Food to avoid for g6pd baby
Foods and Supplements to Choose and Avoid
G6PD deficiency is the most common inherited enzyme disorder. It’s associated with hemolytic anemia, jaundice, dark red urine, and paleness in adults and children.
People assigned male at birth are more likely to develop noticeable symptoms of G6PD deficiency. In the United States, African American males are most likely to be affected (1).
Some foods, medications, and other substances can trigger a hemolytic crisis — a rapid breakdown of red blood cells — in people with G6PD deficiency.
Most people with G6PD deficiency can manage the condition well by avoiding these triggers, and treatment is not usually necessary.
This article explains what G6PD is, the impact of G6PD deficiency, and triggers to avoid.
Glucose-6 phosphate dehydrogenase (G6PD), also called the housekeeping gene, is an enzyme that protects your red blood cells against oxidative stress and related damage (2, 3, 4, 5).
Oxidative stress results from the accumulation of harmful free radicals, which are common byproducts of metabolism, in your body (6).
G6PD is broken down via the pentose phosphate pathway — a metabolic process that creates the building blocks for DNA — and generates the antioxidant compound glutathione (2, 3, 5, 7).
Glutathione is an important antioxidant, a compound that guards your cells against damage from free radicals and oxidative stress. Research has highlighted glutathione’s role in fighting inflammation in some cancer cells (8).
Although it’s found in all your cells, G6PD is especially high in the testes and immune cells, and it helps regulate your immune system (3, 7).
Summary
G6PD is an enzyme that protects your red blood cells from damage and supports immune health by producing an antioxidant called glutathione.
G6PD deficiency occurs when your body does not have enough of the enzyme G6PD.
This is the most common genetic enzyme disorder and is typically diagnosed in childhood. An estimated 330 million individuals are affected worldwide — approximately 4. 9% of the global population (2, 5, 9, 10, 11).
9% of the global population (2, 5, 9, 10, 11).
What causes G6PD deficiency?
G6PD deficiency is an X-linked genetic disorder. This means that a gene found on the X chromosome causes it. A child can inherit G6PD deficiency from a parent through their genes (1).
To understand how X-linked disorders are passed down in families, let’s take a closer look at X and Y chromosomes.
Typically, a child has one biological parent with two X chromosomes and one biological parent with one X chromosome and one Y chromosome. A child receives an X chromosome from one parent and either an X or a Y chromosome from the other parent.
If a child receives an X chromosome containing the gene that causes G6PD deficiency, they will either be a carrier of the condition or develop it.
A child with one X and one Y chromosome (usually assigned male at birth) will develop G6PD deficiency if they receive this gene.
A child with two X chromosomes (usually assigned female at birth) may develop some level of G6PD deficiency, but it’s also possible that they will not be affected by the disorder and will be a carrier only.
Because of these factors, people assigned male at birth are more likely to receive a diagnosis of symptomatic G6PD deficiency. On average, people assigned female at birth are more likely to have the G6PD deficiency gene but less likely to develop serious symptoms (1, 12).
It’s also possible for G6PD deficiency to happen randomly. In this case, the gene causing the deficiency does not come from a parent — the genetic change happens by chance (1).
While anyone can develop G6PD deficiency, the gene is more common in certain groups. People of African, African American, Middle Eastern, Mediterranean, and Asian descent may be more likely to have the gene for G6PD deficiency (1, 5).
If you or a family member has G6PD deficiency or is a known carrier of the condition and you are thinking of having children, you can talk with your doctor or a genetic counselor. They can help you learn more about how these inheritance patterns may be relevant to you.
Also, G6PD deficiency can sometimes happen in people who do not have the gene for the condition.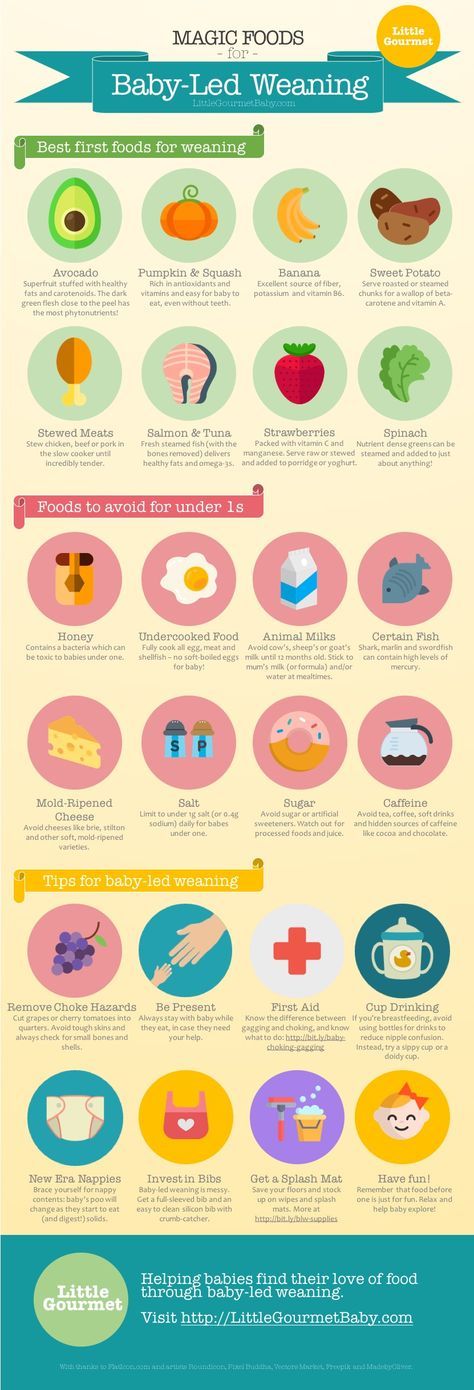 In these cases, it’s referred to as acquired G6PD deficiency. This type is caused by other conditions, such as diabetes and hyperaldosteronism (2, 13).
