Salt and sugar in baby food
Is Salt and Sugar Good for Your Baby?
Salt and sugar are used as flavour enhancers in our food, but excessive consumption of both salt and sugar can lead to serious health problems in adults and children. According to the World Health Organisation (WHO), adults should limit salt consumption to ¾ and one teaspoon per day. Sugar consumption should be limited to 6 teaspoons a day. Salt and sugar should be avoided for babies as excessive consumption is harmful and can cause problems such as impaired kidney function, tooth decay, decreased immunity, etc.
What Is the Daily Requirement of Salt and Sugar in a Baby’s Diet?
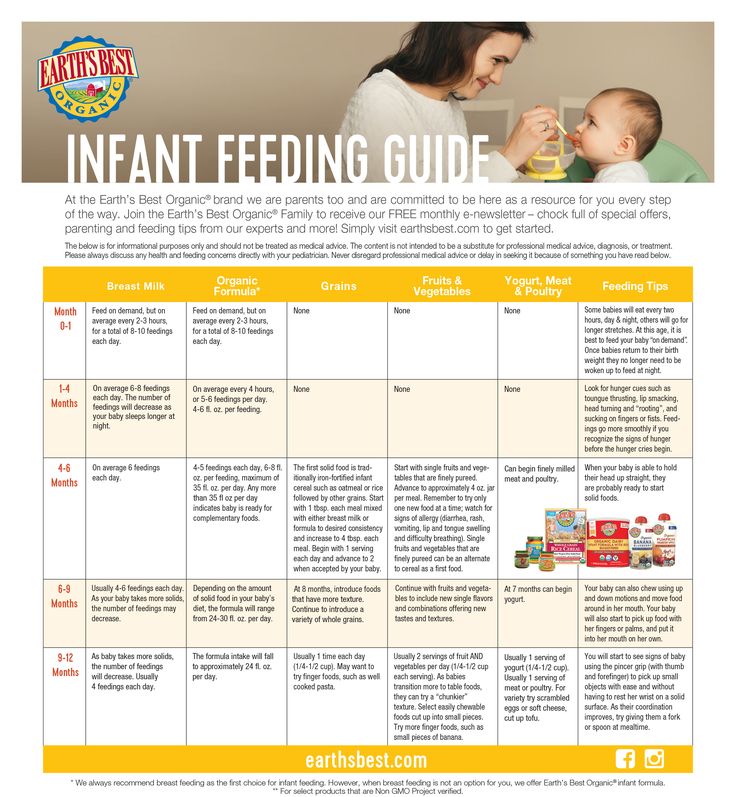
According to various health organisations, infants should not be given any salt until six months of age. Their sodium needs are met by the salt contained in breast milk. Babies aged between 6 months to 1 year should be given no more than 1 gram of salt per day, which contains 0.4 grams of sodium. The salt intake of toddlers aged between 1 and 3 years should be limited to 2 grams per day and children aged 4 to 6 years should consume no more than 3 grams of salt per day.
Babies do not need added sugars or refined sugar in their diet. The sugar requirements of the baby can be met by foods rich in carbohydrates and other naturally sweet foods, such as fruits.
Why Should You Avoid Sugar and Salt in Your Infant’s Diet?
Here are the reasons why you should avoid including salt and refined sugar in your baby’s diet:
1. Affects Kidney Function: Excessive salt intake can impair kidney function as the infant’s kidneys cannot process and eliminate high levels of salt from the blood. This strains the kidneys and can cause kidney-related diseases at a later stage.
2. Causes Kidney Stones: Excess sodium from salt can also cause the body to excrete more calcium in the urine. This calcium can form kidney stones. Kidney stones cause symptoms such as severe pain in the body, fever and chills, nausea and vomiting, burning sensation while urinating, and blood in the urine.
3. High Blood Pressure: Excess salt intake can cause high blood pressure or hypertension. Babies who consume too much salt can develop hypertension as adults.
Babies who consume too much salt can develop hypertension as adults.
4. The Danger of Dehydration: Babies who have excess salt in their bodies are in danger of dehydration, as salt causes the body to lose water in the form of urine and sweat. Infants will not be able to indicate that they are thirsty, and adults may not realise that they are dehydrated until serious symptoms show up. Dehydration can result in kidney stones, joint and muscle damage, constipation, and liver damage.
5. Brittle Bones: Too much salt consumption causes increased sodium levels in the body. This, in turn, causes excretion of too much calcium. Thus, the body loses calcium, which is essential for the development of strong bones. Calcium depletion can lead to a condition called osteoporosis which makes the bones thin and brittle.
6. Tooth Decay: Consuming excessive amounts of added sugars can cause painful cavities and tooth decay. Bacteria in the mouth use sugar from foods to produce acids that damage the teeth.
7. Obesity: Too much sugar in the diet means more calories. Even in an active baby, this could result in a lot of unused calories which get converted to fat and stored in the body. Obesity or having excess body fat is very unhealthy for a baby.
