Baby difficult to feed bottle
What to do when baby won’t take a bottle
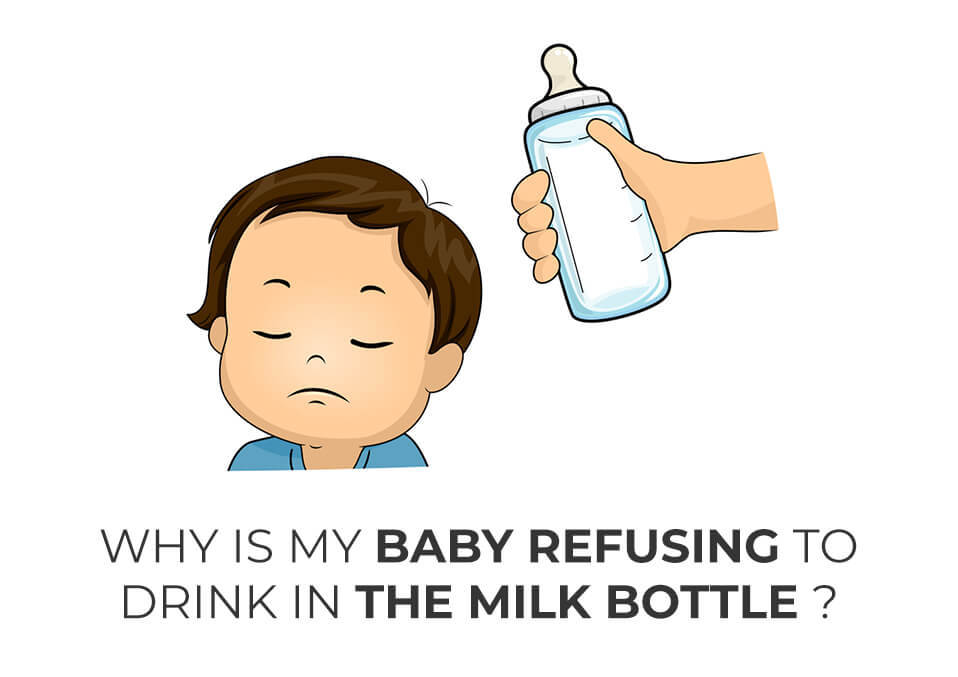
When your breastfed baby won’t take a bottle, it can be stressful and even a little scary. Babies are not always onboard when transitioning from breast to bottle. Whether you’re going back to work or want others to help feed your baby, you might start to wonder: “What if my baby never takes a bottle?”
Don’t panic. Usually when your baby won’t take a bottle, they’re just struggling with the learning curve. They’re new to the world so they have a lot to learn. Sometimes there may be some motor skill or medical condition making it more difficult. But no matter the reason, we’re here to help.
Keep reading to learn the most common reasons why your baby may be refusing a bottle, tips for helping them get used to a bottle, and what may be going on if bottle feeding doesn’t start to improve.
Not all bottle refusal looks the same. There can be a range of signs that your child is struggling to take a bottle, including:
- Turning away from the bottle
- Gagging or fussing as the bottle’s nipple nears their mouth
- Being unable to latch/compress the bottle’s nipple and express milk
- Chewing on the bottle’s nipple
- Sputtering or coughing while feeding
- Not being able to completely swallow their sip of milk, so that some drips from their mouth
Why do many babies have problems when switching to a bottle after breastfeeding?
There’s no one-size-fits-all answer to this question. In most cases, bottle feeding problems aren’t due to abnormal oral motor function, nor are they usually due to an underlying medical issue.
Actually, one of the most common reasons breastfed babies won’t take a bottle right away stems from not being introduced to one early enough in their growth. In fact, the number one mistake families make is offering a bottle too late.
Why timing is so important when introducing a bottle to a breastfed baby
Babies are born with an automatic sucking reflex. But at 2 to 3 months old that reflex becomes voluntary. In effect, that gives babies the ability to turn down a feeding if they’re not comfortable with it.
If a baby hits this stage in their growth and has only fed from their mother’s breast, they may have developed a “preference” for that method of milk delivery. Babies establish a suck-swallow-breathe pattern that works for them and lets them handle their mother’s milk flow.
When given a bottle, not only is the milk flow different, a baby has to adapt to a different nipple shape and texture.![]() They also need to slightly adjust their posture from what they’re used to. For someone so new to the world, making these kinds of changes can be hard and overwhelming, leading to fussing, tears and why your breastfed baby won’t take a bottle.
They also need to slightly adjust their posture from what they’re used to. For someone so new to the world, making these kinds of changes can be hard and overwhelming, leading to fussing, tears and why your breastfed baby won’t take a bottle.
When to introduce a bottle to a breastfed baby
There’s an ideal window of time for introducing a bottle to a breastfed baby. You want to avoid doing it too late, but you also don’t want to do it too early. It’s important to make sure your baby gets the hang of breastfeeding and is getting enough milk before introducing a bottle.
We usually recommend waiting about 2 to 4 weeks after your baby is born before trying to bottle feed. Unless they were born early, most babies are ready by then.
How to get a breastfed baby to take a bottle: 5 helpful tips
1. Switch back and forth between breastfeeding and bottle feeding
You give your baby the best chance at developing their feeding skills if you regularly switch between bottle and breast in the midst of feedings.
2. Try giving the bottle when your baby is waking up
No matter the time of day, babies are more likely to take a bottle when they’re just waking up. The instinct to eat takes over when babies are still a little sleepy. Don’t let your baby get overly hungry before feeding. That can result in fussiness and crying (a late feeding cue), and make it harder to initiate feeding either by bottle or breast.
