Feeding baby after cleft palate surgery
Cleft Palate Repair: Instructions After Surgery
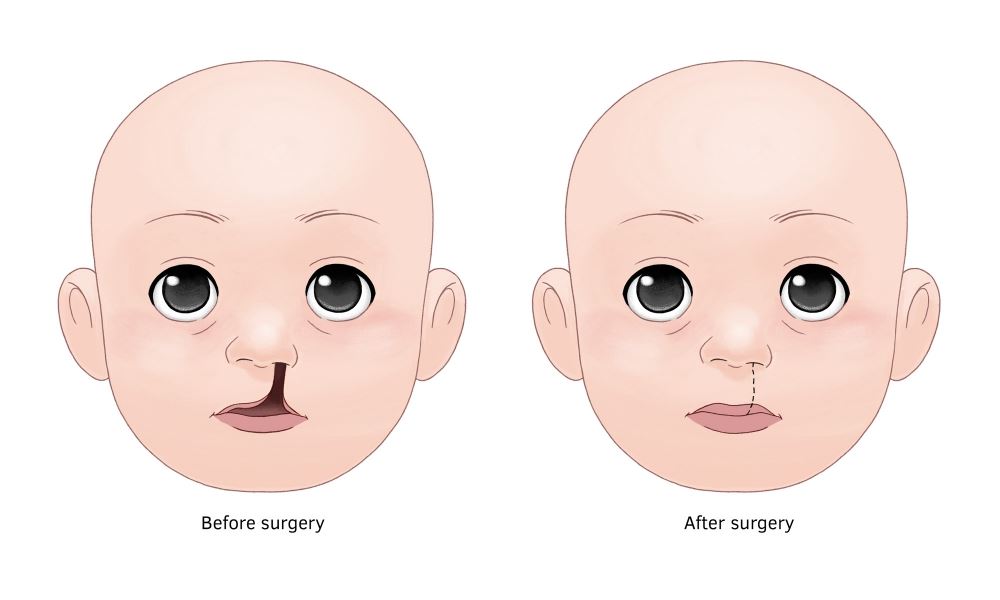
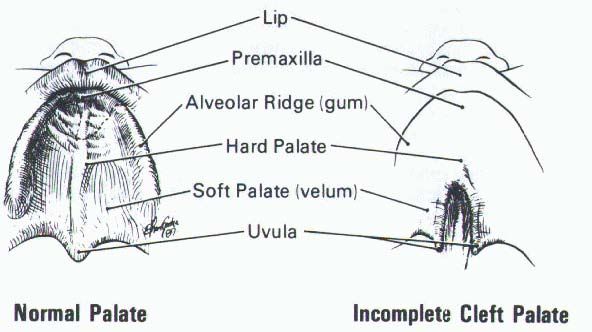
Your child's cleft palate (Picture 1) has been repaired. The opening in the roof of the mouth is now closed (Picture 2). Following surgery, there are a few things to know about your child's care at home. Other than these special instructions, your child should be cared for in the same way as any other child the same age.
Protecting the Repair
The roof of your child’s mouth (the palate) is still healing and should be protected from injury for about 3 weeks after surgery. There may be less feeling in this area for a while after the surgery. This means that your child can injure the roof of the mouth without you or your child knowing it.
Put hard objects away, or keep them out of your child’s reach while the palate is healing. Please discuss with your surgeon the use of a pacifier after surgery. Listed below are objects that could hurt your child’s mouth.
- Small wooden, metal or plastic toys
- Popsicles and their sticks
- Toys with small parts
- Drinking straws
- Toothbrushes
- Suckers and lollipops
- Knives, forks and spoons
- Thermometers
Mouth Care
- To clean your child's teeth and gums, use a gauze pad dipped in plain water or a small amount of alcohol-free mouthwash mixed with water.
Wipe the front of the teeth only.
- Do not use a toothbrush in your child’s mouth for 3 weeks.
- Have your child drink water after eating to keep the mouth clean.
Drinking and Eating
During this time, it is most important to make sure that your child is drinking enough liquids to stay hydrated. You will know if your child gets enough fluids if they have the same number of wet diapers after surgery as before. Your child should have a wet diaper at least every 8 hours. If there are fewer wet diapers, call the Cleft Lip and Palate Center helpline. This may be a sign of dehydration. You can reach the helpline at (614) 722-6299, Monday through Friday, 8 a.m. to 4:30 p.m. During evenings, weekends and holidays please call (614) 722-2000 and ask for the plastic surgeon on call.
For a short while after surgery, your child may not eat as well as before surgery.
- Give soft, pureed or mashed foods for 3 weeks. There is a table on the last page that shows specific soft foods that are and are not allowed.

- Do not give foods that have chunks, lumps or pieces, such as seeds, grains, pulp or skin.
- Do not give hard, crunchy foods such as cold cereal, cookies, crackers or chips.
- Use only a spoon for feeding.
- Do not let your child feed themself.
- Make sure the food is not too hot.
- Your child may drink from a bottle, open cup or sippy cup with a soft spout right after surgery.
- You may continue to feed your child with the same bottle system used before surgery.For more information on the types of bottles to use, see Helping Hand HH-I-21, Cleft Palate: Feeding Your Baby.
Arm Splints
Your child may or may not need to wear arm splints for 3 weeks. Please discuss this with your surgeon. These splints keep your child from putting their fingers into the mouth and accidentally damaging the repair. Before your child leaves the hospital, be sure a nurse shows you how to put the splints on properly. To find out more, refer to Helping Hand HH-II-16, Arm Restraints.
To find out more, refer to Helping Hand HH-II-16, Arm Restraints.
Activity or Play
- Your child may play as usual but needs to be watched more carefully during the first few weeks after surgery.
- Do not let other children give your child things to play with or eat without your approval.
- Soft toys are best for your child to play with while the palate is healing.
Pain and Medicines
It is important for your child to take medicines as directed by the doctor. Your child will go home with an antibiotic. The antibiotic needs to be taken until all of it is gone.
Some pain is normal after palate repair. Your surgeon and medical team will work together to achieve the best pain control possible, but your child may still experience discomfort. For pain, your child may be prescribed a medicine called either Oxycodone or Lortab. Your child may also be given over-the-counter pain medicines such as Tylenol®(acetaminophen), or Motrin or Advil (ibuprofen) instead of Oxycodone or Lortab. After a few days, your child will only need over-the-counter pain medicine.
After a few days, your child will only need over-the-counter pain medicine.
Pain Medicines
|
| Prescription Narcotic Medicine | Over-the-Counter Medicine | |
| Medicine | Lortab (Hydrocodone/Acetaminophen) or Oxycodone | Tylenol (Acetaminophen) | Motrin or Advil (Ibuprofen) |
| How often to take | Lortab or Tylenol - may give every | May give every | |
Things to Know About Side Effects for Oxycodone and Lortab
- Can be taken every 6 hours
- Has a side effect of constipation.
 If your child becomes constipated this may add to their pain and make it hard to tell why the child is uncomfortable.
If your child becomes constipated this may add to their pain and make it hard to tell why the child is uncomfortable. - As soon as possible, switch from using Oxycodone or Lortab to Tylenol alone
Things to Know About Lortab
- Contains both the narcotic hydrocodone and Tylenol
- Should NOT be taken within 6 hours of any other medicines that contains Tylenol (such as Triaminic, certain cold and cough medicines)
Things to Know About Over-the-Counter Pain Medicines
- Either Motrin or Advil (ibuprofen) and Tylenol (acetaminophen) can be used.
- You can give one dose of one kind of medicine every 6 hours. Do not give two kinds of pain medicine at the same time (Picture 3).
- If using both Motrin and Tylenol, you must alternate the dose of each type of medicine. Give one kind of medicine first, then 3 hours later, give the second kind of medicine. For example, start with one dose of Motrin at 9 a.
 m.; 3 hours later at noon, give the dose of Tylenol. At 3 p.m., give Motrin again. At 6 p.m., give Tylenol (Picture 3).
m.; 3 hours later at noon, give the dose of Tylenol. At 3 p.m., give Motrin again. At 6 p.m., give Tylenol (Picture 3). - Do NOT give Tylenol within 6 hours of any other medicine that contains Tylenol (Lortab, Triaminic, cough and cold medicines).
