Baby feeding guide canada
Feeding your baby in the first year
Feeding your baby in the first year of life is an exciting adventure for parents and babies alike. It’s about development, nutrition, curiosity, sharing and learning. Attachment also grows as you go about your daily routine with your baby.
You can help your baby develop a lifetime of healthy eating habits with the right start.
The first 6 months
For the first 6 months of life, breastfed babies will get what they need from their mother’s milk.
- Babies who are exclusively or partially breastfed should get a daily supplement of vitamin D, which is available as drops.
- Breast milk has the right amount and quality of nutrients to suit your baby’s first food needs.
- Breast milk also contains antibodies and other immune factors that help your baby prevent and fight off illness.
If breastfeeding is not an option, use a store-bought iron-fortified infant formula for the first 9 to 12 months.
- Formula should be cow milk-based.
- Homemade formulas made from canned, evaporated, whole milk (cow or goat), or any plant-based beverage, are not recommended as a breast milk substitute.
- Homemade formulas can contain harmful germs and lack important nutrients that can make your baby sick.
- Rice, soy, almond or other plant-based beverages, even when fortified, are not appropriate as a breastmilk substitute as they are nutritionally incomplete for infants. There is no evidence that soy-based formula will prevent your child from developing an allergy.
- Soy-based infant formulas should only be used as an alternative to cow milk-based formula if your baby has galactosemia (a rare disorder that will affect how your baby’s body processes simple sugar) or if your baby cannot consume dairy-based products for cultural or religious reasons.
- Talk to your doctor if you are unsure which formula is best for your child.
If your baby has allergies, or if allergies run in the family, see below for specific recommendations about when and how to introduce allergenic foods (such as eggs or peanuts).
Introducing solid foods
At about 6 months, most babies are ready for solid foods. Along with other foods, you can continue to breastfeed as long as it is comfortable for you and your baby, even well into the toddler years.
You’ll know baby is ready to start other foods when they:
- Can sit up without support, lean forward, and have good control of their neck muscles.
- Ability to pick up food and try to put it in their mouth.
- Hold food in their mouth without pushing it out with their tongue right away.
- Show interest in food when others are eating.
- Open their mouth when they see food coming their way.
- Can let you know they don’t want food by leaning back or turning their head away.
Remember that all babies are different. Some babies may be ready a few weeks before or just after 6 months. However, waiting after 6 months to introduce other foods increases your baby’s risk of iron deficiency.
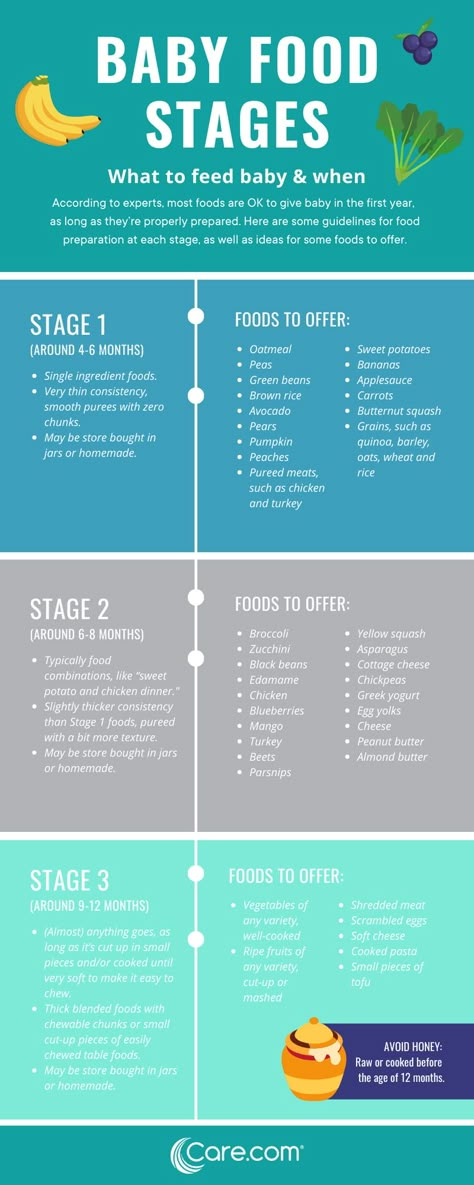
What foods should we start introducing our baby to first?