8. Diabetes: Eating too much sugar can lead to type 2 diabetes later in life. Diabetes is a disease that affects the body’s ability to regulate blood sugar levels.
9. Lethargy: High blood sugar levels can result in the overproduction of the hormone called insulin which regulates blood sugar levels. Too much insulin can cause a sudden drop in blood sugar levels, leading to lethargy, inactivity, and tiredness in the baby.
10. Hyperactivity: Since sugar is absorbed into the blood very quickly, high sugar consumption causes the blood sugar levels to shoot up. This leads to higher adrenaline levels and causes hyperactivity in children.
11. Poor Dietary Habits: Consuming excess salt and sugar as a baby leads to a pattern of poor dietary choices later in life. This, in turn, causes lifestyle diseases like obesity, diabetes, and hypertension.
This, in turn, causes lifestyle diseases like obesity, diabetes, and hypertension.
12. Rejecting Breast Milk: If babies begin to like the taste of salt and sugar, they may avoid or reject breast milk. This is detrimental to the growing baby, as breast milk contains several vital nutrients essential for the baby’s growth and development.
13. Will Not Know the Real Taste of Vegetables: If the baby’s food contains too much salt or sugar, it will mask the original taste of the vegetables. The baby will start disliking the taste of vegetables if it is not masked by too much salt or sugar.
Tips for Introducing Solid Foods to Your Baby
- Introduce one food at a time so that you can easily spot allergic reactions in your baby. Wait for two-three days between offering different types of food.
- Puree everything so that your baby can eat the food easily. As he grows older, you can give him solid food in small pieces but keep an eye out for foods like uncooked peas, firm fruits and vegetables, nuts, etc.
 as they can make him choke.
as they can make him choke. - Avoid using silverware and use spoons made of plastic or silicone as they will be better for the baby’s tender gums.
- Don’t try to overfeed the baby. When the baby stops enjoying the food or avoids eating, you should stop feeding him.
FAQs
Here are the answers to a few frequently asked questions about salt and sugar intake in babies:
1. How will your baby get sodium if you completely avoid salt?
The baby’s sodium needs are met by breast milk for the first six months. Apart from this, most foods naturally contain sodium. So the baby’s salt intake should be less than 1 gram per day for the first year.
2. How can you add flavour to the infant’s food without adding salt?
Foods can be made flavourful without the addition of salt. Spices such as cumin powder, asafoetida, cinnamon, and herbs like coriander and mint can flavour the food and enhance the taste. You can also flavour the food using onion and garlic. However, spices must be added in minute quantities, and new foods should be introduced slowly (1 tablespoon on the first day, two the next, and so on) to make sure there are no allergic reactions. Herbs must be thoroughly washed and finely chopped or minced. They should be introduced into the baby’s diet only after seven months of age.
However, spices must be added in minute quantities, and new foods should be introduced slowly (1 tablespoon on the first day, two the next, and so on) to make sure there are no allergic reactions. Herbs must be thoroughly washed and finely chopped or minced. They should be introduced into the baby’s diet only after seven months of age.
3. What are the substitutes of sugar for baby food?
There are plenty of naturally sweet substances that can be used as sugar substitutes. These include any fruit puree, date syrup, and honey. However, date syrup and honey should not be given to infants below 1year of age.
4. Will my baby eat bland food without salt? What if he does not like it?
Adults cannot eat bland food without salt as they are used to eating food rich in a variety of flavours. A baby has never tasted salt and will therefore not feel that the food is bland. In case the baby does not seem to like the food, you can try to enhance the taste using flavour enhancing spices like cumin, cinnamon or asafoetida, herbs like mint or coriander, and garlic or onion.
5. When do I start adding salt and sugar in baby’s food?
You need not give a baby salt until one year of age. If you do want to introduce salt, limit it to less than 1 gram per day for babies older than six months. However, it is better to avoid salt for babies under one year of age. Giving sugar to infants less than one year of age is not recommended. Baby foods do not require added sugars. You can use natural sugar substitutes like fruit puree, date syrup or honey. Even fruit juices given to babies must be diluted to reduce the sugar content.
Salt and sugar can do more harm than good for babies. Hence, it is better to avoid them at least until the baby turns one year old. Processed foods should also not be given to babies as they contain high amounts of salt. Many commercial baby foods may also contain added sugars. Check the ingredients carefully to determine the salt and sugar content if you use commercial baby food. Keep your baby healthy by giving homemade food without added salt or sugar.
Resources & References: Parents, What to Expect
Also Read: Honey for Babies – Is It Safe?
Why No Salt and Sugar For Babies until 1 year of age
Why No Salt and Sugar for babies till 1 year? This must be one of the foremost doubt for all new moms who start weaning for their babies.
Why No Salt for Babies till 1 year ?
Harmful effects of adding salt to Baby Food
How to add flavor to baby food without adding salt?
How to know whether commercial Baby & children food is high in Salt?
Why No Sugar for Babies until 1 year?
Why is sugar harmful to Babies below 1 year?
What to substitute for sugar in baby foods?