- Use a pediatric measuring device (available at the pharmacy) to measure the exact dose. Do not measure liquid medicines in kitchen spoons.
What to Expect After Surgery
For the first few days after surgery, you may see the following things:
- There may be a small amount of blood in the mucous or saliva (spit) for several days. The mucous or saliva may appear pink.
- More clear drainage (mucous) than usual may come from the nose for several weeks. This is because the opening between the nose and mouth is now closed. Before surgery, mucous drained directly into the mouth.
- Your child may snore and sound congested for several weeks. This will go away when the swelling goes down and there is less drainage.
- It may be harder for your child to sleep as well as before surgery. Sleep habits should return to normal after several weeks.
More Tips
- Dress your child in shirts that either button down or can be zipped so you do not need to lift the shirt over the head and face.
- Your child should wear long-sleeved shirts under the arm splints. The sleeves will help the splints to stay in place and prevent skin irritation.
When to Call the Doctor
Call your child’s doctor or the Cleft Lip and Palate Center’s helpline if your child has:
- Fever over 101°F when taken rectally, axillary (under the arm) or in the ear.
- Pain that does not go away when you give pain medicine.
- Any injury to the incision or any bleeding in the mouth.
- Trouble drinking or eating.
- A dry diaper for 8 hours or more.
- Taken too much medicine or the wrong medicine. Call the Central Ohio Poison Center at (800) 222-1222, TTY (866) 688-0088.
 They will tell you what to do.
They will tell you what to do.
The Cleft Lip and Palate Center Helpline
During regular business hours from 8 a.m. to 5 p.m., Monday to Friday, call (614) 722-6299.
After hours, on weekends or holidays, call (614) 722-2000. Ask to speak with the plastic surgeon on call.
Follow-Up Appointments
For follow-up appointments at the Cleft Lip and Palate Center, call (614) 722-6537.
- 2 weeks____________________________________
- 3 weeks____________________________________
Feeding Guidelines After Palate Surgery
| Food Groups | Foods Allowed | Foods to Avoid |
| Meats and Other Protein | Pureed meats Pureed or fork-mashed lentils or beans (without skins) Yogurt Fork-mashed tofu | Hard cheeses (Swiss, Cheddar) Bacon Nuts or seeds Steak |
| Breads | Soft white bread without crust (torn into pieces) Soft pancake (torn into pieces) | Hard or crunchy breads Waffles |
| Cereals | Cream of wheat Cream of rice Infant oatmeal Grits | Hard or crunchy cereals |
| Fruits | Fork-mashed, pureed, canned or well-cooked fruit Stage 1 or 2 baby fruits | Hard or crunchy fruit |
| Vegetables | Fork-mashed, pureed, canned or well-cooked vegetables Stage 1 or 2 baby vegetables | Hard or crunchy vegetables |
| Potatoes and Starches | Mashed white or sweet potatoes with no lumps, strings or skins | Hard or crunchy toppings on potatoes or noodles Whole grains such as barley, quinoa, kasha, buckwheat |
| Desserts | Pudding Jell-O | Any of the listed desserts with pieces of fruit, nuts, seeds or hard toppings |
| Beverages | Formula or milk | Pulp |
| Utensils | Sippy cups with short, soft spouts Bottles with a soft nipple | Straws |
| Miscellaneous | Seedless jams | Honey, agave or syrup Seeded jams Candy |
Cleft Palate Repair: Instructions After Surgery (PDF), Spanish (PDF), Nepali (PDF)
HH-I-18 1/79, Revised 12/19 Copyright 1979, Nationwide Children’s Hospital
Cleft palate repair: Feeding your child
Start over with a New Search
After surgery for cleft palate, your child needs a balanced diet of non-irritating foods. This is important to prevent infection and encourage healing. Here are some ideas for what and how to feed your child.
This is important to prevent infection and encourage healing. Here are some ideas for what and how to feed your child.
Place your child in a sitting position for feeding. Feed using only a spoon - no fork or other utensils. Do not give any foods served on a stick.
Give liquids from a cup, or use the side of a spoon. Do not use straws. Do not use a bottle, unless your doctor has told you to. In that case, use only the type of nipple supplied by the hospital.
After your child eats, use water to rinse traces of food from the mouth.
What should my child eat?
Your child should eat only smooth foods. Many table foods can be smoothed in a blender or food processor to an even, baby-food texture. Add liquids such as chicken or beef broth, milk, gravy, or smooth sauces to meats and vegetables. Use fruit juice to blend with fruit. See the education sheet "Blenderizing guidelines", and the table of foods to use and foods to avoid, below.
For extra protein:
- Melt cheese into soups, casseroles, scrambled eggs, or other hot dishes.
 Blenderize if needed.
Blenderize if needed. - Add nonfat dry milk powder to milk, ice cream, yogurt, pudding, soup, hot cereal, soft-cooked or scrambled eggs, mashed potatoes, gravies, sauces, and casseroles. Use 1 to 2 tablespoons in each 4-ounce serving. Blenderize casseroles if needed.
- Use commercial products: Pediasure® (made by Abbott), Boost® (made by Nestle), or Carnation Instant Breakfast® (made by Nestle). They can be found at many stores such as Target, Walgreens, Cub, or Rainbow.
What else do I need to know?
Continue using these guidelines until the doctor advises you to increase the texture of the foods your child can eat.
| Food group | Foods allowed | Foods to avoid |
| Milk and dairy products |
|
|
| Meat or meat substitutes |
|
|
| Fruits and vegetables |
|
|
| Breads and other starchy foods |
|
|
| Other |
|
|
Questions?
This is not specific to your child, but provides general information. If you have any questions, call Nutrition Services at your hospital during daytime hours.
If you have any questions, call Nutrition Services at your hospital during daytime hours.
Children's - Minneapolis: (612) 813-6865
Children's - St. Paul: (651) 220-6216
Last reviewed by Children's Nutrition Services 8/2015
Back To Top
This page is not specific to your child, but provides general information on the topic above. If you have any questions, please call your clinic. For more reading material about this and other health topics, please call or visit Children's Minnesota Family Resource Center library, or visit www.childrensmn.org/educationmaterials.
© 2022 Children's Minnesota
How to feed a baby before surgery to close a cleft
nutrients.
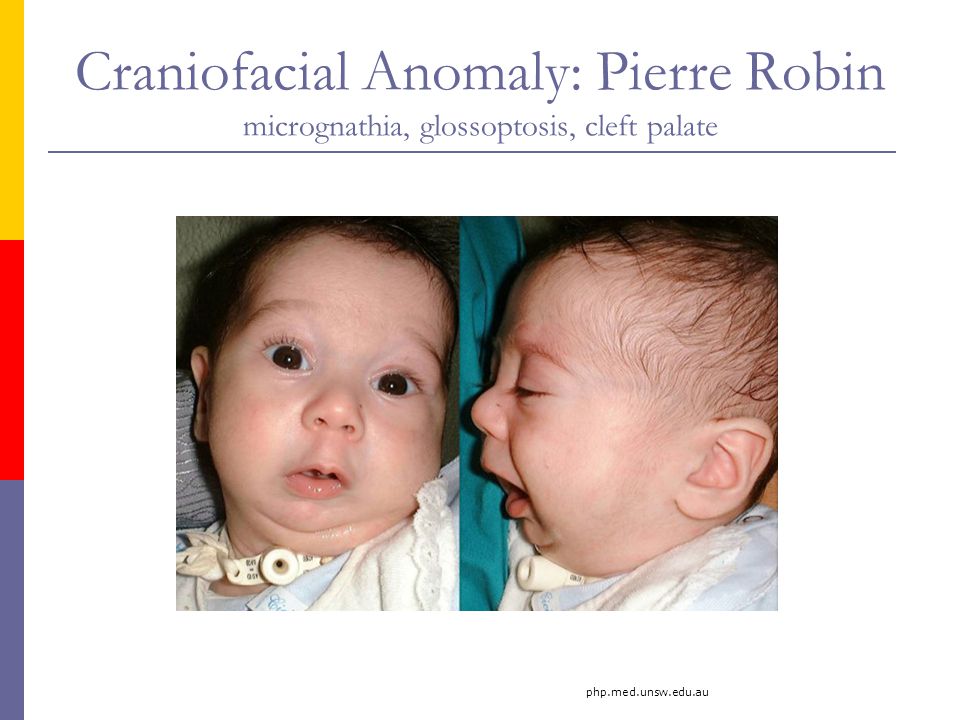
Babies with only cleft lip without palatal integrity usually have no problems with nipple latch and sucking. Children with cleft lip and palate or one cleft palate require some modification of the feeding method, as they have an abnormal communication between the nasal and oral cavity, which prevents the creation of negative pressure necessary for full sucking. Newborns with a cleft palate must squeeze milk out of the nipple by pinching it between the tongue and the rest of the hard palate and alveolar process of the upper jaw.
