Food for baby in loose motion
When your child has diarrhea Information | Mount Sinai
Drinking Fluids
It is easy for a child with diarrhea to lose too much fluid and become dehydrated. Lost fluids need to be replaced. For most children, drinking the kinds of fluids they normally have should be enough.
Some water is OK. But too much water alone, at any age, can be harmful.
Other products, such as Pedialyte and Infalyte, may help keep a child well-hydrated. These products can be bought at the supermarket or pharmacy.
Popsicles and Jell-O can be good sources of fluids, especially if your child is vomiting. You can slowly get large amounts of fluids into children with these products.
You may also give your child watered-down fruit juice or broth.
Do not use medicines to slow down your child's diarrhea without talking to a doctor first. Ask your child's health care provider if using sports drinks is OK.
Diet for Children With Diarrhea
In many cases, you can continue feeding your child as usual. The diarrhea will normally go away in time, without any changes or treatment. But while children have diarrhea, they should:
- Eat small meals throughout the day instead of 3 big meals.
- Eat some salty foods, such as pretzels and soup.
When necessary, changes in the diet may help. No specific diet is recommended. But children often do better with bland foods. Give your child foods such as:
- Baked or broiled beef, pork, chicken, fish, or turkey
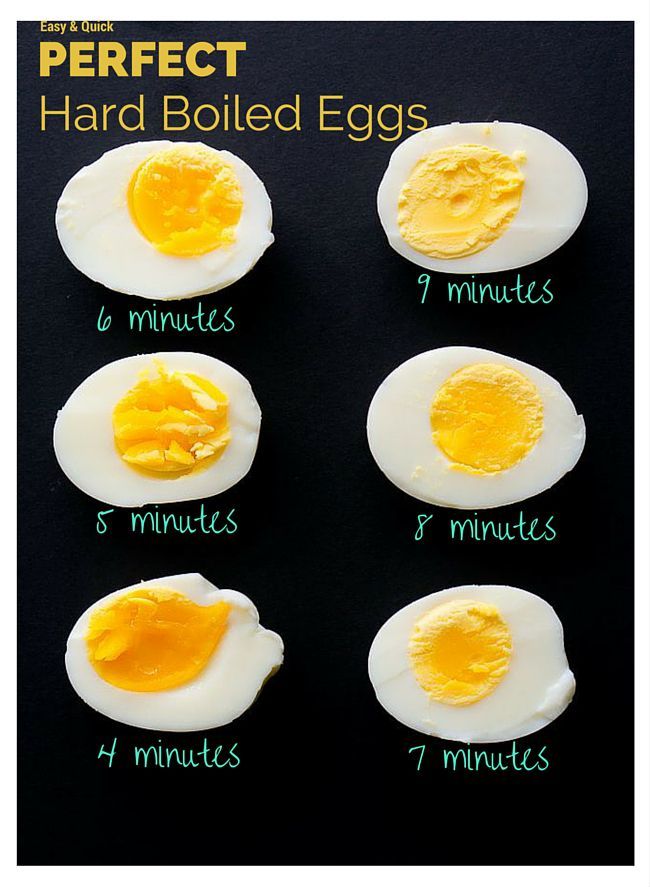
- Cooked eggs
- Bananas and other fresh fruits
- Applesauce
- Bread products made from refined, white flour
- Pasta or white rice
- Cereals such as cream of wheat, farina, oatmeal, and cornflakes
- Pancakes and waffles made with white flour
- Cornbread, prepared or served with very little honey or syrup
- Cooked vegetables, such as carrots, green beans, mushrooms, beets, asparagus tips, acorn squash, and peeled zucchini
- Some desserts and snacks, such as Jell-O, popsicles, cakes, cookies, or sherbet
- Baked potatoes
In general, removing seeds and skins from these foods is best.
Use low-fat milk, cheese, or yogurt. If dairy products are making the diarrhea worse or causing gas and bloating, your child may need to stop eating or drinking dairy products for a few days.
Children should be allowed to take their time returning to their normal eating habits. For some children, a return to their regular diet can also bring a return of diarrhea. This is often due to mild problems the gut has while absorbing regular foods.