Natural Sweeteners for Baby food
Also, if your baby has recently started on solids, you might also be wondering what kind of feeding chair is best for your baby. Check out our detailed post – High Chair Vs Booster Seat: Your Ultimate Guide to Buying a Feeding Chair.
Check out our detailed post – High Chair Vs Booster Seat: Your Ultimate Guide to Buying a Feeding Chair.
Buy Healthy Nutritious Baby, Toddler food made by our own Doctor Mom !
A couple of days back a new mom emailed me to ask ” Can I add Salt to my Baby food” due to a volume of emails I receive everyday, just sent out a short reply that she shouldn’t add salt to baby food till 1 year. Immediately a reply landed in my inbox asking the reason behind the No sugar no salt rule for babies till 1 year.
This generation of parents are very inquisitive and can be satisfied only with a detailed researched article. So decided to tackle this no sugar no salt rule for today’s article.
Let’s reason out some basic concepts first,
” Why do you think that your baby needs salt in his/ her food ? “
You think that the reason your baby is not accepting the first foods because it is bland.
This is where most of us are mistaken, your baby doesn’t show interest in the food, as the baby is used to breastmilk and doesn’t like being fed with new unknown food.
For someone who has tasted only breastmilk till 6 months of age and who never knows the taste of salt before, what is the need to add salt to the food.
He can’t miss something that he hasn’t experienced yet !!!!
Harmful effects of adding salt to Baby Food
A baby’s salt requirement per day is less than 1 g per day (0.4g of sodium) and this is mostly met by the breastmilk or formula. So any extra salt will be a burden on the tiny kidneys and the kidney’s will not be able to function properly due to the excessive load. This may lead to kidney disease and it has also been proven to cause hypertension in the adult life. Excessive intake of salt in childhood has also been attributed to diseases as osteoporosis, cardiovascular diseases, and respiratory illnesses.¹
The SACN ² recommends the following Salt Requirement for babies, toddlers, and children
| Age | Maximum Salt Intake |
|---|---|
| 0-6 months | < 1 g (0. 4g of sodium) 4g of sodium) |
| 6-12 months | < 1 g (0. 4g of sodium) |
| 1-3 years | 2 g (0.8g of sodium) |
| 4-6 years | 3 g (1.2g of sodium) |
| 7-10 years | 5 g ( 2 g of sodium) |
| 11 years and above | 6 g (2.4 g of s0dium) |
Some people advice to add a pinch of salt to baby food which is also equally dangerous.
While the amount of a pinch of salt may vary, Wiki calculates that 1 pinch of salt = ¼ gram.
One pinch of salt added to three meals a day equals to more than 0.75 g of salt that in addition to the salt in breastmilk or formula may skyrocket the salt consumed by the baby per day.
How to add flavor to baby food without adding salt?
You can make your baby food more interesting and tasty by adding spices appropriate to the age of the baby.
Learn ” How, when and what spices to be added to Baby Food”
How to know whether commercial Baby & children food is high in Salt?
While most of us prefer Homemade Baby food, there are few situations like traveling with babies where in we have to depend on commercial baby food.
Not only for babies, even food for children may also be high in salt, and you should always be careful while selecting the food.
The salt content is usually given as figures for sodium. As a rough guide, food containing more than 0.6g of sodium per 100g is considered high in salt ³. You can workout the amount of salt in foods by multiplying the amount of sodium by 2.5.
Why No Sugar for Babies until 1 year?
Many mommies think that no sugar for babies also means no sweet foods for babies and refrain from giving nutritious fruits for their little ones.
By sugar, we always mean the “White Refined Sugar” not the natural sweetness of fruits and natural sweeteners.
Why is sugar harmful to Babies below 1 year?
1. Sugar is refined by lot of chemical processes which may be harmful to children.
2. Excess sugar may cause caries and tooth decay in children.
3. Excess of sugar may depress immunity.
4. Research has also shown that children fed with high sugar diet were prone to cardiovascular, diabetes and obesity.
What to substitute for sugar in baby foods?
Although your baby doesn’t need sweetening of foods daily, you can add natural sweeteners to Kheers, Porridges, baby-friendly cakes, and desserts.
Natural Sweeteners for Baby food
1. Any fruit can be added to baby food to make them naturally sweet
2. Dates Syrup (After 8 months)
3. Honey (After 1 year)
Learn more about Natural sweeteners for Baby Food
Also, if your baby has recently started on solids, you might also be wondering what kind of feeding chair is best for your baby. Check out our detailed post – High Chair Vs Booster Seat: Your Ultimate Guide to Buying a Feeding Chair.Hope your doubts regarding the No Salt and Sugar theory is resolved now, do comment below for any other queries that need answers.

Do follow us on Facebook, Twitter, Pinterest and Google+ for more such informative updates.
To receive the updates directly to your inbox, sign for our newsletter for free Here. We promise not to spam your inbox 🙂
Reference
1. World Action on Salt / Salt and Children Health
2. Scientific Advisor Commission on Nutrition gov.uk
3. How much salt do babies and children need? NHS
4. Effects of salt overload on Kidneys
5. Harmful effects of Sugar
Buy Healthy Nutritious Baby, Toddler food made by our own Doctor Mom !