3. Create a relaxing environment each time you offer the bottle
Play soft, calming music – like classical or folk. Sit down someplace where you can gently rock back and forth. And swaddle your baby with their hands near their face. Having a quiet, dark room with few distractions can help, too.
Doing these things will relax your infant – in part because they will also relax you. Children sense and feed off the energy of the adults around them. And it’s no different when you and your baby are adjusting to bottle feeding. If you can be at ease with the varied routine a bottle brings, your baby will be more content, too.
4. Have a family member other than mom offer the bottle whenever possible
Each person will hold your baby a little bit differently for feedings. When your little one can get used to these differences early, it helps them learn how to adjust their posture so it’s less likely to be an issue when their sucking reflex becomes voluntary.
5. Try giving your baby a different type of bottle or nipple
Sometimes, the solution to bottle feeding problems is as simple as finding the right bottle or nipple. While there are nipple levels associated with age, every baby has their own feeding style, which may not match their age or size. There are many different nipple and bottle types out there – trying to figure out the best choice can be an overwhelming process. Finding the right fit is something that your baby’s doctor or a lactation specialist can help you with.
6. Experiment with baby’s bottle-feeding position
Your baby may also prefer to eat while in a certain position, which typically differs from breastfeeding positions. Try different angles and placements to see if there is one they favor. For example:
Try different angles and placements to see if there is one they favor. For example:
- Cradling them in your arm at a 45-degree angle while keeping their head and neck aligned.
- Sitting upright so that their back is against your stomach.
- While sitting or lying down, bend your legs and position your baby so they face you with their head resting against your knees, their back against your thighs and their feet on your stomach.
No matter what position you use, remember to angle the bottle so that milk only comes out when your baby sucks, and never prop the bottle in their mouth. Also remember to never lay your baby completely flat while feeding.
What to do when an older baby is refusing to take a bottle
The breast to bottle transition is certainly easier if you introduce a bottle at the right age. But even if your baby is already 2 to 3 months old, it’s still possible. In addition to the tips above, you can help your baby practice with a pacifier.
A pacifier can help babies form and strengthen their sucking ability. Consistently offer a pacifier to help soothe your baby when they’re fussy, if you’re not already. This helps your baby learn to organize their mouth movement, which will calm them. Once that becomes routine, begin offering your baby a pacifier for 20 to 30 seconds when you go to make a bottle. Doing so will help them more calmly prepare for bottle feeding.
Gently pull on the pacifier as your baby sucks it. Make sure to do this at least 3 to 5 times a day, including when your baby is using the pacifier to prep for a bottle feeding. These slight tugs will help your baby learn how to resist releasing the seal they’ve formed on the pacifier’s nipple. And that can strengthen their latch on a bottle’s nipple, too.
When the above tips don’t work, there may be another reason your baby is refusing a bottle
If you’ve been trying at-home strategies for a few days and your baby doesn’t seem to be getting more comfortable taking a bottle, call your baby’s doctor. They can help determine whether a medical issue may be present or connect you with a specialist if needed. Other reasons why your baby is refusing a bottle can include:
They can help determine whether a medical issue may be present or connect you with a specialist if needed. Other reasons why your baby is refusing a bottle can include:
Reflux issues can cause pain with eating
Babies can get heartburn, too! When a baby has reflux, food and stomach acid flow from the tummy back into the esophagus (the tube the carries food from the mouth into the stomach).
Reflux causes babies to feel discomfort or pain when eating, which understandably affects feeding. Symptoms that may point to reflux issues include:
- Arching or stiffening their back when feeding
- Crying, fussing and getting red or watery eyes while feeding
- Coughing regularly during feedings or right after them
- Refusing to drink or accepting only 1 ounce of milk or less
- Falling asleep while feeding
- Having poor sucking and breathing coordination
- Taking a long time to eat or drink
It’s important to know these actions can occur and not be related to reflux. It’s common for babies to have a fussy time of day or be more tired some days than others. If symptoms are ongoing, a baby can be evaluated and treated for reflux.
It’s common for babies to have a fussy time of day or be more tired some days than others. If symptoms are ongoing, a baby can be evaluated and treated for reflux.
Facial or oral structural differences can make latching difficult
If reflux doesn’t appear to be the problem, your baby’s doctor may refer you to a rehab specialist like me.
I’ve been helping moms and families who struggle with the transition to bottles for almost a decade. It’s part of my work as a speech therapist at Park Nicollet. You might think, “My baby’s problem is with eating – not talking. What does speech therapy have to do with that?” The answer could be, a lot!
The shape or structure of a baby’s cheeks, mouth, tongue or jaw can impact their feedings. That’s because these body parts affect how they’re able to latch both to the bottle, as well as to the breast. For example:
- Thin cheeks with little to no fat pads make it hard for a baby to hold their tongue in place to feed
- A tongue-tie(where the tissue that attaches the tongue to the bottom of the mouth is too short) can limit a baby’s ability to move their tongue from side to side in their mouth or past their lower lip to feed
- A tongue-tie that’s been clipped requires a baby to relearn how and where to move their tongue to feed, and create new muscle memory
- A “vaulted” palate (where the roof of the mouth is higher and narrower than the typical flat U-shape) causes additional space in a baby’s mouth that can make it harder for their lips to form a tight seal
Weak oral muscle tone or lack of oral stimulation can make it hard to get enough milk during feeding
It’s possible that a baby just doesn’t have the strength to get what they need during a feeding. This could be the case even if they have very normal oral motor actions.
