state of his health in adulthood. In addition, nutrition is important in the development of the child's central nervous system and affects his intelligence and abilities. nine0003
If the child is artificially fed, it is all the more important to consciously approach the issue of his nutrition, carefully choosing the right mixture. Carefully monitor the feeding regime and introduce complementary foods in a timely manner. It is in the power of parents to provide the baby with health for many years.
#PROMO_BLOCK#
It is important to follow a few rules, always remembering that when choosing a diet, consultation with a doctor is required! nine0003
1. Give preference only to adapted mixtures, since in their composition they are as close as possible to the composition of breast milk.
2. Take into account the individual characteristics of the body and the state of health of the baby.
3. Take into account the age of the child and select mixtures of the appropriate stage - initial and subsequent. To make it easier for parents to navigate, the formulas are labeled with numbers: 1 (0–6 months), 2 (6–12 months), 3 (from 12 months). The initial (starter) mixture is indicated by the number 1 and is intended for children in the first six months of life. Subsequent formulas have the numbers 2 and 3 on the packaging. They are intended for older babies from 6 months. It is important to remember that in mixtures for each stage, the composition formula changes, taking into account the age-related characteristics of development and the needs of children. nine0003
4. Observe the dosage in accordance with the instructions on the packaging. Deviation from these norms can adversely affect the well-being and health of the child. If you take too much dry matter, the mixture will come out with an increased content of nutrients, which can lead to more frequent regurgitation, unstable stools and excessive stress on the kidneys and intestines. If you take the powder less than the specified norm, then the mixture will turn out to be low-calorie and insufficiently nutritious - the baby will remain hungry. nine0003
If you take the powder less than the specified norm, then the mixture will turn out to be low-calorie and insufficiently nutritious - the baby will remain hungry. nine0003
5. Use specially prepared water to dilute the mixture. Only clean and boiled water should be used.
With artificial feeding, it is impossible to abruptly transfer the baby to a qualitatively new food and without the need to change the mixture. It is very important to properly control the amount of feeding. For each age, the daily volume is calculated, which is divided by the number of doses. This is done so that the actual volumes eaten by the baby do not exceed the calculated recommended norms. To calculate the amount of feeding for the baby yourself, you should rely on the following data. nine0003
- For a child in the first days of life, the volume of feedings (day and night) per day should be 1/5 of the child's body weight. Approximately 600-900
- In the first 2 months, the volume of feeding per day should not exceed 1/5-1/6 of the child's body weight.
 For example, if a child weighs 4 kilograms, then he should eat no more than 800 g of the mixture per day.
For example, if a child weighs 4 kilograms, then he should eat no more than 800 g of the mixture per day. - For a 2-4 month old baby, the daily formula is 1/6 of body weight (800-1000 g) nine0027 For a 4-6 month old baby, the maximum daily amount of formula should be 1/7 of body weight (900-1000 g).
- After six months and up to 9 months, the baby should eat within the daily volume of the mixture not exceeding 1/8 of his body weight (1000-1100 g).
- At the age of 9–12 months, the daily volume of milk formula is already 1/9 of the child's body weight (1100–1200 g).
To calculate the volume of each feeding, it is necessary to divide the calculated daily volume of milk formula by the optimal number of feedings. With artificial feeding of children in the first months of life, as a rule, 6-7 meals a day are recommended after 3 or 3.5 hours with a 6.5 or 6-hour break. nine0003
0-2 months - 7-10 feedings per day
2-4 months - 6-7 feedings per day
4-6 months - 5-6 feedings per day
6-12 months - 4-5 feedings per day
If a child has at least some deviations in development, a lag in weight gain, then you should definitely consult with a pediatrician to draw up a baby nutrition plan!nine0002 Most doctors and nutritionists are unanimous in their opinion that “free” (on demand) feeding is optimal for the baby.
