Why babies vomit during feeding
Vomiting in babies | Pregnancy Birth and Baby
beginning of content5-minute read
Listen
From birth to 12 months, babies are known to vomit — it’s just one of their design features. However, as normal as vomiting is, it can also be worrying for parents. Occasionally, vomiting can be a sign of illness or complications, but for most babies, vomiting and reflux occurs simply because their guts are still developing.
What are the different types of vomiting
There are a few different types of vomiting and although the result is the same, the reasons are different:
- Possetting is the name for small amounts of milk brought up after a feed.
- Reflux happens when the valve at the top of a baby’s stomach is not tight enough to keep milk in there. A baby’s oesophagus (food pipe) is short, so when the valve opens and there’s only a short distance between it and their mouth, vomiting can occur.
- Projectile vomiting is vomiting with force. Projectile vomiting can be a symptom of a blockage at the outlet of a baby's stomach. If it's happening after most or all feeds, take your baby to a doctor.
What causes babies to vomit?
Generally, mild vomiting occurs because a young baby is still getting used to feeding on, digesting and eliminating milk. On average, a newborn baby’s stomach can hold around 20 millilitres, so it doesn’t take much milk for them to fill up and vomit the excess.
How can I tell if my baby is sick?
Vomiting by itself can be reassuring. However, if your baby has a temperature, is not feeding well, has diarrhoea or a rash, or experiences any other symptoms, your baby needs to see a doctor. If your baby seems healthy and well and is bright and alert, you may just want to monitor their vomiting to see when and how often it happens — but note that the amount that a baby vomits can be hard to work out and may seem larger than it really is.
What’s the difference between vomiting and reflux?
Vomiting caused by reflux generally occurs after feeding. It can seem effortless or cause pain. Some babies with reflux constantly 'spill' after and in-between their feeds. It’s important to think about how your baby’s vomiting affects them. If your baby seems happy, is thriving and gaining weight, you could simply try changing the frequency and amount of feeds you give them. If your baby seems to be in pain and/or not thriving, take them to a doctor. Sometimes medication is necessary for reflux.
Does breast or formula feeding cause more vomiting?
Breastfed babies can vomit as much as babies who are formula fed. There's no real difference between the two. Generally, the only difference is that feeding on formula makes a baby’s vomit smell and look different to that after feeding on breastmilk.
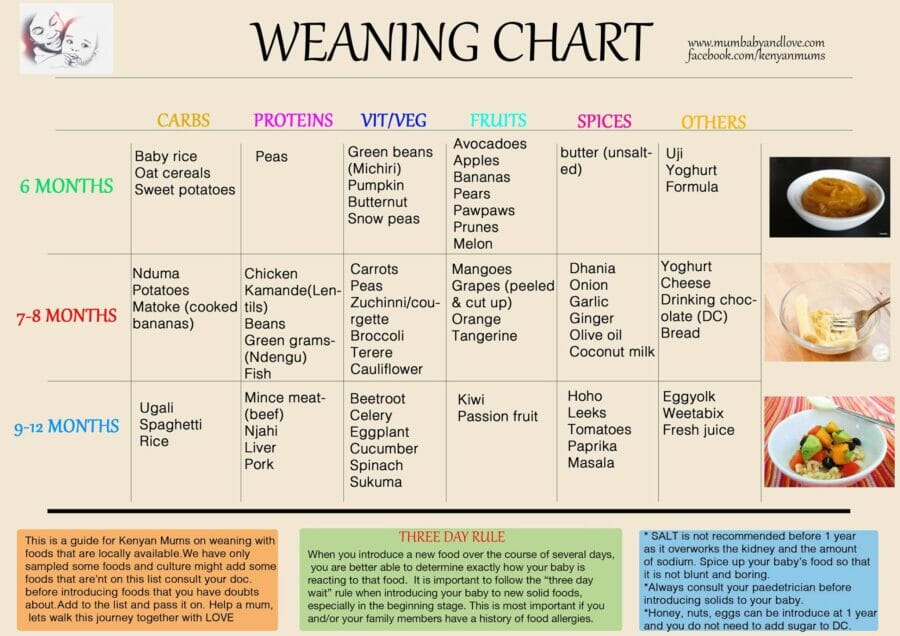
Can solids cause vomiting?
