How to feed baby with flat nipples
Breastfeeding with flat, inverted or pierced nipples
Nipple shapes and sizes can vary a lot from woman to woman. Read our practical tips to help make breastfeeding a little easier – whatever type of nipples you have
Share this content
Most women’s nipples protrude and become more erect when stimulated by touch or sensation, but some have nipples that are flat or inverted. And some women have had one or both nipples pierced. Many mums with inverted, flat, or pierced nipples breastfeed with no problems at all, but others need extra support.
“Don’t panic if you have flat or inverted nipples, it’s often perfectly possible to breastfeed,” reassures Sioned Hilton, a lactation consultant, neonatal nurse and health visitor, who has worked with Medela in the UK for more than a decade. “Remember your baby latches on to a mouthful of breast, not only the nipple itself, when feeding effectively. ”
But in the earliest days, when your baby’s mouth is still tiny and her sucking is less efficient, inverted or flat nipples may make it harder for her to start – particularly if she is premature or unwell.
“If your nipple is flat or inverted, it may not reach the roof of your baby’s mouth to stimulate her palate and trigger her sucking reflex,” Sioned explains. “This could mean she has problems latching, or can’t stayed latched on for effective milk transfer.”
How to tell if you have flat or inverted nipples
Flat nipples1 don’t protrude very far from the areola (the darker area surrounding them), even when stimulated.
An inverted nipple dimples inwards at the centre. It may look like this all the time, or only when stimulated. Sometimes inverted nipples retract back so they are level with the areola, or they may even sink down into the breast tissue.
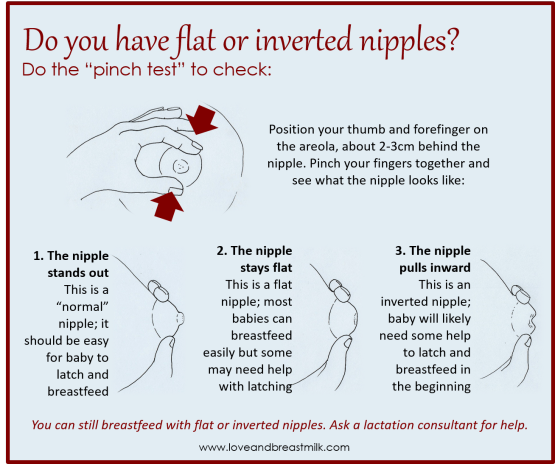
One or both nipples can be affected, and it’s estimated up to 10% of first-time mums have at least one inverted nipple.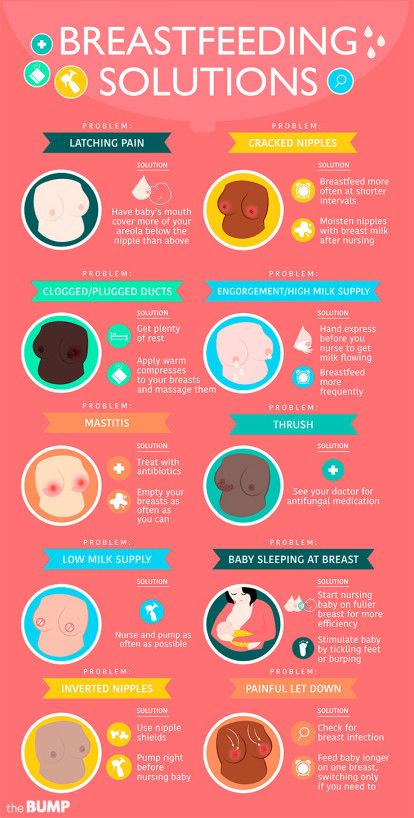 2 If you’re not sure whether your nipple is inverted, try the ‘pinch test’: compress your breast gently, with your thumb and forefinger either side of the areola. Most nipples will poke out, but if yours retracts or pulls inwards, creating a hollow at the end, then it’s inverted.
2 If you’re not sure whether your nipple is inverted, try the ‘pinch test’: compress your breast gently, with your thumb and forefinger either side of the areola. Most nipples will poke out, but if yours retracts or pulls inwards, creating a hollow at the end, then it’s inverted.
Preparing inverted or flat nipples during pregnancy
You may find that, as your breasts change during pregnancy, your nipples begin to protrude more by themselves. If not, and you’re concerned that their shape could make breastfeeding difficult, you can wear nipple formers. These soft, flexible silicone discs fit discreetly inside your bra and place gentle pressure on your nipples, helping draw them out.
“Nipple formers can be worn from week 32 of a normal pregnancy,” advises Sioned. “Start with just an hour a day and build up to around eight hours. If you have an incompetent (weakened) cervix or are otherwise at risk of delivering pre-term, chat to a healthcare professional about the best time to start using them, as nipple stimulation can bring on contractions.
“You can continue to wear the nipple formers once your baby is born,” she adds. “Try popping them inside your bra 30 to 60 minutes before you’re due to breastfeed.”
“I have inverted nipples and, after two or three weeks of trying to get my baby to latch, was on the verge of switching to formula,” remembers Nina, mum of one, Germany. “I sought help from La Leche League and a lovely lady visited and encouraged me to keep going. She suggested nipple formers, which really helped. Somehow my little boy started to understand what to do! Breastfeeding was then great and we kept going until he was 21 months old.”
Helping your baby latch on to flat or inverted nipples
If your baby will suck happily on your finger but seems less interested in your breast, it’s a sign your nipple may not be reaching her palate when she latches on. She may become frustrated and pull away and cry, or even fall asleep at your breast. If this is happening, ask a lactation consultant or breastfeeding specialist to check her latch.
There are several techniques you can use just before each breastfeed to form your nipples into an easier shape for your baby to latch on to. Sioned suggests:
- rolling your nipple between your thumb and forefinger to encourage it to stick out
- compressing your breast just behind your areola with your fingers in a ‘V’ or ‘C’ shape to push your nipple outwards
- touching your nipple briefly with a cold compress or ice cube to make it erect
- hand expressing or using a breast pump for a couple of minutes before a feed to pull your nipple out more
“I have one flat nipple, but only found out when Austin had difficulty feeding on that side,” says Jennifer, mum of two, UK. “There’s nothing anatomically wrong – it just doesn’t perk up as much, which makes the latch a bit trickier. Before feeding on that side I always tweaked and squeezed it a bit and eased it into his mouth. It was a bit tricky early on but got a lot easier as time passed.”
Using a nipple shield to help baby latch on
If none of the above work and your baby is still struggling to maintain her latch, your lactation consultant or breastfeeding specialist may advise you to feed your baby through a nipple shield. This is a thin, flexible piece of silicone, shaped like a nipple, with holes in the tip for your milk to pass through.
This is a thin, flexible piece of silicone, shaped like a nipple, with holes in the tip for your milk to pass through.
The nipple shield offers your baby a larger, firmer target, as well as stimulating her palate to encourage her to suck. In general nipple shields should be considered as a short-term solution. If problems or pain occur, consult your lactation consultant or breastfeeding specialist, who will ensure your baby is latching well with the shield in place. You’ll also need to monitor your baby’s weight gain to ensure your milk supply is building to meet her needs.3
Over time, as your baby’s suck gets stronger and your nipples become more accustomed to breastfeeding, you might be able to breastfeed without the nipple shields.