In these cases, it’s referred to as acquired G6PD deficiency. This type is caused by other conditions, such as diabetes and hyperaldosteronism (2, 13).
Symptoms
G6PD is necessary to replenish the antioxidant glutathione. That’s why a deficiency (lack) of the enzyme can cause immune system impairment and an increased risk of infections and non-nutritional anemia (3, 14).
G6PD deficiency is a manageable condition, and if a person is not exposed to triggers, they may never experience any symptoms. Many people with G6PD deficiency never learn they have it (1).
If triggered by certain foods, drugs, or infections, G6PD deficiency can lead to the following symptoms (2, 4, 5, 10, 15):
- yellowing of the eyes and skin (jaundice)
- dark red urine
- paleness (pallor) due to anemia
- headaches
- fatigue
- rapid heartbeat
- shortness of breath (dyspnea)
- stomach pain
When red blood cells are broken down, a yellow byproduct called bilirubin forms. During a hemolytic crisis in someone with G6PD, bilirubin levels build up above expected levels. This leads to the yellowing of the skin and eyes.
During a hemolytic crisis in someone with G6PD, bilirubin levels build up above expected levels. This leads to the yellowing of the skin and eyes.
However, most people with the deficiency remain asymptomatic (2, 4, 5, 10).
Types
There are five types of G6PD deficiency, based on the activity of the G6PD enzyme in your body (3, 5):
- Class 1: less than 10% G6PD enzyme activity with chronic hemolytic anemia, meaning that red blood cells are broken down quicker than they’re replenished
- Class 2: 10% or less G6PD enzyme activity with the breakdown of red blood cells only when you’re exposed to trigger foods, medications, or infections
- Class 3: 10%–60% G6PD enzyme activity, with symptoms appearing only in response to infections
- Class 4: more than 60% G6PD enzyme activity, with only mild symptoms
- Class 5: higher G6PD enzyme activity compared with healthy individuals; people are often asymptomatic and unaware that they have this condition
Classes 1–3 are clinically significant. This means there is a high risk of hemolytic anemia when exposed to triggers, often requiring medical intervention and treatment (3, 5).
This means there is a high risk of hemolytic anemia when exposed to triggers, often requiring medical intervention and treatment (3, 5).
Diagnosis
To diagnose G6PD deficiency, a healthcare professional will take a blood sample to determine the level of G6PD in your blood.
According to a 2009 study, a standard G6PD range for adults is 6.75–11.95 units per gram of hemoglobin. If your results are within the standard range, it typically means that you don’t have a G6PD deficiency (16).
However, results can vary based on the test used and many other factors. Your doctor will need to interpret your test results.
Qualified healthcare professionals must test for and diagnosis the condition.
Summary
G6PD deficiency is the most common genetic enzyme disorder. It can cause hemolytic anemia, jaundice, dark red urine, and paleness. There are five types, although only classes 1–3 may need medical treatment.
Specific foods and medications have been shown to trigger hemolytic anemia in those with G6PD deficiency, so you may want to avoid them if you have this condition.
Foods to avoid
Fava beans can lead to hemolytic anemia in some individuals with G6PD deficiency. In one study, 33% of participants with G6PD deficiency experienced hemolytic anemia due to eating fava beans. However, many people with this deficiency do not develop symptoms after eating fava beans (1, 10).
If you’re not sure whether fava beans are safe to include in your diet, talk with your doctor.
In a 2018 review, no other foods found in a typical U.S. diet were linked to G6PD deficiency-related symptoms (11).
One study in Egypt found links to the following legumes (10):
- falafel
- chickpeas
- broad beans
- green peas
- peanuts
- lentils
- black eyed peas
However, no other research has shown these to be trigger foods. Removing foods from your diet can lead to nutritional deficiencies, so it’s best to talk with your doctor before eliminating any foods (10, 11).
Medications to avoid
Certain medications can also trigger episodes of hemolytic anemia in those with G6PD deficiency. Some of these medications are commonly used in the United States (1, 12).
Some of these medications are commonly used in the United States (1, 12).
If you have G6PD deficiency, it’s important to talk with your doctor and pharmacist about which medications you should avoid or use with extra caution (12).