Some babies take time to adjust to digesting solid foods. They can vomit more when solids are introduced. This can occur because of overfeeding. Their stomachs are simply too small to accommodate extra volume. Start small when introducing solids — around 1-2 teaspoons of solids are ideal.
This can occur because of overfeeding. Their stomachs are simply too small to accommodate extra volume. Start small when introducing solids — around 1-2 teaspoons of solids are ideal.
Is vomiting a sign of allergies?
Some allergies can cause vomiting, especially allergies to cow's milk. Your baby can react to particular foods or ingredients if they’re sensitive to them. Your doctor can help guide you to decide which foods are best for your baby.
How can I treat my vomiting baby?
Most babies recover quickly after vomiting and don't need any specialised care. They can seem hungry again straight away or take a while to want to feed again. However, if they vomit a lot and have other symptoms, a doctor needs to assess them.
Generally, babies are not given medication for vomiting unless they can’t keep any milk or fluids down. Dehydration is generally managed by giving intravenous fluids.
Sometimes changing feeding positions and frequency can reduce the likelihood of vomiting. It's still important to always follow the safe sleeping guidelines when settling your baby, even if they vomit. Back sleeping is protective against choking.
It's still important to always follow the safe sleeping guidelines when settling your baby, even if they vomit. Back sleeping is protective against choking.
When should you see a doctor?
You should take your baby to see your doctor if:
- you are concerned about your baby's vomiting
- your baby is showing other signs of illness
- your baby seems lethargic, sleepy and not interested in feeding
- your baby is losing weight and not thriving
- there is blood or bile in their vomit
- their vomiting isn’t stopping or getting worse
Sources:
Raising Children (Vomiting), Red Nose Australia (Will baby choke if he/she vomits while sleeping on the back?), Safer Care Victoria (Vomiting in neonates), The Royal Australian College of General Practitioners (The vomiting child)Learn more here about the development and quality assurance of healthdirect content.
Last reviewed: September 2022
Back To Top
Related pages
- Vomiting in children
- Reflux
- How to know when your baby is well - video
- Knowing your baby is well - podcast
Healthdirect Australia acknowledges the Traditional Owners of Country throughout Australia and their continuing connection to land, sea and community. We pay our respects to the Traditional Owners and to Elders both past and present.
This information is for your general information and use only and is not intended to be used as medical advice and should not be used to diagnose, treat, cure or prevent any medical condition, nor should it be used for therapeutic purposes.
The information is not a substitute for independent professional advice and should not be used as an alternative to professional health care. If you have a particular medical problem, please consult a healthcare professional.
If you have a particular medical problem, please consult a healthcare professional.
Except as permitted under the Copyright Act 1968, this publication or any part of it may not be reproduced, altered, adapted, stored and/or distributed in any form or by any means without the prior written permission of Healthdirect Australia.
Support this browser is being discontinued for Pregnancy, Birth and Baby
Support for this browser is being discontinued for this site
- Internet Explorer 11 and lower
We currently support Microsoft Edge, Chrome, Firefox and Safari. For more information, please visit the links below:
- Chrome by Google
- Firefox by Mozilla
- Microsoft Edge
- Safari by Apple
You are welcome to continue browsing this site with this browser. Some features, tools or interaction may not work correctly.
Vomiting (0-12 Months)
Is this your child's symptom?
- Vomiting (throwing up) stomach contents
- Other names for vomiting are puking, barfing and heaving
Causes of Vomiting
- Viral Gastritis.
 Stomach infection from a stomach virus is the most common cause. Also called stomach flu. A common cause is the Rotavirus. The illness starts with vomiting. Watery loose stools may follow within 12-24 hours.