Things Your Child Should Avoid Eating or Drinking
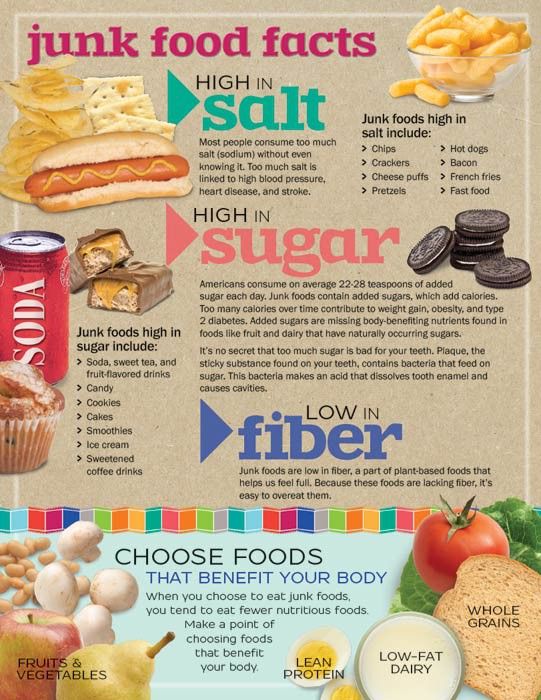
Children should avoid certain kinds of foods when they have diarrhea, including fried foods, greasy foods, processed or fast foods, pastries, donuts, and sausage.
Avoid giving children apple juice and full-strength fruit juices, as they can loosen stool.
Have your child limit or cut out milk and other dairy products if they are making diarrhea worse or causing gas and bloating.
Your child should avoid fruits and vegetables that can cause gas, such as broccoli, peppers, beans, peas, berries, prunes, chickpeas, green leafy vegetables, and corn.
Your child should also avoid caffeine and carbonated drinks at this time.
When children are ready for regular foods again, try giving them:
- Bananas
- Crackers
- Chicken
- Pasta
- Rice cereal
When to Call the Doctor
Call your child's provider if your child has any of these symptoms:
- Much less activity than normal (not sitting up at all or not looking around)
- Sunken eyes
- Dry and sticky mouth
- No tears when crying
- Not urinated for 6 hours
- Blood or mucus in the stool
- Fever that does not go away
- Stomach pain
Easter JS. Pediatric gastrointestinal disorders and dehydration. In: Bakes KM, Buchanan JA, Moreira ME, Byyny R, Pons PT, eds. Emergency Medicine Secrets. 7th ed. Philadelphia, PA: Elsevier; 2022:chap 65.
Pediatric gastrointestinal disorders and dehydration. In: Bakes KM, Buchanan JA, Moreira ME, Byyny R, Pons PT, eds. Emergency Medicine Secrets. 7th ed. Philadelphia, PA: Elsevier; 2022:chap 65.
Kotloff KL. Acute gastroenteritis in children. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics. 21st ed. Philadelphia, PA: Elsevier; 2020:chap 366.
Schiller LR, Sellin JH. Diarrhea. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 16.
Last reviewed on: 12/10/2021
Reviewed by: Neil K. Kaneshiro, MD, MHA, Clinical Professor of Pediatrics, University of Washington School of Medicine, Seattle, WA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
When your child has diarrhea: MedlinePlus Medical Encyclopedia
Diarrhea is the passage of loose or watery stools. For some children, diarrhea is mild and will go away within a few days. For others, it may last longer. It can make your child lose too much fluid (dehydrated) and feel weak.
For some children, diarrhea is mild and will go away within a few days. For others, it may last longer. It can make your child lose too much fluid (dehydrated) and feel weak.
The stomach flu is a common cause of diarrhea. Medical treatments, such as antibiotics and some cancer treatments can also cause diarrhea.
This article speaks of diarrhea in children over 1 year of age.
It is easy for a child with diarrhea to lose too much fluid and become dehydrated. Lost fluids need to be replaced. For most children, drinking the kinds of fluids they normally have should be enough.
Some water is OK. But too much water alone, at any age, can be harmful.