This could be the case even if they have very normal oral motor actions.
If your baby is refusing to take a bottle, we’re just a phone call away
Always feel empowered to call your baby’s doctor or make an appointment with them. They can connect you with different types of breastfeeding support, including drop-in breastfeeding support groups and lactation consultants who help with both bottle and breastfeeding issues. They can also refer you to a pediatric rehabilitation specialist.
Our incredible nursing staff is also here for you. HealthPartners patients can call 800-551-0859. Park Nicollet patients can call their clinic directly during regular business hours, or 952-993-4665 if it’s after hours. For questions and advice on new baby care, you can also call our 24/7 BabyLine at 612-333-2229.
Find a doctor who can help
Are you still looking for the right doctor for your new baby? We have hundreds of doctors and clinicians across the Twin Cities, central Minnesota and western Wisconsin, that can help you with all your questions.
While you may be wondering how to get them to take a bottle today, you’ll get it figured out. Then the question will be: How can I get my child to eat their vegetables?
Bottle Feeding Problems - Why Your Baby Squirms, Appears Uncomfortable – Baby Care Advice
When your baby squirms, appears uncomfortable during a feed, fusses, cries or refuses a bottle, seemingly fights the bottle despite being hungry, it can be challenge to figure out the cause. The timing and type of behavior she exhibits provides vital clues.
Signs of bottle-feeding problemsDoes your baby display troubled behavior in relation to bottle-feeding, such as….
- Refuses a bottle
- Turning away from the bottle.
- Refusing to close her mouth around the nipple.
- Holding nipple in the mouth but not sucking.
- Taking only a small amount and then refusing more.
- Screaming when placed into a feeding position or at the sight of the bottle.
- Milk pouring out of baby's mouth.
- Feeding too quickly.
- Feeding too slowly.
- Falling asleep before the feed is completed.
- Coughing and spluttering when feeding.
- Not consuming as much milk as expected.
- Wanting more milk than expected.
- Throwing up large amounts of milk.
Then there may be steps you can take to remedy the situation and get your baby to calmly and happily take a bottle.
Behavioral reasons‘Behavioral’ means baby’s behavior is in response to the circumstances rather than a physical cause. Behavioral reasons are the most common of all reasons for infant feeding problems. There are numerous behavioral reasons for a baby to experience feeding problems and/or display problematic feeding behavior. Common reasons include:
1. Misinterpreting baby's cues as signs of hunger Does baby at times refuse feeds?Does she take only a little and not want more?
Babies are in an oral stage of develop. Sucking is the primary way babies soothe. They also learn by sucking and mouthing objects. Many babies have a strong desire to suck for reasons that extend beyond hunger, such as tiredness, boredom, discomfort and soothing. There may be times when you mistake your baby’s desire to suck for these reasons as hunger.
Sucking is the primary way babies soothe. They also learn by sucking and mouthing objects. Many babies have a strong desire to suck for reasons that extend beyond hunger, such as tiredness, boredom, discomfort and soothing. There may be times when you mistake your baby’s desire to suck for these reasons as hunger.
Newborn babies have an active sucking reflex. This means a newborn baby may accept a feed even when she’s not hungry, and she might guzzle down the bottle because she cannot choose to not suck when her sucking reflex is triggered. Once her sucking reflex has disappeared (usually by 3 months of age) she will willingly take only the amount she wants to take.
If you have mistakenly interpret her fussing or desire to such as hunger and offer her a feed, she might take a little and refuse the rest, or she refuse from the start. If you try to make her drink more than she wants, she will understandably get upset and fuss, cry and pull back from the bottle.
WHAT TO DO- See Hungry baby for more reasons why babies often appear
- See Infant reflexes
 Unrealistic expectationsIs baby not drinking as much as you expect?Is she fussing if you try to get her to finish a bottle?
Unrealistic expectationsIs baby not drinking as much as you expect?Is she fussing if you try to get her to finish a bottle?In around one third of consultations I have had with parents regarding an infant feeding problem, I found that parents were trying to make their baby drink more than he or she needed. In some cases, this was because of errors made their health professionals. They either failed to adjust calculations as baby matured or failed to consider baby as an individual. As a result, overestimated baby’s milk requirements.
If you think your baby is not drinking enough milk (breast milk or infant formula) you’re naturally going to feel concerned. If your concern translates into trying to pressure her to drink more than she wants or needs (gently or otherwise), you’re going to upset her. So it is very important for your peace of mind and your baby’s enjoyment at feeding times that you have realistic expectations about how much she needs.
- See How much milk does baby need for standard estimations for age and weight, and reason why a baby might take more or less than recommended.
- Follow your baby's feeding cues. Don't try to make her take more when she indicates she has had enough.
Sleeping and feeding are closely related when it comes to the needs of babies. Both are equally important to a baby's health, growth and development and feelings of wellbeing. You are no doubt aware that if your baby does not feed well she might not sleep well. But are you aware that the opposite is equally true. If she’s not getting enough sleep this has the potential to negatively impact on her feeding.
Physical fatigue can cause baby to fuss during feeds or falling asleep before the feed is completed. If you have a hungry/tired baby on your hands, tiredness will usually win out.
If you have a hungry/tired baby on your hands, tiredness will usually win out.
- Ensure baby gets enough sleep.
- Feed her before she becomes too tired.
- Aim to establish a flexible feeding and sleep routine to minimize the risk of feeding and sleep times clashing.