“My nipples are rather flat. A healthcare professional recommended nipple shields for my two babies, and I used them with great success,” says Anne-Sophie, mum of two, Sweden. “My secret to make them stick to the skin is to wet the edge slightly before use.![]() ”
”
Breastfeeding with pierced nipples
Many women with pierced nipples find it has no impact on their ability to breastfeed – although you’ll need to remove jewellery before feeds as it’s a choking hazard and could graze your baby’s tongue, gums or palate.
“I had a nipple piercing, but removed it a year later when I got pregnant as my breasts felt sensitive,” says Kellie, mum of three, UK. “I breastfed my daughter exclusively, and then her two younger brothers, with no issues whatsoever. If anything, the pierced nipple was the favourite!”
Other mums find breast milk leaks from their piercing holes, or suspect scarring from the piercing is reducing their milk supply4 – although there has been limited research in this area.
“It’s impossible to know how a piercing will affect breastfeeding until your milk comes in,” says Sioned. “Get advice from a lactation consultant or breastfeeding specialist if you’re worried. And remember babies can get all the nutrition they need from just one breast if there’s a problem with the other. ”
”
If you can’t breastfeed with flat or inverted nipples
If you’ve tried everything and breastfeeding’s just not working, you still need to feed your baby.
“The most important thing is a well mum and baby,” says Sioned. “Exclusive pumping, so your baby has expressed milk at every feed, might work for you. Or you could try a supplemental nursing system so your baby can practise feeding from your breast while being topped up with expressed milk through a tube. This means she still gets the breastfeeding experience and stimulates your milk supply, which in turn may help you express more milk.”
“I have inverted nipples. After a disastrous breastfeeding experience with my first son, I was determined to succeed with my second,” says Babettli, mum of two, Italy. “I got advice from experts and tried nipple formers and nipple shields, but without success. In the end pumping exclusively using a hospital-grade Medela Symphony double electric breast pump was the best option for us.![]() I pumped every feed for four months.”
I pumped every feed for four months.”
Caring for different types of nipples
You may need to take extra care of your flat or inverted nipples as your baby might suck on them more strongly, which could make them sore at first. For tips on combatting sore nipples, read nipple care for breastfeeding mums.
If your nipples retract after feeding, any dampness could make them sore and increase the risk of infections, including thrush. Pat them dry after a feed before they have the chance to sink back.
Flat and inverted nipples can be harder to deal with if your breasts are engorged – when even nipples that are usually erect can temporarily flatten. Read our article on breast engorgement for advice.
The great news is that repeated breastfeeding or pumping can alter your nipple form, so breastfeeding might get easier as your baby grows. And you may not have any problems at all if you have another baby – as Leanne, mum of two, UK, found:
“Second time round breastfeeding was a dream,” she says. “Nearly four months of expressing for my first son had helped stretch out my flat nipples and my second son latched straight away without nipple shields. He’s still feeding now at nine months.”
“Nearly four months of expressing for my first son had helped stretch out my flat nipples and my second son latched straight away without nipple shields. He’s still feeding now at nine months.”
References
1 Pluchinotta AM. The Outpatient Breast Clinic. Springer International Publishing; 2015.
2 Alexander JM, Campbell MJ. Prevalence of inverted and non-protractile nipples in antenatal women who intend to breast-feed. The Breast. 1997;6(2):72-78.
3 McKechnie AC, Eglash A. Nipple shields: a review of the literature. Breastfeeding Medicine. 2010;5(6):309-314.
4 Garbin CP, Deacon JP, Rowan MK, Hartmann PE, Geddes DT. Association of nipple piercing with abnormal milk production and breastfeeding. JAMA, Journal of the American Medical Association. 2009;301(24):2550-2551.
Read more
Inverted and Flat Nipples - La Leche League International
Inverted or Flat Nipples
Prepared by Mary Marine
The size and shape of nipples and breasts vary from person to person and can change during the breastfeeding journey. It is common for nipples to gradually change shape, become more elastic and protrude more during pregnancy and while breastfeeding. When babies suck at the breast, they stretch the nipple and surrounding breast tissue into their mouth. The more elastic or stretchy the nipple, the easier it will be for your baby to latch. However, even if the nipples don’t protrude more during pregnancy, you can still breastfeed. These variations often have very little to do with the baby’s ability to breastfeed, because baby latches to the nipple and surrounding breast tissue.
It is common for nipples to gradually change shape, become more elastic and protrude more during pregnancy and while breastfeeding. When babies suck at the breast, they stretch the nipple and surrounding breast tissue into their mouth. The more elastic or stretchy the nipple, the easier it will be for your baby to latch. However, even if the nipples don’t protrude more during pregnancy, you can still breastfeed. These variations often have very little to do with the baby’s ability to breastfeed, because baby latches to the nipple and surrounding breast tissue.
If you have inverted or flat nipples, your baby may need more time and patience to breastfeed. A flat nipple is smooth next to the breast tissue. Inverted nipples withdraw below the surface of the nipple. If you think your nipple may be inverted, try placing your thumb and finger on opposite sides of the areola (the darker area of skin surrounding the nipple) and squeezing gently inwards. Sometimes nipples may be partly inverted, looking dimpled or folded. Severely inverted nipples retract deeply when compressed or stimulated. A nipple that stands out when stimulated is not inverted.
Severely inverted nipples retract deeply when compressed or stimulated. A nipple that stands out when stimulated is not inverted.
After your baby is born, your nipples may appear flatter than usual but babies often lick the nipple to stimulate it before latching on. Your nipples may also appear flatter if your breasts are very full or engorged.
A deep latch and comfortable position helps your baby latch and breastfeed effectively. In the beginning, the following techniques may help you initiate breastfeeding:
- Immediately after birth, place your baby in skin-to-skin contact on your chest. Continue to use skin to skin during early breastfeeding to soothe your baby and to ease frustrations during breastfeeding. Ideally, the breastfeeding dyad is kept together until both are discharged.
- Being with your baby helps you to recognize your infant’s hunger cues.
- Before breastfeeding, express several drops of milk, so the milk is immediately available when your baby latches.

- You may massage your breast while breastfeeding to assist your baby in receiving milk.
To help evert the nipple:
- Pull back on breast tissue so nipple will protrude more.
- Breastfeed in a laidback or side-lying position especially if you have large breasts.
- Breast engorgement can contribute to the nipple being less protruded. Massage the nipple and areolar area so milk will move back into the breast or will leak out, softening the areola and everting the nipple. Also try reverse nipple softening. Reverse pressure softening involves using gentle finger pressure around the base of the nipple to temporarily move some of the swelling slightly backward and upward into the breast.
- Roll the nipple between the thumb and index finger and immediately afterwards touch the nipple with a moist cold cloth. Avoid making the nipple too cold because it can result in the nipple being numb, and inhibit let down.
- Use nipple and breast support to help protrude the nipple.
 Use both hands on each side of breast to make a “sandwich”, to squeeze nipple and areola. Use hands to press in on breast like the way you hold a big sandwich to put in the mouth.
Use both hands on each side of breast to make a “sandwich”, to squeeze nipple and areola. Use hands to press in on breast like the way you hold a big sandwich to put in the mouth. - Use a breast pump for several minutes to draw out the nipple. The suction from a pump will often cause the nipple to protrude more.