There are many ways to introduce solid food.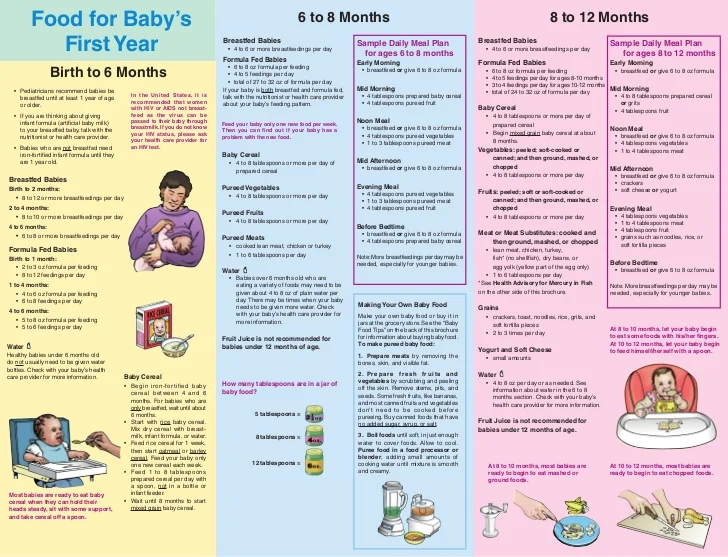 The first foods usually vary from culture to culture and from family to family.
The first foods usually vary from culture to culture and from family to family.
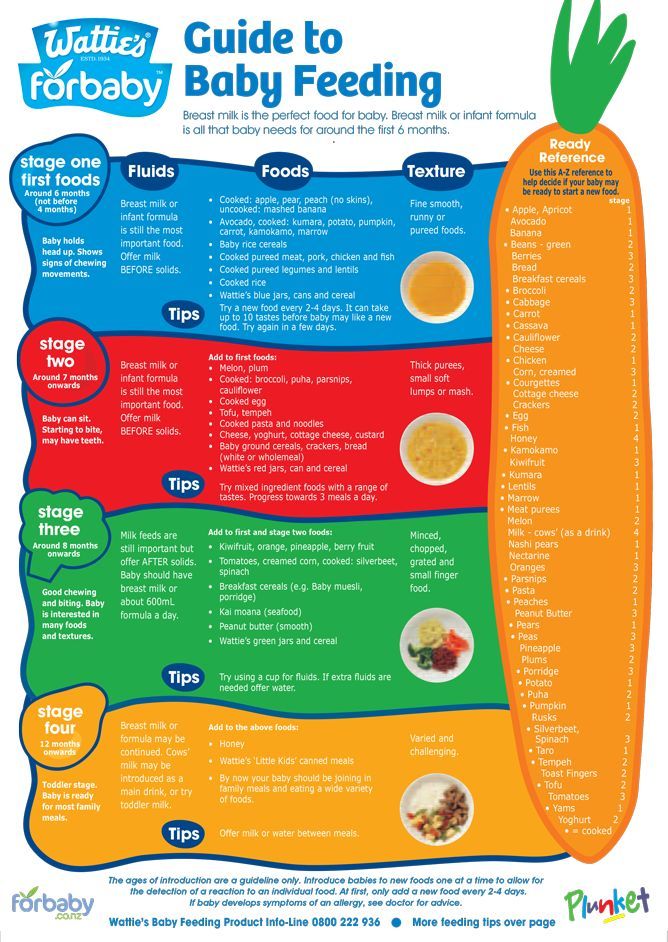
Start with foods that contain iron, which babies need for many different aspects of their development. Meat, poultry, cooked whole egg, fish, tofu, and well-cooked legumes (beans, peas, lentils) are good sources of iron. Store-bought iron-fortified infant cereals such as oat, wheat, barley or rice are also common first foods because they are good sources of iron. Offer iron-rich foods at least twice per day.
Healthy foods that your whole family is eating are the best choice for your baby. You can use commercial baby foods, but read the label to ensure there is no added salt or sugar. A variety of textures (such as lumpy, tender-cooked and finely minced, puréed, mashed or ground), and soft finger foods are recommended. As baby gets older, offer foods with more texture.