If your baby is often irritable and not sleeping enough, (see Overtired baby for signs and symptoms) you might find that resolving any underlying sleeping problem will cause feeding difficulties to spontaneously resolve once she receives adequate sleep.
- See our sleep section.
- Download or order a paperback copy of my infant sleep book Your Sleepless Baby: The Rescue Guide. There you will find comprehensive information on the reasons and solutions to various infant sleeping problems.
Babies over the age of 4 months can easily become distracted while feeding. They are often much more interested in the activities going on around them than they are in feeding.
They are often much more interested in the activities going on around them than they are in feeding.
Feed your baby in a quiet environment away from noise and distractions of other children.
5. Feeding managementSome feeding problems can be related to what may appear like insignificant details but which can make feeding difficult or uncomfortable for a baby. For example, how you hold your baby will affect her ability to feed from a bottle. If her head is too far forward or too far back or her neck is twisted this can make it difficult for her to suck or swallow.
WHAT TO DOSee How to bottle-fed a baby
6. Feeding aversionDoes your baby refuse to feed even when hungry?Does she scream at the sight of a bottle or when placed into a feeding position?Have you resorted to trying to feed her while asleep?A baby can develop an aversion to feeding when past feeding experiences have taught her that feeding is unpleasant, stressful or painful. Typically, baby is diagnosed with reflux and/or milk protein allergy or intolerance to explain her aversive feeding behavior. However, a behavioral feeding aversion (related to feeding management rather than a physical cause) is a far more common cause of infant feeding aversion.
Typically, baby is diagnosed with reflux and/or milk protein allergy or intolerance to explain her aversive feeding behavior. However, a behavioral feeding aversion (related to feeding management rather than a physical cause) is a far more common cause of infant feeding aversion.
A feeding aversion is the most complex of all infant feeding problems. An effective solution relies heavily on accurate identification of the cause.
WHAT TO DOSee Feeding aversion for more information. Or purchase or download a copy of 'Your Baby's Bottle-Feeding Aversion: Reasons and Solutions'.
7. Feeding equipmentDoes your baby gag, cough or splutter during feed?Does baby make clicking sounds while feeding?It could be the nipple is too long, too short, too fast or too slow.
The most important piece of feeding equipment is the nipple. The nipple needs to be the right size and speed for your baby's size, age and sucking ability. If the nipple is too long, too short, too fast or too slow for your baby, she may experience feeding difficulties and express her frustration by fuss or crying.
If the nipple is too long, too short, too fast or too slow for your baby, she may experience feeding difficulties and express her frustration by fuss or crying.
- See Feeding equipment for more information on choosing a feeding nipple.
- Experiment with nipples of different lengths, shapes and speed.
It's possible her feeding difficulties could be due to the nipple ring being screwed on too tight.
In order to maintain a neutral balance in air pressure within the bottle air needs to be able to enter the bottle to replace the void left by the milk the baby is removing. If the bottle is vented, this is achieved via the venting system. However, in the case of a non-vented bottle, the only ways air can enter the bottle are between the nipple ring and the rim of the bottle and through the holes at the end of the nipple. While sucking, a baby will maintain a seal over the holes at the end of the nipple with her tongue and prevent air entry in this way. If the nipple ring is screwed down tightly this also prevents air entry.
While sucking, a baby will maintain a seal over the holes at the end of the nipple with her tongue and prevent air entry in this way. If the nipple ring is screwed down tightly this also prevents air entry.
If air is prevented from entering the bottle, this causes a negative pressure to build in the bottle. As the pressure builds, baby need to work harder and harder to extract further milk, until such time and the air pressure is returned to normal. The effort required to suck against the negative pressure can cause a newborn baby to tire and fall asleep before completing the feed. An older baby may simply give up or express her frustration.
WHAT TO DOThe nipple collapsing (not all will) or stopping to burp baby allows air to enter through the holes and neutralize the pressure. But you don’t want to wait for this to resolve the problem. By then baby is already tiring or getting frustrated. See ‘Collapsing nipple’ for ways to manage this problem.
9. Feeding patternsIs your baby often take only small amounts, refuse more, but then wants to feed again an hour or two later?
Feeding patternsIs your baby often take only small amounts, refuse more, but then wants to feed again an hour or two later?Some babies develop a grazing or snacking feeding pattern where they will only drink small amounts of formula at a time and then want to be feed frequently, possibly every hour or two. Although this will not cause any problems for a baby, provided she drinks enough formula in total over a 24 hour period, it can become very tiring for parents to keep up with her constant demands for feeding.
WHAT TO DO- Try to encourage your baby to take as much milk as possible within 45 minutes. But don't try to make her feed if she doesn't want to. Stop sooner if she does not want to continue.
- Ensure baby gets plenty of sleep.
- Avoid allowing baby to fall asleep while feeding.
- Support your baby to extend the time between feeds, by offering a little water, a pacifier, a nap, playing with her, or taking her for a walk.
 Aim to encourage her to wait at least 3 hours from time you started her previous feed, but only if it's reasonable to do so without distressing her. If necessary extend the time between feeds gradually. As your baby gets used to going longer periods between feeds she will gradually take larger amounts at each feed.
Aim to encourage her to wait at least 3 hours from time you started her previous feed, but only if it's reasonable to do so without distressing her. If necessary extend the time between feeds gradually. As your baby gets used to going longer periods between feeds she will gradually take larger amounts at each feed.