Stomach infection from a stomach virus is the most common cause. Also called stomach flu. A common cause is the Rotavirus. The illness starts with vomiting. Watery loose stools may follow within 12-24 hours. - Food Allergy. Vomiting can be the only symptom of a food reaction. The vomiting comes on quickly after eating the food. Uncommon in infants, but main foods are eggs and peanut butter.
- Coughing. Hard coughing can also cause your child to throw up. This is more common in children with reflux.
- Serious Causes. Vomiting alone should stop within about 24 hours. If it lasts over 24 hours, you must think about more serious causes. An example is a kidney infection. A serious cause in young babies is pyloric stenosis. See below for more on this.
Pyloric Stenosis (Serious Cause)
- The most common cause of true vomiting in young babies.
- Onset of vomiting is age 2 weeks to 2 months
- Vomiting is forceful.
 It becomes projectile and shoots out.
It becomes projectile and shoots out. - Right after vomiting, the baby is hungry and wants to feed. ("hungry vomiter")
- Cause: The pylorus is the channel between the stomach and the gut. In these babies, it becomes narrow and tight.
- Risk: Weight loss or dehydration
- Treatment: Cured by surgery.
Vomiting Scale
- Mild: 1 - 2 times/day
- Moderate: 3 - 7 times/day
- Severe: Vomits everything, nearly everything or 8 or more times/day
- Severity relates even more to how long the vomiting goes on for. At the start of the illness, it's common for a child to vomit everything. This can last for 3 or 4 hours. Children then often become stable and change to mild vomiting.
- The main risk of vomiting is dehydration. Dehydration means the body has lost too much fluid.
- The younger the child, the greater the risk for dehydration.
Dehydration: How to Tell
- The main risk of vomiting is dehydration. Dehydration means the body has lost too much water.
- Vomiting with watery diarrhea is the most common cause of dehydration.
- Dehydration is a reason to see a doctor right away.
- Your child may have dehydration if not drinking much fluid and:
- The urine is dark yellow and has not passed any in over 8 hours.
- Inside of the mouth and tongue are very dry.
- No tears if your child cries.
- Slow blood refill test: Longer than 2 seconds. First, press on the thumbnail and make it pale. Then let go. Count the seconds it takes for the nail to turn pink again. Ask your doctor to teach you how to do this test.
When to Call for Vomiting (0-12 Months)
Call 911 Now
- Can't wake up
- Not moving
- You think your child has a life-threatening emergency
Call Doctor or Seek Care Now
- Dehydration suspected.
 No urine in over 8 hours, dark urine, very dry mouth and no tears.
No urine in over 8 hours, dark urine, very dry mouth and no tears. - Stomach pain when not vomiting. Exception: stomach pain or crying just before vomiting is quite common.
- Age less than 12 weeks old with vomiting 2 or more times. Exception: normal spitting up.
- Vomited 3 or more times and also has diarrhea
- Severe vomiting (vomits everything) more than 8 hours while getting Pedialyte (or breastmilk)
- Head injury within the last 24 hours
- Weak immune system. Examples are sickle cell disease, HIV, cancer, organ transplant, taking oral steroids.
- Vomiting a prescription medicine
- Fever over 104° F (40° C)
- Fever in baby less than 12 weeks old. Caution: Do NOT give your baby any fever medicine before being seen.
- Your child looks or acts very sick
- You think your child needs to be seen, and the problem is urgent
Contact Doctor Within 24 Hours
- All other infants (age less than 1 year) with vomiting.
 See Care Advice while waiting to discuss with doctor.
See Care Advice while waiting to discuss with doctor.
Seattle Children's Urgent Care Locations
If your child’s illness or injury is life-threatening, call 911.
- Bellevue
- Everett
- Federal Way
- Seattle
- Virtual Urgent Care
Care Advice for Vomiting
- What You Should Know About Vomiting:
- Most vomiting is caused by a viral infection of the stomach.

- Vomiting is the body's way of protecting the lower gut.