Shop now!From what age can salt and sugar be given to a child | The benefits and harms of salt and sugar in baby food
Salt and sugar are quite controversial foods in the diet of even an adult. But what about the nutrition of children, especially the smallest - babies up to a year old?
Everyone knows that taste preferences and eating habits are developed in a person from early childhood - from the moment the first complementary foods are introduced. And the main task of parents during this period is to instill in the child a love for the natural taste of products, not to provoke the development of taste buds in only one zone, for example, sweet and salty.
And the main task of parents during this period is to instill in the child a love for the natural taste of products, not to provoke the development of taste buds in only one zone, for example, sweet and salty.
Salt and sugar for children under one year old
Many mothers and fathers worry that without the introduction of sugar and salt, the child will not receive sucrose, which gives energy and mineral salts necessary for cellular metabolism. However, this is a big misconception, as scientists nutritionists have long proven, sucrose is absolutely not needed for children under one year old. Healthy sugars should get into the children's body in the form of fructose, which is found in fruits and vegetables.
As for salt, the product that we see on the shelves of stores with the inscription "Table salt" is again not the salt that a growing body needs. Mineral salts involved in every metabolic process of our body are the most complex substances in terms of their chemical composition. Here are just some of the components of these compounds - sodium chloride (salt itself), zinc, copper, manganese, iodine, selenium, etc. - and all these trace elements are found in complementary foods (vegetables, meat, fish, and others), and can fully cover the daily need of the child's body.
Here are just some of the components of these compounds - sodium chloride (salt itself), zinc, copper, manganese, iodine, selenium, etc. - and all these trace elements are found in complementary foods (vegetables, meat, fish, and others), and can fully cover the daily need of the child's body.
That is why Materna dairy and dairy-free baby food does not contain refined sugars and table salt. The required amount of nutrients and trace elements of Materna nutrition is calculated taking into account the age needs of the child. Materna infant formulas for babies of the first year of life are as close as possible in composition to mother's milk and are enriched with additional components for comfortable digestion and full growth of the child.
Sugar in baby food
The need for sugar in a child up to a year is only 4 g (slightly less than a teaspoon). Babies up to 4-6 months of age receive easily digestible sugars from mother's milk or formula. Since the introduction of complementary foods, natural sugars of vegetables and fruits, juices are added.
It is advisable to add refined white sugar to children after a year, in an amount of not more than 6 g per day (full teaspoon). Use it to sweeten sour fruit drinks, when baking fruits, in desserts or pastries.
Too early or too much sugar in a child's diet leads to a number of problems:
- fermentation processes in the intestines increase, which provokes bloating and painful colic. Products of incomplete protein breakdown from the intestine are absorbed into the bloodstream, thereby causing allergic reactions;
- excess sugar is deposited in fat depots, prerequisites for the development of obesity, diabetes mellitus and changes in the central nervous system appear;
- tooth enamel is destroyed;
- interferes with proper nutrition: sweetened food creates an “illusion” of satiety in a child, therefore, having eaten quite a bit, for example, sweet porridge or cookies, he will refuse the main meal;
- sugar in children is addictive! No matter how scary it sounds, but this pattern has been repeatedly proven: a child, receiving a portion of glucose, experiences an emotional upsurge, he is cheerful and active, but as soon as the blood sugar level drops to normal, lethargy and boredom will set in, so the child will begin to ask himself, and then demand sweets.

Materna Sugar Free Infant Formula does not have these drawbacks.
Salt in the diet of children under one year old
The stereotype that has been strengthened over the years that the human body without salt can get serious functional disorders, and to this day encourages young mothers to add salt to complementary foods for their beloved child. But is salt really necessary for children under one year old? Many pediatricians agree that the child receives all the necessary mineral salts from milk nutrition or complementary foods without the addition of common table salt.
The daily salt requirement for a child up to a year is 0.3 g (after a year 0.5 g). Before the introduction of complementary foods, babies receive all this amount from mother's milk or an adapted milk formula. After that, mineral salts of complementary foods are added: from vegetables, fruits, cereals, meat and other foods. If parents want to further “enrich” the child’s diet with salt and add salt to complementary foods, this will create a greater burden on the kidneys (since salt retains fluid) and the child’s pancreas.
Another concern of young parents is the lack of flavor diversity, which is lost in the absence of salt in complementary foods. This myth also needs to be dispelled. The child's taste buds are very poorly developed, and in the first year of life, he does not distinguish the delicate taste of dishes well. But at the same time, if you regularly add salt or sweeten food, the zones of receptors that perceive sweet or salty will begin to develop faster and require more “flavor enhancers”.
Sugar and salt in the diet of young children: impact on health | Skvortsova
1. Poltyrev S.S., Kurtsin I.T. Physiology of digestion. Tutorial. - M .: Higher school; 1980. - 256 p. [Poltyrev SS, Kurtsin IT. Physiologiya pishchevareniya. Educational Posobie. Moscow: Vysshaya shkola; 1980. 256 p. (In Russ).]