Unless your baby was born prematurely or is very small for her age, developmentally she no longer requires feeding during the night beyond the age 6 months. If nighttime feeding continues past this age its not going to harm her but it could have a negative effect on her appetite and feeding patterns during the day.
Your baby only needs a certain number of calories in her day (24 hours) to provide for her growth and energy needs. If after the age of 6 months she continues to receive calories from nighttime feeds this will dampen her appetite during the day and she will not need to drink as much formula during daytime feeds. You might find she is content to go for long periods of time between feeds (which is usually what would happen at night). She might fuss or refuse some of her daytime bottles when they are offered simply because she's not hungry at the time. Or she might graze during the day.
You might find she is content to go for long periods of time between feeds (which is usually what would happen at night). She might fuss or refuse some of her daytime bottles when they are offered simply because she's not hungry at the time. Or she might graze during the day.
Nighttime feeding will cause your baby no harm, so if you're happy to continue feeding her during the night there's no reason to change a thing. However, it is important that you don't expect her to consume as much milk during the day as she may have otherwise taken if she did not feed at night.
Many babies will give up night time feedings on their own accord, but others will continue to wake and demand feeds overnight for months and possibly years while parents continue to provide feeds at night. Usually the reason babies continues to demand night feeds beyond the age of 6 months is because they have learned to rely on feeding as a way to fall asleep, or because their internal body clock gets turned around - where the baby has decreased appetite during the day because of the continued night feeds and as a consequence of small feeds during the day the baby wakes hungry during the night. Body clock problems can easily become a cyclical pattern that will continue over the long term unless parents take steps to change the situation. Healthy, thriving babies who continue to demand feedings at night beyond the age of 6 months often require guidance and support from parents to cease feeding at night and turn their body clock around to a normal day-night feeding pattern.
Body clock problems can easily become a cyclical pattern that will continue over the long term unless parents take steps to change the situation. Healthy, thriving babies who continue to demand feedings at night beyond the age of 6 months often require guidance and support from parents to cease feeding at night and turn their body clock around to a normal day-night feeding pattern.
Aim to cease overnight feeds after 6 months of age. However, before attempting to do this it's important to address any feeding to sleep issues your baby might have. She would need to learn to fall asleep in a different way before you will be able to successfully encourage her to cease night feeds.
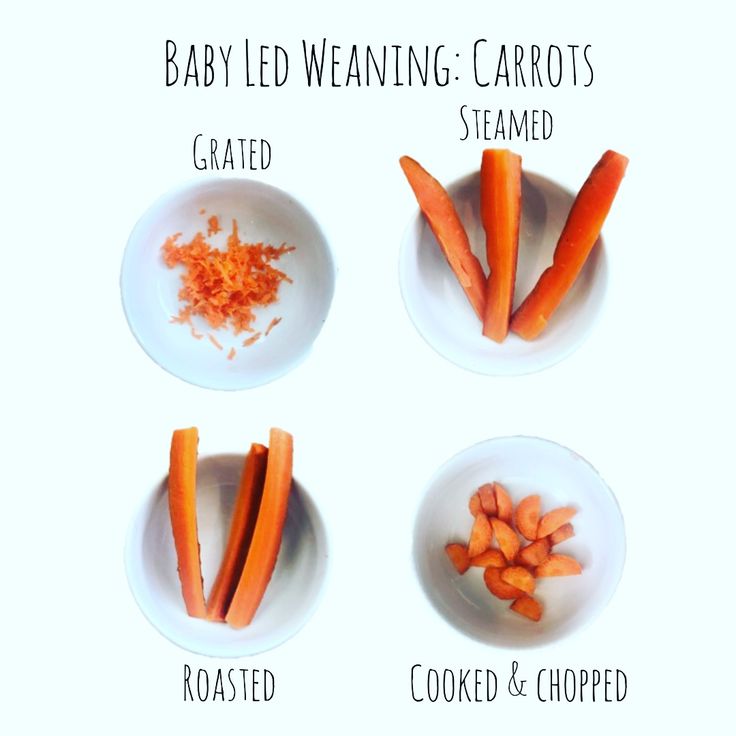
11. Starting solids earlyHave you started giving your baby solids before the age of 4 months?Have you been advised to start solids early?6 months is the recommended age for starting solid foods. Although a small number of babies may benefit from solids prior to this age, it's generally not recommended to start a baby on solid foods before the age of 4 months. An early start on solids has the potential to cause bottle feeding problems because solid foods may decrease the baby's appetite for milk (breast milk or formula).
Although a small number of babies may benefit from solids prior to this age, it's generally not recommended to start a baby on solid foods before the age of 4 months. An early start on solids has the potential to cause bottle feeding problems because solid foods may decrease the baby's appetite for milk (breast milk or formula).
- If your baby is less than 6 months old, either cease or reduce the amount of solids you offer to see if this helps to improve the situation.
- See our article on starting solids.
If solids are offered prior to bottle feeds, either directly before or mid way between feeds, when it's time for your baby's bottle feed she might be feeling full from the solids, in which case she's probably not going to take much milk from her bottle.
WHAT TO DO- For babies 4 - 9 months (when milk is still the most important food) offer solids 15 - 20 minutes after bottle feeds.
- For babies 9 - 12 months (when solids are becoming increasingly more important to a baby's diet) offer solids shortly before or shortly after her bottle, whichever you find works best. Babies at this age are often down to 3 bottles per day plus 3 main meals and 1 or 2 snacks.