Other products, such as Pedialyte and Infalyte, may help keep a child well-hydrated. These products can be bought at the supermarket or pharmacy.
Popsicles and Jell-O can be good sources of fluids, especially if your child is vomiting. You can slowly get large amounts of fluids into children with these products.
You may also give your child watered-down fruit juice or broth.
Do not use medicines to slow down your child's diarrhea without talking to a doctor first. Ask your child's health care provider if using sports drinks is OK.
In many cases, you can continue feeding your child as usual. The diarrhea will normally go away in time, without any changes or treatment. But while children have diarrhea, they should:
- Eat small meals throughout the day instead of 3 big meals.
- Eat some salty foods, such as pretzels and soup.
When necessary, changes in the diet may help. No specific diet is recommended. But children often do better with bland foods. Give your child foods such as:
- Baked or broiled beef, pork, chicken, fish, or turkey
- Cooked eggs
- Bananas and other fresh fruits
- Applesauce
- Bread products made from refined, white flour
- Pasta or white rice
- Cereals such as cream of wheat, farina, oatmeal, and cornflakes
- Pancakes and waffles made with white flour
- Cornbread, prepared or served with very little honey or syrup
- Cooked vegetables, such as carrots, green beans, mushrooms, beets, asparagus tips, acorn squash, and peeled zucchini
- Some desserts and snacks, such as Jell-O, popsicles, cakes, cookies, or sherbet
- Baked potatoes
In general, removing seeds and skins from these foods is best.
Use low-fat milk, cheese, or yogurt. If dairy products are making the diarrhea worse or causing gas and bloating, your child may need to stop eating or drinking dairy products for a few days.
Children should be allowed to take their time returning to their normal eating habits. For some children, a return to their regular diet can also bring a return of diarrhea. This is often due to mild problems the gut has while absorbing regular foods.
Children should avoid certain kinds of foods when they have diarrhea, including fried foods, greasy foods, processed or fast foods, pastries, donuts, and sausage.
Avoid giving children apple juice and full-strength fruit juices, as they can loosen stool.
Have your child limit or cut out milk and other dairy products if they are making diarrhea worse or causing gas and bloating.
Your child should avoid fruits and vegetables that can cause gas, such as broccoli, peppers, beans, peas, berries, prunes, chickpeas, green leafy vegetables, and corn.
Your child should also avoid caffeine and carbonated drinks at this time.
When children are ready for regular foods again, try giving them:
- Bananas
- Crackers
- Chicken
- Pasta
- Rice cereal
Call your child's provider if your child has any of these symptoms:
- Much less activity than normal (not sitting up at all or not looking around)
- Sunken eyes
- Dry and sticky mouth
- No tears when crying
- Not urinated for 6 hours
- Blood or mucus in the stool
- Fever that does not go away
- Stomach pain
Easter JS. Pediatric gastrointestinal disorders and dehydration. In: Bakes KM, Buchanan JA, Moreira ME, Byyny R, Pons PT, eds. Emergency Medicine Secrets. 7th ed. Philadelphia, PA: Elsevier; 2022:chap 65.