Newborns with a cleft palate must squeeze milk out of the nipple by pinching it between the tongue and the rest of the hard palate and alveolar process of the upper jaw.
When milk is squeezed into the mouth of a child with cleft palate, some of it will go into the nose. In addition, during feeding, more air can enter the stomach than in healthy children. This requires frequent changes in the position of the baby when feeding to ensure regurgitation of air. In the first weeks of life, this swallowing of air can lead to disorders such as colic, regurgitation of food, or even slight vomiting. Usually, the child outgrows all these problems within a few months, as the tone of the stomach muscles increases and the activity of the muscles of the digestive tract is coordinated. If some of these symptoms persist for a long time, contact your pediatrician.
Feeding babies with cleft lip and/or palate
For babies with clefts, as with all newborns, there are two best ways to feed: breastfeeding and bottlefeeding. Cup feeding is not the method of choice, and in the case of normal breastfeeding or bottle feeding, there is no need to resort to this method.
Cup feeding is not the method of choice, and in the case of normal breastfeeding or bottle feeding, there is no need to resort to this method.
Breastfeeding
There are different opinions about breastfeeding children with clefts. Although it is undeniable that breast milk is the best food for a baby. When a child with a cleft lip or palate is first placed on the breast, there may be some difficulties that are automatically associated with the existence of the cleft. Meanwhile, feeding a baby requires a certain period of trial and error before normal feeding is established.
A baby born with only a cleft lip often has no more difficulty feeding than a baby without a cleft lip, as the breast tends to fill the empty space, adapting and sealing the baby's mouth as much as possible.
Feeding children with perforated cleft lip and palate is also possible if there are no other problems. However, additional patience and modification of feeding technique will be needed to provide the baby with an adequate supply of nutrients, reduce maternal stress, and optimize the baby's responses.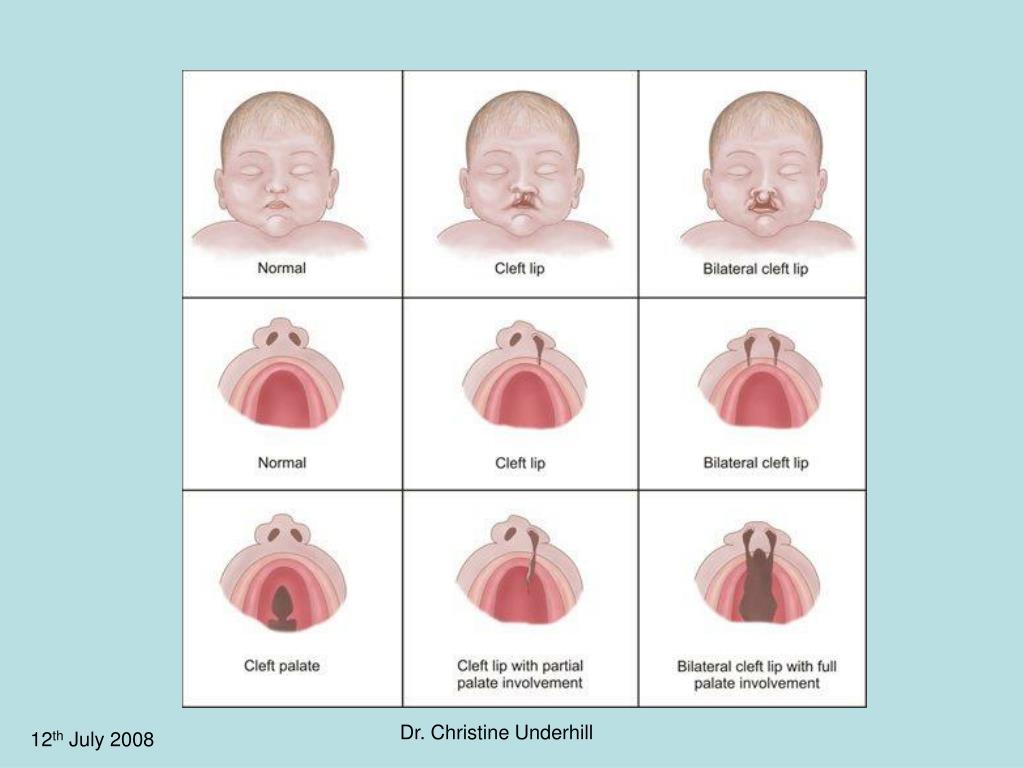
The following tips may be helpful to you.
- Massaging the breast before feeding promotes reflex milk release, which in turn facilitates the flow of milk into the baby's mouth.
Warm compresses applied to the breasts for 20 minutes prior to feeding ensure good blood flow to them.
Frequent breastfeeding (every 2-3 hours) in the first 2 weeks of life is often recommended to establish normal lactation.
Mothers are sometimes advised to increase their fluid intake. - Uses the areola (dark area around the nipple) digital pressure technique to help increase the protrusion of the nipple, making it easier to grab and hold in the baby's mouth. The nipple will enlarge during breastfeeding.
Sometimes the process of feeding is complicated by the appearance of cracks in the nipple. Such cracking may be due to infection or drug therapy. In such cases, to facilitate the feeding of the child, special pads are used to ensure the normal shape of the nipple and alleviate the mother's condition. Subsequently, when the cracks disappear, the nipple will bulge normally.
Subsequently, when the cracks disappear, the nipple will bulge normally. - If, after several attempts, the baby is unable to hold on to the nipple, or if you feel that the baby is not fully satiated, collect the remaining milk with a breast pump and finish feeding this milk from the bottle. In any case, when you are supplementing a baby from a bottle, you should always give the baby the breast first and then the bottle. With gradual adaptation, increasing strength and patience of your baby, the process of breastfeeding can become longer.
Bottle-feeding
It happens that it is not possible to establish normal sucking strength during attachment to the breast, especially in children with bilateral cleft lip and palate, in which the child cannot compensate for the pathological communication between the mouth and nose . In such cases, the only way to obtain breast milk is to bottle feed expressed breast milk. It is advisable to feed the baby with milk expressed using a breast pump for several weeks or, if possible, longer.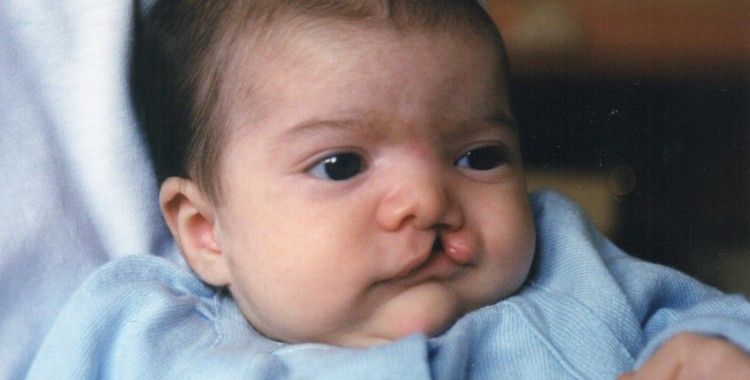 Even when your baby has been breastfed but breastfeeding has been delayed due to surgery or other reasons, you can bottle feed your baby with expressed milk until you can return to normal breastfeeding. In addition, there are currently ways to harvest breast milk for a certain period. Questions about how and when to store milk should be discussed with your pediatrician. In addition, there are currently a large number of breast pumps that significantly reduce the pumping time and ensure the maintenance of lactation for a long time.