- The good news is that stomach illnesses last only a short time.
- The main risk of vomiting is dehydration. Dehydration means the body has lost too much fluid.
- Here is some care advice that should help.
- Most vomiting is caused by a viral infection of the stomach.
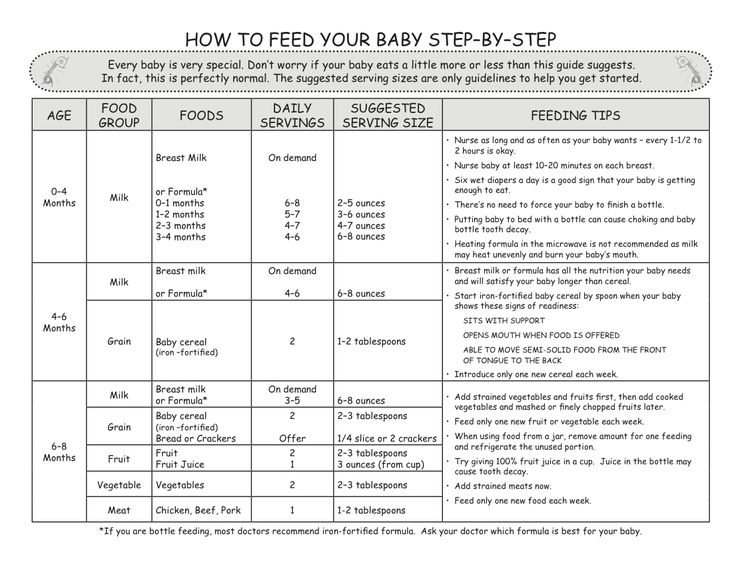
- Formula Fed Babies - May Give Oral Rehydration Solution (ORS) for 8 Hours:
- If vomits once, give half the regular amount of formula every 1 to 2 hours.
- If vomits formula more than once, offer ORS for 8 hours. If you don't have ORS, use formula until you can get some.
- ORS is a special fluid that can help your child stay hydrated. You can use Pedialyte or the store brand of ORS. It can be bought in food stores or drug stores.
- Spoon or syringe feed small amounts. Give 1-2 teaspoons (5-10 mL) every 5 minutes.
- After 4 hours without throwing up, double the amount.
- Return to Formula. After 8 hours without throwing up, go back to regular formula.

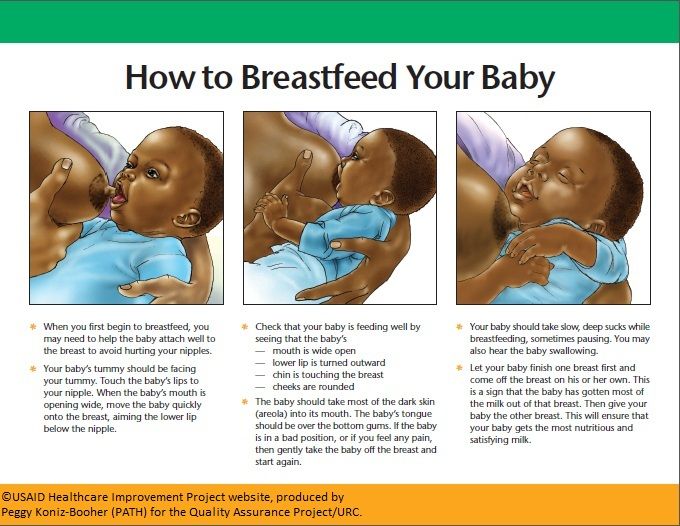
- Breastfed Babies - Reduce the Amount Per Feeding:
- If vomits once, nurse half the regular time every 1 to 2 hours.
- If vomits more than once, nurse for 5 minutes every 30 to 60 minutes. After 4 hours without throwing up, return to regular nursing.
- If continues to vomit, switch to pumped breastmilk. (ORS is rarely needed in breastfed babies. It can be used if vomiting becomes worse).