Kotloff KL. Acute gastroenteritis in children. In: Kliegman RM, St. Geme JW, Blum NJ, Shah SS, Tasker RC, Wilson KM, eds. Nelson Textbook of Pediatrics.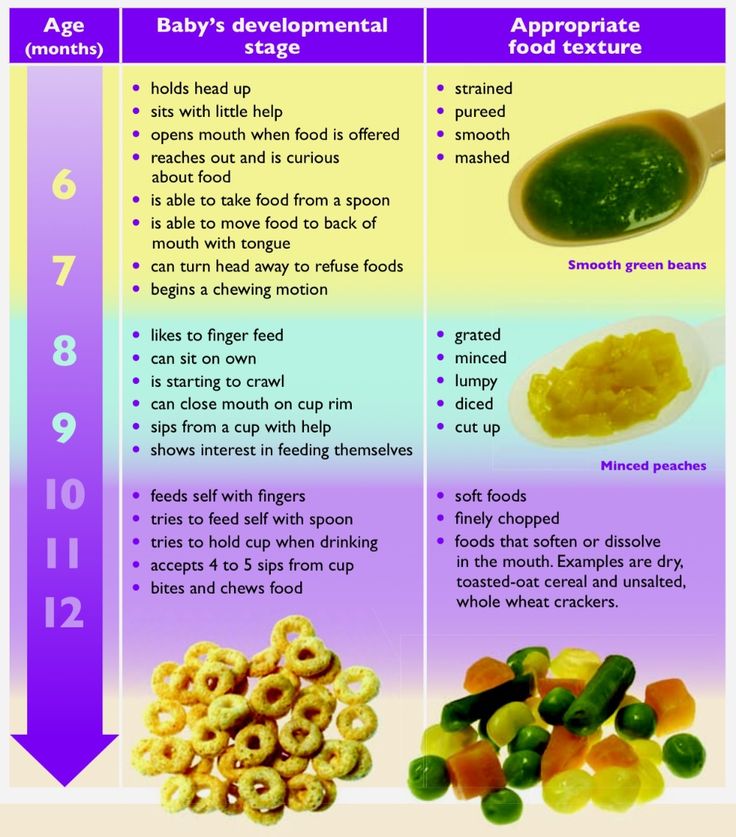 21st ed. Philadelphia, PA: Elsevier; 2020:chap 366.
21st ed. Philadelphia, PA: Elsevier; 2020:chap 366.
Schiller LR, Sellin JH. Diarrhea. In: Feldman M, Friedman LS, Brandt LJ, eds. Sleisenger and Fordtran's Gastrointestinal and Liver Disease. 11th ed. Philadelphia, PA: Elsevier; 2021:chap 16.
Updated by: Neil K. Kaneshiro, MD, MHA, Clinical Professor of Pediatrics, University of Washington School of Medicine, Seattle, WA. Also reviewed by David Zieve, MD, MHA, Medical Director, Brenda Conaway, Editorial Director, and the A.D.A.M. Editorial team.
Browse the Encyclopedia
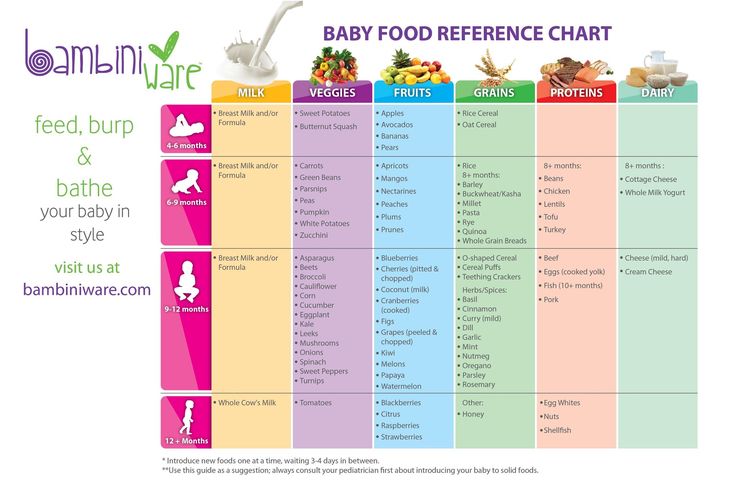
Proper nutrition of the baby in the first year of life
Let's talk about proper nutrition of the baby in the first year of life. Conventionally, it is divided into stages - the first and second half of the year. For four to six months, the child receives only mother's milk, in the second half of the year he gets acquainted with complementary foods.