- If you have had assistance with latch and tried the tips in this article and your nipples are still sore, consider trying a nipple shield. The nipple shield is a thin silicone devise that goes on top of your nipple and areola while breastfeeding. It looks like a brimmed hat. The nipple shield is a commercially made product. A nipple shield can be used temporarily to help establish breastfeeding or in some cases to help ensure that breastfeeding continues. A shield provides a firm stimulus at the roof of a baby’s mouth where the soft and hard palate meet. This may help your baby suckle more effectively.
- Commercial products that are intended to assist in drawing out inverted nipples such as breast shells or everters are best used only with the guidance of a trained lactation consultant.

If Nipple Soreness Occurs
- You may experience nipple soreness for about the first two weeks of nursing while your flat or inverted nipple is gradually drawn out by baby’s suckling. This discomfort is generally the result of adhesions or skin binding to underlying breast tissue. If the soreness is severe, or continues past the initial two weeks, consult your health professional.
- If your nipple retracts after feedings, that skin may remain moist, leading to chapping of the skin. After feeding, pat your nipples dry and apply a moisturizer safe for breastfeeding. You may also want to wear breast shells or other devices to keep your nipple out between feedings so the skin can dry.
When Nipple Soreness is Prolonged
Rarely, sore nipples may persist for a longer period because instead of stretching, the adhesions remain tight. This can create a stress point which may lead to cracks or blisters.
- If one breast is easier for your baby to grasp and he nurses well from that breast, you can continue to feed on that side.
 You can pump the breast with the deeply inverted nipple until the adhesions loosen and the nipple is drawn out. Your baby will get all the milk he needs from one breast if allowed unlimited and unrestricted time at the breast.
You can pump the breast with the deeply inverted nipple until the adhesions loosen and the nipple is drawn out. Your baby will get all the milk he needs from one breast if allowed unlimited and unrestricted time at the breast. - If both nipples are deeply inverted, you can pump both breasts simultaneously for 15-20 minutes 8 or more times in 24 hours. You can feed your baby with an alternative feeding device until she is able to latch on effectively and comfortably.
- How long you will need to pump in order to draw out your nipples depends upon the strength of the adhesions and the degree of inversion. One pumping may be enough to completely draw out the nipple. If the nipple continues to deeply invert, you may need to continue pumping. When your nipple stays out after pumping, you can resume breastfeeding immediately.
- Once your nipple can be drawn into the baby’s mouth correctly and the baby can breastfeed effectively, you should be able to discontinue pumping and breastfeed without discomfort.

- On rare occasions you may continue to feel some discomfort even after your nipple has been drawn out. This could be due to the correction to the nipple.
- The nipple may invert again as your baby pauses during a feeding. In this case, you may need to stop breastfeeding and pump again for a few minutes before putting baby back to the breast.
- As a temporary transition to exclusive breastfeeding, breast compressions or the use of a nursing supplementer might help to encourage continuous sucking and swallowing so that the nipple won’t be as likely to invert during feeding.
If you do encounter challenges during your breastfeeding journey, support from a La Leche League Leader and other participants in Group meetings may help you to overcome the challenges. (Find a Leader or meeting.)
Additional Resources
Cotterman, Jean K., Reverse Pressure Softening, http://breastfeedingmadesimple.com/wp-content/uploads/2016/02/SimplerRPSsheet2. pdf
pdf
Cotterman, Jean K., Reverse Pressure Softening, http://www.breastfeedingonline.com/rps.shtml#sthash.2MPE4KHE.T3v63FBt.dpbs
Cotterman, Jean K., Engorgement Help: Reverse Pressure Softening
… a technique to aid latching when a mother is engorged, https://kellymom.com/bf/concerns/mother/rev_pressure_soft_cotterman/
Cotterman, Jean K. Reverse Pressure Softening, http://www.health-e-learning.com/articles/RPS_JCotterman_ver2005.htm
Genna, Catherine Watson, Supporting Sucking Skills in Breastfeeding Infants, C. Burlington, MA: Jones & Bartlett, 2012.
La Leche League Great Britain, Nursing Supplementers, https://www.laleche.org.uk/nursing-supplementers/
Mohrbacher, N. Breastfeeding Answers: A guide to helping Families, 2nd edition
(Revised February 2022)
Breastfeeding with pierced, flat or inverted nipples
The shape and size of nipples can vary greatly from woman to woman. Our practical tips will help you make breastfeeding easier, no matter what your nipples are.
Share this information
Most women's nipples protrude, enlarge and swell when touched, but some have flat or even inward nipples. In addition, some women pierce one or both nipples. Usually flat, inverted or pierced nipples do not cause problems when breastfeeding, but in some cases additional help may be needed.
“Don't panic if you have flat or inverted nipples. As a rule, this does not interfere with breastfeeding in any way,” says Shawnad Hilton, a lactation consultant, health visitor and newborn care specialist who has worked with Medela in the UK for more than a decade. “Remember that your baby takes into his mouth not only the nipple, but also part of the breast.”
However, in the early days, when the baby's mouth is still very small and suckling skills have not developed, inverted or flat nipples can make feeding difficult, especially if the baby is unwell or born prematurely.
“Flat or inverted nipples may not reach the baby's palate and therefore not trigger the sucking reflex,” Schoned explains.![]() “That is, the baby may have trouble grasping and holding the breast in the mouth, and the baby will not get enough milk.”
“That is, the baby may have trouble grasping and holding the breast in the mouth, and the baby will not get enough milk.”
How to tell if you have flat or inverted nipples
Flat nipples 1 do not protrude much from the areola (the darker
area surrounding the nipple) even when stimulated.
Inverted nipples seem to be recessed in the center. They may look like this all the time or only if they are stimulated. Sometimes inverted nipples are on the same level with the areola, and sometimes even sink deep into the breast tissue.
This feature may occur on one or both nipples. It is estimated that approximately 10% of nulliparous women have at least one retracted nipple. 2 If you're not sure what type of nipples you have, try a simple pinch test: Gently squeeze your breast with your thumb and forefinger on both sides of the areola. The nipple should come forward. If your nipple hides inside, creating a depression, then it is retracted.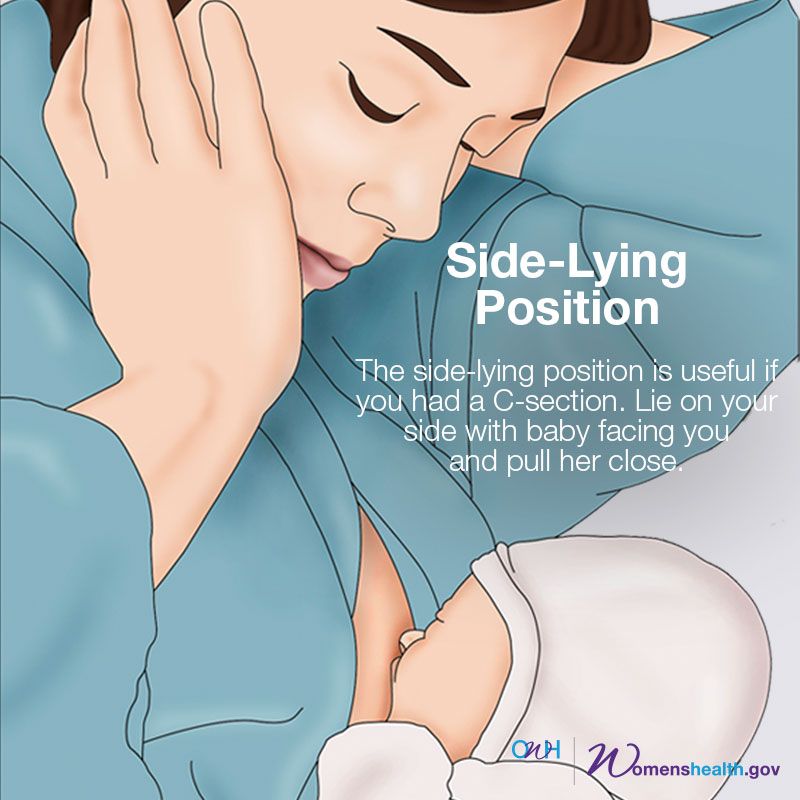
Preparing inverted and flat nipples during pregnancy
You may have noticed that during pregnancy your breasts have changed and your nipples have become more protruding. If this does not happen and you are worried that the shape of your nipples will make breastfeeding difficult, try using nipple formers* in consultation with your doctor. These are soft and flexible silicone discs that are discreetly placed in the bra and slightly squeeze the nipples, helping to pull them out.