- Spoon or syringe feed small amounts of pumped milk. Give 1-2 teaspoons (5-10 mL) every 5 minutes.
- After 4 hours without throwing up, return to regular feeding at the breast. Start with small feedings of 5 minutes every 30 minutes. As your baby keeps down the smaller amounts, slowly give more.
- Pumped Breastmilk Bottle-Fed Infants - Reduce the Amount per Feeding:
- If vomits once and bottle-feeding breastmilk, give half the regular amount every 1-2 hours.
- If vomits more than once within last 2 hours, give 1 ounce (30 mL) every 30 to 60 minutes.
- If continues to vomit, give 1-2 teaspoons (5-10 mL) every 5 minutes. Only if not tolerating breastmilk, switch to ORS (e.g., Pedialyte) for every 5 minutes for a few hours.
- After 4 hours without vomiting, return to regular feedings. Start with 1 ounce (30 mL) every 30 minutes and slowly increase as tolerated.
- Stop All Solid Foods:
- Avoid all solid foods and baby foods in kids who are vomiting.
- After 8 hours without throwing up, gradually add them back.
- If on solid foods, start with starchy foods that are easy to digest. Examples are cereals, crackers and bread.
- Do Not Give Medicines:
- Stop using any drug that is over-the-counter for 8 hours. Reason: Some of these can make vomiting worse.
- Fever. Mild fevers don't need to be treated with any drugs. For higher fevers, you can use an acetaminophen suppository (such as FeverAll). This is a form of the drug you put in the rectum (bottom).
 Ask a pharmacist for help finding this product. Do not use ibuprofen. It can upset the stomach.
Ask a pharmacist for help finding this product. Do not use ibuprofen. It can upset the stomach. - Call your doctor if: Your child vomits a drug ordered by your doctor.
- Try to Sleep:
- Help your child go to sleep for a few hours.
- Reason: Sleep often empties the stomach and removes the need to vomit.
- Your child doesn't have to drink anything if his stomach feels upset and he doesn't have any diarrhea.
- Return to Child Care:
- Your child can return to child care after the vomiting and fever are gone.
- What to Expect:
- For the first 3 or 4 hours, your child may vomit everything. Then the stomach settles down.
- Vomiting from a viral illness often stops in 12 to 24 hours.
- Mild vomiting and nausea may last up to 3 days.
- Call Your Doctor If:
- Vomits clear fluids for more than 8 hours
- Vomiting lasts more than 24 hours
- Blood or bile (green color) in the vomit
- Stomach ache present when not vomiting
- Dehydration suspected (no urine in over 8 hours, dark urine, very dry mouth, and no tears)
- You think your child needs to be seen
- Your child becomes worse
And remember, contact your doctor if your child develops any of the 'Call Your Doctor' symptoms.

Disclaimer: this health information is for educational purposes only. You, the reader, assume full responsibility for how you choose to use it.
Last Reviewed: 02/28/2023
Last Revised: 12/30/2022
Copyright 2000-2023 Schmitt Pediatric Guidelines LLC.
Spitting up and vomiting in infants
Spitting up and vomiting in babies is a common reason for visiting a doctor.
Regurgitation and vomiting is a reflex action that occurs when receptors located in various anatomical zones are irritated, incl. in the stomach, esophagus, pharynx, oral cavity. The signal is transmitted to the vomiting center, which is located in the medulla oblongata and a gag reflex occurs.
What is the difference between regurgitation and vomiting?
The difference lies in the volume and kinetics (movement) of the gastric contents expelled to the outside. When regurgitation occurs, leakage occurs without the participation of the diaphragm and abdominal muscles, i. e. passively. There is little content, up to about 10-15 ml. If the child does not swallow it, it quietly expires from the oral cavity. When vomiting, a wave-like bending of the upper half of the body occurs as a result of contraction of the muscles of the diaphragm and the anterior wall of the abdomen, the volume of vomit is greater, and they are erupted with pressure from the oral cavity with an ejection trajectory of up to 50 cm. In children of the first year of life, this is defined by the term "fountain vomiting" .
e. passively. There is little content, up to about 10-15 ml. If the child does not swallow it, it quietly expires from the oral cavity. When vomiting, a wave-like bending of the upper half of the body occurs as a result of contraction of the muscles of the diaphragm and the anterior wall of the abdomen, the volume of vomit is greater, and they are erupted with pressure from the oral cavity with an ejection trajectory of up to 50 cm. In children of the first year of life, this is defined by the term "fountain vomiting" .