Common medications that may trigger G6PD-related hemolytic anemia include (5, 10, 12, 17):
- Acetaminophen: an analgesic (pain-relieving) drug
- Acetylsalicylic acid (aspirin): an anti-inflammatory drug
- Chloramphenicol: an antibiotic drug
- Chloroquine: an immunosuppressant and antimalarial drug
- Colchicine: a gout medication
- Diaminodiphenyl sulfone (Dapsone): an antibiotic and antimalarial drug
- Diclofenac sodium: an anti-inflammatory drug
- Diphenhydramine: an antihistamine drug
- Glyburide: a diabetes drug
- Ibuprofen: an anti-inflammatory drug
- Izoniazid: an antibiotic drug
- L-dopa: a Parkinson’s disease treatment
- Methylene blue: a dye and blood disorder treatment
- Nitrofurantoin: an antimicrobial drug
- Phenazopyridine: an analgesic drug
- Primaquine: an antimalarial drug
- Rasburicase: a gout medication
- Streptomycin: an antibiotic drug
- Sulfa drugs: a group of antibiotics that includes co-trimoxazole, sulfacetamide, and trimethoprim
- Tripelennamine: an antihistamine drug
- Vitamin K: a dietary supplement
A 2019 review also suggests caution if using herbal supplements or extracts containing Rhizoma coptidis (also called Huang Lian) or Coptis chinensis.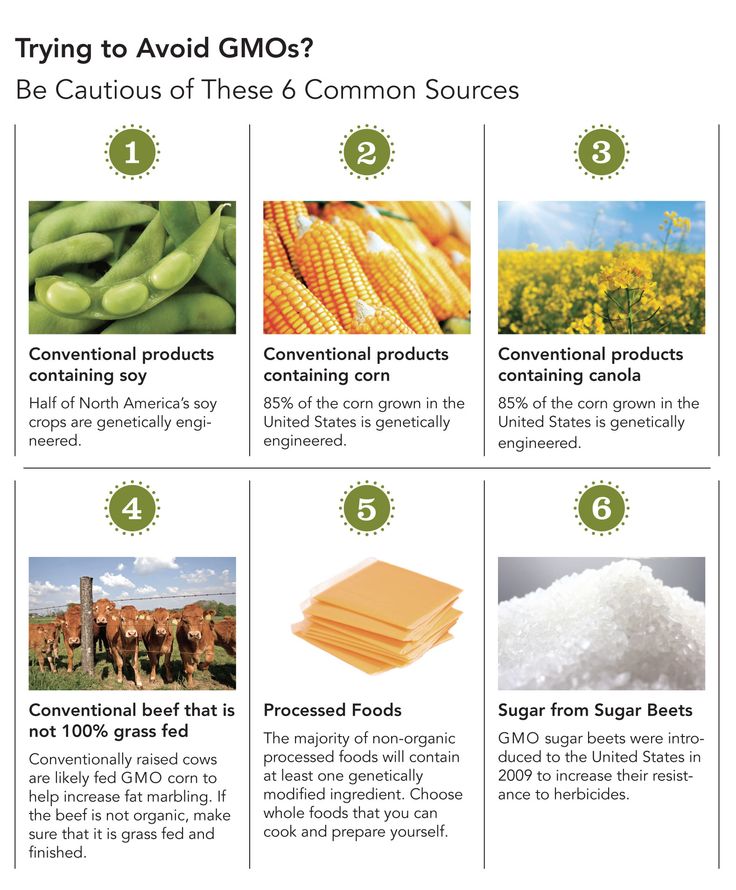 These herbs can be used to produce a supplement called berberine. Some evidence suggests that Rhizoma coptidis and Coptis chinensis may cause symptoms for those with G6PD deficiency (11).
These herbs can be used to produce a supplement called berberine. Some evidence suggests that Rhizoma coptidis and Coptis chinensis may cause symptoms for those with G6PD deficiency (11).
Substances to avoid
Substances used for tattoos and in scientific labs may also trigger G6PD symptoms. Examples include (5):
- Henna: a plant-derived dye sometimes used for decorating the body
- Naphthalene: a substance found in mothballs
- Toluidine blue: a dye used in some lab tests
Summary
Foods and substances that may trigger hemolytic anemic in people with G6PD deficiency include fava beans, some medications such as sulfa drugs, and henna.
Individuals with G6PD deficiency can enjoy a similar diet and lifestyle to those without the condition, as long as they avoid the potential triggers discussed earlier. Knowing and avoiding the triggers is the best way to prevent issues that can arise from G6PD deficiency.
There is no reliable evidence to suggest that any foods or supplements can improve the condition. As in any situation, taking good care of your general health is beneficial. Do your best to eat a healthy diet that includes a variety of nutrient-rich foods.
Some studies have looked at extracts and supplements that may affect the activity of G6PD enzymes and glutathione. However, the research on these remedies is very limited. There’s no evidence that they are safe or beneficial for people with G6PD deficiency.
One animal study examined the alcoholic extract of the Premna integrifolia Linn plant. This extract increased the concentration of glutathione and reduced markers of inflammation in rats fed a high fat diet (18).
Other studies suggest that L-cysteine — the precursor to glutathione — could help increase glutathione in G6PD-deficient cells (5, 19).
Still, more studies, particularly in humans, are needed to determine whether any supplements would benefit those with this condition.
Summary
Individuals with G6PD deficiency can maintain a standard diet and lifestyle, as long as they avoid trigger foods and substances.
The highest prevalence of hemolytic crises in G6PD deficiency is in children ages 1–3 (10).
For example, crises may present as hyperbilirubinemia — a buildup of bilirubin resulting from the breakdown of red blood cells — and severe jaundice, which may require phototherapy (5, 20).
Newborn screening for G6PD deficiency is not yet routine in the United States.