2. Vorob'eva E.A., Gubar' A.V., Safyannikova E.B. Anatomy and physiology. Textbook. — M.: Medicine; 1988. - 432 p. [Vorob'eva EA, Gubar' AV, Saf'yannikova EB. Anatomiya i fiziologiya. Uchebnik. Moscow: Meditsina; 1988. 432 p. (In Russ).]
Uchebnik. Moscow: Meditsina; 1988. 432 p. (In Russ).]
3. Arshavsky I.A. Essays on age physiology. — M.: Medicine; 1967. - 474 p. [Arshavskii IA. Ocherki po vozrastnoi fiziologii. Moscow: Meditsina; 1967. 474 p. (In Russ).]
4. Liley AW. Disorders of amniotic fluid. In: Assali NS, editor. Pathophysiology of gestation. Vol. 2. New York: Academic Press; 1972. p. 157–206.
5. Mennella JA, Jagnow CP, Beauchamp GK. Prenatal and postnatal flavor learning by human infants. Pediatrics. 2001;107(6):E88. doi:10.1542/peds.107.6.e88.
6. Beauchamp GK, Mennella JA. Flavor perception in human infants: development and functional significance. Digestion. 2011; 83 Suppl 1:1–6. doi: 10.1159/000323397.
7. Steiner JE, Glaser D, Hawio ME, Berridge KC. Comparative expression of hedonic impact: affective reactions to taste by human infants and other primates. Neurosci Biobehav Rev. 2001;25(1): 53–74. doi: 10.1016/S0149-7634(00)00051-8.
8. Zakharova I.N., Sugyan N. G., Dmitrieva Yu.A., Svintsitskaya V.I. Taste preferences in young children: what determines them? // Questions of modern pediatrics. - 2015. - T. 14. - No. 6 - S. 706–709. [Zakharova IN, Sugyan NG, Dmitrieva YA, Svintsitskaya VI. Taste preferences in infants: what defines them? current pediatrics. 2015;14(6):706–709. (In Russ).] doi: 10.15690/vsp.v14i6.1480.
G., Dmitrieva Yu.A., Svintsitskaya V.I. Taste preferences in young children: what determines them? // Questions of modern pediatrics. - 2015. - T. 14. - No. 6 - S. 706–709. [Zakharova IN, Sugyan NG, Dmitrieva YA, Svintsitskaya VI. Taste preferences in infants: what defines them? current pediatrics. 2015;14(6):706–709. (In Russ).] doi: 10.15690/vsp.v14i6.1480.
9. Beauchamp GK, Cowart BJ, Moran M. Developmental changes in salt acceptability in human infants. DevPsychobiol. 1986;19(1): 17–25. doi: 10.1002/dev.4201
.
10. Schwartz C, Issanchou S, Nicklaus S. Developmental changes in the acceptance of the five basic tastes in the first year of life. Br J Nutr. 2009;102(9):1375–1385. doi: 10.1017/S0007114509990286.
11. Stein LJ, Cowart BG, Beauchamp GK. Salty taste acceptance by infants and young children is related to birth weight: longitudinal analysis of infants within the birth normal weight range. Eur J Clinic Nutr. 2006;60(2):272–279. doi: 10.1038/sj.ejcn.1602312.
12. Stein LJ, Cowart BJ, Beauchamp GK. The development of salty taste acceptance is related to dietary experience in human infants: a prospective study. Am J Clinic Nutr. 2012;95(1):123–129. doi: 10.3945/ajcn.111.014282.
13. Sucrose. In: Great Soviet Encyclopedia. — M.; 1976. - V.23. — P. 14. [Sakharoza. In: Bol’shaya sovetskaya entsiklopediya. Vol. 23. Moscow; 1976.p. 14. (In Russ).]
14. Sugar industry. In: Great Soviet Encyclopedia. — M.; 1976. - T.23. — S. 12. [Sakharnaya promyshlennost’. In: Bol’shaya sovetskaya entsiklopediya. Vol. 23. Moscow; 1976.p. 12. (In Russ).]
15. Zbarsky B.I., Ivanov I.I., Mardashev S.R. Biological chemistry. - L .: Medicine; 1972. - 582 p. [Zbarskii BI, Ivanov II, Mardashev SR. Biological khimiya. Leningrad: Meditsina; 1972. 582 p. (In Russ).]
16. Baby food. A Guide for Physicians, ed. 3 / Ed. V.A. Tutel'yana, I.Ya. Horse. — M.: MIA; 2013. — S. 75–82. [Children's food. Rukovodstvo for dlya vrachei. 3d edn. Ed by Tutel'yan V. A., Kon' I.Ya. Moscow: MIA; 2013. p. 75–82. (In Russ).]
A., Kon' I.Ya. Moscow: MIA; 2013. p. 75–82. (In Russ).]