Choose foods for the first feeding
Feeding the baby in the first year with breast milk
After birth, the only food for which the tiny body is ready is mother's milk. An important component of the proper nutrition of the baby in the first year is attachment to the mother's breast immediately after birth. The baby receives colostrum - a valuable and highly nutritious product. And for the female body, early application helps to establish the process of milk production. On the 3rd–5th day, transitional milk appears, and by the 2nd–3rd week, the milk becomes mature. nine0003
An important component of the proper nutrition of the baby in the first year is attachment to the mother's breast immediately after birth. The baby receives colostrum - a valuable and highly nutritious product. And for the female body, early application helps to establish the process of milk production. On the 3rd–5th day, transitional milk appears, and by the 2nd–3rd week, the milk becomes mature. nine0003
With the natural nutrition of the baby, the frequency of attachments to the breast is not limited and is determined only by the needs of the child. This is especially important in the first 2-3 months of life. As the child grows and the volume of lactation increases, the number of feedings decreases from 10–15 in the first days and weeks of life to 5–7 times a day in subsequent periods. The transition from free feeding to regime feeding is individual and ranges from 10–15 days to 1.5 months. But even in the future, some “flexibility” is assumed depending on the state of lactation on a particular day, physical activity and the state of health of the child. nine0003
nine0003
Important!
The average duration of one feeding should be 20-30 minutes.
Transfer from free feeding to regime feeding is a mandatory process. Unreasonably frequent attachment of the baby to the breast, exceeding its physiological needs, can lead to overfeeding of the child and the development of obesity.
Mother's milk is not excluded from the baby's diet even after the introduction of complementary foods. Moreover, it still remains the main food of the child. Mother's milk should be present in the baby's nutrition not only in the first year, but also in the subsequent, up to about 1.5 years. WHO experts recommend breastfeeding up to 2 years. After one year of age, the number of applications is reduced to 1-3 times a day. nine0003
Important!
Crying is not always a sign of a child's hunger. Objective signs of hunger, in addition to loud persistent crying, are rotational movements of the head in search of the mother's breasts, active sucking movements of the lips and smacking.
A baby's nutritional intake in the first year of life is directly related to age. The average amount of milk per day in the first ten days of life ranges from 70–80 ml (on the first day) to 700–800 ml (on the tenth day of life). The volume of daily nutrition until the tenth day of life is calculated by the formula: a day of life multiplied by 70–80 ml. Further, caloric or volumetric methods are used. nine0003
From the tenth day of life to two months, the amount of food per day is 1/5 of the child's body weight. At the age of one month, a child receives an average of 800 ml of milk, i.e. when applied to the breast 7 times a day, the volume of each feeding will be 110 ml of milk. In the first year of life, a child should not receive more than 1000–1100 ml of food per day.
Signs of sufficient nutrition and quantity of milk are:
- First of all, the behavior of the child. After feeding, he calmly releases the breast, falls asleep, has a good sleep until the next feeding.
 nine0032
nine0032 - Adequate weight gain and other indicators (length, head circumference) in accordance with age norms.
- Normal skin condition, turgor (tissue elasticity).
- Sufficient urination (at least 7 per day).
Feeding the baby in the first year of life with complementary foods
Four to six months pass, and mother's milk can no longer satisfy the needs of the baby, because he grows and develops so quickly. This means that the time has come to introduce the child to new products. In addition, complementary foods in the baby's diet in the first year help the baby learn to chew, so it has a dense structure and is given from a spoon. nine0003
To understand whether it is time for complementary foods, parents can focus on the following signs:
- the child looks into his mother's plate with interest, eagerly follows an adult eating;
- babies are able to sit in a highchair without falling to the sides;
- the baby is no longer enough of the previous food, he has to be fed more often, and he eats much more than before.

It must be remembered that complementary foods in the baby's diet in the first year do not aim to feed the child to satiety, because he still receives mother's milk. It is necessary to introduce the baby to new tastes, replenish the missing nutrients and teach him to swallow solid food. Therefore, you should not be very upset if in the first months after the introduction of complementary foods, the baby eats quite a bit of vegetable or meat puree or porridge. nine0003
Important!
WHO recommends starting complementary foods at 6 months. A specialist will help to clarify the time of introduction of complementary foods.
In the nutrition of children in the first year, experts recommend using only industrial products. They have a guaranteed composition that provides for the age-related needs of the baby, raw materials of excellent quality and the required degree of grinding.
With proper nutrition, the following complementary foods are introduced into the baby's diet in the first year: porridge, vegetable, fruit and meat purees and juices. What kind of products to give the baby, their order and time of introduction of complementary foods - all this will be determined by the specialist. nine0003
What kind of products to give the baby, their order and time of introduction of complementary foods - all this will be determined by the specialist. nine0003
Important!