However, the American Academy of Pediatrics recommends screening jaundiced newborns who undergo phototherapy, especially if they have a family history of the deficiency or are of African, Asian, or Mediterranean descent (5).
Children with G6PD deficiency can lead a typical lifestyle, as long as they avoid any known triggers.
Here are some recommendations for caregivers of children with G6PD deficiency:
- Observe them for symptoms of jaundice or anemia and seek immediate medical treatment if symptoms appear.

- Keep mothballs and medications out of reach to avoid a hemolytic crisis.
- Avoid fava beans, unless directed otherwise by your doctor.
Summary
The highest prevalence of hemolytic crises in people with G6PD deficiency is in those ages 1–3. Avoid food, substance, and medication triggers. Seek immediate medical attention if symptoms of jaundice or anemia appear.
Exercise can induce oxidative stress, which is a trigger for hemolytic anemia in people with G6PD deficiency (5, 21).
However, studies in athletes suggest that oxidative stress brought about by exercise is not significantly higher in people with G6PD deficiency (5).
So, it’s likely safe for individuals with G6PD deficiency to use exercise to improve their quality of life (21).
Still, more studies on exercise in people with G6PD deficiency are needed.
Summary
Exercise causes oxidative stress, a potential trigger in people with G6PD deficiency.
However, studies have not shown a significant difference in oxidative stress in people with and without the condition. This suggests that people with G6PD deficiency can engage in exercise.
G6PD is an enzyme that protects your red blood cells from oxidative stress and damage.
A deficiency (lack) of this enzyme is associated with hemolytic anemia, jaundice, and dark red urine. Hemolytic crises are most prevalent in children ages 1–3.
Triggers to be avoided include certain foods, such as fava beans; some medications; and some substances, including henna.
While anyone can develop G6PD deficiency, people assigned male at birth are more likely to have symptoms of the condition.
Individuals with G6PD deficiency can continue to exercise to support their quality of life without an increased risk for hemolytic anemia.
Just one thing
Try this today: Ask a doctor about G6PD deficiency testing if you have a family history and think you may have the condition. You may request testing for your child if they have jaundice and need phototherapy; are of African, African American, Middle Eastern, Asian, or Mediterranean descent; or have a family history of the deficiency.
You may request testing for your child if they have jaundice and need phototherapy; are of African, African American, Middle Eastern, Asian, or Mediterranean descent; or have a family history of the deficiency.
G6PD Deficiency Foods To Avoid List
This G6PD Deficiency Foods To Avoid List was created to share food triggers for this genetic disorder.
What is G6PD? G6PD Deficiency (glucose 6 phosphate dehydrogenase deficiency) is a hereditary genetic disorder that can lead to problems with anemia.
G6PD Deficiency as defined by G6PD.org:
G6PD Deficiency is a hereditary abnormality in the activity of an erythrocyte (red blood cell) enzyme. This enzyme, glucose-6-phosphate dehydrogenase (G-6-PD), is essential for assuring a normal life span for red blood cells, and for oxidizing processes. This enzyme deficiency may provoke the sudden destruction of red blood cells and lead to hemolytic anemia with jaundice following the intake of fava beans, certain legumes and various drugs.

Table Of Contents:
G6PD Deficiency Foods To Avoid
For a full list of G6PD Deficiency Drugs to Avoid, you can visit this Unsafe Medications to Take list. Your medical practitioner should provide you extensive information as well.
If you or a loved one lives with the g6pd deficiency at home, then you should know about these trigger foods that can cause problems.
Here’s information on G6PD deficiency triggers according to KidsHealth.org (source):
Triggers of hemolysis in kids with G6PD deficiency include: – illness, such as bacterial and viral infections, some painkillers and fever-lowering drugs [including aspirin], some antibiotics (most often those with “sulf” in their names), Quinine and other antimalarials derived from quinine. Most antimalarial drugs with “quine” in their names, Fava beans (also called broad beans) and Naphthalene (a chemical found in mothballs and moth crystals)
For a complete and official list of g6pd foods to avoid, your doctor should provide you all the information you need. These are just some of the main foods to avoid that I’ve compiled up myself as of recently.
These are just some of the main foods to avoid that I’ve compiled up myself as of recently.
Foods To Avoid List
Legumes are one of the worst culprit trigger food groups with the broad bean or Fava Bean being the worst. So number 1 on the avoid list are, Fava Beans.
- Fava Beans (Broad Beans):
Fava or Fave Beans are one of the the worst g6pd foods to avoid. If you’re nursing a baby with this genetic condition or you yourself have it, make sure you never consume these.
Because it’s good to know, and you never know, here’s how to say Fava Beans in many other languages: (source)
- Arabic: Foolle
- Catalan: Fava
- Chinese: Tzan-Doo
- Dutch: Tuinboon
- English: Fava or Broad Bean
- Farsi (Persian): Ba-ghe-Leh
- French: Fève
- German: Favabohnen (Fava bean), Dicke Bohnen (thick bean), Saubohnen (sow bean)
- Greek: Koukia (“Fava” is an appetizer made from dried fava beans)
- Hebrew: Polle
- Hungarian: Lóbab
- Italian: Fava (pl.
 fave)
fave) - Kurdish: Paqla
- Malay: Kacang Parang
- Spanish: Haba
- Turkish: Bakla (“Fava” is an appetizer made from dried fava beans)
- Urdo (Pakistan and India): Lobhiya, Rajma, Jheam
- Thai (Thailand): two-ah pak-ah
- Legumes: Legumes in general are g6pd foods to avoid. Like fava beans/broad beans, many other legumes can bring on a hemolytic response.