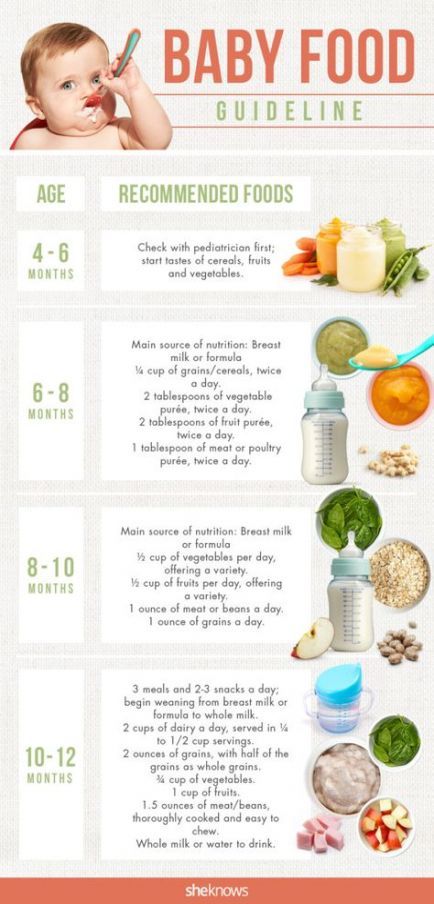
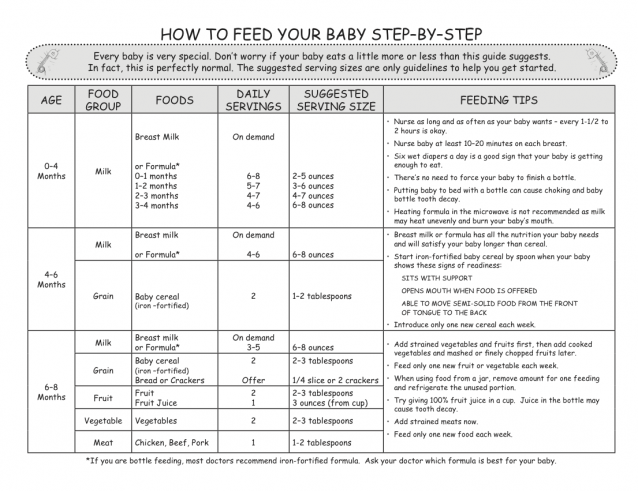
| First foods - Around 6 months | |
|---|---|
| Iron-rich foods | Puréed, minced, diced or cooked meat, fish, chicken, tofu, mashed beans, peas or lentils, eggs, iron-fortified infant cereal.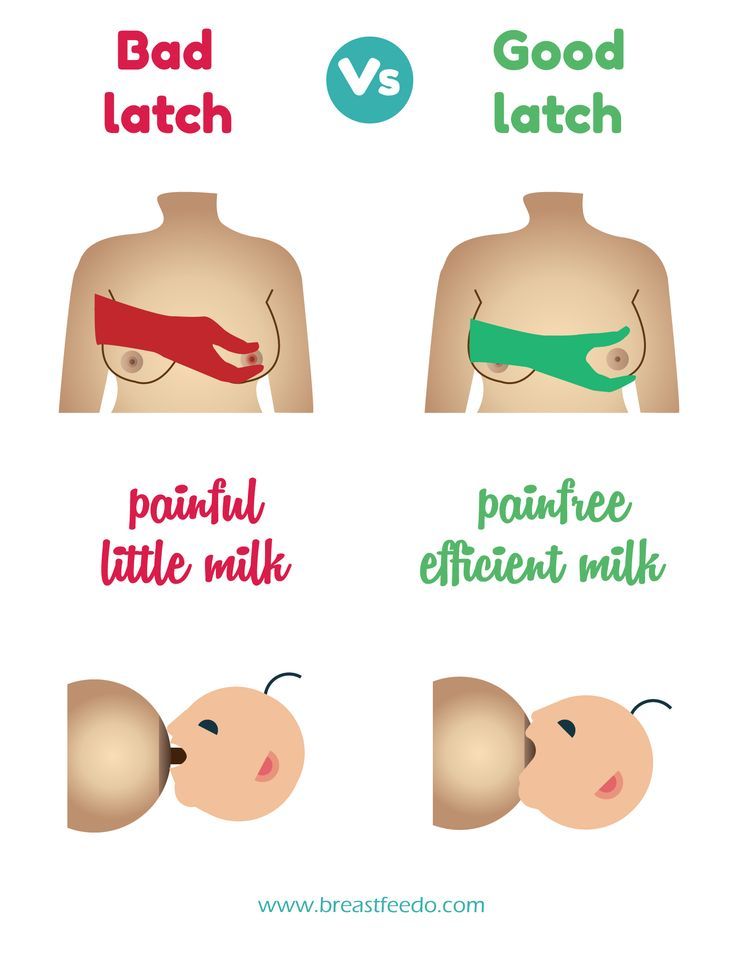 |
| After 6 months | |
| Grain products | Iron-fortified infant cereal, small pieces of dry toast, small plain cereals, whole grain bread pieces, rice and small-sized pasta. |
| Vegetables | Puréed, mashed, lumpy or pieces of soft cooked vegetables. |
| Fruit | Puréed, mashed or lumpy soft fruit. Pieces of very ripe soft fresh fruit, peeled, seeded and diced or canned fruit (not packed with syrup). |
| Milk products | Dairy foods like full-fat yogurt, full-fat grated or cubed pasteurized cheeses, cottage cheese. |
| 9 to 12 months | |
| Milk | Whole cow’s milk (3.25%) can be introduced if breastmilk is no longer available, between 9-12 months. After 12 months of age, your baby should not take more than 25 ounces (750 mL) of milk per day. |
Introducing common food allergens
You can start to introduce common allergenic foods—like peanut products or eggs—when you are starting your baby on other solid foods, usually around 6 months of age.
