Should i keep feeding my baby if she spits up
How to Know Whether You Should
Your baby just threw up all the milk they’ve chugged down so far, and you’re wondering if it’s OK to continue feeding. How soon should you feed your baby after vomiting?
It’s a good question — just about every parent has likely pondered this. Spit-up is almost a rite of passage for babies (and parents). Baby vomiting is also common and can happen for many reasons. Most of the causes aren’t serious.
The short answer — because you may have a very fussy baby on your hands and want to get back to them ASAP — is yes, you can usually feed your baby after they vomit all over your favorite sweater, sofa throw, and rug.
Here’s just about everything you need to know about feeding your baby after vomiting.
Baby vomit and spit-up are two different things — and they can have different causes. Spitting up is common in babies under the age of 1 year. It typically happens after feeding. Spit-up is usually an easy flow of milk and saliva that dribbles from your baby’s mouth. It often happens with a burp.
Spit-up is normal in healthy babies. It can happen for several reasons. About half of all babies 3 months and under have a type of acid reflux called infant reflux.
Spit-up from infant reflux is especially bound to happen if your baby has a full stomach. Being careful not to overfeed a bottle-fed infant can help. Spitting up typically stops by the time your baby is a year old.
On the other hand, vomiting is typically a more forceful throwing-up of milk (or food, if your baby is old enough to eat solids). It happens when the brain signals the muscles around the stomach to squeeze.
Vomiting (like gagging) is a reflex action that can be triggered by a number of things. These include:
- irritation from a viral or bacterial infection, like the stomach bug
- fever
- pain, such as from a fever, earache, or vaccination
- blockage in the stomach or intestines
- chemicals in the blood, like medicine
- allergens, including pollen; very uncommon in babies under 1 year
- motion sickness, such as during a car ride
- dizziness, which might happen after being twirled around too much
- being upset or stressed
- strong smells
- milk intolerance
Vomiting is also common in healthy babies, but it might mean that your baby has caught a bug or is feeling a bit under the weather.
Too much vomiting can cause dehydration and even weight loss in very serious cases. Milk feeding can help prevent both of these. Offer your baby a feeding after they’ve stopped throwing up. If your baby is hungry and takes to the bottle or breast after vomiting, go right ahead and feed them.
Liquid feeding after vomiting can sometimes even help settle your baby’s nausea. Start with small amounts of milk and wait to see if they vomit again. Your baby might vomit the milk right back up, but it’s better to try than not.
If your little one is at least 6 months old and doesn’t want to feed after throwing up several times, offer them water in a bottle or a spoon. This can help prevent dehydration. Wait a short while and try feeding your baby again.
In some cases, it’s better not to feed a baby right after vomiting. If your baby is throwing up because of an earache or fever, they may benefit from medication first.
Most pediatricians recommend pain medications like infant Tylenol for babies in their first year. Ask your doctor about the best medication and dosage for your baby.
Ask your doctor about the best medication and dosage for your baby.
If giving pain medication based on your doctor’s advice, wait about 30 to 60 minutes after doing so to feed your little one. Feeding them too soon might cause another bout of vomiting before the meds can work.
Motion sickness isn’t common in babies under the age of 2 years, but some babies may be more sensitive to it. If your baby vomits from motion sickness, it’s better not to offer a feeding afterward.
You’re in luck if your baby likes to nod off in the car. Wait until you’re out of the car to feed your baby milk.
Baby vomiting can be worrying, but it usually goes away by itself — even if your baby has the stomach bug. Most babies with gastroenteritis don’t need medical treatment. This means that most of the time, you’ll have to bravely wait out your baby’s vomiting.
But sometimes, throwing up is a sign that something’s not right. You know your baby best. Trust your gut and call their doctor if you feel your little one is unwell.
In addition, take your baby to a doctor immediately if they’ve been vomiting for 12 hours or longer. Babies and children can dehydrate quickly from too much vomiting.
Also call your baby’s pediatrician if your baby can’t hold anything down and has signs and symptoms of being unwell. These include:
- constant crying
- pain or discomfort
- refusal to feed or drink water
- diaper that hasn’t been wet for 6 hours or longer
- diarrhea
- dry lips and mouth
- crying without tears
- extra sleepiness
- floppiness
- vomiting blood or fluid with black flecks (“coffee grounds”)
- lack of smile or response
- vomiting green fluid
- bloated tummy
- blood in bowel movements
You won’t usually have any control over when or how much your baby vomits. When it happens on occasion, repeat this mantra to help you cope: “Healthy babies sometimes vomit.”