 To meet the needs of the child, it is important for parents to listen to the child. However, when a child is bottle-fed, you should pay attention to some nuances. Already in the first days of life, babies show their individual character - one eats in moderation, the other can overeat. Therefore, when feeding with milk formulas, it is recommended to stick to the golden mean and choose a partially limited "free mode", when there are no restrictions on the time and frequency of feeding, but the volume of the mixture eaten is controlled. nine0003
To meet the needs of the child, it is important for parents to listen to the child. However, when a child is bottle-fed, you should pay attention to some nuances. Already in the first days of life, babies show their individual character - one eats in moderation, the other can overeat. Therefore, when feeding with milk formulas, it is recommended to stick to the golden mean and choose a partially limited "free mode", when there are no restrictions on the time and frequency of feeding, but the volume of the mixture eaten is controlled. nine0003 From the first days of the transition to artificial feeding, it is important to carefully monitor the reactions of the baby and record them. The best option is to keep a child's food diary, where you need to write down all the nuances associated with feeding: time, amount of food, baby's reactions after feeding. If necessary, such a diary will help you and your baby's pediatrician adjust the schedule and volume of feedings, as well as understand the possible causes of problems with nutrition and growth.
It's all about the large amount of casein, a protein that is difficult to digest and thereby increases the load on the child's digestive systems, which do not produce enough hydrochloric acid and enzymes to digest casein.
The ideal option for children from the age of one is a special baby milk or milk drink that will provide the child's body with all the necessary nutrients, helping to occur a natural transition and adaptation to the next, adult, stage of nutrition.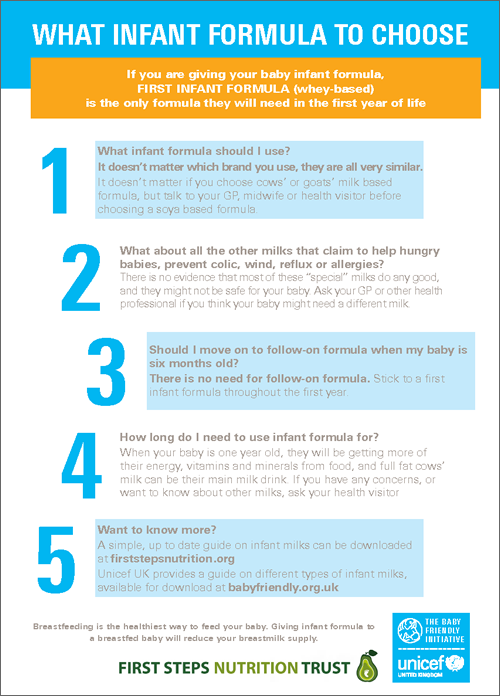 Valio specialists have developed a special baby milk Valio Baby 3, which can be used with mixed and artificial feeding. It is ideal for children from one year old, who become more mobile and active every day. You can also learn more about the correct complementary foods menu in our blog. nine0003
Valio specialists have developed a special baby milk Valio Baby 3, which can be used with mixed and artificial feeding. It is ideal for children from one year old, who become more mobile and active every day. You can also learn more about the correct complementary foods menu in our blog. nine0003
five 1
FoodShare:
Author: Reetta Tikanmäki
Palm oil in baby food
Infant milk formulas are made from cow's milk. However, in terms of fat composition, it differs significantly from that of the mother.
Read
Author: Ivargizova Oksana
How to choose milk formula for a baby
Breast milk is the best food for a newborn baby. It contains all the necessary nutritional components that fully meet the needs of the child and are necessary for his healthy and harmonious development. nine0003
Read
Show all
How to formula feed | Nutrilak
02/15/2022 Reading time: 5 min 26295 nine0003
Contents of article
- Can I formula feed my baby?
- What formula to feed the baby
- How do I choose formula for my baby?
- How long should I formula feed my baby?