“In a normal pregnancy, nipple formers can be worn from 32 weeks,” advises Schoned. - Start wearing them for an hour a day, gradually increasing the time to eight hours. If you have an incompetent (weakened) cervix or are at risk of preterm labor, check with your healthcare provider about when you can start using shapers, as nipple stimulation can trigger contractions.”
“Nipple formers can continue to be worn after childbirth,” adds Schoned. “Try to put them in a bra 30 to 60 minutes before feeding. ”
”
“I have inverted nipples, and after two or three weeks of constantly trying to latch on, I almost switched to formula,” recalls Nina, a mother from Germany. “I turned to La Leche Liga for help, and one nice woman came to me and supported me to continue to feed. She suggested trying nipple shapers and they really helped me. Somehow my baby began to understand what to do! Breastfeeding went well and I nursed him until he was 21 months old.”
How to help your baby latch on to flat or inverted nipples
If your baby enjoys sucking on your thumb but isn't as interested in your breast, chances are your nipple isn't reaching the palate. The baby may become nervous, push off the breast and cry or even fall asleep on your chest. If this happens, ask a lactation consultant or healthcare professional to check the grip.
There are several tricks you can use before every feed to make your nipples more comfortable to latch on to. Schoned recommends the following:
- twist the nipple between thumb and forefinger so that it protrudes better;
- place fingers in a "V" or "C" shape and squeeze the breast just behind the areola to push out the nipple;
- apply a cold compress or ice cube to the nipple to push it forward;
- Express milk manually or with a breast pump for a couple of minutes before feeding so that the nipple comes out more.
“I had a flat nipple, but I only found out about it when I noticed Austin was having trouble suckling on that side,” says Jennifer, mother of two in the UK. “From an anatomical point of view, there is nothing abnormal in this, it’s just that my nipple does not protrude so much, and this requires some skill when feeding. Before giving this breast, I always pinched and squeezed the nipple a little and tried to put it into the baby's mouth. It was a little difficult at first, but over time I learned.”
Using nursing pads
If none of the above work and your baby still has difficulty latch-on, your lactation consultant or healthcare professional may recommend that you breastfeed with a nursing pad*. They are thin and flexible nipple-shaped silicone funnels with holes at the tip through which milk will flow.
It is easier for the baby to put the feeding pad in his mouth, as it is larger and more rigid. In addition, such an overlay will reach him to the sky, causing a sucking reflex. Do not use nursing pads for a long time. If you experience pain or other problems, contact your lactation consultant or healthcare professional to check that your baby is latching on properly with a breastfeeding pad. You will also need to monitor your baby's weight gain to ensure that milk production is meeting his needs. 3
Do not use nursing pads for a long time. If you experience pain or other problems, contact your lactation consultant or healthcare professional to check that your baby is latching on properly with a breastfeeding pad. You will also need to monitor your baby's weight gain to ensure that milk production is meeting his needs. 3
Over time, as your baby learns to suckle properly and your nipples get used to breastfeeding, you will be able to breastfeed without breast pads.
“My nipples are rather flat. The doctor advised me nursing pads, and I was successfully able to feed my two babies,” says Ann-Sophie, mother of two from Sweden. “My secret is to make them adhere better to the skin, I lightly wet the edges before use.”
Breastfeeding with pierced nipples
Many women with pierced nipples find it does not affect their ability to breastfeed. However, jewelry must be removed before feeding, as the child may choke on them or injure their tongue, gums or palate.
“I had a nipple piercing, but I got it off a year later when I got pregnant because my breasts were very sensitive,” says Kelly, mother of three from the UK. “I breastfed my daughter exclusively, and then her two younger brothers, and never had any problems. And the pierced nipple was my favorite!”
Some women report that milk can leak from piercings, while others believe that piercing scars reduce milk production 4 - but this has not been well researched.
“You can't predict how a piercing will affect breastfeeding until milk production begins,” Schoned explains. - If you are concerned, talk to a lactation consultant or healthcare professional. And remember that one breast may be enough for babies to get the nutrition they need if there are problems with the second. ”
What to do if you can't breastfeed with flat or inverted nipples
If you've tried all the options and still can't breastfeed, you still shouldn't deprive your baby of breastmilk.
“Mom and baby's health is the most important thing,” says Schoned. “Maybe you should switch to full pumping and feed your baby only expressed milk. You can also try the supplementary feeding system** where the baby continues to feed at the breast while receiving additional expressed milk through a tube. That is, the baby will still suck on the breast and stimulate the production of milk, which, in turn, will help you pump even more.
“I have inverted nipples. After the disastrous experience of breastfeeding my first son with my second, I decided to get my way after all,” says Babettli, mother-of-two from Italy. - On the advice of experts, I tried nipple formers and nursing pads, but everything was unsuccessful. In the end, pumping with the Medela Symphony*** Double Electronic Clinical Breast Pump proved to be the best solution for us. I fed exclusively on expressed milk for up to four months.”
Care for different types of nipples
Flat or inverted nipples may require extra care as the baby may squeeze them harder and they may become inflamed at first. Tips on how to care for sore nipples can be found in Nursing Nipple Care.
Tips on how to care for sore nipples can be found in Nursing Nipple Care.
If your nipples become inverted after a feed, any moisture can lead to inflammation and increase the risk of infections, including thrush. Blot your nipples dry after each feed before they have time to hide inside.
With swelling of the mammary glands, when even protruding nipples can become flat, flat or inverted nipples can be difficult. Read the helpful tips in the article on breast swelling.
The good news is that continuous breastfeeding or pumping can change the shape of your nipples and breastfeeding will become easier over time. With the arrival of the next child, you may not have to face this problem at all, as happened with Leanne, a mother of two from the UK.
“The second feeding was like a fairy tale,” she says. “After almost four months of pumping for my first son, my flat nipples were so extended that with my second son I no longer had to use breast pads - he was able to suck directly from the breast.![]() The youngest is now nine months old and I still breastfeed him.”
The youngest is now nine months old and I still breastfeed him.”
Literature
1 Pluchinotta AM. The Outpatient Breast Clinic. Springer International Publishing ; 2015. - Pluchinotta A.M., "Treatment of breast diseases on an outpatient basis". Springer International Publishing. 2015.