However, if your baby often vomits (or spits up) after feeding, you may be able to take some preventative steps. Try these tips:
Try these tips:
- avoid overfeeding
- give your baby smaller, more frequent feeds
- burp your baby often between feeds and after feeds
- prop up your baby so they’re upright for at least 30 minutes after feeding (but don’t prop your baby up for sleep or use anything to position them in their crib or elevate their mattress)
If your baby has a tummy bug and is old enough to eat solid foods, avoid feeding solids for about 24 hours. A liquid diet can help the stomach settle after a bout of vomiting.
Vomiting and spit-up are common in healthy babies. In most cases, you can milk feed shortly after your baby vomits. This helps to prevent your baby from getting dehydrated.
In some cases it’s best to wait a little while before trying to feed your baby again. If you’re giving your child medication like pain and fever relievers, wait a bit so the meds don’t come back up.
If your baby is vomiting a lot or seems otherwise unwell, call your pediatrician immediately. If you’re unsure if your baby’s vomiting or spit-up is cause for concern, it’s always best to check with your doctor.
If you’re unsure if your baby’s vomiting or spit-up is cause for concern, it’s always best to check with your doctor.
Breastfeeding FAQs: Spitting Up, Gagging, and Biting (for Parents)
Breastfeeding is natural, but it takes practice to get it right. Here's what you need to know about spitting up, gagging, and other concerns during breastfeeding.
Is it Normal for My Baby to Spit Up After Feedings?
Sometimes, babies spit up when they eat too much, or when they burp or drool. Many infants will spit up a little after some — or even all — feedings or during burping because their digestive systems are immature. That's perfectly normal.
As long as your baby is growing and gaining weight and doesn't seem uncomfortable with the spitting up, it's OK. The amount of spit-up often looks like more than it actually is. But spitting up isn't the same as forcefully vomiting all or most of a feeding.
What’s the Difference Between Spitting Up and Vomiting?
Vomiting is a forceful projection of stomach fluids. Spitting up is a more gentle "flow" of fluids that come up. Babies don’t usually react to spitting up, but a vomiting baby will usually look upset or cry.
Spitting up is a more gentle "flow" of fluids that come up. Babies don’t usually react to spitting up, but a vomiting baby will usually look upset or cry.
If you're concerned that your baby is vomiting, call your doctor. In rare cases, there may be an allergy, digestive problem, or other problem that needs medical care. It helps to keep track of how often and how much your baby is vomiting or spitting up.
How Can I Keep My Baby From Spitting Up?
If the doctor says your baby's spitting up is normal, here are some things you can do to help lessen it:
- Burp your baby after each feed from each breast. Sometimes giving smaller feeds more often can help, rather than giving larger-volume feeds.
- Keep your baby upright after feedings for at least 30 minutes. Holding your baby is best, since the way your baby sits in an infant seat may actually make spitting up more likely.
- Don't jiggle, bounce, or actively play with your baby right after feedings.

- Keep your baby's head above the feet while feeding. Don't hold your baby in a dipped-down position when feeding.
- Raise the head of your baby's crib or bassinet. Roll up a few small hand towels or receiving blankets (or you can buy special wedges) to place under — not on top of — the mattress. Never use a pillow under your baby's head. Make sure the mattress doesn’t fold in the middle, and that the incline is gentle enough that your baby doesn’t slide down.
If your baby also gets bottles of breast milk or infant formula supplements:
- Burp after your baby drinks 1–2 ounces from a bottle.
- Don't give the bottle while your little one is lying down.
- Make sure the hole in the nipple is the right size and/or flow for your baby. For example, fast-flow nipples may cause babies to gag or may give them more milk than they can handle at once.
 Many breastfed babies do well with the slow-flow nipple until they are 3 months old, or even older.
Many breastfed babies do well with the slow-flow nipple until they are 3 months old, or even older.
Many babies outgrow spitting up by the time they're sitting up.
How Can I Keep My Baby From Gagging?