Here, the Honor Society of Nursing has a good explanation of why legumes are bad for g6pdd.
Legumes and carbohydrates are the two main food groups that traditionally trigger G6PD deficiency symptoms. Legumes are plant products that include beans, peas, lentils, and soy. Fava beans in particular tend to trigger side effects. The carbohydrates that cause the most problems include white flour, refined sugars, and high fructose corn syrup, Additional food products that can cause G6PD deficiency syndromes to appear include tonic water, items that use blue food coloring, and products that contain sulfites, such as wine and dried fruits.
– STTI
- Kidney beans
- Lima beans
- Black beans
- Refried beans
- Lima beans
- Kidney beans
- Soybeans
- Alfalfa sprouts
- Peanuts
- Licorice
- Carob
- Peas
- Lentils
- Soy
- Tofu
- Bean curds
- Hummus
- Soy Beans:
- Food products with soy (a lot of packaged products have it): Miso soup, tofu, soy protein and the countless packaged foods with soy derivatives.
- Black & Green tea and their extracts
- Blueberries
There are mixed opinions on fresh blueberries and g6pd deficiency. The joy of freshly baked blueberry muffins in the morning may still be attainable. There are over 440 variants of this genetic disorder that range from mild to severe. Those with a moderate to mild type may handle blueberries without getting triggered, but in general, if playing it safe, blueberries are on the trigger foods list.
The joy of freshly baked blueberry muffins in the morning may still be attainable. There are over 440 variants of this genetic disorder that range from mild to severe. Those with a moderate to mild type may handle blueberries without getting triggered, but in general, if playing it safe, blueberries are on the trigger foods list.
- Bitter Gourd
- Garden eggs (Eggplant):
From what I can see these are the same thing as eggplants. Garden egg may refer to the smaller eggplants common to Africa, the Mediterranean and parts of Asia.
- Sulfites
Sulfites can cause hemolysis in G6PD deficient persons. Sulfite foods include very common ones like dried fruits, wine, wine vinegar, pickled foods, shrimp and even trail mix.
Many people besides those who have G6PDD have a sulfite sensitivity. The following foods taken from a WebMD list of sulfite containing foods and ingredients are good to avoid for g6pdd:
- Baked goods
- Soup mixes
- Jams
- Canned vegetables
- Pickled foods
- Gravies
- Dried fruit
- Potato chips
- Trail mix
- Beer and wine
- Vegetable juices
- Sparkling grape juice
- Apple cider
- Bottled lemon juice and lime juice
- Tea
- Many condiments
- Molasses
- Fresh or frozen shrimp
- Guacamole
- Maraschino cherries
- Dehydrated, pre-cut, or peeled potatoes
Ingredients with sulfite to look for on food labels include: (source)
- Sulfur dioxide
- Potassium bisulfite or potassium metabisulfite
- Sodium bisulfite, sodium metabisulfite, or sodium sulfite
- Menthol & Mints: chewing gum, mints, vapors, sprays, etc.

G6pd and menthol don’t pair well together. This means staying away from most toothpastes and mouthwashes. Luckily there are many great alternatives for teeth care and your dentist can refer some good menthol free products.
- Packaged meat
- Canned fish
- Margarine
- Packaged salad dressings
- Hot dogs
- Dried potatoes and potato chips
- Low fat cheese
- Sausage and other processed meats
- Sweet & sour sauce
- Worcestershire sauce
- Ascorbic acid
- Packaged Gluten Free Foods
- Tonic water
- Bitter melon
- Simple carbohydrates: corn syrup, white flour and refined sugar
- Peanut containing foods
- Vitamin K:Vitamin K3 may be tied with hemolytic anemia.

- Artificial Blue Coloring: Blue food colorings like Toluidine Blue are dangerous for those with g6pd. All artificial dyes could be g6pd deficiency triggers.
- Chinese Herbs:
Certain Chinese herbs like Rhizoma coptidis, Flos Ionicerae and Calculus Boris have been known to cause hemolytic responses in people with g6pdd. For more on Chinese herbs to avoid for g6pd deficiency, go here to see all the avoid herbs list Chinese Herbs to Avoid.
Conclusion: G6PD Deficiency Foods To Avoid
G6pd deficiency foods to avoid are just one category out of multiple that must be learned if you or someone in your family has the g6pd deficiency inheritance. It’s easy to work around any potential triggers if everyone in the household becomes knowledgeable about it.
The key to staying symptom free and not letting g6pd deficiency negatively affect you is to avoid triggers.
Exposing red blood cells to triggers leads to hemolytic anemia.
G6PD deficiency is a lifelong condition that can be very successfully managed forever. 700,000,000 have g6pd deficiency. It’s easily manageable if you know all the trigger dangers.
For a full list of medications to avoid, this list from G6PD.org is a good one available online.
As well as foods to avoid, there are many medications and household common chemicals that need to be avoided, like mothballs (naphthalene), hair dyes, henna tattoos, menthol containing cleaners, rubs and also pesticides.
If there’s a G6PD Deficiency diet, it may be a diet rich in antioxidants and healthy fats.