Even when your baby has been breastfed but breastfeeding has been delayed due to surgery or other reasons, you can bottle feed your baby with expressed milk until you can return to normal breastfeeding. In addition, there are currently ways to harvest breast milk for a certain period. Questions about how and when to store milk should be discussed with your pediatrician. In addition, there are currently a large number of breast pumps that significantly reduce the pumping time and ensure the maintenance of lactation for a long time.
Formula feeding
Formula feeding is a simple and reliable substitute for breast milk. For this type of feeding, the same principles are acceptable as for breastfeeding, with the exception of small additions to the technique if necessary. In addition, the easier intake of food with wide cleft lip and palate will help your child more easily compensate for the difficulties that arise from pathological communication of the oral cavity and nose.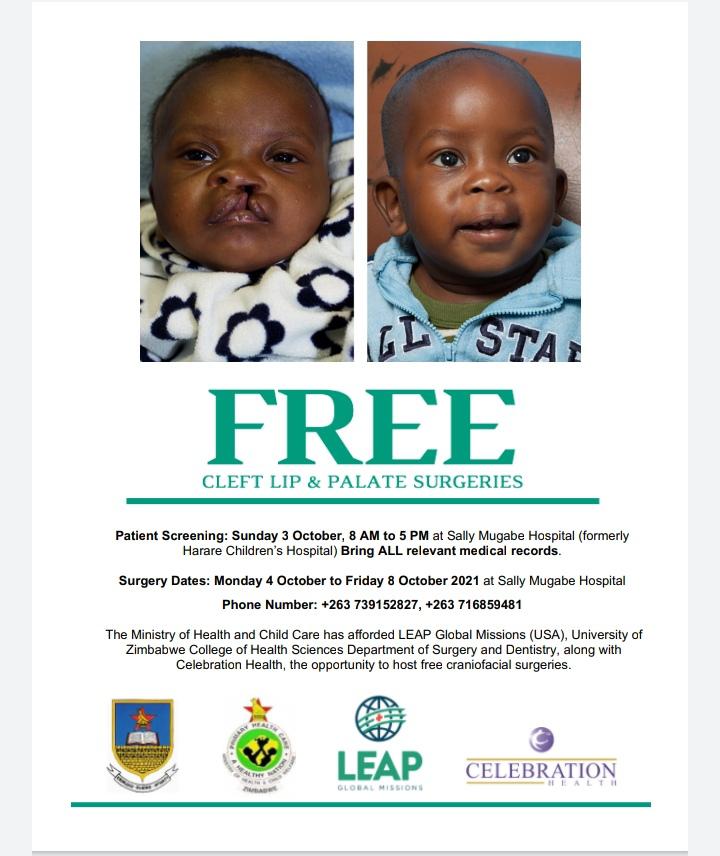 The selection of the necessary mixture for your baby can be adequately carried out by your pediatrician, who is guided by the peculiarities of the metabolism and digestive system of each child. Remember that you need to carefully study the instructions for preparing the mixture, which is usually located on the label of each package. Sometimes the pediatrician may recommend increasing the concentration of the mixture to speed up the weight gain of the child. This is a temporary measure, since the intake of water into the child's body is no less important than the amount of food consumed. For children with a cleft, a pacifier and bottle may need to be matched. Usually, parents start with simple types of nipples and bottles, and often, especially for children with small cleft lips, they are suitable. If the baby is not satisfied with the proposed devices, you can try using special orthodontic nipples and soft bottles. Your main task is to select the nipple and bottle that will make feeding the baby easy and complete.
The selection of the necessary mixture for your baby can be adequately carried out by your pediatrician, who is guided by the peculiarities of the metabolism and digestive system of each child. Remember that you need to carefully study the instructions for preparing the mixture, which is usually located on the label of each package. Sometimes the pediatrician may recommend increasing the concentration of the mixture to speed up the weight gain of the child. This is a temporary measure, since the intake of water into the child's body is no less important than the amount of food consumed. For children with a cleft, a pacifier and bottle may need to be matched. Usually, parents start with simple types of nipples and bottles, and often, especially for children with small cleft lips, they are suitable. If the baby is not satisfied with the proposed devices, you can try using special orthodontic nipples and soft bottles. Your main task is to select the nipple and bottle that will make feeding the baby easy and complete.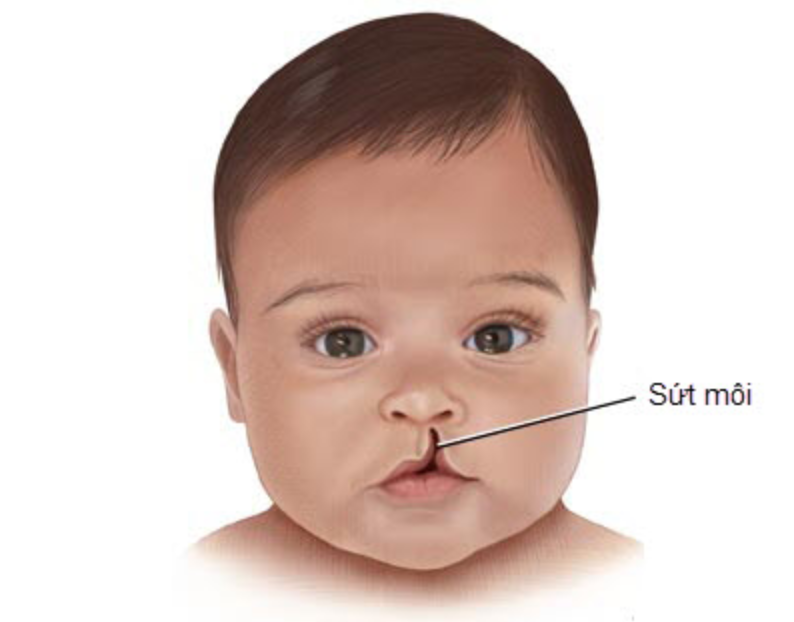
Soft nipples are usually better than hard nipples. You can soften the nipple by boiling. Subsequently, with the strengthening of your baby's chewing muscles, soft nipples can be replaced with soft orthodontic or harder nipples.
Some children with clefts may have difficulty with both very long and very short nipples. Short nipples cannot provide good contact with the tongue and palate, while long nipples can provoke a gag reflex.
One of the ways to regulate the flow of milk into the baby's mouth is the cross hole on the tip of the nipple. Such cuts facilitate the flow of liquid from the bottle. Cross-shaped incisions are very convenient, as they allow the child to regulate the strength and speed of milk flow with a constant sucking rhythm, preventing choking. A simple enlargement of the opening in the nipple causes a steady increase in the flow of milk into the baby's mouth, which leads to difficulty in sucking control and disruption of the interaction between swallowing and breathing. On the contrary, the cruciform incision ensures the flow of milk only at the moment of squeezing the nipple. Any nipple can be made into a cross-cut nipple with a regular razor blade. If it is required to make an incision on the orthodontic nipple, then it is better to perform it not at the very top, but a little closer to the lingual surface, as this will contribute to a dosed flow of fluid.
On the contrary, the cruciform incision ensures the flow of milk only at the moment of squeezing the nipple. Any nipple can be made into a cross-cut nipple with a regular razor blade. If it is required to make an incision on the orthodontic nipple, then it is better to perform it not at the very top, but a little closer to the lingual surface, as this will contribute to a dosed flow of fluid.
Another way to make milk flow easier while conserving baby's energy is to use soft bottles. The compression of such a bottle should be carried out rhythmically and correspond to the frequency of sucking and swallowing food by the child (approximately every 2-3 sips). Following the rhythm of the child, you can be sure that there will be no excessive intake of milk into the oral cavity and its reflux into the respiratory tract. The bottle must be squeezed and then released without continued compression. Feeding is usually easier if the bottle is angled to the opposite side of the mouth from the cleft, so that the nipple can be compressed between the tongue and the remaining normal part of the alveolar process of the maxilla and hard palate. Your baby will make the necessary adjustments on his own, adjusting to the position of the nipple, making it easier for him to get milk from the bottle. To do this, you only need to hold the bottle in one position and give the child the opportunity to shift the nipple from one corner of the mouth to another.