Sometimes the force of your milk (especially when it “lets down”) is so strong that it can cause your baby to gag and pull off of the breast. If this happens during feeding:
- Try nursing your baby in a more upright position (head above the breast). This may ease the force of the milk.
- Nurse in a side-lying position, which also might help slow the flow of milk.
- Make sure your breasts are not engorged or over-full. Nursing every 2–3 hours can help prevent engorgement. If your breasts are too full and you’re concerned about a forceful letdown, express or pump a little bit of milk a few minutes before feeding time to avoid a strong letdown.
If your baby is pulling off and gagging or coughing during feeding, sit your baby up in a seated burp position. Gently pat the back to help your baby calm down before continuing feeding. If you’ve tried the steps above and this continues to happen, talk to your doctor or lactation consultant.
Gently pat the back to help your baby calm down before continuing feeding. If you’ve tried the steps above and this continues to happen, talk to your doctor or lactation consultant.
If your baby sometimes gags or chokes while taking a bottle of breast milk:
- Try a different nipple with a slower flow.
- Practice “paced” bottle feeding. This is where you slow down the milk flow from the bottle by holding it at less of an angle and allowing your baby to pause for breaks.
My Baby Bites During Breastfeeding. What Can I Do?
Babies will often play with their mothers' nipples with their gums, not meaning to cause any harm. But once they start teething, a baby might bite down, not knowing this is hurting mom.
Sometimes you can tell when your baby's about ready to bite down — usually when satisfied and starting to pull away from the breast. When you sense that your baby is finished feeding and may be bored or feeling playful, end the feeding. Break the suction by slipping your finger into the corner of your baby’s mouth.
Break the suction by slipping your finger into the corner of your baby’s mouth.
If your baby is already biting down, pull your baby closer to you to make it more difficult to pull off easily. Then, break the suction. React calmly without raising your voice.
Here are more ways to make baby less likely to bite:
- Before a feed, give your baby something to chew on. Make sure it's big enough that it can't be swallowed or choked on and that it can't break into small pieces. A wet washcloth placed in the freezer for 30 minutes makes a handy teething toy. Be sure to take it out of the freezer before it becomes rock hard — you don't want to bruise those already swollen gums. Wash after each use.
- Say, "Mommy is not for biting. You can bite this." Then, offer your little one a teething toy or ring.
- Praise your baby — with a hug, kiss, or cuddle — whenever they nurse without biting or trying to bite.
Usually this is enough to stop the biting, but if your baby continues, talk to your doctor or lactation consultant for advice.
Reviewed by: Jamila H. Richardson, BSN, RN, IBCLC
Date reviewed: January 2021
How to help the baby when regulating
Support icon ofKeywords for searching
Home ›!! How to help a child in sprinkling
Home Home ›!! How to help a child in regurgitation
↑ Verki
Breastal feeding - completely special time for mom and her newborn baby. Together with the feeling of closeness and affection that feeding brings, understanding its nuances cannot but raise many questions, including the question of how to help an infant spit up. Regurgitation in a newborn is by no means always the result of a simple pat on his back.
In this article, we'll talk about the basics of helping a newborn spit up, as well as other questions you may have about spitting up.
Why do babies spit up?
Let's get it straight: why do newborns need to burp in the first place? During feeding, children usually swallow extra air - this is called aerophagy. Spitting up helps prevent this air from entering the intestines, as well as vomiting, gas, and crankiness in the baby. To avoid the return of milk after feeding, you should give the baby the opportunity to burp more often.
Spitting up helps prevent this air from entering the intestines, as well as vomiting, gas, and crankiness in the baby. To avoid the return of milk after feeding, you should give the baby the opportunity to burp more often.
How to help a newborn spit up?
During the first six months, the baby should be kept upright in a column for 10-15 minutes after each feed. This will help keep the milk in his stomach, but if the baby occasionally burps anyway, parents need not worry. While carrying your baby in an upright position, you can put a baby diaper or wipes on your shoulder to keep your clothes clean.
We've already seen why spitting up is important, now let's find out how to help your baby spit up. Parents should gently pat the baby on the back with a hand folded in a handful until he burps. Folding your hand into a handful is important because clapping with a flat palm may be too strong for an infant.