In these early stages of learning to eat solids (4 - 7 months) solids are not needed to add value to a baby's nutritional intake, rather they are offered primarily to provide learning experiences. The baby is exposed to new food proteins that help prime her immune system. She gets to discover new tastes and textures and become accustomed to eating from a spoon. It is at this age that babies are most willing to accept new tastes. So variety rather than quantity is what solids are about.
Many babies, particularly very young babies, experience difficulty self-regulating their dietary intake. Some babies will continue to eat solid foods for as long their parents keep offering. Some babies will prefer eating solids compared to drinking formula. However, too much solids and not enough milk is not a balance diet for a baby. It may be necessary for parents to limit the amount of solids they offer in order to encourage their baby to have a greater appetite for milk feeds.
Some babies will continue to eat solid foods for as long their parents keep offering. Some babies will prefer eating solids compared to drinking formula. However, too much solids and not enough milk is not a balance diet for a baby. It may be necessary for parents to limit the amount of solids they offer in order to encourage their baby to have a greater appetite for milk feeds.
See our article on estimating how much milk your baby needs to make sure she's getting enough.
14. Weaning difficultiesDoes your breastfed baby refuse bottle-feeds?Does your baby have a breast preference?While some breastfed babies willing accept milk from a bottle many will not, at least not straight away.
Difficulty weaning from breast to bottle is rarely resolved by finding the 'right' feeding nipple. (All feeding nipples will feel equally foreign to a breastfed baby.![]() ) Nor does a solution lie in finding a formula with the 'right' taste. All formula will taste strange to a breastfed baby). The difficulty associated with weaning to a bottle most often lies in the fact that bottle-feeding requires a very different sucking action to breastfeeding. While breastfeeding the movement of your baby's tongue milks the breast, where as bottle-feeding requires a sucking action. A baby who has been exclusively breastfed beyond the age of 3 months will often refuse milk from a bottle because it "doesn't feel right" and she doesn't know how to suck from a bottle.
) Nor does a solution lie in finding a formula with the 'right' taste. All formula will taste strange to a breastfed baby). The difficulty associated with weaning to a bottle most often lies in the fact that bottle-feeding requires a very different sucking action to breastfeeding. While breastfeeding the movement of your baby's tongue milks the breast, where as bottle-feeding requires a sucking action. A baby who has been exclusively breastfed beyond the age of 3 months will often refuse milk from a bottle because it "doesn't feel right" and she doesn't know how to suck from a bottle.
It takes time and practice before a breastfed baby learns how to suck on a bottle.
WHAT TO DO- Try offering expressed breast milk in a bottle initially. (Don't be too optimistic and put too much in to start with. It would be a shame to waste it).
- A soft flexible nipple often works better.
NOTE: Many breast fed babies will refuse to accept a bottle while they are still being breastfed at times. They will simply wait until a breastfeed is offered. For these babies it will be the case of breastfeeding or bottle-feeding, but not both.
They will simply wait until a breastfeed is offered. For these babies it will be the case of breastfeeding or bottle-feeding, but not both.
- Your Baby's Bottle-feeding Aversion book
- Baby Care Advice consultation
- Rowena Bennett's Online Bottle-Feeding Aversion Program
In my book, ‘Your baby’s Bottle-feeding Aversion’, I have described physical and behavioral reasons for babies to develop an aversion to bottle-feeding. How to identify the cause and the solutions to match. Included are step-by-step instructions on how to regain your baby’s trust and resolve a feeding aversion caused or reinforced by repeated pressure to feed.
While the book was written for bottle-fed babies, many nursing mothers have found that applying the same strategies has also helped them to successfully resolve a breastfeeding aversion.
You might find that reading this book is all you need to do to understand the steps you need to take to resolve your baby’s feeding aversion and get him back to the point of enjoying eating until satisfied.
Baby Care Advice ConsultationsIf you would like an individualized assessment of all reasons for infant feeding problems, not just feeding aversion, we also provide a consultation service. Baby Care Advice consultants have extensive experience in pinpointing the cause of feeding aversion and other behavioral feeding problems such as those related to equipment and the parent’s feeding practices. (For more on what’s included in a consultation).
By Rowena Bennett, RN, RM, CHN, MHN, IBCLC.
Copyright www.babycareadvice.com 2021. All rights reserved. Permission from the author must be obtained to reproduce all or any part of this article.
Rowena's Online Bottle-Feeding Aversion ProgramSix time-saving modules to help your family enjoy feeding again with Rowena's step-by-step plan. Enjoy additional tools to manage anxiety, troubleshoot any issues, introduce new carers, how to manage illness/teething and much more.
Enjoy additional tools to manage anxiety, troubleshoot any issues, introduce new carers, how to manage illness/teething and much more.
- Module 1: Understanding feeding aversions
- Module 2: Identify the cause
- Module 3: Prepare for success
- Module 4: How to resolve your baby's bottle-feeding aversion
- Module 5: What to expect
- Module 6: Troubleshooting
- BONUS: Guided meditations
Baby won't take a bottle | Philips Avent
search support iconSearch Keywords
Home ›› What to do when your baby refuses a bottle
↑ top
any problems. If your breastfed baby refuses a bottle, don't worry. This is a common occurrence in many babies who are used to breastfeeding. Obviously, this can create certain difficulties for moms, especially if you need to return to work in the near future.
Obviously, this can create certain difficulties for moms, especially if you need to return to work in the near future.
3 Philips Avent products to help you bottle feed:
So why is your baby refusing to bottle and crying? There are many ways to quickly and easily teach a breastfed baby to a bottle. Here are important tips on what to do when your baby refuses a bottle.