The ideal food for an infant is breast milk.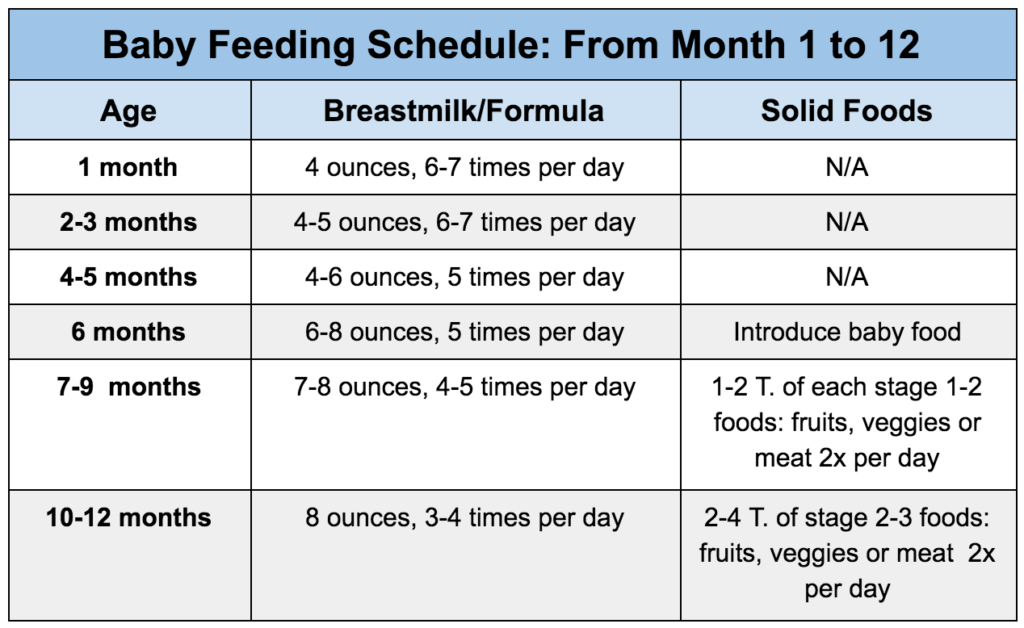 This position is voiced by the World Health Organization and shared by Russian pediatricians. But there are times when breastfeeding is impossible for objective reasons, and sometimes mothers underestimate its importance and think about whether it would not be easier to transfer the child to a formula. nine0003
This position is voiced by the World Health Organization and shared by Russian pediatricians. But there are times when breastfeeding is impossible for objective reasons, and sometimes mothers underestimate its importance and think about whether it would not be easier to transfer the child to a formula. nine0003
Can I formula feed my baby?
In cases where breastfeeding is not possible, the child is not only possible, but also necessary to be fed with mixtures. Modern adapted milk formulas for baby food are close to breast milk and contain all the necessary components for the normal growth and development of the child.
Milk formula is much better for feeding a child in the first year of life than, for example, whole cow or goat milk, liquid semolina. The baby's digestive tract is not ready for such loads, they can cause serious disturbances in the body. nine0003
If the baby is separated from the mother, if the woman is forced to take medications that are incompatible with breastfeeding, if she has diseases that make natural feeding impossible, then formula milk is a means of salvation.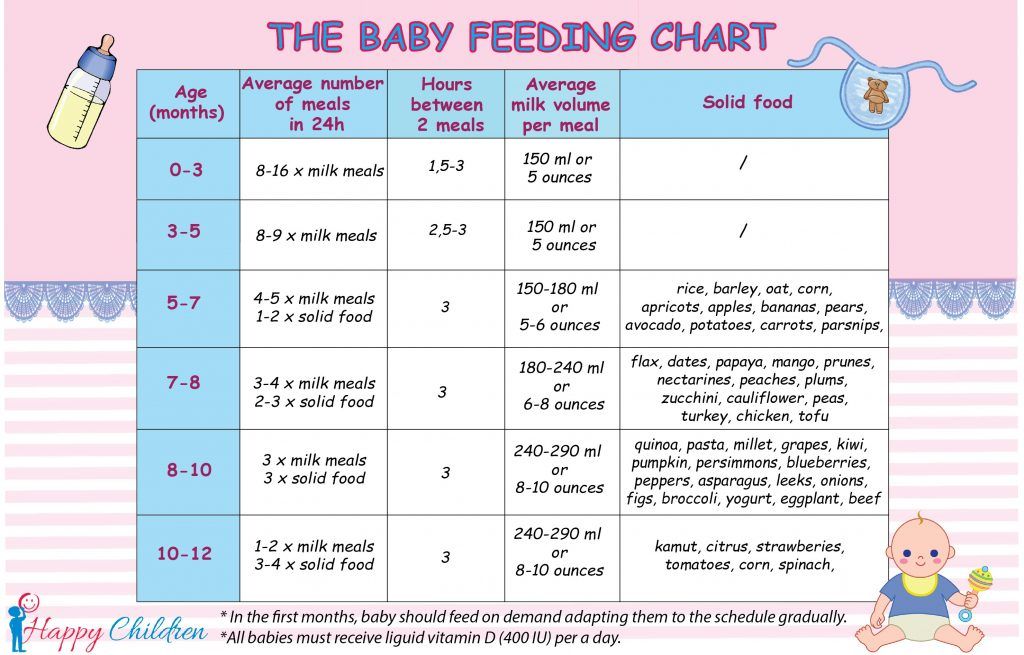 It will not only allow the child to stay alive without mother's milk, but will also give the opportunity to live a full life.
It will not only allow the child to stay alive without mother's milk, but will also give the opportunity to live a full life.
At the same time, without objective reasons, formula feeding a child is a bad decision. Although the milk formula is close in composition to breast milk, it does not reproduce it: this is not yet possible at the current level of development of science. The mixture does not adapt to the needs and condition of the baby, as it happens with breast milk. nine0003