17. Skurikhin I.M. Tutelyan V.A. Tables of the chemical composition and calorie content of Russian food products. Directory. — M.: DeLi print; 2008. - 276 p. [Skurikhin IM, Tutel'yan VA. Tablitsy khimicheskogo sostava i kaloriinosti rossiiskikh produktov pitaniya. Reference book. Moscow: DeLi print; 2008. 276 p. (In Russ).]
18. Reference tables of amino acids, fatty acids, vitamins, macro- and microelements, organic acids and carbohydrates / Ed. THEM. Skurikhin and M.N. Volgarev. — M.: Agropromizdat; 1987. - 360 p. [Spravochnye tablitsy soderzhaniya aminokislot, zhirnykh kislot, vitaminov, makro-i mikroelementov, organicheskikh kislot i uglevodov. Ed by Skurikhin I.M., Volgarev M.N. Moscow: Agropromizdat; 1987. 360 p. (In Russ).]
19. Fushan AA, Simons CT, Slack JP, et al. Allelic polymorphism within the TAS1R3 promoter is associated with human taste sensitivity to sucrose. Curr Biol. 2009;19(15):1288–1293. doi: 10.1016/j.cub.2009.06.015.
doi: 10.1016/j.cub.2009.06.015.
20. Dias AG, Eny KM, Cockburn M, et al. Variation in the TAS1R2 gene, sweet taste perception and intake of sugars. J Nutrigenet Nutrigenomics. 2015;8(2):81–90. doi: 10.1159/000430886.
21. Mennella JA, Nicklaus S, Jagolino AL, Yourshaw LM. Variety is the spice of life: strategies for promoting fruit and vegetable acceptance during infancy. Physiol Behav. 2008;94(1):29–38. doi: 10.1016/j.physbeh.2007.11.014.
22. Beauchamp GK, Mennella JA. Early flavor learning and its impact on later feeding behavior. J Pediatr Gastroenterol Nutr. 2009; 48 Suppl 1:S25–30. doi: 10.1097/MPG.0b013e31819774a5.
23. Birch LL, Doub AE. Learning to eat: birth to age 2 y. Am J Clinic Nutr. 2014;99(3):723S–728S. doi: 10.3945/ajcn.113.069047.
24. Gibson E L, Wardle J. Energy density predicts preferences for fruit and vegetables in 4-year-old children. Appetite. 2003;41(1):97–98. doi: 10.1016/S0195-6663(03)00077-1.
25. National program for optimizing the feeding of children in the first year of life in the Russian Federation. — M.; 2011. - 68 p. [Natsional'naya programma optimizatsii vskarmlivaniya detei pervogo goda zhizni v Rossiiskoi Federatsii. Moscow; 2011. 68 p. (In Russ).]
— M.; 2011. - 68 p. [Natsional'naya programma optimizatsii vskarmlivaniya detei pervogo goda zhizni v Rossiiskoi Federatsii. Moscow; 2011. 68 p. (In Russ).]
26. Baby food. A Guide for Physicians / Ed. V.A. Yana Tutel, I.Ya. Horse. — M.: MIA; 2009. 945 p. [Children's food. Rukovodstvo for dlya vrachei. Ed by Tutel'yan V.A., Kon' I.Ya. Moscow: MIA; 2009. 945 p. (In Russ).]
27. Martinchik A.N., Maev I.V., Petukhov A.B. Human Nutrition (Fundamentals of Nutrition) / Ed. A.N. Martinchik. - M .: GOU VUNMTs of the Ministry of Health of the Russian Federation; 2012. - 576 p. [Martinchik AN, Maev IV, Petukhov AB. Pitanie cheloveka (osnovy nutritsiologii). Ed by Martinchik A.N. Moscow: GOU VUNMTs MZ RF; 2012. 576 p. (In Russ).]
28. Blass EM, Watt LB. Suckling- and sucrose-induced analgesia in human newborns. Pain. 1999;83(3):611–623. doi: 10.1016/s0304-3959(99)00166-9.
29. Harrison D, Stevens B, Bueno M, et al. Efficacy of sweet solutions for analgesia in infants between 1 and 12 months of age: a systematic review. Arch DisChild. 2010;95(6):406–413. doi: 10.1136/adc.2009.174227.
Arch DisChild. 2010;95(6):406–413. doi: 10.1136/adc.2009.174227.
30. Pepino MY, Menella JA. Sucrose-induced analgesia is related to sweet preferences in children but not adults. Pain. 2005; 119(1–3):210–218. doi: 10.1016/j.pain.2005.09.029.
31. Lucey P, Howlett J, Corn J, et al. Improving pain recognition through better utilization of temporal information. Int Conf Audit Vis Speech Process. 2008;2008:167–172.
32. Howlett J, Ashwell M. Glycemic response and health: summary of a workshop. Am J Clinic Nutr. 2008;87(1):212S–216S.
33. Fomon SJ. Feeding normal infants: rationale for recommendations. J Am Diet Assoc. 2001;101(9):1002–1005. doi: 10.1016/S0002-8223(01)00248-6.