2 Alexander JM, Campbell MJ. Prevalence of inverted and non-protractile nipples in antenatal women who intend to breast-feed. The Breast . 1997;6(2):72-78. — Alexander JM, Campbell MJ, "Prevalence of inverted and intractable nipples in pregnant women who intend to breastfeed." Ze Brest (Chest). 1997;6(2):72-78.
3 McKechnie AC, Eglash A. Nipple shields: a review of the literature.Breastfeeding Medicine. 2010;5(6):309-314. — McKechnie A.S., Eglash A., "Nipple Covers: A Review of the Literature". Brestfeeding Medicine (Breastfeeding Medicine). 2010;5(6):309-314.
2010;5(6):309-314.
4 Garbin CP0106 , Rowan MK , Hartmann PE , Geddes DT . Association of nipple piercing with abnormal milk production and breastfeeding. JAMA, Journal of the American Medical Association. 2009;301(24):2550-2551. - Garbin S.P., Deacon J.P., Rowan M.C., Hartmann P.I., Geddes D.T., "Nipple piercing and its impact on abnormal milk production and breastfeeding", JAMA (Journal of the American medical association). 2009;301(24):2550-2551.
Read instructions before use. Consult a specialist about possible contraindications. inflated nipples - La Leche Liga Russia
Remember that you are breastfeeding, not a NIPPLE. If your baby is latching deep enough (the mouth and gums are gripping the areola, the nipple is deep in the mouth), in most cases flat or inverted nipples will not interfere with breastfeeding.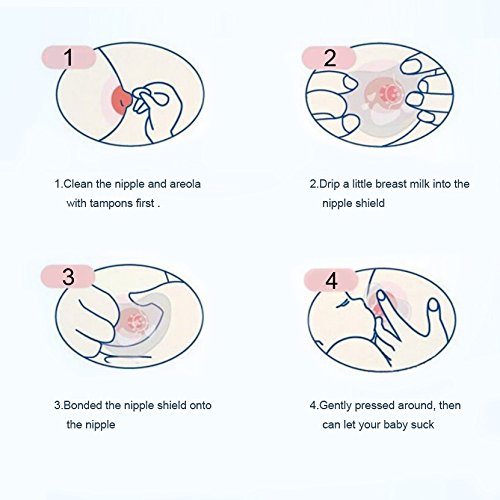 Some types of nipples may be difficult for a baby to latch on to at first, but most of the time, with patience, practice with positions and attachment, you and your baby will be able to breastfeed.
Some types of nipples may be difficult for a baby to latch on to at first, but most of the time, with patience, practice with positions and attachment, you and your baby will be able to breastfeed.
Remember that you are breastfeeding, not a NIPPLE.
How to recognize flat or inverted nipples?
Just because your nipples look flat or inverted doesn't mean they are. Do a "compression test" to check. Gently squeeze the areola a couple of centimeters from the base of the nipple. If the nipple does not protrude when pressed, it is considered flat. If the nipple retracts or becomes sunken, it is considered retracted. In addition, true inverted and flat nipples do not harden during stimulation and in the cold. If the nipple protrudes during the areola compression test, it is not considered to be truly retracted or flat, and no special action is required.
Inverted and flat nipples
- Asymmetrical :
only part of the nipple protrudes when squeezed.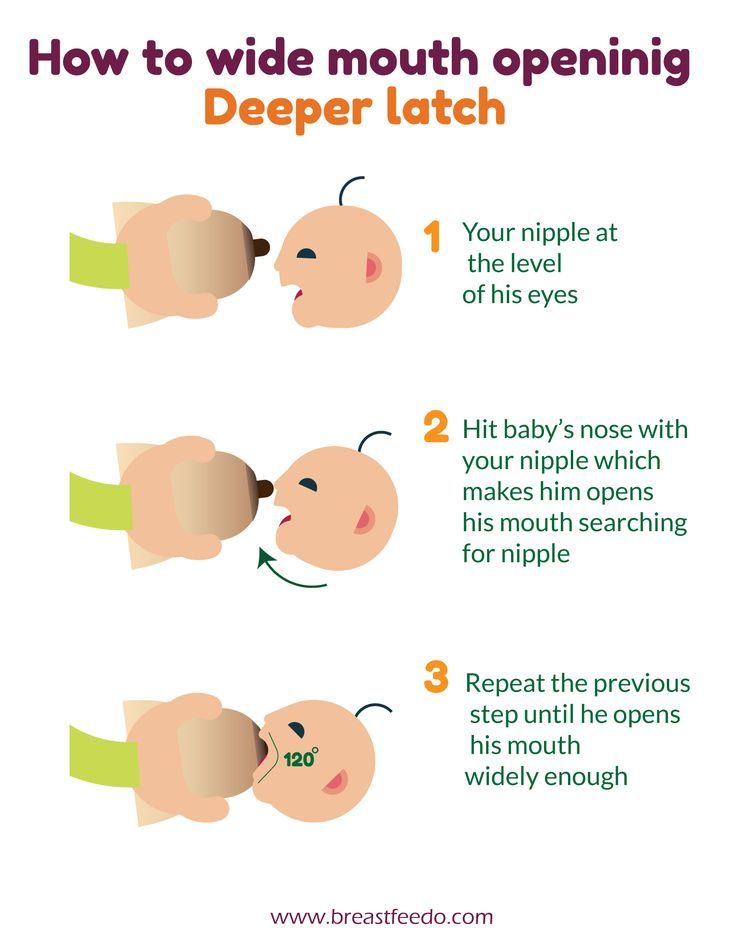 The nipple can be pulled out, but it quickly returns back.
The nipple can be pulled out, but it quickly returns back. - Unilateral :
flat or inverted nipple on one breast only. - Inverted :
there are different degrees of inverted nipples. With slight retraction , a baby with a normal latch and sucking reflex successfully pulls out the nipple, although premature babies or weak suckers may experience some difficulty at first.
Moderate to severe retraction is when the nipple is pressed down to or below the areola level. It may be difficult for a baby to latch on to the breast, but deep latch-on and some special techniques can help. Shaper pads can be useful, especially if used already during pregnancy. If you find inverted nipples after your baby is born, a few tricks can also help, but proper feeding posture and a deep latch are the key to successful breastfeeding.
Tips and tricks for breastfeeding with flat or inverted nipples
Despite the controversy on this subject, many mothers and lactation consultants have noticed that one or another method of correcting inverted or flat nipples has been effective.![]() There is no consensus on whether to check the shape of the nipples in pregnant women, and whether it is worth routinely recommending measures to correct the shape of the nipple before delivery. For example, according to the British Royal College of Midwives, during pregnancy and childbirth, hormonal changes occur in a woman's body, under the influence of which the nipples naturally protrude forward. Although the issue of correcting flat or inverted nipples during pregnancy is controversial, the following tips may be helpful in latching on to a baby who has difficulty latch-on with flat or inverted nipples.
There is no consensus on whether to check the shape of the nipples in pregnant women, and whether it is worth routinely recommending measures to correct the shape of the nipple before delivery. For example, according to the British Royal College of Midwives, during pregnancy and childbirth, hormonal changes occur in a woman's body, under the influence of which the nipples naturally protrude forward. Although the issue of correcting flat or inverted nipples during pregnancy is controversial, the following tips may be helpful in latching on to a baby who has difficulty latch-on with flat or inverted nipples.