Simple carbohydrates are g6pd deficiency foods to avoid in themselves, so a more paleo style of eating or Mediterranean with the healthy oils and fats, minus the wines, could be good. Step one is learning all the G6pd deficiency foods to avoid. Next it seems like a good idea to learn about any successful G6PD Deficiency diets or ways of eating that have a good track record of keeping complications away.
Thanks for visiting our g6pd deficiency foods to avoid list blog post.
If you have any questions, comments, corrections or suggestions, please let us know!
UP NEXT: An article here on the site about the Carnivore Diet Plan, and its potential in helping with autoimmune conditions.
Foods and Supplements to Choose and Avoid - Drink-Drink
G6PD deficiency is the most common hereditary enzyme disorder. It is associated with hemolytic anemia, jaundice, dark red urine, and pallor in adults and children.
In particular, G6PD deficiency is predominantly found in African American men, but is also common in men of Asian and Mediterranean ancestry.
Some foods, drugs, and other substances can cause a hemolytic crisis in people with G6PD. Hemolytic crisis refers to the rapid breakdown of red blood cells.
This article explains what G6PD is, the effects of G6PD deficiency, and triggers to avoid.
What is G6PD?
Glucose-6-phosphate dehydrogenase (G6PD), also called the housekeeping gene, is an enzyme that protects red blood cells from oxidative stress and related damage.1, 2, 3, 4).
Oxidative stress refers to the accumulation of harmful free radicals in the body, which are common by-products of metabolism (5).
G6PD is cleaved through the pentose phosphate pathway—the metabolic process that creates the building blocks for DNA—to generate the antioxidant compound glutathione (1, 2, 4, 6).
Glutathione is an important antioxidant. An antioxidant is a compound that protects your cells from free radical damage and oxidative stress.
Studies have identified the role of glutathione in fighting inflammation in some cancer cells.7).
Although it is found in all your cells, G6PD is especially high in testicles and immune cells and helps regulate your immune system (2, 6).
Conclusion
G6PD is an enzyme that protects your red blood cells from damage and supports immune health by producing an antioxidant called glutathione.

What is G6PD deficiency?
G6PD deficiency is when your body does not have enough G6PD enzyme.
This is the most common genetic enzyme disorder and is usually diagnosed in childhood. It is estimated that 330 million people worldwide are affected, which is approximately 4.9% of world population.1, 4, 8, 9, 10).
It has also been observed that G6PD deficiency can develop in adulthood, termed acquired G6PD deficiency. A 2020 study found that this type is common in people with obesity and diabetes.1, 11).
Insulin resistance and elevated blood sugar due to diabetes or increased body fat have been shown to reduce G6PD enzyme activity, which is usually worse in people with G6PD deficiency.11).
It is also worth noting that gender and ethnicity appear to be risk factors for deficiency. In particular, men of African, African American, Asian, and Mediterranean descent may be at increased risk (4, 11).
symptoms
G6PD is required to replenish the antioxidant glutathione. That's why an enzyme deficiency (deficiency) can cause a compromised immune system and an increased risk of infections and non-nutritive anemia (2, 11, 12).
That's why an enzyme deficiency (deficiency) can cause a compromised immune system and an increased risk of infections and non-nutritive anemia (2, 11, 12).
G6PD deficiency caused by certain foods, drugs, or infections can lead to the following symptoms (1, 3, 4, 9, 13):
- jaundice, which is yellowing of the eyes and skin
- dark, red urine
- pallor, which is pallor due to anemia
- headaches
- fatigue
- rapid heartbeat
- shortness of breath, i.e. shortness of breath
- pain in the abdomen
yellow blood cells are formed, called biliary However, during a hemolytic crisis in a person with G6PD, bilirubin levels rise above what is expected. This leads to yellowing of the skin and eyes.
However, most people with deficiency remain asymptomatic (1, 3, 4, 9).
Select
There are five types of G6PD deficiency, depending on the activity of the G6PD enzyme in the body (2, 4):
- Grade 1: G10PD enzyme activity is less than 6% in chronic hemolytic anemia, which means that red blood cells are destroyed faster than replenished
- Grade 2: 10% or less G6PD enzyme activity with RBC destruction only when exposed to trigger foods, drugs, or infections
- Grade 3: G10PD enzyme activity is 60-6% and symptoms appear only in response to infection.
- Grade 4: G60PD enzyme activity greater than 6%, with only mild symptoms
- Grade 5: higher G6PD enzyme activity compared to healthy people, and people often do not have symptoms and do not know they have this condition
Grades 1-3 are clinically significant. This means that there is a high risk of hemolytic anemia when exposed to triggers, often requiring medical intervention and treatment.2, 4).
Diagnosis
To diagnose a G6PD deficiency, a healthcare professional will take a blood sample to determine the level of G6PD in your blood.
According to the University of Rochester Medical Center, the standard range for adults is 5.5–20.5 units per gram of hemoglobin. The standard range means you are not deficient in G6PD.
Thus, hemoglobin levels below 5.5 units per gram may indicate G6PD deficiency (14).
Testing and diagnosis should be performed under the supervision of a qualified healthcare professional.
Conclusion
G6PD deficiency is the most common genetic enzyme disorder. This can cause hemolytic anemia, jaundice, dark red urine, and pallor. There are five types, although only grades 1 through 3 may require treatment.