Your baby will make the necessary adjustments on his own, adjusting to the position of the nipple, making it easier for him to get milk from the bottle. To do this, you only need to hold the bottle in one position and give the child the opportunity to shift the nipple from one corner of the mouth to another.
When choosing a method of feeding, parents should understand for themselves some of the main advantages of bottle feeding:
- the most adequate supply of milk to the baby's body;
- saving physical energy spent on feeding, both by the child and the parent;
- the method allows to normalize suckling;
- is the most affordable, inexpensive and easiest way to feed.
Other feeding recommendations
Feeding position
It is very important that the breastfeeding parent finds the most comfortable position for himself. Sometimes, for comfort, it is useful to use a pillow to support the child.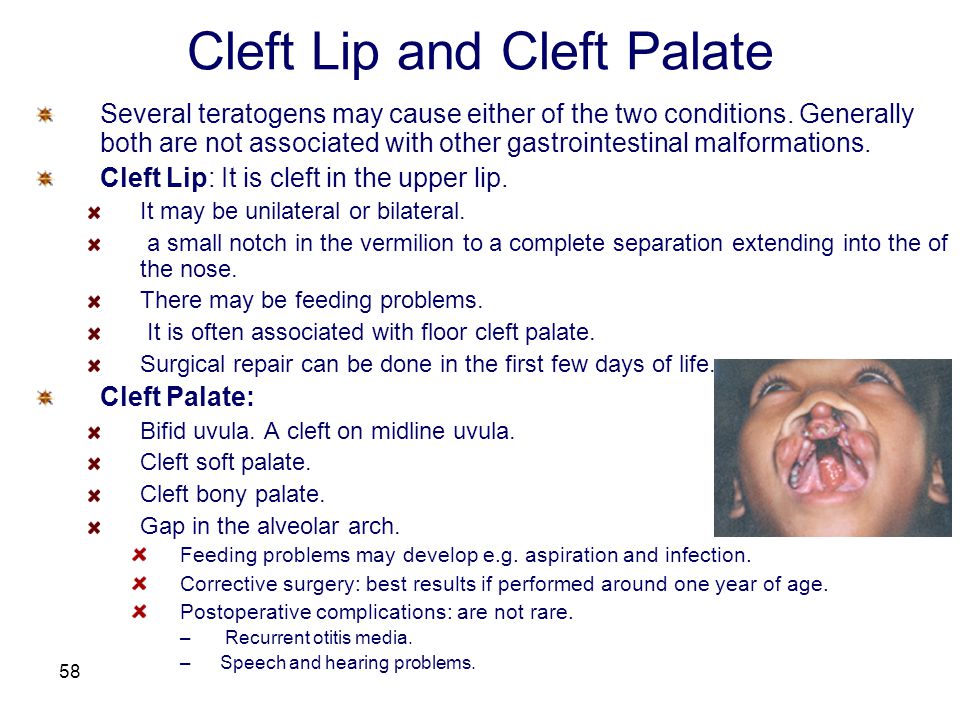 It also makes it easier to support the child with a footrest, on which the parent can lean with both one and two legs. Since feeding a baby can take up to 30 minutes. several times a day, the adult feeding the child should choose the most comfortable and relaxed position for himself.
It also makes it easier to support the child with a footrest, on which the parent can lean with both one and two legs. Since feeding a baby can take up to 30 minutes. several times a day, the adult feeding the child should choose the most comfortable and relaxed position for himself.
The baby should be well supported during feeding, usually in a slightly elevated position or sitting. This position helps prevent milk from entering the nose and choking the baby.
While breastfeeding, the mother can use several positions that can make the process much easier. The first position, when the child sits on a mattress or pillow, his back is supported by the mother's forearm, and her head by her hand. In this position, gravity helps the nipple to be placed in the baby's mouth.
It is very important to push the chest away from the baby's nose so as not to interfere with adequate breathing.
Another position where the child sits on the mother's lap, facing her, with the child's legs wide apart, embracing the mother's stomach. Sometimes it is necessary to use a pillow in order to lift the child higher.
Sometimes it is necessary to use a pillow in order to lift the child higher.
In order to suckle effectively, the baby's lower jaw must be in a stable position. If the mother supports the child by the lower jaw or chin, then the baby will not get tired so quickly. It is also useful for the baby's head to be turned first to one side and then to the other during feeding. Such a change allows the muscles of the oral region to work evenly. When bottle feeding, it is important that the baby is supported in an elevated position. The nipple should be placed in the area where all tissues are most preserved.
How to choose the right time to feed
When a baby starts crying loudly and seems agitated, there is a good chance that he is very hungry and this can make feeding very difficult. It is necessary to feed the child before he becomes too hungry. The child eats better when he is slightly hungry and does not feel much discomfort.
Many parents find that they can learn their baby's feeding schedule by watching for certain "signals" of the baby during awakening (moving the eyes under closed eyelids, moving the mouth, or moving the hands to the mouth).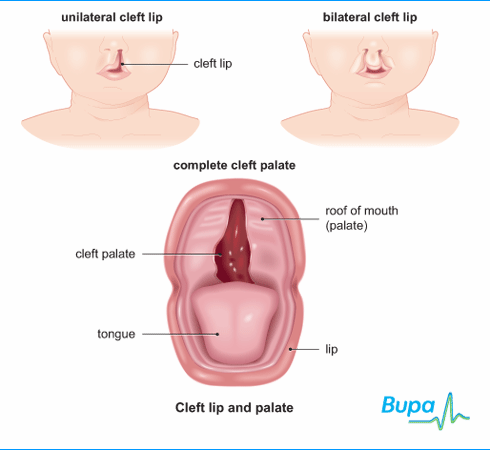 However, it must be remembered that the child does not eat the same amount of liquid during each feeding. It depends on the time elapsed between feedings.
However, it must be remembered that the child does not eat the same amount of liquid during each feeding. It depends on the time elapsed between feedings.
Help with food in the nose
Even when a fed baby is in a semi-elevated position, there is a risk of milk entering the nose (nasal regurgitation). Sometimes such regurgitation can be associated with a sudden change in body position. Parents should not be overly concerned about this, as food getting into the nose is quite common at first. It does not harm the child and gradually decrease with the growth of the baby. When regurgitation occurs, it is necessary to temporarily stop feeding and give the baby some time to cough or sneeze. This will allow the baby to clear the nasal passages and you can continue feeding. However, if the child has persistent regurgitation, cough is frequent and severe, you should consult your doctor.
Use of palatal obturators
Some specialists involved in the treatment of children with cleft lip and palate believe that obturators (special palatal plates that follow the curvature of the palate) should be used when feeding children with cleft palate, as they separate the oral and nasal cavity, which can greatly facilitate feeding. Such obturators tend to damage the mucosa. A more reliable result is obtained when the fitting of the obturator is carried out in the first few days of life. If you agree to use such a device, then you must be in close contact with a specialist who will manufacture, try on and adjust the device, periodically replacing it with a new one.
Such obturators tend to damage the mucosa. A more reliable result is obtained when the fitting of the obturator is carried out in the first few days of life. If you agree to use such a device, then you must be in close contact with a specialist who will manufacture, try on and adjust the device, periodically replacing it with a new one.
Most babies born with cleft palate and lip can be adequately fed without the use of such a machine when parents use combinations of feeding positions, appropriate feeding pattern (bottle or while breastfeeding), and appropriate technique.
Solid food introduction
Your child should be ready for pureed food at the same age as other children. Pureed food should be introduced at 4–6 months of age. Feeding should be done with a spoon, not a bottle. This is the time when the child begins to be interested in the difference in tastes and states. Again, moving from an elevated position to a sitting position reduces the number of episodes of regurgitation. Initially, the child should receive a small amount of liquid (no lumps) cereal porridge mixed with artificial formula until he learns to feel the pieces of food in his mouth. Pureed food should be given to the child until he is very hungry, otherwise the child will refuse to eat. The child must be gradually accustomed to more adult food, which takes time and patience. At first, the baby will try to suck in new food, which can again lead to episodes of food entering the nose. If this happens, give the child some water to drink. As soon as the child learns to swallow food, the density of porridge can be increased by mixing it with less milk. After that, you can add other complementary foods. If a child continues to have difficulty learning to eat solid foods for a long time, it is necessary to seek advice from specialists involved in the treatment of children with cleft lip and palate.