However, if your baby is at high risk of developing an allergy (has allergies such as eczema, or a parent or sibling with an allergic condition) you can start after baby is 4 months old, but not sooner. Talk to your doctor if you are unsure.
Waiting until after 6 months to try to prevent an allergy is not recommended.
- When introducing foods that are common food allergens, it’s best to offer no more than one new food per day. You may want to wait a day or two before you introduce another. This makes it easier to identify a food that may have caused a reaction.
- If your baby is tolerating the allergenic food, continue offering it a few times a week to maintain tolerance.
 If an allergic reaction occurs, contact your doctor.
If an allergic reaction occurs, contact your doctor. - Make sure these new foods are smooth and small enough so that your baby isn’t at risk of choking. When introducing peanut products to young infants, try mixing a bit of peanut butter with some water, breast milk, or a puréed fruit or vegetable that your baby has had before. For older infants, spread a bit of smooth peanut butter on a piece of thin toast crust or offer a peanut puff product.
How much should I feed my baby?
Follow your baby’s cues for how much to feed. Start by offering a teaspoon or two. Don’t rush. Some babies need to try a food many times before accepting it. If she’s not hungry, she’ll turn her head and close her mouth. If she’s hungry, she’ll get excited and open up.
Never trick or coax her to eat more by playing games or offering sweetened foods. Babies who are allowed to follow their own hunger cues are much less likely to overeat later in life.
Try foods with different tastes and textures to help your baby learn how to handle foods in her mouth.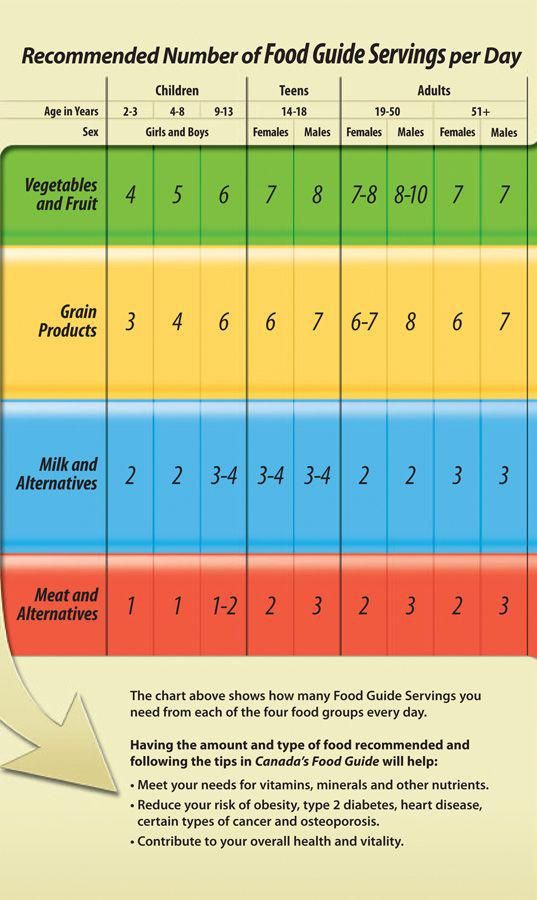
Water and juice
Babies who are exclusively breastfed don’t need extra water. When your baby begins to eat other foods, you can start to offer water occasionally, in an open cup.