- Nipple shields or nipple formers worn in a bra can help elongate flat or inverted nipples. The pads consist of two parts and are made of silicone. In the inner part of the lining there is a hole that is superimposed on the nipple. The edges of the hole press on the tissues around the nipple and this pulls it out. The pads can be worn during pregnancy when the skin is especially elastic - gentle constant pressure will help stretch the connective tissue, pulling the nipple.
 After the baby is born, the pads can be worn between feedings. Do not wear pads at night. The milk that collects in them is not suitable for feeding the baby.
After the baby is born, the pads can be worn between feedings. Do not wear pads at night. The milk that collects in them is not suitable for feeding the baby. - After the baby is born, the effective breast pump or other nipple puller, such as a syringe without a tip, can help shape the nipple just before feeding. In this case, it is easier for the child to grab the breast. You can also use these devices between feedings to stretch the connective tissue under the nipple by applying constant pressure to the center of the nipple.
- Another application - nipple stimulation before feeding . If you can grab the nipple, roll it between your thumb and forefinger for a couple of minutes. Then apply cold for a moment - a wet diaper or ice wrapped in a towel. This method can help "pull out" the nipple. Do not apply cold for a long time, as hypothermia of the areola and nipples can slow down the flow of milk.
- While applying, holding the breast with your thumb above and four fingers under the areola, gently pull the tissues under your fingers towards the chest , releasing the nipple.

- Soften the areola with back pressure (Kotterman method). Place your fingertips around the base of the nipple and gently press towards the chest. Hold pressure 1-3 minutes before feeding. This technique will help free the areola area from other fluids, making it easier for the milk to flow out and the nipple to be drawn out. Now it is easier for the baby to grab the breast. Read more about this method in our article on engorgement.
- The nursing pad is a thin, flexible silicone pad that fits over the nipple. At the tip of the lining there are holes through which milk flows to the baby. If other methods fail, pads can help your baby latch on and suckle by stimulating the upper palate and triggering the sucking reflex. Breastfeeding pads should only be used when accompanied by a consultant or a lactation support group meeting leader, as their use can lead to problems. Editor's note: Why can the overlay be a problem? Once the baby has tried the breast in the breastplate, it is more difficult to encourage him to suckle the breast with the inverted nipple without the breastplate.
 Indeed, in the lining, the nipple immediately “sticks out” and when it touches the palate, the baby immediately begins to suck. The inverted nipple is pulled out only after the child has already begun to suck . When the breast enters the mouth, it does not stimulate the palate, does not include sucking in the same way as a pad. The baby must learn that the nipple will stretch in process . If he has already tried the pad, it will be more difficult for him to get used to the shape of the chest. If only your breasts enter his mouth, he does not get tangled and adapts much easier to what he has. Therefore, they try to avoid overlays as much as possible, as well as bottles and nipples - all items in which the nipple sticks out initially, and does not stretch “in the process”.
Indeed, in the lining, the nipple immediately “sticks out” and when it touches the palate, the baby immediately begins to suck. The inverted nipple is pulled out only after the child has already begun to suck . When the breast enters the mouth, it does not stimulate the palate, does not include sucking in the same way as a pad. The baby must learn that the nipple will stretch in process . If he has already tried the pad, it will be more difficult for him to get used to the shape of the chest. If only your breasts enter his mouth, he does not get tangled and adapts much easier to what he has. Therefore, they try to avoid overlays as much as possible, as well as bottles and nipples - all items in which the nipple sticks out initially, and does not stretch “in the process”.
For the first time in the maternity hospital they advised linings. Used them for a month. It was painful without them. They are less painful. For a month, the chest “got used to” (it’s hard to formulate, just after a month the chest stopped hurting) and I removed the pads.
The second time I already bought the pads in advance, but the child categorically refused them. And just like that time, the first month was painful to tears, although I thought that for 9months of break breasts will not forget how to feed, but she forgot. A month later, the nipples stretched out again and feeding ceased to be a pain. By the way, there have never been any problems with gripping, postures, etc., and I'm sure it's the nipples.
(from Anna's story)
The consultant instructed me to be confident, but not harsh, so that the child would not refuse guards at all. Therefore, I offered three or four times without an overlay, and if my daughter refused, then without leading to hysteria, I put on an overlay and fed with it. I also had a way - I started with an overlay, when my daughter satisfies her first hunger, she took off and offered just breasts)
(from Ekaterina's story)
Successful start of breastfeeding
• Seek help
It is very important to get professional help if you have flat or inverted nipples. The child needs to learn to open his mouth wide, grabbing the areola, not the nipple. You can try different positions (see the maternity hospital leaflet) and find the most comfortable and effective for you and your baby. Some mothers find that the under-arm position and cross cradle allow them to control attachment, helping the baby latch on deeply.
The child needs to learn to open his mouth wide, grabbing the areola, not the nipple. You can try different positions (see the maternity hospital leaflet) and find the most comfortable and effective for you and your baby. Some mothers find that the under-arm position and cross cradle allow them to control attachment, helping the baby latch on deeply.
• Start breastfeeding on demand as soon as possible
Try to start breastfeeding as soon as possible after delivery. Then put the baby to the breast at least every 2-3 hours. This will help to avoid breast engorgement, and the baby will practice applying before the arrival of large volumes of milk. Crowded breasts become firmer, making it harder to latch onto the nipple, so it's important that the baby gets more practice feeding from soft breasts.
• Get a deep grip
When applying, hold the baby close to you so that the ear, shoulder and hip are in a line. Position the baby so that his nose is at the level of the nipple. Gently pull the breast tissue away from the nipple to make it easier for your baby to latch onto the breast. Touch the baby's lips with the nipple and wait until he opens his mouth very wide (as if yawning). Now attach the baby, while making sure that the nipple is deep in the mouth and the baby has captured the areola. The result is an asymmetric grip - the lower jaw captures more of the areola than the upper. The nose may touch the chest, but is not "buried" into it. The lips are turned out, like those of a fish stuck to the wall of an aquarium.
Gently pull the breast tissue away from the nipple to make it easier for your baby to latch onto the breast. Touch the baby's lips with the nipple and wait until he opens his mouth very wide (as if yawning). Now attach the baby, while making sure that the nipple is deep in the mouth and the baby has captured the areola. The result is an asymmetric grip - the lower jaw captures more of the areola than the upper. The nose may touch the chest, but is not "buried" into it. The lips are turned out, like those of a fish stuck to the wall of an aquarium.
• Calm down an upset baby
We need to experiment, look for something suitable for me and my child personally.
Breastfeeding should evoke positive associations in the child. If your baby gets frustrated, stop trying to feed and calm him down. Offer to suck your finger, scold on the handles, shake, sing a song. Try again when both of you are in a good mood. Remember to feed your baby regularly: if he has not breastfed for a long time, offer expressed milk from non-sucking objects.
Sore nipples
Discomfort with stretching of the connective tissue
Some mothers experience nipple pain in the first couple of weeks of feeding, when flat or inverted nipples gradually stretch under the influence of sucking. If the pain gets worse or lasts longer than two weeks, contact an LLL Volunteer Consultant (contacts).