Regurgitation is observed only in children of the first year of life and, mainly, up to 6 months. Contribute to this anatomical and physiological features of the esophagus and stomach of the baby. Their esophagus is short and wide, the angle of connection of the esophagus with the stomach is less pronounced, and its obturator function is weak. These regurgitations are physiological. They can be after each feeding, up to 15 ml, do not affect the well-being and weight gain of the baby. They can also be caused by excessive feeding, aerophagia (swallowing air while sucking), straining during intestinal colic. The frequency and volume of such regurgitation decreases with the growth of the child. With the introduction of complementary foods, and this is a thicker food, regurgitation stops or becomes much less frequent.
They can also be caused by excessive feeding, aerophagia (swallowing air while sucking), straining during intestinal colic. The frequency and volume of such regurgitation decreases with the growth of the child. With the introduction of complementary foods, and this is a thicker food, regurgitation stops or becomes much less frequent.
If regurgitation persists in a child older than 1 year, then this is a sign of a pathological process.
Vomiting, unlike regurgitation, is accompanied by vegetative symptoms - increased salivation, pallor of the skin, palpitations. This is due to the fact that next to the vomiting center there are additional centers of autonomic regulation, which are reflexively excited, and active biological substances such as serotonin, dopamine, histamine and others are released into the blood.
Regurgitation and vomiting, from the moment of eating, may occur during feeding, after feeding for the first 20-30 minutes or delayed, sometimes after several hours.
Regurgitation and vomiting that occurs immediately after feeding unchanged breast milk or formula may be due to narrowing of the esophagus. If they persist until the next feeding, and the milk / mixture is curdled, has a sour or musty smell, then this is the result of a long standing food in the stomach. The reason for this may be the low tone of the muscle layer of the stomach and, as a result, its peristalsis or narrowing of the output section due to an anomaly in the development or high tone of the sphincter of the lower stomach. With narrowing of the duodenum, bile is present in the regurgitated masses.
Gastroesophageal reflux is a common cause of regurgitation in infants. It is likely that there is a complex problem here, starting with the immaturity of the gastrointestinal tract and disorders of the central nervous system. Perinatal injuries of the central nervous system accompany every second child. Their manifestations are varied. Regurgitation and vomiting can be facilitated by an increase in intracranial pressure, disorders in the segment of the cervical spine, and so on. Therefore, quite often, when carrying out rehabilitation measures for neurological dysfunctions, a positive effect is manifested in the form of a decrease or cessation of regurgitation. A hernia of the esophageal opening of the diaphragm will also manifest itself in a similar way.
Therefore, quite often, when carrying out rehabilitation measures for neurological dysfunctions, a positive effect is manifested in the form of a decrease or cessation of regurgitation. A hernia of the esophageal opening of the diaphragm will also manifest itself in a similar way.
We should not forget about allergic gastrointestinal reactions in the form of regurgitation and vomiting. The most common cause of this is cow's milk protein. With intolerance to cow's milk protein, inflammation of the mucous membrane of the esophagus, stomach and intestines occurs. And, as a result of this, regurgitation and vomiting, pain and increased gas formation, diarrhea or constipation.
Rare endocrine disorders (adrenogenital syndrome) are manifested by vomiting in children from the first weeks of life. In such cases, vomiting is frequent, there may be an admixture of bile, the child loses weight due to loss of fluid and nutrients, and severe metabolic disorders develop.