Every baby is different and there is no one right position for spitting up. To get started, you can try the following options:
To get started, you can try the following options:
- Sitting position with the baby on the chest. In this position, the parent puts the baby's head with his chin on his shoulder and with one hand supports the baby under the back. With the other hand, you can gently pat the baby on the back. This method is most effective in a rocking chair or when the baby is gently rocking.
- Holding the child upright on your legs. With one hand, parents can hold the baby by the back and head, supporting his chin and placing his palm on the baby’s chest, with the other hand, you can gently pat him on the back. At the same time, it is important to be careful: do not press the child on the throat, but only gently support his chin.
- Holding a baby on your lap while lying on your tummy. Make sure his head is above his chest and gently pat your baby on the back until he burps.
Here are some tips on how best to help your newborn spit up:
- Let your baby spit up during feeding.
 If the baby is restless or has swallowed air, it is worth giving him the opportunity to burp during feeding, and not just after.
If the baby is restless or has swallowed air, it is worth giving him the opportunity to burp during feeding, and not just after. - When bottle feeding, let the newborn burp after every 50-60 ml.
- When breastfeeding, let the baby burp at every breast change.
It is important to let your baby spit up after eating, even if he spit up during feeding!
If your baby is gassy, spit up more often. Also, if he vomits frequently or suffers from gastroesophageal reflux disease (GERD), have him spit up after every 30 ml bottle-feeding or every five minutes while breastfeeding.
How long should a baby be held for it to burp? It's different for everyone, but generally keeping a newborn upright for 15 to 20 minutes after a feed helps the milk stay in the baby's stomach.
Minimize the amount of air you swallow. Gas production and regurgitation result from aerophagia during feeding. The baby will inevitably swallow air, but there are ways to prevent it from swallowing too much. Whether you bottle feed your baby or combine breastfeeding with bottle feeding, the Philips Avent anti-colic bottle with AirFree valve is designed so that the nipple is always filled with milk without excess air, even in a horizontal position, thus preventing the baby from swallowing excess air during feeding.
Whether you bottle feed your baby or combine breastfeeding with bottle feeding, the Philips Avent anti-colic bottle with AirFree valve is designed so that the nipple is always filled with milk without excess air, even in a horizontal position, thus preventing the baby from swallowing excess air during feeding.
Reducing the amount of air your baby swallows can help reduce your baby's risk of colic, gas, and spitting up.
Breastfeeding is a wonderful time to strengthen the bond between parent and baby. Every mom and every baby is different, so learning to help your newborn burp properly can take time and practice.
Articles and tips from Philips Avent
Baby+ app
Download the app and track your child's development and growth with trackers, and keep those special moments forever.
Download app:
You are leaving the Philips Healthcare (“Philips”) official website. Any links to third party websites that may be included on this site are provided solely as a convenience to you. Philips makes no warranties regarding any third party websites or the information they contain.
Philips makes no warranties regarding any third party websites or the information they contain.
I understand
You are about to visit a Philips global content page
Continue
You are about to visit the Philips USA website.
I understand
Regurgitation in babies
Regurgitation in children is associated with the anatomical features of this age. The newborn eats liquid food, is in a horizontal position most of the time, has a relatively high intra-abdominal pressure and weak muscles. This indicates a tendency to burp, but does not "oblige" them. The amount of regurgitation is very individual. In some children, this phenomenon is observed constantly, and some spit up so rarely that they scare their parents with it. However, there is a medical name for belching, gastroesophageal reflux. From the point of view of medicine, this is a passive reflux of gastric contents into the esophagus and oral cavity. If there is such a term, then the condition requires attention from parents. What should it be and what should be regarded as an alarm signal?
If there is such a term, then the condition requires attention from parents. What should it be and what should be regarded as an alarm signal?