Transferring to a mixture should be treated in the same way as taking a medicine: if there are indications for it, then artificial nutrition, like a medicine, will be for the good. If it is possible to feed the child with breast milk, then at least in the first 3-4 months after birth, one should strive to maintain breastfeeding. This is necessary for the baby's digestive system to mature and begin to produce enough enzymes, the intestines to be populated with normal microflora.
nine0002 WHO recommends exclusive breastfeeding up to 6 months, and then, combining it with complementary foods, continue to breastfeed the child up to 2 years and longer, at the request of mother and baby. Russian pediatricians recommend the introduction of complementary foods from 4 to 6 months.
Russian pediatricians recommend the introduction of complementary foods from 4 to 6 months. What formula to feed the baby
If there is a need to give the baby formula milk, you need to discuss this with the pediatrician. He will recommend what kind of mixture to feed the child, so as not to harm his digestion. nine0002 Whichever formula you use, there are general rules to follow when feeding your baby:
- Use sterile bottles and teats for feeding. After each feeding, they must be thoroughly washed and sterilized so as not to become a breeding ground for pathogenic bacteria.
- Do not store reconstituted formula, feed immediately to baby. In case of emergency (it is not possible to dilute a new portion, leave the baby with a relative who does not know how to cook baby food, etc.
- The mixture must be prepared immediately before feeding.
This is important!
The prepared mixture should be used within 2 hours.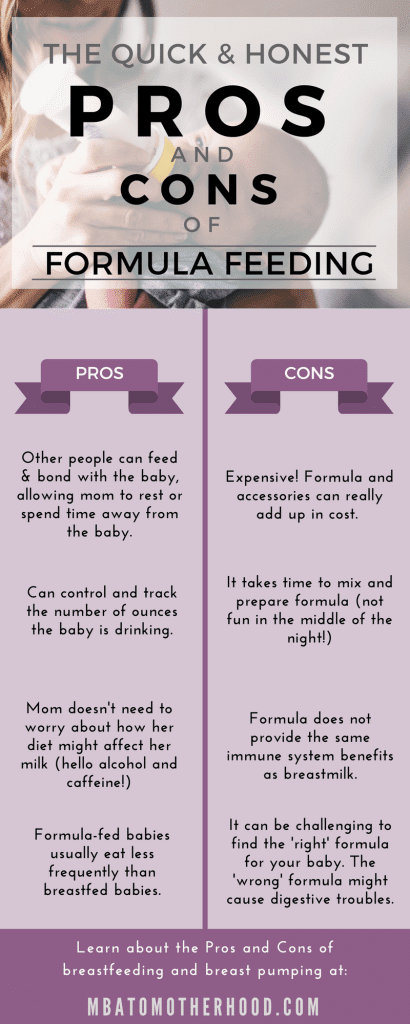 For subsequent feeding, the remains of the prepared mixture in the bottle cannot be used.