Initially, the child should receive a small amount of liquid (no lumps) cereal porridge mixed with artificial formula until he learns to feel the pieces of food in his mouth. Pureed food should be given to the child until he is very hungry, otherwise the child will refuse to eat. The child must be gradually accustomed to more adult food, which takes time and patience. At first, the baby will try to suck in new food, which can again lead to episodes of food entering the nose. If this happens, give the child some water to drink. As soon as the child learns to swallow food, the density of porridge can be increased by mixing it with less milk. After that, you can add other complementary foods. If a child continues to have difficulty learning to eat solid foods for a long time, it is necessary to seek advice from specialists involved in the treatment of children with cleft lip and palate.
Recommended feeding steps
| 4-6 months | introduction of porridge and puree soups |
| 8 months | give liquid, pureed food, introduce more hard or crushed food |
12 m. | give liquid, coarser chopped food, include chewy meat food |
| 18 mo. | give liquid, coarser chopped food, increase the amount of meat food, and increase the amount of raw vegetables |
General questions
1. How often does the baby need to burp?
Frequent regurgitation usually occurs in children who swallow large amounts of air during feeding. The baby usually signals impending regurgitation by slowing down or stopping suckling. This is the time when the baby can burp, and not at the moment of active sucking.
2. Does the cleft area need cleaning?
A child's mouth, whether it has a cleft or not, tends to clean itself. Some newborns with cleft lip do not need additional cleaning, but you should come to such a decision with your pediatrician. Removal of small amounts of curdled milk in the area of the cleft can be successfully carried out by giving the child a few sips of water.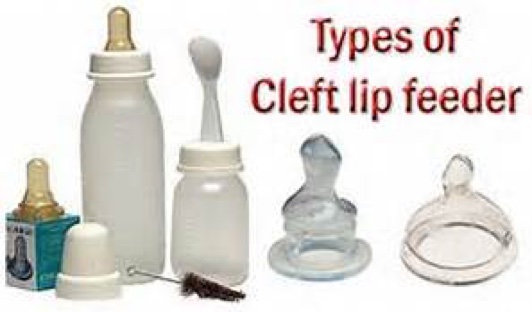 In any case, it may be necessary to gently wipe the baby's face and mouth area with a damp cloth. The use of cotton swabs or rinsing with a syringe is not recommended, as this can damage the baby's delicate mucous membrane.
In any case, it may be necessary to gently wipe the baby's face and mouth area with a damp cloth. The use of cotton swabs or rinsing with a syringe is not recommended, as this can damage the baby's delicate mucous membrane.
3. How to feed during the early postoperative period?
The surgeon who will operate on your child will definitely tell you about the features of feeding the baby after the restoration of the lip or palate. Mostly, parents should change the way of feeding immediately after surgery, and then the usual way of feeding will be restored. You will undoubtedly receive advice on restrictions and the introduction of a new way of feeding a few weeks before the operation so that you can gradually get used to this way.
4. When can cup feeding be introduced?
A cleft baby can be cup fed in the same way as other babies. Most babies are ready for this way of eating at 8-9 months of age. There are many types of cups for babies, which can greatly reduce the adjustment period, as some cups may make a baby drink better than others.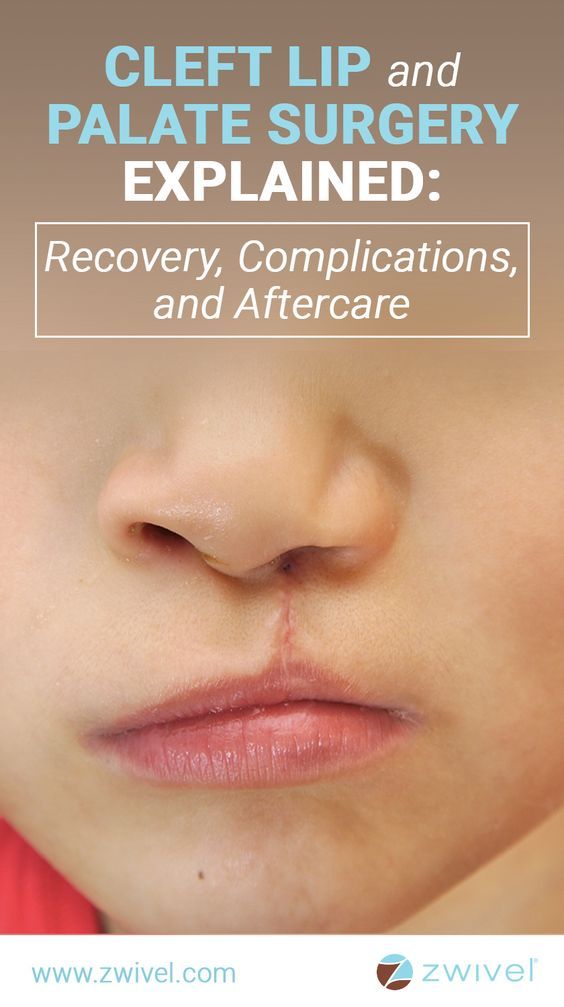 This helps to establish this way of feeding before palate plasty, especially if your child is already ready for the operation. Drinking from a cup does not adversely affect the newly operated lip and will allow you to return to your usual way of feeding after the operation. Since bottle-feeding is not allowed after palate plasty, gradually weaning the child from it will allow you to avoid unnecessary whims after the operation.
This helps to establish this way of feeding before palate plasty, especially if your child is already ready for the operation. Drinking from a cup does not adversely affect the newly operated lip and will allow you to return to your usual way of feeding after the operation. Since bottle-feeding is not allowed after palate plasty, gradually weaning the child from it will allow you to avoid unnecessary whims after the operation.
The experience of feeding a baby is extremely important for both parents and their baby. Newborn children adapt more easily, and infants learn faster if the parents have the necessary support, patience and love. Remember that there are many experienced professionals ready to provide you with the support you need.
Features of postoperative care for children with congenital cleft palate after uranoplasty
References:
Shatova, EA Peculiarities of postoperative care for children with congenital cleft palate after uranoplasty / EA Shatova.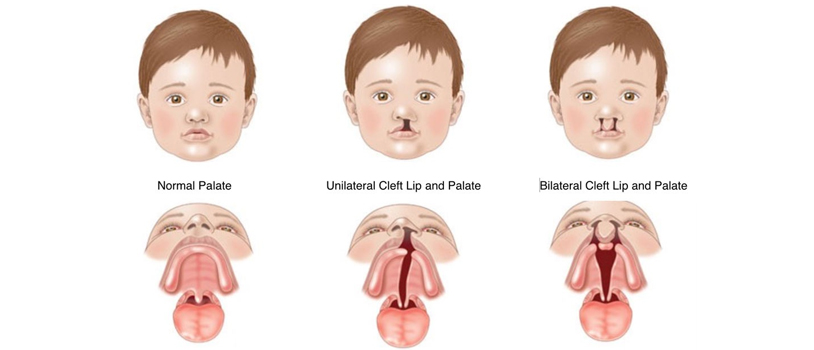 - Text: direct // Medicine and health care: materials of the VII Intern. scientific conf. (Krasnodar, January 2019). - Krasnodar: Novation, 2019. - S. 21-28. — URL: https://moluch.ru/conf/med/archive/318/14763/ (date of access: 11/19/2022).
- Text: direct // Medicine and health care: materials of the VII Intern. scientific conf. (Krasnodar, January 2019). - Krasnodar: Novation, 2019. - S. 21-28. — URL: https://moluch.ru/conf/med/archive/318/14763/ (date of access: 11/19/2022).