Inverted nipple diaper rash
If the nipple is inverted after a feed and its surface remains wet, this can lead to diaper rash. After feeding, pat your nipples dry and apply a very thin layer of a nourishing-safe moisturizer such as lanolin. You may find it comfortable to put on nipple formers between feedings to keep the nipple bulging and the skin from becoming soggy.
If the soreness does not go away
In rare cases, mothers experience soreness that does not go away for a long time. This can happen if the connective tissue does not stretch, but remains very tight. As a result, cracks or calluses may appear.
As a result, cracks or calluses may appear.
Sometimes, if the nipple is very deeply recessed, when suckling, the child does not squeeze the milk ducts, but the nipple. In this case, the baby fails to get enough milk, and such feeding is painful for the mother. In such cases, a double-sided electric breast pump can come in handy, which does not compress the areola, but evenly "sucks" the center of the nipple. Often over time, the connective tissue develops and the nipple is pulled out.
If your baby is more comfortable suckling effectively on one of the breasts, you can continue feeding on the side that is comfortable. You can pump the other breast for now so that the nipple stretches out. The baby will get the necessary milk from one breast if he feeds as often and for as long as he wants.
If both nipples are deeply inverted, you can express both sides at the same time for 15-20 minutes, eight or more times a day. You can feed your baby with non-sucking items until effective and comfortable latching is achieved.![]()
How long will the pumping last? It depends on the degree of retraction of the nipples and on the elasticity of the connective tissue. For some mothers, one pumping with a breast pump is enough to completely elongate the nipple. If the nipple remains prominent after pumping, you can breastfeed immediately.
Once deep and effective attachment is achieved, pumping can be completed and breastfeeding can be completed without problems.
In rare cases, you may feel discomfort even when the nipple is pulled out. This may be due to a fairly strong effect on the tissue of the nipple.
Sometimes, after a nipple correction, the nipple stretches during feeding, but immediately retracts if the baby has paused in suckling. In such cases, you can interrupt feeding, connect the breast pump for a few minutes, and then attach the baby again. You can try breast compression or feeding at the breast so that the baby does not stop and the nipple does not “run away” during feeding.
If you have difficulty feeding with flat or inverted nipples, you can contact the LLL Volunteer Counselor (contact).
Source at llli.org:
https://www.llli.org/breastfeeding-info/inverted-flat-nipples/
Translation: Ada Torchinova, Editing: Varya Karu, Maria Sorokina. Proofreading: Tatyana Romanova.
Many thanks to the mothers of the La Leche League Facebook group for sharing their stories! (All our social networks are here.)
Thanks for the photo: Victoria Levchenko
Ekaterina
I have a flat nipple on one breast. She had huge problems. From the maternity hospital with overlays, I suffered a lot, because it infuriated me to constantly wash, sterilize, put on in the twilight, instead of just calmly giving breasts. When it reached a peak and lactostasis developed due to overlays, she called a consultant. Helped with poses, showed the correct application. We got rid of the overlays in a day, my daughter was three weeks old. Since then, it is on this breast that the grip often deteriorates, if not controlled, and the nipple is more sensitive, but in general we have been feeding successfully for 15 months and do not plan to finish;)
Since then, it is on this breast that the grip often deteriorates, if not controlled, and the nipple is more sensitive, but in general we have been feeding successfully for 15 months and do not plan to finish;)
I was instructed by a consultant to be confident, but not harsh, so that the child does not refuse guards at all. Therefore, I offered three or four times without an overlay, and if my daughter refused, then without leading to hysteria, I put on an overlay and fed with it. I also had a way - I started with an overlay, when my daughter satisfied her first hunger, she took it off and offered just breasts)
Plus, of course, it was still difficult to overpower myself, since the overlays were mainly for me - it hurt until sparks from my eyes. The pain remained for some time until everything healed. I took hand cream in my teeth and go;))
Anna
“We need to experiment, look for something suitable for me and my child personally” I don't know if my story will work. Normally, I have an almost normal nipple. Well, between normal and flat. But the first thing I heard in the hospital after giving birth: “M, flat nipple, how will you feed it?” This was said by the midwife on duty, who gave me a daughter to breastfeed. When the milk came in and the breasts swelled, the nipples became really flat. At first it was not easy to give a breast, I called a consultant. But in the end all is well.
Normally, I have an almost normal nipple. Well, between normal and flat. But the first thing I heard in the hospital after giving birth: “M, flat nipple, how will you feed it?” This was said by the midwife on duty, who gave me a daughter to breastfeed. When the milk came in and the breasts swelled, the nipples became really flat. At first it was not easy to give a breast, I called a consultant. But in the end all is well.
I fed my daughter up to 1.7. My son is now 1.5 while we are breastfeeding 🙂
I want to share what helped me in the end:
- Absolute confidence that I will breastfeed. I didn't even have any doubts. And so does my family.
- A consultant who told that all women on earth have different breasts and milk supply in different ways, but this does not prevent them from feeding.
- I fed calmly and systematically. She knew what the correct grip should be and just boldly folded her breast so that it was inserted into the baby’s mouth as correctly as possible.

- Sometimes it was difficult with a full breast, I fed my daughter in several stages, a little bit. Then she was able to calmly take the breast and suck.
- And the book The Art of Breastfeeding revealed to me that the picture: the baby just takes the breast and sucks, and then takes care of himself for three hours is an illusion. It is necessary to experiment, look for something suitable for me personally and my child.
Elena
So, back in 2011, I gave birth to my first child in Moscow. While I was lying sprawled in a chair, the midwife came and said: will you apply to the breast? Will. She brings a swaddled log, picks out my breasts from my shirt with her hands, puts it in a log, after which she says: well, what are you going to feed with such nipples, you had to pull out the whole pregnancy every day, and what did you do? It was a hint. The story was like this. For a day I put the baby under oohs, ahhs, whining about supplementary feeding, daivodichki and that's it, the next day the milk came abruptly, the nipples began to hurt. They told me that they needed lining, my husband brought it, I began to try with lining. By evening, the situation was close to critical - the child slept completely satisfied, and his chest was boulders, his nipples hurt. At night, my sister “sprayed” me, this is the worst torture in my entire life. Then we went home, the child perfectly took the breast in the pad, but the engorgement continued, everything hurt wildly, it was impossible to touch the nipples. A wonderful consultant came to me, which was given to me by a friend, she helped with the seizure, showed what needs to be taken into account, we came up with a “technique” with her that would suit us with a child, developed a strategy for dealing with stagnation. As soon as I got better with the grip, I suddenly realized that I didn’t need pads. I just tried it without and never came back. She fed for more than two years until the disappearance of milk during pregnancy. The second child was born at home, with the best midwife in the world, who took care of me from the 20th week.
They told me that they needed lining, my husband brought it, I began to try with lining. By evening, the situation was close to critical - the child slept completely satisfied, and his chest was boulders, his nipples hurt. At night, my sister “sprayed” me, this is the worst torture in my entire life. Then we went home, the child perfectly took the breast in the pad, but the engorgement continued, everything hurt wildly, it was impossible to touch the nipples. A wonderful consultant came to me, which was given to me by a friend, she helped with the seizure, showed what needs to be taken into account, we came up with a “technique” with her that would suit us with a child, developed a strategy for dealing with stagnation. As soon as I got better with the grip, I suddenly realized that I didn’t need pads. I just tried it without and never came back. She fed for more than two years until the disappearance of milk during pregnancy. The second child was born at home, with the best midwife in the world, who took care of me from the 20th week. And the baby just crawled on a self latch, and I only helped with my practiced movement - and there will never be any problems again. I think it's all very individual. But this is what I think about my situation: a proper latch is possible without any nipple at all, because technically the nipple is just a “faucet spout”, the entire milk supply system is inside, and where this spout is is of very little importance if you know how address. That is, yes, the child's mouth has grown a little, we have settled down a little to each other. But it could be done right away, there was no significant problem there. And in order to somehow survive, while nothing is clear, linings, of course, can help. But the main thing that can help is capture and calmness. My midwife was speechless. He says: damn it, I've already prepared to somehow set it all up, and you're just a goddess of capture - how did you do it?)) That's all that Moscow consultant, I am still grateful to her.