34. Mattes RD, Shikany JM, Kaiser KA, Allison DB. Nutritively sweetened beverage consumption and body weight: a systematic review and meta-analysis of randomized experiments. Obes Rev. 2011;12(5):346–365. doi: 10.1111/j.1467-789X.2010.00755.x.
35. Stephen A, Alles M, de Graaf C, et al. The role and requirements of digestible dietary carbohydrates in infants and toddlers. Eur J Clinic Nutr. 2012;66(7):765–779. doi: 10.1038/ejcn.2012.27.
The role and requirements of digestible dietary carbohydrates in infants and toddlers. Eur J Clinic Nutr. 2012;66(7):765–779. doi: 10.1038/ejcn.2012.27.
36. Grimes CA, Riddell LJ, Campbell KJ, Nowson CA. Dietary salt intake, sugar-sweetened beverage consumption, and obesity risk. Pediatrics. 2013;131(1):14–21. doi: 10.1542/peds.2012-1628.
37. Guseva I.M. Features of catering and physical development of children from 1 to 3 years (on the example of the cities of the Central Federal District of the Russian Federation): author. dis. … cand. honey. Sciences. — M.; 2015. - 24 p. [Guseva IM. Osobennosti organizatsii pitaniya i fizicheskoe razvitie detei ot 1 to 3 let (na primere gorodov Tsentral’nogo federal’nogo okruga Rossiiskoi Federatsii). [dissertation abstract] Moscow; 2015. 24 p. (In Russ).]
38. Netrebenko O.K. Metabolic programming in the antenatal period // Issues of gynecology, obstetrics and perinatology. - 2011. - T. 11. - No. 6 - S. 58–65. [Netrebenko OK. Metabolic programming in the antenatal period. Problems of gynecology, obstetrics, and perinatology. 2012;11(6):58–64. (In Russ).]
Metabolic programming in the antenatal period. Problems of gynecology, obstetrics, and perinatology. 2012;11(6):58–64. (In Russ).]
39. Sarr O, Yang K, Regnault T. In utero programming of later adiposity: the role of fetal growth restriction. J Pregnancy. 2012; 2012:134758. doi: 10.1155/2012/134758.
40. Khodzhieva M.V., Skvortsova V.A., Borovik T.E. Modern views on the development of overweight and obesity in children // Pediatric pharmacology. - 2015. - T. 12. - No. 5 - S. 67–71. [Khodzhiyeva MV, Skvortsova VA, Borovik TE, et al. Contemporary views on the development of excess body weight and obesity in children. Part I. Pediatric pharmacology. 2015;12(5):573–578. (In Russ).] doi: 10.15690/pf.v12i5.1460.
41. Gidding SS, Daniels SR, Kavey RE. Developing the 2011 Integrated Pediatric Guidelines for Cardiovascular Risk Reduction. Pediatrics. 2012;129(5):e1311–1319. doi: 10.1542/peds.2011-2903.
42. Hojak I. Digestible and non-digestible carbohydrates. In: Koletzko B, Bhatia J, Bhutta ZA, et al, editors. Pediatric nutrition in practice. 2nd revised edition. Basel: Karger AG; 2015. p. 46–50.
Pediatric nutrition in practice. 2nd revised edition. Basel: Karger AG; 2015. p. 46–50.
43. Guideline: Sugars intake for adult and children. Geneva: World Health Organization; 2015.
44. Karjalainen S, Soderling E, Sewon L, et al. A prospective study on sucrose consumption, visible plaque and caries in children from 3 to 6 years of age. Community Dent Oral Epidemiol. 2001;29(2): 136–142. doi: 10.1111/j.1600-0528.2001.290208.x.
45. Moynihan PJ, Kelly SA. Effect on caries of sugar intake: systematic review to inform WHO guidelines. J Dent Res. 2014; 93(1):8–18. doi: 10.1177/0022034513508954.
46. National program for optimizing the nutrition of children aged 1 to 3 years in the Russian Federation. - M .: Pediatric; 2016. - 35 p. [Natsional'naya programma optimizatsii pitaniya detei v vozraste ot 1 goda do 3 let v Rossiiskoi Federatsii. Moscow: Pediatr; 2016. 35 p. (In Russ).]
47. Norms of physiological needs for energy and nutrients for various groups of the population of the Russian Federation. MP 2.3.1.2432-08. — M.; 2008. MR 2.3.1. 2432-08. Moscow; 2008. (In Russ).]
MP 2.3.1.2432-08. — M.; 2008. MR 2.3.1. 2432-08. Moscow; 2008. (In Russ).]
48. Bernabe E, Sheiham A. Extent of differences in dental caries in permanent teeth between childhood and adulthood in 26 countries. Int Dent J. 2014;64(5):241–245. doi: 10.1111/idj.12113.
49. Salt industry. In: Great Soviet Encyclopedia. — M.; 1976. - T. 24. - S. 166-167. [Solyanaya promyshlennost’. In: Bol’shaya sovetskaya entsiklopediya. Vol. 24 Moscow; 1976.p. 166–167. (In Russ).]