Foods and Substances to Avoid
Certain foods and drugs have been shown to cause hemolytic anemia in people with G6PD deficiency, so you may want to avoid them if you have the condition.
Foods to avoid
Fava beans have been shown to cause hemolytic anemia in 33% of people with G6PD deficiency.1, 4, 9, 10).
In addition, a 5-year study in 1,000 people with G6PD deficiency showed that the following foods cause hemolytic anemia in some participants (9): lentils
Drugs to avoid
Drugs are the least common cause of hemolytic anemia in patients with G6PD.
However, here are the types you should avoid if you have this condition (4, 9, 15):
- Diclofenac sodium: anti-inflammatory drug
- Ibuprofen: anti-inflammatory drug
- ): anti-inflammatory drug
- Acalifs indicates: Traditional plant medicinal drug
- Coptis Chinese: Traditional plant drug
substances that should be avoided for tattoos and can also be caused in scientific laboratories and can also be caused G6PD.
 4) Such as:
4) Such as: - Henna: a dye of plant origin, sometimes used for body decoration
- Naphthalene: found in mothballs
- Toluidine blue: dye used in some laboratory tests
Conclusion
like henna can cause hemolytic anemia in some people with G6PD and should be avoided.
Choice foods and substances
People with G6PD can enjoy the same diet and lifestyle as people without the condition, provided they avoid the potential triggers discussed earlier.
People with and without G6PD may want to focus on eating foods rich in antioxidants, which protect against oxidative damage, protect red blood cells, and support good health. Examples of foods high in antioxidants include cinnamon, ginger, passion fruit, dark chocolate, and more (16, 17, 18, 19).
Interestingly, recent studies show that there is an association between vitamin D levels, G6PD deficiency, and the severity of infections such as COVID-19. eleven).
eleven).
Glutathione, which is under-replenished in people with G6PD deficiency, is needed to maintain vitamin D levels in the body.11).
Vitamin D regulates your immune health by increasing the release of anti-inflammatory compounds (20).
Thus, individuals with G6PD deficiency are at greater risk of vitamin D deficiency and immunosuppression and benefit from increased vitamin D intake.11, 20).
Food sources rich in vitamin D include (21, 22):
- Fish: trout, salmon, sardine, fish oil
- mushrooms : UV dried shiitake.
- Sources of animal origin: beef liver, egg yolks
- Fortified drinks: Orange juice, chocolate milk
- dairy products: cow's milk, yogurt, cheese
- Lighted milk: tonsils: tonsils: tons rice milk
Alcoholic extract from Premna integrifolia Lynn medicinal plant may also benefit people with G6PD deficiency. According to animal studies, this extract increased glutathione levels and reduced inflammatory markers in rats fed a high-fat diet.23).
According to animal studies, this extract increased glutathione levels and reduced inflammatory markers in rats fed a high-fat diet.23).
Similarly, test-tube studies have shown that L-cysteine, a precursor of glutathione, can help restore glutathione in G6PD cells.4, 24).
However, more research is needed, especially in humans, to determine if any supplements will benefit those who have them. state.
Conclusion
People with G6PD deficiency can follow a standard diet and lifestyle, provided they avoid trigger foods and substances. They may also benefit from increased vitamin D intake.
Recommendations for children
The highest prevalence of hemolytic crises in people with G6PD occurs between 1 and 3 years of age.8).
For example, crises can present with hyperbilirubinemia—an accumulation of bilirubin from the breakdown of red blood cells—and severe jaundice that may require phototherapy.4, 25).
Newborn screening for G6PD deficiency is not yet routine in the United States.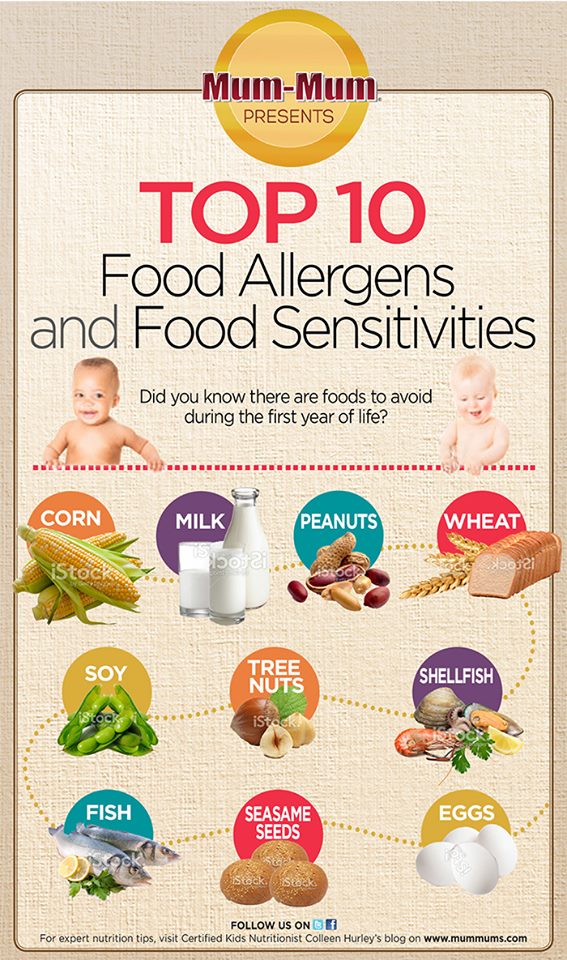
However, the American Academy of Pediatrics recommends screening for newborns with jaundice receiving phototherapy, especially if they have a family history of deficiency or are African, Asian, or Mediterranean, which increases their risk.4).