For subsequent feeding, the remains of the prepared mixture in the bottle cannot be used.
- Label the date the pack or can of formula was opened. It is necessary to use baby food from an opened package within 3 weeks. After the expiration of the period indicated on the packaging, the manufacturer does not guarantee the safety of its products. nine0028
- If it is necessary to switch the baby to another formula, do it gradually: on the first day, give a couple of teaspoons of the new formula in one feeding, then during the week increase the volume of the new formula and the number of feedings in which you will give it until you completely replace the old mixture for a new one.
- The introduction and change of the mixture is stressful for the body, so do not change the mixture without indications from the health of the child. Be sure to consult your doctor if you are concerned about any symptoms in your baby while taking the mixture. nine0028
This is important!
You can heat the finished mixture only once.
How do I choose formula for my baby?
Formula for a child should be recommended by a doctor, but you also need to understand the types of baby food in order to understand why such an appointment is made, whether options are possible and when to change the prescribed mixture.
To choose the right formula for your baby, you need to consider the following conditions:
- Child's health status. If the baby is healthy, he is prescribed a standard mixture. If he was born prematurely, his mother had a caesarean section, if he was allergic to cow's milk protein or lactose intolerance, if functional digestive disorders are expressed - regurgitation, constipation, colic - the child will need a specialized or therapeutic mixture.
- Child's age. Standard mixtures are produced under the marking 1, 2, 3, sometimes 4. These numbers show what age the mixture is designed for: 1 - for babies in the first half of the year, 2 - for children from 6 to 12 months, 3 - over a year, 4 - over one and a half years.
 nine0114
nine0114 - Mix availability. If possible, choose a brand of infant formula that you can easily buy at your nearest store or pharmacy. If a child needs a certain type of therapeutic mixture, which will be brought to you on order, nothing can be done, you will have to purchase food with a margin and replenish it in time. But if the child is healthy, then choose the food that is easier for you to purchase so that you can buy a new package at any time.
nine0027 Individual reactions of the child. Sometimes a child may react differently to mixtures of the same composition from different manufacturers. It is impossible to calculate in advance whether the mixture is suitable. Therefore, without a doctor's prescription, you should not transfer the child to another mixture, for example, goat's milk or with some additives, based only on the fact that these mixtures are more expensive, “premium”, more environmentally friendly, more popular. - Expiry date, package integrity.
 Check the expiration date of infant formula, the condition of the packaging. Do not use a mixture from damaged, dented, wet packs and cans. nine0114
Check the expiration date of infant formula, the condition of the packaging. Do not use a mixture from damaged, dented, wet packs and cans. nine0114
How long should I formula feed my baby?
During the first year of life, infant formula, like breast milk, is the main food for the baby. For children older than one year, formula, or baby milk, is an important addition to the basic diet, a source of essential vitamins and minerals. If the mixture is selected in accordance with age, then it is possible to feed a child with it up to one and a half to two years, and sometimes longer. However, the number of formula feedings at this age is reduced to 1-2 times a day, for example, as an afternoon snack or second dinner. nine0114 As for specialized and therapeutic mixtures, only the doctor determines the duration of their intake. The pediatrician will explain how to switch to special formulas correctly and how and when to leave them for standard nutrition.
List
- The baby can be formula fed if breastfeeding is not possible.