Vomiting can also be caused by an intestinal infection. Viral gastroenteritis is now common. It must be remembered that the younger the child, the more severe the disease. Within a few hours, the child's condition can go from satisfactory to extremely serious.
Viral gastroenteritis is now common. It must be remembered that the younger the child, the more severe the disease. Within a few hours, the child's condition can go from satisfactory to extremely serious.
As you can see, the causes of regurgitation and vomiting in children of the first year of life are quite diverse, but most often these are transient conditions that disappear with the growth of the child.
Prevention of regurgitation in children of the first months of life is quite simple. Don't overfeed your baby. If he cries, it does not always mean that he is hungry. Excess feeding leads to increased gas formation and colic, during which the child is worried, straining, thereby increasing the likelihood of spitting up. After feeding, hold the baby more upright so that he can burp the swallowed air. This will take 15-20 minutes. If the child is bottle-fed, do not change his formula milk without the recommendation of a pediatrician.
If the child has frequent regurgitation and vomiting, it is necessary to consult a pediatrician or gastroenterologist to diagnose the cause.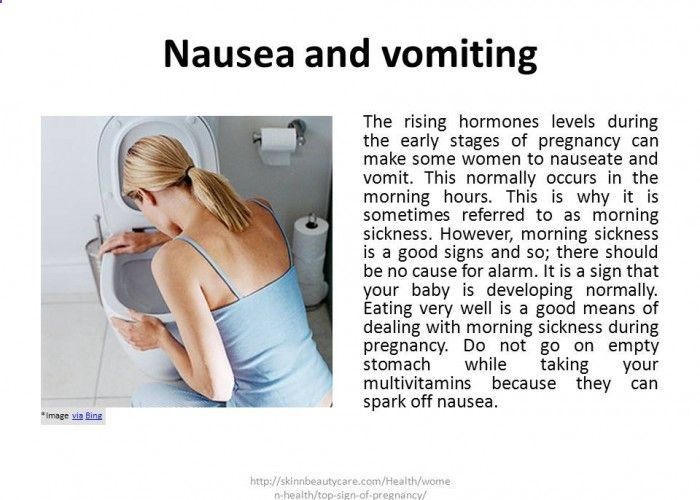 To make a diagnosis, it is sometimes enough to carry out simple and affordable diagnostic methods in a polyclinic. These include an ultrasound of the stomach and, if necessary, stool tests. However, the approach in each case is individual. Examination and treatment will be assigned to your baby, depending on the diagnosis. Perhaps it will be preventive measures or a certain milk formula, perhaps drug therapy. Rarely, but it happens that it is necessary to examine the child in a hospital and surgical treatment.
To make a diagnosis, it is sometimes enough to carry out simple and affordable diagnostic methods in a polyclinic. These include an ultrasound of the stomach and, if necessary, stool tests. However, the approach in each case is individual. Examination and treatment will be assigned to your baby, depending on the diagnosis. Perhaps it will be preventive measures or a certain milk formula, perhaps drug therapy. Rarely, but it happens that it is necessary to examine the child in a hospital and surgical treatment.
Article | Neurotic vomiting in children
Bobylova M.Yu. (neurologist)
Vomiting in children is not an independent disease, but a manifestation of various diseases. Vomiting can be caused by disorders of the gastrointestinal tract, metabolic diseases, tonsillitis, inflammation of the nasopharynx, pneumonia, influenza, SARS, acute appendicitis. Such vomiting is treated by a pediatrician. But there are also vomiting associated with dysfunction of the central nervous system. It develops in children of the first months of life who have undergone hypoxia during fetal development or childbirth. After 6 months, habitual vomiting is often associated with improper introduction of complementary foods if the child is force fed. Also, vomiting can be a sign of increased intracranial pressure. Vomiting attacks are characteristic of the childhood form of migraine.
But there are also vomiting associated with dysfunction of the central nervous system. It develops in children of the first months of life who have undergone hypoxia during fetal development or childbirth. After 6 months, habitual vomiting is often associated with improper introduction of complementary foods if the child is force fed. Also, vomiting can be a sign of increased intracranial pressure. Vomiting attacks are characteristic of the childhood form of migraine.