Children with G6PD deficiency can lead normal lives if they avoid any known triggers.
Here are some suggestions for children with G6PD:
- Monitor them for symptoms of jaundice or anemia and seek immediate medical attention if they appear.
- Keep mothballs and medicines out of reach to avoid hemolytic crisis.
- Avoid beans and other food triggers.
Conclusion
The highest prevalence of hemolytic crises in G6PD is observed at the age of 1 to 3 years. Avoid foods, substances, and medications that cause triggers. Seek immediate medical attention if you develop symptoms of jaundice or anemia.
Exercise and G6PD
Exercise can cause oxidative stress, which is a trigger for hemolytic anemia in people with G6PD deficiency. 4, 26).
4, 26).
However, studies in athletes show that exercise-induced oxidative stress is not significantly higher in individuals with G6PD deficiency.4).
Thus, it is likely that people with G6PD deficiency can use exercise to improve their quality of life.26).
However, more research is needed on exercise in people with G6PD deficiency.
Conclusion
Exercise causes oxidative stress, which is a potential trigger for people with G6PD. However, studies have not shown a significant difference in oxidative stress in people with and without the condition. This suggests that individuals with G6PD deficiency may be able to exercise.
Bottom line
G6PD is an enzyme that protects your red blood cells from oxidative stress and damage.
Deficiency (deficiency) of this enzyme is associated with hemolytic anemia, jaundice and red-dark urine. Hemolytic crises are most common between the ages of 1 and 3 years.
Triggers to avoid include certain foods such as beans, certain medications, and substances including henna.
A high intake of vitamin D is recommended for people with this condition. This may help improve immune health, which is impaired in people with G1PD deficiency classes 3 to 6.
Individuals with G6PD deficiency may continue to participate in sports to maintain quality of life without an increased risk of hemolytic anemia.
Just one
Try this today: Consult your healthcare team for testing for G6PD deficiency if you have a family history and think you may have the disorder. You can also request testing for your child if they have jaundice and require phototherapy, are of African American or Mediterranean descent, or have a family history of a deficiency.
symptoms, drugs and foods to avoid • musanews
Home early news Favism symptoms, drugs and foods to avoid
- Advertisement -
Among seasonal vegetables in spring we find Fave . We have already told you about the many health benefits of Fave, which unfortunately do not apply to those suffering from favism .
Favism is a serious disease that requires people suffering from it to avoid eating beans and other foods.
Favism and bean allergy
Favism and bean allergy they are not the same . We must not confuse favism, a disease, with bean allergy , which is a food allergy that affects about 3 percent of the Italian population, especially in childhood. However, bean allergy is quite rare.
Causes of favism
Favism is a pathology in which there is a congenital defect in the enzyme is usually found in red blood cells. This enzyme defect is inherited X chromosome . Favism this severely affects males , while females are healthy carriers and may pass the genetic defect to sons or become mildly ill. Favism is a widespread disease, especially in Sardegna e Greece , South Asia and Africa. The enzyme involved in favism is glucose-6-phosphate dehydrogenase .
- Advertisement -
People with favism are deficient in this enzyme. Parents afflicted with favism may pass the disease on to their children, who usually have a milder form of the disease. Bean Consumption Exposes G6PD Deficiency risk of hemolytic crises due to the presence of oxidizing substances such as Divicine and Convicin in the seeds.
Symptoms of favism
Symptoms of favism and the disease itself appear. 12-24 hours after taking fresh beans . In severe cases about half of the red blood cells are destroyed , L ' The Italian association of favism explains that when the disease appears shortly after taking fresh beans (or other drugs or foods that cause favism), the patient takes intense yellow on a pale background . The skin and mucous membranes become very pale. Urine becomes too colored, signs of cardiovascular insufficiency may appear.
I the main symptoms of favism they are:
- Sudden onset of fever and jaundice of the skin and mucous membranes.
- Urine yellow-orange with hypercoloration.
- Paleness, weakness, impaired general condition.
- Frequent labored breathing.
- Pulse is frequent, weak, not very noticeable.
How to diagnose favism
Diagnosis of favism is due to blood test specific, which serves to determine the presence of the enzyme glucose-6-phosphate dehydrogenase in erythrocytes. The test is used both to diagnose the present disease and to detect i. healthy carriers of favism .
- Advertisement -
Products to avoid
At the moment there would be no real means and solutions to prevent the symptoms of favism, if it were not for the instruction on to avoid food and drugs that cause illness. Those with enzyme deficiency associated with favism should avoid swallowing :
- Fave
- peas
- Verbena hybrid
- Certain drugs (eg sulfonamides, salicyls, quinidine, menadione)
- Lupins
- Peanuts
Some patients prefer to avoid also :
- All legumes, including soy and its derivatives
- blueberry
- Red wine
- Tonic
These foods and drugs act as favism triggers by inhibiting the activity of the enzyme glucose-6-phosphate dehydrogenase in red blood cells and unfortunately further depleting red blood cells that are already deficient in this enzyme.