- Babies and children don’t need to drink juice. Too much juice can cause diarrhea and can fill up small stomachs, decreasing your baby’s appetite for nutritious foods. Too much juice can also cause early childhood tooth decay.
- Offer water to babies and young children between meals and snacks if they are thirsty. If you choose to offer juice, be sure it is only 100% fruit juice (with no added sugar). Limit juice to 125 mL (4 oz.) per day.
Are there any foods my baby shouldn’t eat?
- Babies shouldn’t be offered sugary drinks or foods, such as candies, soda/pop or energy drinks.
- Don’t give honey to babies under a year old, as there is a risk of infant botulism (food poisoning).
- If you have concerns, please speak to your health care provider.

Is there anything else I should know about feeding my baby?
- Always wash your hands before preparing your baby’s food, and wash your baby’s hands before they eat.
- Wipe your baby’s gums with a soft, damp cloth twice a day for good oral health.
How can I prevent choking?
Young children don’t know how to chew food into tiny pieces. And they haven’t learned how to bring a piece of food back up when it gets caught going down. Foods most likely to cause choking are small, round or cylindrical in shape, like hot dogs, whole grapes, carrot slices, seeds and hard candy.
To protect your baby:
- Always supervise them while they are eating.
- Make sure your baby is sitting down to eat.
- Grate raw vegetables such as carrots to make them easier to chew.
- Cook hard fruits and vegetables to soften them.
- Slice round foods such as hot dogs or grapes lengthwise.
- Remove pits from fruits.

- Chop or scrape stringy meat and add broth to moisten it.
- Spread sticky foods like nut butters thinly on a cracker or toast rather than bread.
- Don’t feed your baby whole nuts, raisins, popcorn, gummy candies, hard candy, or fish with bones.
Developmental milestones related to feeding
| Age | Physical milestones | Social milestones |
|---|---|---|
| Birth to 4 months |
|
|
| 4 to 6 months |
|
|
| 6 to 9 months |
|
|
| 9 to 12 months |
|
|
| 12 to 18 months |
|
|
| 18 to 24 months |
|
|
More information from the CPS
Additional resources
Reviewed by the following CPS committees
- Allergy Section
- Nutrition and Gastroenterology Committee
- Public Education Advisory Committee
Last updated: January 2020
Introducing Solid Foods to Your Baby
Topic Contents
- Topic Overview
- Related Information
- References
- Credits
Topic Overview
Canadian experts recommend giving only breast milk for the first 6 months and continuing to breastfeed for up to two years and beyond. footnote 1 Breast milk is the ideal food for babies. If you are not able to breastfeed your baby, feed your baby iron-fortified formula. Babies don't need any other liquids or solids for the first 6 months of life.
footnote 1 Breast milk is the ideal food for babies. If you are not able to breastfeed your baby, feed your baby iron-fortified formula. Babies don't need any other liquids or solids for the first 6 months of life.
Breastfed babies and babies fed a combination of breast milk and formula need 400 IU of vitamin D each day from a supplement.footnote 1, footnote 3 Babies who are fed only formula do not need a vitamin D supplement.
Your baby is ready to start eating solid foods at 6 months of age, which is around the time he or she:
- Demonstrates a curiosity about solid foods and your family's eating behaviour.
- Has started to transition from using the sucking reflex to swallowing and does not push a spoon or other object out with the tongue when it is placed in the mouth.
- Can sit with support.
- Has good head and neck control.
When your baby is ready to start eating solid foods, keep these general guidelines in mind:
- Continue to offer breast milk or formula while introducing solid foods.
- Offer your baby iron-rich foods first, such as iron-fortified infant cereal, finely minced meat or fish, mashed cooked egg yolk, mashed beans, or tofu.
- The order in which other foods from Canada's Food Guide are introduced is not important.
- Don't add cereal to bottles. Instead, spoon-feed your baby cereal that is made with breast milk, formula, or water, gradually making the mixture thicker.
- As the variety in your baby's diet increases, include foods rich in vitamin C—such as oranges, berries, tomatoes, and spinach—along with iron-rich foods. Vitamin C helps your baby absorb iron.footnote 4
- Observe your baby before introducing another new food. This strategy helps you quickly identify a food that may be causing a reaction, such as hives, redness, a rash, vomiting, or diarrhea.