Is the baby refusing the bottle? Take a step back
If your baby cries while bottle feeding, the first thing to do is to start over and rethink your feeding approach and technique. Try the following steps when bottle feeding your baby: [1]
- Lift and tilt your baby's head forward. Before inserting the pacifier into the baby's mouth, make sure that the baby's head is raised and tilted over his body to avoid choking: so that the baby does not choke and have the opportunity to burp during bottle feeding.
- Insert the pacifier.
 Bring the pacifier to the baby's lips and gently guide it into the baby's mouth. In no case do not try to press the nipple on the baby's lips and try to push it into his mouth. After touching the pacifier to the baby's lips, wait for the baby to open his mouth and take the pacifier.
Bring the pacifier to the baby's lips and gently guide it into the baby's mouth. In no case do not try to press the nipple on the baby's lips and try to push it into his mouth. After touching the pacifier to the baby's lips, wait for the baby to open his mouth and take the pacifier. - Hold the bottle at an angle. Tilt the bottle at an angle so that the nipple is only half full. So the child can eat at his own pace.
- Let the baby burp during and after feeding. It can be useful for a child to burp not only after feeding, but also approximately in the middle of the process. This will help reduce gas or tummy discomfort that your baby may experience from swallowing too much air.
- Stop in time, do not overfeed the baby. If the baby begins to turn his head away from the bottle or closes his mouth, then he is full and you need to stop feeding.
- Perhaps the flow of milk from the nipple to the baby is weak or, on the contrary, too fast, so he is naughty and refuses the bottle.
 Try changing the nipple to a nipple with a different flow.
Try changing the nipple to a nipple with a different flow.
Other tips if your baby refuses the bottle
If you've followed the steps above and your baby still refuses the bottle, don't worry. There are other ways to help bottle feed your baby. Here are some simple tricks you can add to your bottle feeding process. [2]
1. Remind your child about mom.
Sometimes a child can be fed by someone other than his mother - dad, grandmother or, for example, a nanny. If your baby fusses while bottle feeding, try wrapping the bottle in something that smells like mommy, like a piece of clothing or some fabric. This will make it easier to feed the baby when the mother is not around.
2. Try to maintain skin contact while bottle feeding.
Some babies need contact with their mother, so try bottle feeding while leaning against you. However, some babies are better at bottle feeding when they are in the exact opposite position than when they are breastfed. For example, there is a position with bent legs. Lay the child on your bent knees, facing you, pointing the child's legs towards your stomach. During feeding, the baby will be able to look at you and contact you in this way. If your baby refuses a bottle, experiment to see which works best.
For example, there is a position with bent legs. Lay the child on your bent knees, facing you, pointing the child's legs towards your stomach. During feeding, the baby will be able to look at you and contact you in this way. If your baby refuses a bottle, experiment to see which works best.
3. Move while feeding.
Sometimes all it takes to get your baby to take the bottle is a little wiggle or walk. The next time your baby starts crying while bottle feeding, try moving around a little rhythmically to calm him down.
4. Try changing the milk temperature.
If the baby still does not want to take the bottle, check if the milk in the bottle is too hot or too cold. Before feeding, put some warm breast milk on the inside of your wrist to check the temperature. Milk should be warm, but if it seemed hot to you, just place the bottle for a short while under a stream of cold water.
Choosing the right bottle for your baby If you plan to combine bottle feeding with breastfeeding, it is advisable to choose bottles with a nipple that will have a wide base as the bottle will grip closer to the breast.
 Also pay attention to the fact that the nipple is firm and flexible, the child must make an effort to drink from the bottle, as well as from the breast. Give preference to nipples with an anti-colic valve that vents air out of the bottle.
Also pay attention to the fact that the nipple is firm and flexible, the child must make an effort to drink from the bottle, as well as from the breast. Give preference to nipples with an anti-colic valve that vents air out of the bottle. Natural bottle allows you to combine breast and bottle feeding. 83.3% of babies switch from a Natural bottle to breastfeeding and back.*
If you choose a bottle for artificial feeding, traditional bottles are fine, but it is desirable that the nipple is made of a hypoallergenic material, such as silicone, has an anti-colic valve and did not stick together when bottle fed. In case your baby spit up often, then use special bottles with anti-colic and anti-reflux valve, which reduces the risk of spitting up and colic.
Bottle with unique AirFree valve reduces the risk of colic, gas and spitting up. With this bottle, you can feed your baby in an upright or semi-upright position to reduce spitting up. Due to the fact that the nipple is filled with milk and not air during feeding, the baby does not swallow air, which means that feeding will be more comfortable.
Both bottles are indispensable if you want to breastfeed, bottle feed or just bottle feed your baby.
“My baby refuses to breastfeed but bottle feeds – help!”
Sometimes a baby gets used to bottle feeding and refuses to breastfeed. Therefore, it is important to use bottles that are suitable for combining breastfeeding with bottle feeding. If, nevertheless, you are faced with the fact that the child refuses to take the breast, try using silicone nipple covers to make the transition from the bottle to the breast and back more imperceptible.
Remember that if you want to combine breastfeeding and bottle feeding, it is worth waiting at least a month before offering a bottle, so that you are lactating and have time to get used to each other and develop a breastfeeding regimen.
Breastfeed and bottle feed your baby with pleasure
Remember that it takes a while for your baby to get used to bottle feeding. This is completely normal. If you have to go to work, be sure to set aside enough time to bottle train your baby beforehand.
This is completely normal. If you have to go to work, be sure to set aside enough time to bottle train your baby beforehand.