And the baby just crawled on a self latch, and I only helped with my practiced movement - and there will never be any problems again. I think it's all very individual. But this is what I think about my situation: a proper latch is possible without any nipple at all, because technically the nipple is just a “faucet spout”, the entire milk supply system is inside, and where this spout is is of very little importance if you know how address. That is, yes, the child's mouth has grown a little, we have settled down a little to each other. But it could be done right away, there was no significant problem there. And in order to somehow survive, while nothing is clear, linings, of course, can help. But the main thing that can help is capture and calmness. My midwife was speechless. He says: damn it, I've already prepared to somehow set it all up, and you're just a goddess of capture - how did you do it?)) That's all that Moscow consultant, I am still grateful to her.
Olga
In the maternity hospital they told me “uuu, you won’t be able to feed with such breasts, your nipples are bad”.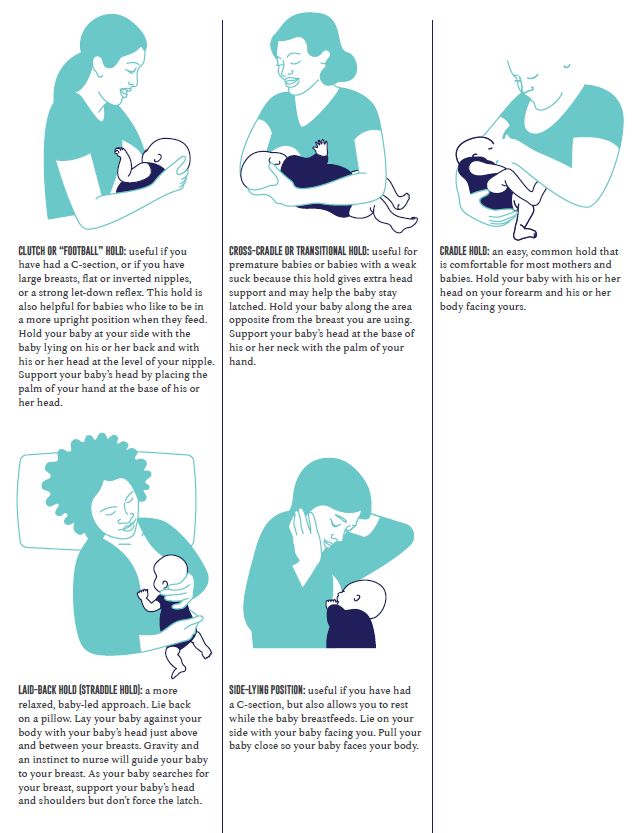 I fed the first child up to 4 years old, at the start there was a consultant for guards and a lot of support from LLL , I feed the second child for two years. There were difficulties with attaching both the first and the second child, but at the very beginning, it can also be associated with the child himself, his ability to open his mouth. And after 3 months, I already forgot that I have some kind of nipples that are not like that
I fed the first child up to 4 years old, at the start there was a consultant for guards and a lot of support from LLL , I feed the second child for two years. There were difficulties with attaching both the first and the second child, but at the very beginning, it can also be associated with the child himself, his ability to open his mouth. And after 3 months, I already forgot that I have some kind of nipples that are not like that
Yana
I have “flat”, well, that’s how they called it in the maternity hospital. The normal application helped me, which the consultant showed me, when you wait for the child until he “finds the center” and opens his mouth, and “roll” him on his chest at that moment, and not push the boob into his mouth forcibly, as they tried to show in the maternity hospital .
Anna
I have flat ones. For the first time in the maternity hospital, linings were advised. Used them for a month. It was painful without them.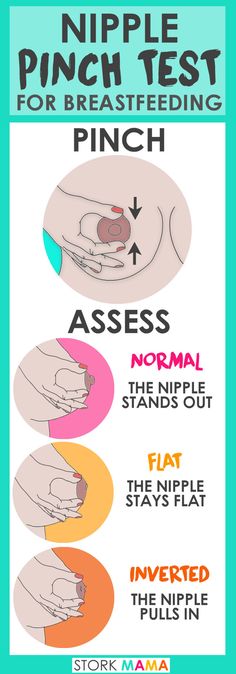 They are less painful. For a month, the chest “got used to” (it’s hard to formulate, just after a month the chest stopped hurting) and I removed the pads. The second time I already bought the pads in advance, but the child categorically refused them. And just like that time, the first month was painful to tears, although I thought that for 9months of break breasts will not forget how to feed, but she forgot. A month later, the nipples stretched out again and feeding ceased to be a pain. By the way, there have never been any problems with gripping, postures, etc., and I'm sure it's the nipples. As a result, two times in three years. Now the nipples are flat again. I did not call the consultant. But then my sister was studying for him, she gave me a lot of information, too, remotely, since she lives in another city. Probably, the breast itself adapted to the new sensations, the children got used to taking the breast correctly, and not grasping it like a pincer. Nipples stretched, yes.
They are less painful. For a month, the chest “got used to” (it’s hard to formulate, just after a month the chest stopped hurting) and I removed the pads. The second time I already bought the pads in advance, but the child categorically refused them. And just like that time, the first month was painful to tears, although I thought that for 9months of break breasts will not forget how to feed, but she forgot. A month later, the nipples stretched out again and feeding ceased to be a pain. By the way, there have never been any problems with gripping, postures, etc., and I'm sure it's the nipples. As a result, two times in three years. Now the nipples are flat again. I did not call the consultant. But then my sister was studying for him, she gave me a lot of information, too, remotely, since she lives in another city. Probably, the breast itself adapted to the new sensations, the children got used to taking the breast correctly, and not grasping it like a pincer. Nipples stretched, yes. Well, lactation was more or less established, and I myself could also “grab” the areola without pain in order to give the child. At first, my chest was bursting so that there was nothing left of the nipple, and because of the pain, I couldn’t even grab it.
Well, lactation was more or less established, and I myself could also “grab” the areola without pain in order to give the child. At first, my chest was bursting so that there was nothing left of the nipple, and because of the pain, I couldn’t even grab it.
Yes, there were no problems during the transition from overlays. And I didn’t use them every feeding, you won’t use them all the time.
Irina
Before pregnancy were flat-retracted. Well, the courses said that it happens. He was born and immediately began to apply it, and he took the breast, and there were no problems. There were no bottles, somehow it was lucky that there was a calm attitude towards this. After that, they stopped being flat.
Svetlana
I had one breast “flat” and the other normal. In the hospital they said 'overlay and period'. The baby had a different opinion that this was not for him. A week and a half later, a friend arrived and the flat nipple became normal. As it still remains, although I visually do not see that something has changed there.