- If you have a family history of allergies, talk to a dietitian or health care provider. Experts do not recommend waiting to introduce any foods in order to prevent allergy. This includes the common allergens such as peanut, tree nuts, egg, milk product (yogurt, cheese), wheat, soy, seafoods, and sesame. You can start offering these foods to your baby at around 6 months.
- Introduce these foods one at a time. This will help you quickly identify whether a food is causing a reaction such as hives, swelling, redness, and a rash.
- If you think your baby has had an allergic reaction to a food, stop offering it and talk to your baby’s doctor.
- Offer your baby a variety of foods with soft textures. He or she can eat food that is lumpy, tender-cooked and finely minced, pureed, mashed, or ground. Offer finger foods like dry cereal, crunchy toast, well-cooked noodles, small pieces of chicken, cooked egg, and small chunks of banana. Make sure that there are no pieces that could cause your baby to choke such as hard raw vegetables (such as carrots), whole nuts and seeds and lumps of nut butters, popcorn, raisins, candies, and marshmallows.
- Don't feed your baby directly from a food container. Instead, put some of the food onto a small dish. That way, germs from your baby's mouth won't get into the container and spoil the food that is left.
- When you first start, don't choose foods with mixed textures, such as broth with vegetables. These kinds of meals are the hardest for a baby to eat.
- Offer an open cup for liquids other than breast milk or formula. Your baby can use a cup with your help starting around 6 months of age.
 Work toward a goal of not using a bottle or sippy cup by 12 to 18 months of age.
Work toward a goal of not using a bottle or sippy cup by 12 to 18 months of age. - When your baby is no longer breastfeeding or taking formula, your doctor may recommend a vitamin D supplement. Talk with your doctor about how much and what sources of vitamin D are right for your baby.
- When your baby is 9 to 12 months old and eating a variety of iron-rich foods, he or she can start to drink pasteurized whole-fat cow's milk. Limit cow's milk to no more than 3 cups (750 mL) per day for children 9 to 24 months old. If you are not breastfeeding and do not want to give your child cow's milk, give your child soy infant formula until your child is 2 years of age. After age 2, you can serve low-fat milk or fortified alternatives.
- Other kinds of milk such as skim milk, 1% milk, or 2% milk, or fortified soy beverage don't have as many nutrients as whole-fat cow's milk. It is best not to give your baby these beverages, until he or she is 2 years of age.
- Food's made from milk such as yogurt and cheese can be introduced at 6 months as long as your baby is eating a variety of iron-rich foods.
Keep these things in mind, too:
- Always stay with your baby when he or she is eating or drinking.
- Don't add salt or sugar to your baby's food.
- Don't give your baby honey until 1 year of age.
- Don't give your baby sugary drinks or foods.
- Juice is not necessary for a healthy diet. Juice does not have the valuable fibre that whole fruit has. Unless the label says the drink has only 100% juice, beware that many fruit drinks are just water, a little juice flavouring, and a lot of added sugar. The Canadian Paediatric Society recommends limiting juice to ½ cup (125 mL) of 100% unsweetened fruit juice a day. Juice isn't recommended for babies 0 to 6 months.
As you introduce new foods, it is important to pay attention to your baby's cues. When your baby's head turns away from a spoonful of food, don't force it. But try again later. Let your baby tell you when he or she is full. Also, it may help to introduce new foods when your baby is well rested and there are no distractions, such as a TV.
When your baby's head turns away from a spoonful of food, don't force it. But try again later. Let your baby tell you when he or she is full. Also, it may help to introduce new foods when your baby is well rested and there are no distractions, such as a TV.
As your baby learns to feed himself or herself, keep in mind that your job is to provide a variety of nutritious foods, but your baby will decide how much to eat. If your baby doesn't accept a new food right away, try again later. It can take many tries before your child accepts a food.