To maintain breast milk production after feeding with complementary foods, you need to attach the baby to the breast.
With proper nutrition of the baby in the first year, the consistency of food gradually changes. Until about seven to eight months, food is given semi-liquid, by nine to ten months the consistency becomes thicker, and by the year the child is already able to chew small lumps of food, he develops a chewing skill, the first chewing teeth appear. nine0003
Proper nutrition of the baby in the first year will determine the culture of food consumption for many years to come. Balanced, age-appropriate feeding of a child will lay the foundations for lifelong health.
Breastfeeding and its benefits for the normal development of the infant.

Mother's milk is a natural biological product that provides physiologically adequate nutrition for babies. This is the "gold standard" of early childhood nutrition, and far from all aspects of its multifaceted influence have been studied. nine0003
When breastfeeding, a mother can follow different dietary patterns for her baby. Free feeding, or "on demand" feeding, is the diet of a child of the first year of life, when the mother puts the child to the breast as many times and at the time as the child requires, including at night. The duration of feeding is also determined by the child. It is more often carried out in the first months of life and with exclusive breastfeeding. Regulated feeding is such a diet of a child when feedings are carried out at more or less fixed hours, the frequency and volume of feedings is recommended by the doctor, taking into account the age, body weight, appetite and individual characteristics of the child. It is more often carried out after 1-2 months of life, especially with the option of mixed feeding. The duration of feeding of newborns ranges from 20 to 30 minutes, and for children older than 1 month - from 10 to 20 minutes. The water requirement of children in the first months of life is satisfied by breast milk with a sufficient level of lactation, so they do not need additional drinking. nine0003
The duration of feeding of newborns ranges from 20 to 30 minutes, and for children older than 1 month - from 10 to 20 minutes. The water requirement of children in the first months of life is satisfied by breast milk with a sufficient level of lactation, so they do not need additional drinking. nine0003
The criteria for a sufficient level of lactation are normal daily diuresis (600-700 ml), weight gain adequate to the age of the child and psychomotor development. If you suspect a lack of milk, you should determine the daily volume of lactation using control weighing and compare it with the calculated one, take measures to restore lactation or introduce supplementary feeding.
Breast milk is the most complex biologically active substance with unique properties:
- regulation of the processes of growth, development and differentiation of tissues;
- anti-infective protection;
- formation of immunological tolerance to dietary antigens;
- influence on the formation of the maxillofacial skeleton, speech, hearing;
- prevention of obesity, diabetes, atherosclerosis;
- beneficial effect on mental and behavioral responses, intelligence, learning ability and social adaptation;
- reduction in the risk of cancer in the mother, contraceptive effect in the first months of lactation.
 nine0032
nine0032
Breast milk provides anti-inflammatory (antioxidants, enzymes that break down pro-inflammatory neurotransmitters, anti-inflammatory cytokines) and immunomodulatory substances (live CD4 and CD8 lymphocytes, nucleotides, IgA, cytokines IL-2, IL-10, IL-12, etc., soluble cytokine receptors). Breastfeeding and the state of the intestinal microflora play a key role in maintaining a balance in the Thh Th3, Th4 cytokine system. Thanks to the bifidogenic properties of human milk, a complete intestinal microbiota of the child is formed, innate immunity and protective mechanisms of the intestinal mucosa are activated, and the immune response matures. nine0003
Digestive system:
- One of the main advantages of women's milk is the proximity of its proteins in terms of qualitative composition to blood serum proteins. Breast milk contains mainly finely dispersed, that is, consisting of the smallest particles, albumin proteins, which are easily absorbed in the child's digestive tract.
Digestibility, absorption completeness of women's milk proteins reaches 98-99%, for cow's milk proteins this figure is much less. The main protein component of cow's milk is casein, the content of which is up to ten times higher than that in human breast milk. Casein, being a large and aggressive soluble protein, is able to penetrate the intestinal walls, forcing the child's body to produce an endogenous inflammatory mediator - histamine. What can cause both intestinal bleeding, which is fraught with the subsequent development of anemia, and various kinds of allergic reactions. nine0003
- The residence time of food in the gastrointestinal tract of the baby with natural and artificial feeding is also different. The child's stomach is freed from food after 2-3 hours with breastfeeding, and with artificial feeding - after 3-4 hours. Thus, artificial feeding puts a lot of stress on the digestive tract and on the baby's body as a whole.