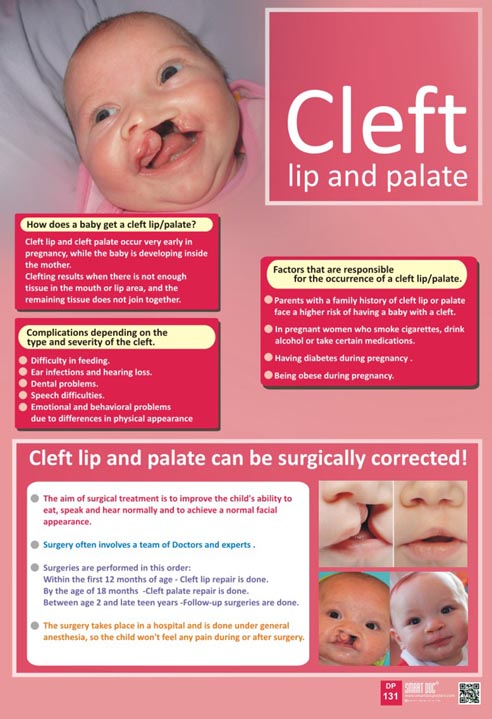
Congenital malformations can be defined as structural or functional abnormalities (e.g., metabolic disorders) that appear during fetal development and can be identified before birth, during birth, or later in life, such a definition of congenital malformations is given by WHO [ 19].
In the structure of congenital malformations (CM) of the fetus, the leading place is occupied by anomalies of the cardiovascular system (50.8%), the second is congenital malformations of the MPS (13.8%), and the third is congenital malformations of the musculoskeletal system (11.5%) , on the fourth - MVPR (6.0%), on the fifth - congenital malformations of the central nervous system (5.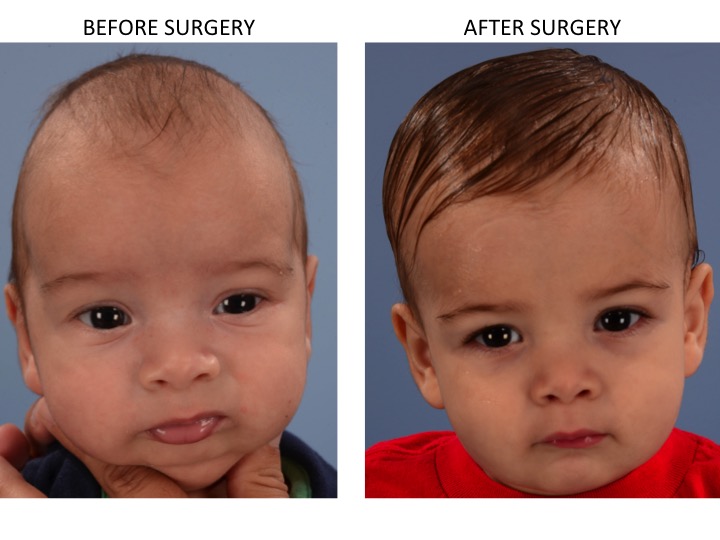 76%), on the sixth - cleft lip and palate (4.12%) [7].
76%), on the sixth - cleft lip and palate (4.12%) [7].
Congenital malformations constitute a significant group in the structure of surgical diseases of the maxillofacial region (MAR) in children. Among all types of malformations of the MLF, the frequency of birth of children with cleft lip and palate is the highest and varies in different regions of the Russian Federation from 1:500 to 1:1000 newborns. According to WHO, the average frequency of this anomaly in the world is 1:700 newborns [12].
Occupying the 4th–7th place in the structure of congenital anomalies, cleft palate occupies one of the first places in terms of the significance of anatomical and functional disorders [10].
The analysis of the frequency of congenital malformations (CM) in children of the Chuvash Republic over the past 22 years in 1991–2011. indicates that it ranged from 1.75% to 4.77%, and there is a steady increase in the frequency of congenital malformations over the years [7].
In Volgograd and the Volgograd region, the frequency of congenital cleft lip and palate is 1.5 per 1000 newborns, with a tendency to increase [14].
According to the scientific work of Varfolomeyeva L.G., the predicted increase in the number of births of children in the Tula region with congenital anomalies of the maxillofacial region is associated with the living conditions of parents in the zone with an increased level of radiation on its territory after the Chernobyl accident. So from 1993 to 2001, their number increased from 0.853 to 1.166 per 1000 live births. Most children with CCLP are born in warm spring (1.5% 0 ) and autumn (1.3% 0 ) seasons. Summer (0.8% 0 ) and in winter (1% 0 ), children with CCLP are born less frequently.
A number of researchers note an increase in the number of congenital anomalies in Russia after the accident at the Chernobyl nuclear power plant in 1986 (Minkov I.P., 1990; Vertai V. V., 1991; Korneev Yu., 1992; Vaganov N.N., 1994) [6 ].
V., 1991; Korneev Yu., 1992; Vaganov N.N., 1994) [6 ].
The prevalence of congenital cleft lip and palate in the Lipetsk region was 1:566 in 2000 and 1:800 in 2003. The frequency of births of patients with congenital cleft lip and palate is higher in the districts of the region than in the city of Lipetsk. 44% of children with congenital cleft lip and palate are rural residents, 25% are residents of district centers. For the period from 1994 to 2004, 90 children with congenital cleft lip and palate were born in the region, of which 23% were children with congenital cleft lip; 33% - with congenital unilateral cleft lip and palate; 10% - with congenital bilateral cleft lip and palate; 33% are children with congenital cleft palate [13].
According to the Office of the Federal Service for Surveillance on Consumer Rights Protection and Human Welfare in the Kursk Region, among the causes of childhood disability in 2012, as in 2011, mental and behavioral disorders rank first, accounting for 28. 7 % of disability, the second - diseases of the nervous system (25% of disability), congenital anomalies (malformations) close the top three, whose indicator in the structure of causes of childhood disability is 17.9% [17].
7 % of disability, the second - diseases of the nervous system (25% of disability), congenital anomalies (malformations) close the top three, whose indicator in the structure of causes of childhood disability is 17.9% [17].
In the structure of the General morbidity of the population of the Kursk region in 2012–2014. (per 1000 population) congenital anomalies (malformations), deformities and chromosomal disorders amounted to 6.33 in 2014 [5].
According to the study conducted by Demikova N.S., Lapina A.S., Podolnaya M.A., Kobrinsky B.A., the most common malformations (per 1000 births), both according to our data and according to EUROCAT, are hypospadias ( 1.21 and 1.53 respectively), Down syndrome (1.13 and 0.98), cleft lip/palate (0.67 and 0.81).
Congenital cleft lip and palate (CLCL) is the most common human malformation [15].
According to the Order of the Ministry of Labor and Social Protection of the Russian Federation of December 17, 2015 N 1024n “On the classifications and criteria used in the implementation of medical and social examination of citizens by federal state institutions of medical and social examination”, this pathology is one of the criteria for establishing disability groups.
The problem of CCLP treatment remains an urgent issue of eliminating this pathology of childhood. It requires specialized comprehensive medical care, including the efforts of specialists in various fields (neonatologist, pediatrician, speech therapist, otorhinolaryngologist, orthodontist, surgeon, teacher, psychologist, psychiatrist, audiologist, rehabilitator), whose task is the comprehensive rehabilitation of patients in a specialized center [6].
The main method of treating children with this pathology is the surgical removal of the palate defect. Despite numerous studies, the optimal timing of the treatment of patients with congenital cleft lip and palate has not yet been determined [15].
Cleft palate can be located only in the region of the hard and soft palate with a preserved alveolar process (cleft secondary palate) and can be located in the region of the alveolar process, hard and soft palate. These variants are the most common [12].
Children with congenital cleft palate have problems with feeding, since from the first days after birth, a disorder in the functions of sucking and swallowing is found. Also, in a child with a cleft palate, when inhaling, the communication of the nasal and oral cavities leads to the free entry of outside air into the upper respiratory tract. And in turn, the inferiority of external respiration causes the susceptibility of children to inflammatory diseases of the upper respiratory tract and lungs and leads to the development of bronchopulmonary diseases.
Also, in a child with a cleft palate, when inhaling, the communication of the nasal and oral cavities leads to the free entry of outside air into the upper respiratory tract. And in turn, the inferiority of external respiration causes the susceptibility of children to inflammatory diseases of the upper respiratory tract and lungs and leads to the development of bronchopulmonary diseases.
The weakness of exhalation further negatively affects the formation of the child's speech. Patients with this pathology pronounce words indistinctly, in a quiet voice. With a cleft palate, palatal, palatine-lingual and hissing sounds sound incorrectly. Speech has a pronounced nasal tone (open rhinolalia). The constant ingress of liquid and soft food from the oral cavity into the nasal cavity causes irritation of the mucous membrane of the nose and nasopharynx, which leads to the development of persistent foci of chronic inflammation in this area. Inflammation of the auditory (Eustachian) tube and chronic otitis media lead to hearing loss in children with this defect.