Remember that every child is different, so what works for one may not work for another. With a little time and patience, you will find out what works best for your baby when he refuses a bottle.
You will identify your child's unique needs. However, if your baby still refuses the bottle after all the steps above, check with your pediatrician.
Articles and tips from Philips Avent
References:
*O.L. Lukoyanova, T.E. Borovik, I.A. Belyaeva, G.V. Yatsyk; NTsZD RAMS; 1st Moscow State Medical University THEM. Sechenova, "The use of modern technological methods to maintain successful breastfeeding", RF, 10/02/2012 3 llli.org - The Baby Who Doesn't Nurse
llli.org - Introducing a Bottle to a Breastfed Baby
Baby+ app
Download the app and track your child's development and growth with trackers and save those special moments forever.
Download app:
You are leaving the Philips Healthcare (“Philips”) official website. Any links to third party websites that may be included on this site are provided solely as a convenience to you. Philips makes no warranties regarding any third party websites or the information they contain.
I understand
You are about to visit a Philips global content page
Continue
You are about to visit the Philips USA website.
I understand
Bottle feeding | Bebbo
Submitted by Ilya Danshyn on Wed, 12/08/2021 - 18:40
Sometimes the baby cannot breastfeed, so you have to express milk and bottle feed the baby. Some babies are formula fed because for some reason breastfeeding is not possible, or lactation has stopped prematurely, or you have chosen to formula feed your baby.
- Make sure that the rate at which milk flows from the bottle through the nipple is appropriate for the baby.

- To check this, turn the filled bottle upside down.
- Milk should drip quickly, not squirt. If you have to shake the bottle hard to make the milk drip, it means that the nipple is not providing the normal intensity of feeding.
- The baby can fall asleep even before he has eaten everything from the bottle.
- It is normal for a small amount of milk to leak from the corners of the mouth; it will stop when the child gets older.
- If you can't find the perfect nipple, choose the one that produces the most milk; it's okay if you have to go through how many nipples before you find one that's right for you and your baby.
How to bottle feed your baby
- Sit back and hold your baby in your arms, gently but firmly. It is better for the baby to be in a more upright position, similar to the position when breastfeeding.
- Place the pacifier between the baby's lips; he will open his mouth and start sucking.

- Hold the bottle at an angle so that the nipple and mouth of the bottle are constantly filled with milk; this will prevent the child from swallowing air.
- When the baby stops actively sucking or has eaten half the milk from the bottle, carefully remove the bottle and check if he wants to burp; after that, you can continue feeding.
- Change the position of the baby during feeding or at least at each feeding; this allows even stimulation of the baby's sensations on both sides of the body and prevents positional deformation of the head.
How much milk does a baby need?
- The number of meals and the amount of milk is determined by the baby! Different babies require different amounts of breast milk or formula. Feeding time is not always evenly distributed over the time of day, sometimes children eat more during the day, followed by a long night break.
- If you are formula feeding, check the chart on the box.
 Of course, the recommended serving size for your age will only serve as a guideline and may not necessarily be appropriate for your child.
Of course, the recommended serving size for your age will only serve as a guideline and may not necessarily be appropriate for your child. - When a baby begins to receive complementary foods, as the amount of solid food increases, the baby's need for milk decreases.
- The amount of formula your baby eats will decrease when he switches from bottle to cup.
- By the age of 12 months, when a baby can switch to cow's milk, he usually receives 500-600 ml of breast milk or formula per day.
Some babies never eat the recommended amount of milk for their age and height. For some, this "recommended" volume is not enough. At least six wet diapers during the day, constant but not excessive weight gain, a healthy and active child - all this indicates that everything is in order. If you are concerned that your baby is not getting enough milk or formula, contact your doctor.
Responsive feeding from the bottle in accordance with the needs of the child
- Feed the baby when he shows that he is hungry and not according to the schedule, follow his signals.

- Do not feed the baby if he is not hungry, just because the formula is already prepared - this can lead to overfeeding the baby.
- When a baby is bottle fed, there is no difference between foremilk and hindmilk that affects the feeling of fullness in a breastfed baby.
- The child is often held so that the milk simply flows into the mouth, rather than actively suckling; in this case, he eats too much milk too quickly.
- During feeding, watch the baby for signs of satiety - he turns away from the bottle, sucks lazily - and stop feeding in time.
- Hold the baby close to you during feeding, hug and talk to him; it stimulates growth and development and also strengthens the bond between you and your child.
- The baby did not eat everything from the bottle and fell asleep while eating.
- Don't worry if the baby didn't eat everything; he knows how much formula or breast milk he needs.
- If the child falls asleep while eating, put him on your shoulder, stroke or pat him on the back and legs; Changing diapers is also an effective way to wake up a baby.

- Wait until the baby is awake before giving the rest of the milk.
Always empty the remaining milk from the bottle if more than an hour has passed!
Night feeding
- Every baby is different. Some wean from night feeding at four months, and some at two years. From the 6th month of life, healthy children no longer need night feeding. Now it's just a habit that gets harder to change the older the child gets.
- If a baby is bottle fed, this is the last age to stop eating at night! Do not replace milk with juices or other sweetened drinks to protect your child's teeth from cavities.
- If your baby drinks 60 ml of milk or less during the night, you can simply stop feeding at night and calm the baby as you normally would, then put him back in his crib to fall asleep on his own.
- If your baby eats more than 60 ml every night, gradually reduce the amount of milk over 5-7 nights and cradle the baby as you normally do.