- The activity of the enzyme lipase, which is responsible for the breakdown of fat in the gastrointestinal tract of the child, is much higher in human breast milk.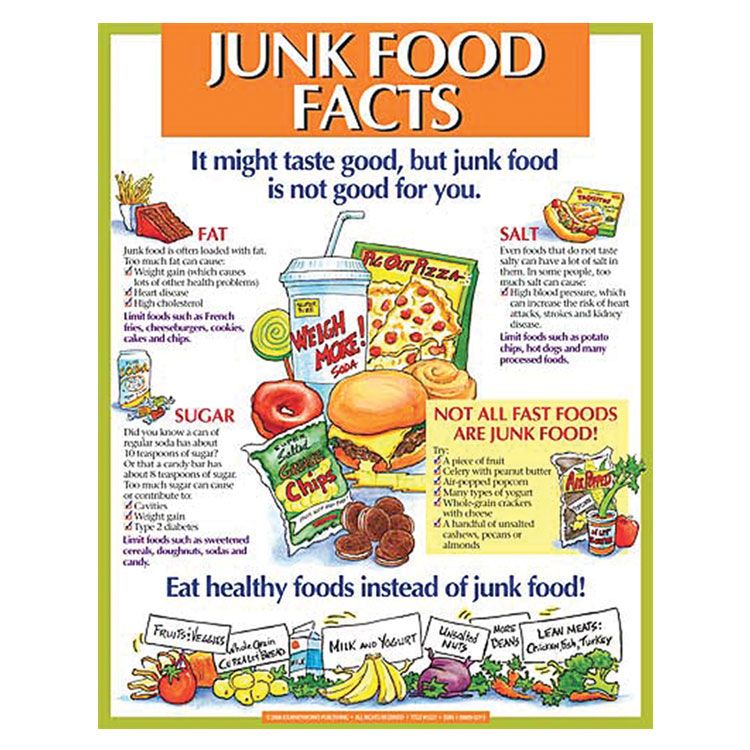 Due to the activity of maternal lipase, a high degree of fat dispersion is achieved, which facilitates their further absorption and assimilation. As a result of the action of breast milk lipase, there is a significantly lower load on the pancreas and liver of the baby, the organs responsible for the digestion of fat
Due to the activity of maternal lipase, a high degree of fat dispersion is achieved, which facilitates their further absorption and assimilation. As a result of the action of breast milk lipase, there is a significantly lower load on the pancreas and liver of the baby, the organs responsible for the digestion of fat
- Women's milk contains 5-6 times more linoleic acid. With a lack of this polyunsaturated fatty acid, a child may experience a delay in physical development, metabolism is disturbed, and adverse changes in the condition of the skin are possible.
Immune system:
- The most important advantage of mother's milk in comparison with its artificial substitutes is the presence in it of a large group of substances that protect the child's body from infections. These are secretory immunoglobulin A - sIgA, interferon, lysozyme, lactoferrin, bifidus factor, cells of the immune system. nine0003
- Immunoglobulin A is contained in secrets (fluids) on the surface of mucous membranes in contact with the external environment - lungs, nasal cavity, gastrointestinal tract, urinary tract. Maternal secretory immunoglobulin A provides protection against infection of the vital organs and systems of the child.
Maternal secretory immunoglobulin A provides protection against infection of the vital organs and systems of the child.