50. Table salt. In the book: Great Medical Encyclopedia / Ed. K.S. Petrovsky. — M.; 1984. - T. 20. - S. 29-30. [Sol' povarennaya. In: Bol'shaya meditsinskaya entsiklopediya. Ed by Petrovskii K.S. Vol. 20 Moscow; 1984. p. 29–30. (In Russ).]
51. Prince EN, Fuchs GJ. fluid and electrolytes. In: Koletzko B, Bhatia J, Bhutta ZA, et al, editors. Pediatric nutrition in practice. 2nd revised edition. Basel: Karger AG; 2015. p. 56–61.
52. Rebrov V.G., Gromova O.A. Vitamins, macro- and microelements. - M: GEOTAR-Media; 2008. - 960 p. [Rebrov VG, Gromova OA. Vitaminy, makro- i mikroelementy. Moscow: GEOTAR-Media; 2008. 960 p. (In Russ).]
- M: GEOTAR-Media; 2008. - 960 p. [Rebrov VG, Gromova OA. Vitaminy, makro- i mikroelementy. Moscow: GEOTAR-Media; 2008. 960 p. (In Russ).]
53. Fleger K, Magner P. Get excess salt out of our diet. CMAJ. 2009;180(3):263–265. doi: 10.1503/cmaj.082050.
54. hc-sc.gc.ca [Internet]. Health Canada. Sodium targets for Canadian Foods - Information on upcoming meetings. 2009 [cited 2016 Sep 9]. Available from: http://www.hc-sc.gc.ca/fn-an/legislation/index-eng.php.
55. Barr S. Reducing dietary sodium intake: the Canadian context. Appl Physiol Nutr Metab. 2010;35(1):1–8. doi: 10.1139/H09-126.
56. Kwak MK, Choi D, Lee J, et al. Relationship between decrease in serum sodium level and bone mineral density in osteoporotic fracture patients. J Bone Metab. 2015;22(1):9-fifteen. doi: 10.11005/jbm.2015.22.1.9.
57. WHO. Guideline: Sodium intake for adults and children. Geneva: World Health Organization; 2012. 56 p.
58. Strazzullo P, D'Elia L, Kandala NB, Cappuccio FP. Salt intake stroke, and cardiovascular disease: a meta-analysis of prospective studies. BMJ. 2009;339:b4567. doi: 10.1136/bmj.b4567.
Salt intake stroke, and cardiovascular disease: a meta-analysis of prospective studies. BMJ. 2009;339:b4567. doi: 10.1136/bmj.b4567.
59. WHO. Effect reduced sodium intake on cardiovascular disease, coronary heart disease, and stroke. Geneva: World Health Organization; 2012. 86 p.
60. Grimes CA, Campbell KJ, Riddell LJ, Nowson CA. Sources of sodium in Australian children’s diets and the effect of the application of sodium targets to food products to reduce sodium intake. Br J Nutr. 2011;105(3):468–477. doi: 10.1017/S0007114510003673.
61. Bouhlal S, Issanchou S, Nicklaus S. The impact of salt, fat and sugar levels on toddler food intake. Br J Nutr. 2011;105(4): 645–653. doi: 10.1017/S0007114510003752.
62. Heird WC, Ziegler P, Reidy K, Briefel R. Current electrolyte intakes of infants and toddlers. J Am Diet Assoc. 2006;106(1 Suppl 1):S43–51. doi:10.1016/j.jada.2005.09.043.
63. Maalouf J, Cogswell ME, Yuan K, et al. Top sources of dietary sodium from birth to age 24 mo, United States, 2003–2010. Am J Clinic Nutr. 2015;101(5):1021–1028. doi: 10.3945/ajcn.114.099770.
Am J Clinic Nutr. 2015;101(5):1021–1028. doi: 10.3945/ajcn.114.099770.
64. Elliott CD. Sweet and salty: nutritional content and analysis of baby and toddler foods. J Public Health (Oxf). 2011;33(1):63-70. doi: 10.1093/pubmed/fdq037.
65. Institute of Medicine. Dietary reference intakes for water, potassium, sodium, chloride, and sulfate. Washington, DC: National Academies Press; 2005. 640 p.
66. Vitamins and minerals. From A to Z. - St. Petersburg: Neva; 2006. - 640 p. [Vitamin and mineral. From A to Ya. St. Petersburg: Neva; 2006. 640 p. (In Russ).]
67. Unified sanitary-epidemiological and hygienic requirements for goods subject to sanitary-epidemiological supervision No. 299 dated October 28, 2010, as amended. — M.; 2010. [Edinye sanitarno-epidemiologicheskie i gigienicheskie trebovaniya k tovaram, podlezhashchim sanitarnoepidemiologicheskomu nadzoru ot 28.10.2010 goda No. 299 s changes. Moscow; 2010. (In Russ).]
68. Technical regulation for fruit and vegetable juice products (TR TS 021/2011) dated 09.