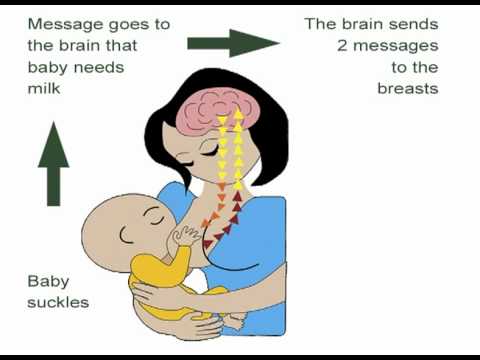
In infants , especially in the first 3 months of life, regurgitation of a small amount of food (15-30 ml) 2-3 times a day is a common occurrence that disappears with the growth of the child. The horizontal position of the baby and the relatively large amount of food predispose to the occurrence of regurgitation in healthy infants. It is also characteristic of regurgitation when swallowing air during breastfeeding, when there is not enough breast milk in the mammary gland, or when the baby does not capture the areola. With artificial feeding - swallowing of air occurs when the nipple is not completely filled with milk, when there is a large hole in the nipple, when the position of the bottle during artificial feeding is horizontal.
With artificial feeding - swallowing of air occurs when the nipple is not completely filled with milk, when there is a large hole in the nipple, when the position of the bottle during artificial feeding is horizontal.
Swallowing air is more common in infants who are hyperexcitable, greedily sucking, and also with general muscular hypotension.
Regurgitation, unlike vomiting, occurs suddenly, does not affect the behavior and general well-being of the child, while children do not lose weight gain.
Helping a baby with spitting up: firstly, immediately after feeding and during sleep, you should hold the baby in an upright position. If regurgitation has occurred, it is necessary to turn the child's head to one side, toilet the child's nose and mouth (clean it from food debris). Wash and caress the baby.
Feeding rules must be observed: the baby should be fed in a semi-upright position, which helps to expel swallowed air. These babies should sleep with their heads up.
If regurgitation is frequent and profuse, and the baby begins to lag behind in weight, then this may be a manifestation of a disease of the stomach or intestines (pylorospasm or pilostenosis). It is necessary to contact a pediatrician for timely examination, diagnosis, treatment and prevention of complications.
Neurological disorders as a cause of vomiting in a child
The vomiting center of a person is located in the brain, therefore, in case of any damage to the head (trauma, infection, vegetative-vascular dystonia, increased intracranial pressure), vomiting occurs not associated with food intake and fever .
Vomiting in children under 1 year of age is associated with hypoxia during fetal development and at birth.
Neurotic vomiting develops as a manifestation of neurotic reactions in response to nasty and undesirable actions: coercion, protest against punishment, feeding. Functional vomiting in such children is more often combined with refusal to eat, with selectivity in food, behavioral changes, and stubbornness. More common is functional vomiting in children who are emotional, easily excitable, vulnerable. There are no signs of intoxication of the body, pain in the stomach, diarrhea or temperature in the child. This behavior requires prompt treatment to a neurologist.
More common is functional vomiting in children who are emotional, easily excitable, vulnerable. There are no signs of intoxication of the body, pain in the stomach, diarrhea or temperature in the child. This behavior requires prompt treatment to a neurologist.
Vomiting in children, even if it is not accompanied by diarrhea and fever, requires the attention of parents. In no case should you self-medicate, since for each disease the methods of treatment are different.
Only a doctor can recognize the causes of the problem after a series of examinations. To clarify the cause of constant vomiting in a child, it is necessary to clarify when it began, what kind of character it is (periodic, after each feeding), whether it is somehow connected with food intake and with the time of day. Important information about possible diseases is also provided by the diagnosis of vomit. The masses are checked for the presence of mucus, bile, milk, blood, digested and undigested food debris. When making a diagnosis, the age of the child is taken into account.