Uranoplasty is a reconstructive surgery to correct a cleft palate. In the course of uranoplasty, the tasks of restoring the anatomical integrity of the palate and middle part of the pharynx are solved by plastically closing the defect with a flap formed from adjacent soft tissues. Modern methods of radical uranoplasty make it possible to achieve a complete anatomical restoration of the palate in 92–98% of patients [20].
There is no single point of view on the timing of uranoplasty, but the general trend is defined as a recommendation for the introduction of early operations (1–4 years), which finds many supporters, and also helps patients quickly adapt to modern society.
Treatment of the child is carried out only in a specialized hospital. The child is prepared for surgery by a pediatric dentist-surgeon, a pediatrician, an anesthesiologist-resuscitator [12].
Care of surgical patients has a number of features. The nurse working with such patients has an important task - to create the best conditions for recovery, to prevent complications that may arise at any stage of perioperative care.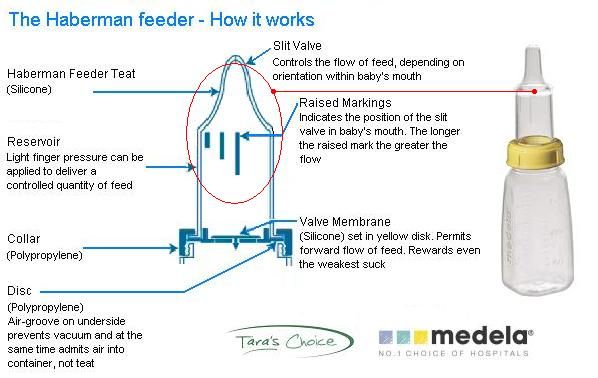
In pediatric surgery, a nurse has to deal with not one, but several patients - a sick child and his parents, relatives.
Many surgeons quite rightly argue that the operation is only the beginning of surgical treatment, its outcome is determined by good nursing, that is, appropriate care is needed in the postoperative period. Patient care is the area where professionalism gets its first expression.
Until now, a standard has not been developed for the organization and implementation of nursing care for patients with congenital cleft palate and lips, namely, nursing care after uranoplasty.
Features of postoperative care for a child with congenital cleft palate are as follows.
A protective plate made in advance is put on the upper jaw after the operation. When plastic surgery is performed only on the soft palate, a protective plate is made according to special indications.
After the operation, complete silence is prescribed for 8-10 days.
Daily irrigate the oral cavity with a warm antiseptic solution and repeat it after each meal.
On the 7-9th day after the operation, the first dressing is done, then the dressings are carried out every 2-3 days.
On the 13-15th day after the operation, a thermoplastic mass is layered on the inner surface of the protective plate so that it pushes up the tissues of the posterior parts of the hard and soft palate. As the scars are smoothed out, the thickness of the mass layer is increased. After the operation, the child wears the plate for 1.5 months, removing it for meals, speech therapy sessions and sleep.
Feed children after surgery need liquid high-calorie food.
After healing of the palatal mucosa (approximately 3–4 weeks after the operation), it is necessary to start palatal massage [14].
To classes with a speech therapist start after the first dressing.
The speech therapist evaluates the functional state of the palatopharyngeal closure, and the degree of these changes, established by the methods of endonasopharyngoscopy, radiography, electromyography, determines the indications and the choice of the method of operation to eliminate the palatopharyngeal insufficiency, if it is established and not corrected by the speech therapist.
Compliance with the dispensary regulations and treatment standards is the most important aspect of the rehabilitation of patients in this group. The professional role of a nurse is also enormous at all stages of the complex rehabilitation of a child with congenital cleft lip and palate.
Many experts argue that it is better to complete the treatment before the child enters school (at the age of 4–5 years), given the importance of the operation for the development of speech and the creation of conditions for limiting or preventing underdevelopment and deformities of the jaws due to the influence of postoperative scars.
The purpose of early operations is to reduce the period of maladaptation of the child.
The subsequent stages of orthodontic, speech therapy, psychological and pedagogical and other types of treatment are carried out in the center or by a pediatric dentist-surgeon at the place of residence according to the recommendations of the center [12].
Thus, taking into account functional disorders in the development of palate defects and the peculiarities of postoperative care for a child with congenital cleft palate, it became necessary to develop nursing care after uranoplasty. A nurse in children's departments of maxillofacial surgery is a methodological consultant for parents and relatives of a patient-child, as a result, it becomes necessary to develop guidelines for caring for a child with congenital cleft lip and palate for nurses and parents.
Literature:
- Order of the Ministry of Health of the Russian Federation dated November 13, 2012 No. 910n “On Approval of the Procedure for Providing Medical Care to Children with Dental Diseases”.
- Order of the Ministry of Labor and Social Protection of the Russian Federation of December 17, 2015 N 1024n "On the classifications and criteria used in the implementation of medical and social examination of citizens by federal state institutions of medical and social examination"
- Andreeva O.
 V. Staged rehabilitation of children with congenital cleft lip and palate // Bulletin of the Chuvash University. - 2012. - No. 3. - S. 269–275.
V. Staged rehabilitation of children with congenital cleft lip and palate // Bulletin of the Chuvash University. - 2012. - No. 3. - S. 269–275. - Demikova N. S., Lapina A. S., Podolnaya M. A., Kobrinsky B. A. Dynamics of the frequency of congenital malformations in the Russian Federation (according to the federal monitoring base for congenital malformations for 2006–2012) Russian Bulletin of Perinatology and Pediatrics, 2, 2015
- “STATE PROGRAM “Health development in the Kursk region” Passport of the state program of the Kursk region “Health development in the Kursk region”, 2016
- Varfolomeeva LG Organization of specialized care for children with congenital maxillofacial pathology in the Tula region, taking into account the environmental situation. Scientific work. Moscow, 2003
- Ignatieva O. V. Congenital cleft lip and palate in children in the Chuvash Republic. Electronic scientific journal "Modern problems of science and education".
 - 2013. - No. 3.
- 2013. - No. 3. - Kasimovskaya N. A., Shatova E. A. Search for personnel potential of maxillofacial departments in solving the problems of patients with congenital cleft lip and palate and their families at the stage of rehabilitation and care. Collection of scientific papers based on the materials of the XVI International Scientific Conference "Scientific Dialogue: Questions of Medicine". November 15, 2018 St. Petersburg.
- Oleinik T.V., Savin A.B., Shatova E.A. Problems of adaptation of children with congenital cleft lip and palate at the stage of complex rehabilitation. Knowledge misel journal No. 25/2018.
- Rubtsova NV Comparative evaluation of the results of surgical treatment of children with congenital unilateral penetrating cleft palate. Scientific work. Moscow, 2006
- Spevakova E. A. Nursing care for children with congenital maxillofacial pathology. Nurse, No. 2, 2012
- Dentistry for children. Surgery / Ed.
 S. V. Dyakova .- M .: OJSC “Publishing House “Medicine”. - 2009. - 384 p.: Ill. - ISBN 5-225-03431-4
S. V. Dyakova .- M .: OJSC “Publishing House “Medicine”. - 2009. - 384 p.: Ill. - ISBN 5-225-03431-4 - Sutulov VV Provision of specialized care for children with congenital cleft lip and palate in modern conditions of healthcare development (on the example of the Lipetsk region) Scientific work. Tver, 2006
- Fomenko I. V., Filimonova E. V., Kasatkina A. L. Rehabilitation program for children with congenital pathology of the maxillofacial region. Informational and methodical writing. Volgograd, 2007.
- Fomenko I. V., Filimonova E. V., Kasatkina A. L., Kraevskaya N. S. Analysis of the results of complex treatment of children with congenital unilateral cleft lip and palate depending on the method of palatal defect plasty. Clinical Dentistry, 1 / 77 / January - March 2016
- Fomenko I. V., Kraevskaya N. S., Vologina M. V., Kasatkina A. L. Features of the psychological state and self-esteem of children with congenital unilateral cleft lip and palate.


 )
)