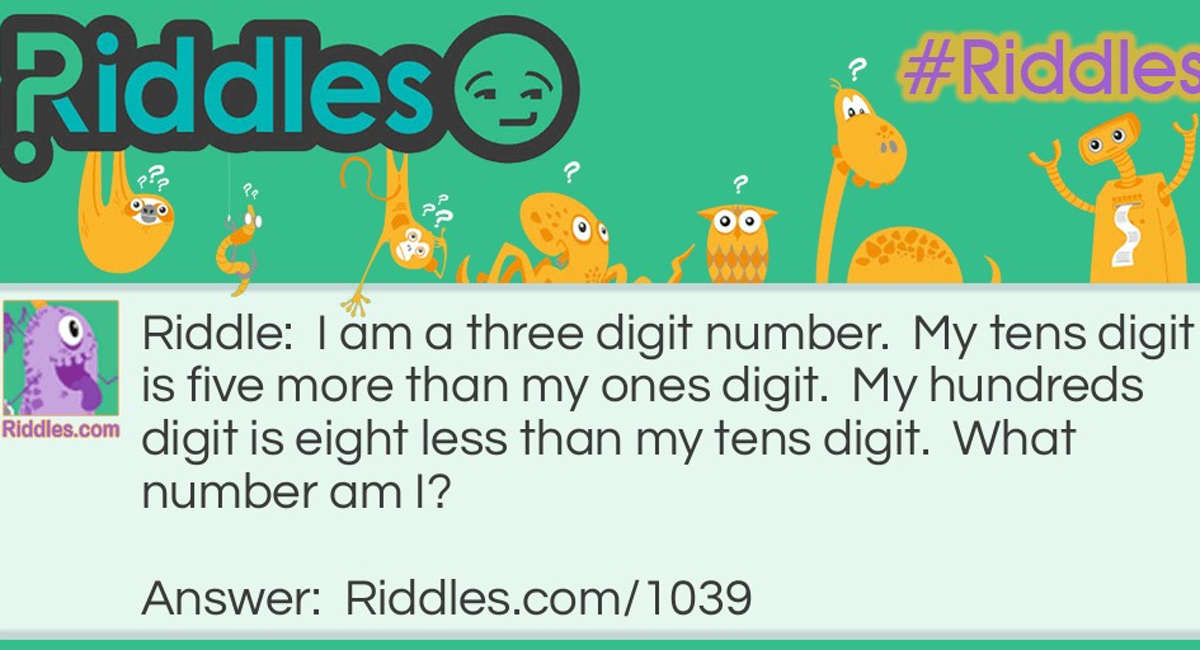
Key facts
Here are 4 postulates that all parents should remember:
- Reflux occurs in almost all children.
- The first eructations appear at the age of 2-3 weeks.
- The most "large-scale" and frequent regurgitation occurs at 4-5 months.
- By the age of one, eructations most often stop.
Why reflux goes away
In order for burping to stop, the full development of the lower esophageal sphincter is necessary. This is facilitated by the physical development of the baby (increased muscle tone), reducing the time spent in a horizontal position, introducing solid food into the diet. Obviously, all this happens naturally - as the child grows up.
How to deal with regurgitation?
The intensity of manifestations of reflux sometimes depends on the actions of the parents. Accordingly, with the help of simple measures, adults can reduce or minimize the frequency as well as the volume of burping. For this you need:
Accordingly, with the help of simple measures, adults can reduce or minimize the frequency as well as the volume of burping. For this you need:
- Do not overfeed. If a child eats more than his stomach can hold, then all the excess will soon come out.
- Observe correct posture. Organize the baby's bed so that the head end is raised. Use a wedge-shaped pillow, and also do not be lazy to scold the crumbs in your arms with a “column” after eating. Make sure that for the next half hour the child is in a position with a slightly raised upper body.
- Avoid activity after meals. Try to organize your leisure time in such a way that the first half hour after the meal passes calmly. Schedule gymnastics and games for a later time.
- Monitor feeding technique. When breastfeeding, it is important to properly attach the baby to the breast. It does not hurt to take breaks in feeding and continue it after belching air. When artificial feeding, use special nipples that prevent swallowing air.
- Change the diet. If the baby burps profusely, it makes sense for the mother to reconsider her own diet. Perhaps the child's body does not accept the substances that she consumes. With artificial feeding, it is worth discussing the issue of regurgitation with a pediatrician. Sometimes you need to change the mixture.
- Change mode. Belching, as a result of overeating, can be eliminated by feeding the baby more often, but in smaller portions.
Isn't it dangerous?
Reflux can be a symptom of a disease. Parents should be alert:
- lack of appetite and complete refusal to eat;
- arching of the back and harsh crying when feeding;
- greenish or bloody masses;
- vomiting "fountain";
- eructations too frequent;
- infrequent urination;
- poor weight gain;
- occurrence of cough, apnea, fever;
- late onset of eructations (after 6 months).