- Human milk lactoferrin plays an exceptional role in protecting the baby from viral infections, preventing the penetration of viral particles through the cell membrane, thus preventing infection from entering the baby's body. In addition to the antiviral action, lactoferrin also has antibacterial properties. Many microorganisms contain receptors for lactoferrin on their surface, and the binding of lactoferrin to the corresponding receptor leads to the death of a foreign bacterial cell. Lactoferrin has a bactericidal effect against a large number of gram-positive and gram-negative bacteria. nine0003
- the bifidus factor of human milk is represented by a whole complex of various sugars (oligosaccharides) and their monomers: beta-lactose, galactooligosaccharides, D-glucose, D-galactose, N-acetylglucosamines, L-fucose and sialic acids. The bifidus factor of human milk stimulates the formation of the intestinal microflora, mainly consisting of bifidobacteria (B. Bifidum) and lactobacilli. Normal intestinal microflora lines the intestinal crypts like a blanket, creating a protective layer that prevents foreign bacteria and allergens from entering the baby's circulatory system. Also, bifido- and lactobacilli create a favorable intra-intestinal environment with a shift in the pH of the contents of the colon to the acid side, which inhibits the growth of pathogenic and conditionally pathogenic bacteria and promotes the absorption of iron, calcium, vitamin D and other micro- and macroelements; participates in the synthesis of vitamins B1, B2, B3, PP, B6, B12, folic acid, biotin. In addition, the normal intestinal microflora makes the baby's immunity stronger. nine0003
At present, using the latest scientific methods, the existence of oligosaccharides containing up to 32 sugar fragments and up to 15 fructose fragments has been established. This means that the number of different types of oligosaccharides in human breast milk can reach several tens of thousands of units. Naturally, even modern artificial mixtures containing prebiotics (industrial analogues of the bifidus factor) cannot be compared in quality and variety with breast milk.
Naturally, even modern artificial mixtures containing prebiotics (industrial analogues of the bifidus factor) cannot be compared in quality and variety with breast milk.
Urinary system:
- The formation of the child's urinary system and the development of its functions takes place in the first year of life. In an infant at the time of birth, the plasma flow and the process of formation of primary urine by filtering plasma in the renal glomeruli are reduced, osmotic concentration of urine is not effective enough. The main indicators of kidney function come to the level of an adult by the beginning of the second year of life. Therefore, it is very important that the load on the kidneys, depending on the content of proteins and mineral salts in the food taken, be adequate to the physiological age of the child. nine0032
- The protein level in women's milk averages from 0.8 to 1.2 g / 100 ml, while even in the adapted ready-made milk formula this figure is 40 - 70% higher and is 1.
 4 - 1, 6 g/100 ml. The increased content of proteins increases the load on the glomerular apparatus of the kidney.
4 - 1, 6 g/100 ml. The increased content of proteins increases the load on the glomerular apparatus of the kidney. - Another problem of milk mixtures is their normalization by mineral composition. Excess salt can overload the kidneys and cause thirst, which is reflected in the addition of water to formula-fed babies. nine0032
- Many pediatricians still recommend giving babies about 100 ml of water daily to avoid dehydration. However, at present, the World Health Organization and UNICEF insist that there is no need for supplementation and the introduction of any foreign liquids and products before the child reaches the age of 6 months.
- What is the basis for these recommendations? If breastfeeding is organized correctly (the mother feeds the baby on demand, approximately every 1.5 - 2 hours, keeping night feedings), then the baby receives enough water from milk in the first six months of life. nine0032
This section describes only the main advantages of breastfeeding.
Is there any benefit from breastfeeding for the mother and does this process affect the "usual" way of life?
The benefits for the mother can be divided into three groups:
1. Health benefits
- Breastfeeding within the first hour after birth significantly reduces the risk of postpartum uterine bleeding.
- Breastfeeding maintains a high level of hormones (oxytocin and prolactin) in the blood of the mother, which contributes to the formation of strong maternal feelings. nine0032
- If a woman breastfeeds her baby exclusively, then in the first 4-6 months after childbirth, the probability of pregnancy is reduced by 95%.
- Long-term breastfeeding reduces the risk of breast cancer by 50%, and if a mother breastfeeds multiple children, breastfeeding each child reduces the risk of ovarian cancer by 25%. Also, women who breastfeed for a long time are less likely to suffer from osteoporosis.\
2. Economic benefits
- You don't need to buy breast milk, you don't need additional accessories - nipples, sterilizers, heaters, breast pumps, which you still need to run around and choose exactly those that fit the size and shape of your breasts.