Your child can sit with you at the table for short periods of time during meals. Sharing meals with your child allows him or her see you eating a variety of foods, which makes it more likely that your child will also eat a variety of foods as he or she gets older.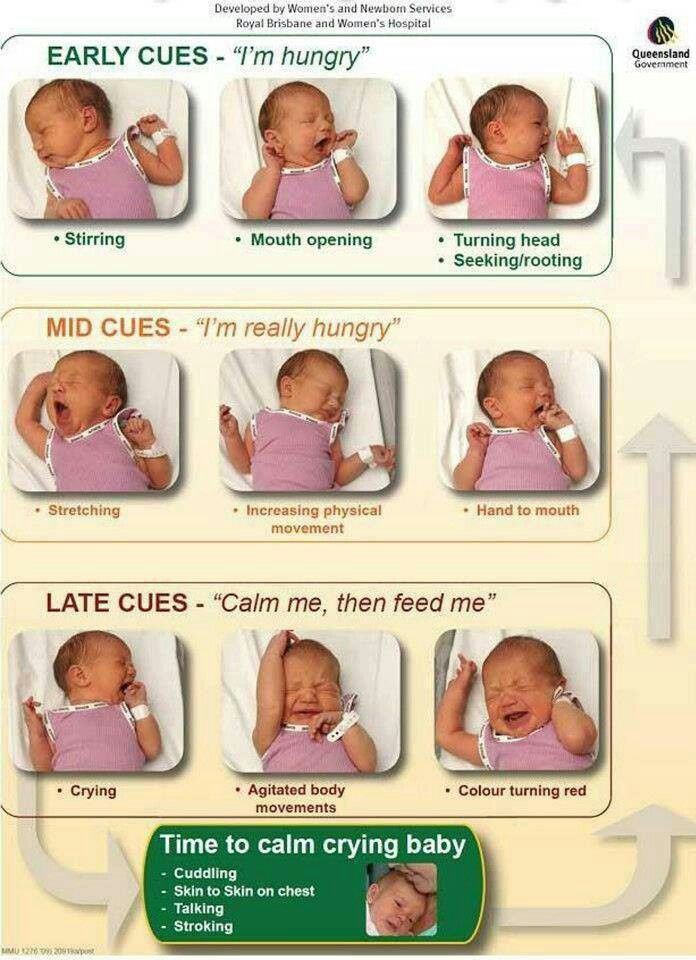 By 12 months, your child will be able to eat many of the same foods the rest of the family eats.
By 12 months, your child will be able to eat many of the same foods the rest of the family eats.
Expect messes
Your baby will quickly gain new eating skills, such as chewing, swallowing, and using cups and utensils, at about 6 to 12 months of age. Offer your baby a variety of nutritious foods and gradually allow him or her to explore different tastes and textures. Try to be patient as your baby experiments and learns, and be tolerant of messes. Your baby will likely enjoy playing with a spoon, but most of the food will fall off it. It's natural for your baby to "make a mess" while learning about food. Until your baby can handle a spoon better, you can give your baby a clean spoon to hold while you feed him or her with a different spoon.
To help reduce your cleanup, use a child's high chair that has a detachable tray and raised rims. The rims on the tray help keep dishes and food from sliding off. And you can carry the tray to the sink for cleaning. Cover the seat with a removable, washable pad. Also, think about covering the floor around the high chair. Remember—your child is learning by experimenting.
The rims on the tray help keep dishes and food from sliding off. And you can carry the tray to the sink for cleaning. Cover the seat with a removable, washable pad. Also, think about covering the floor around the high chair. Remember—your child is learning by experimenting.
References
Citations
- Health Canada, et al. (2012). Nutrition for healthy term infants: Recommendations from birth to six months. A joint statement of Health Canada, Canadian Paediatric Society, Dietitians of Canada, and Breastfeeding Committee for Canada. Available online: http://www.hc-sc.gc.ca/fn-an/nutrition/infant-nourisson/recom/index-eng.php.
- Health Canada, et al. (2014). Nutrition for healthy term infants: Recommendations from six to 24 months. Health Canada. http://www.hc-sc.gc.ca/fn-an/nutrition/infant-nourisson/recom/recom-6-24-months-6-24-mois-eng.php. Accessed April 28, 2014.
- Togias A, et al. (2017).
Addendum guidelines for the prevention of peanut allergy in the United States: Report of the National Institute of Allergy and Infectious Diseases-sponsored expert panel. Journal of Allergy and Clinical Immunology, 139(1): 29-44. DOI: 10.1016/j.jaci.2016.10.010. Accessed August 23, 2017.
- Chan E, et al. (2013). Dietary exposures and allergy prevention in high-risk infants. Canadian Paediatric Society. http://www.cps.ca/documents/position/dietary-exposures-and-allergy-prevention-in-high-risk-infants. Accessed February 12, 2014.
Other Works Consulted
- American Academy of Pediatrics (2010). Diagnosis and prevention of iron deficiency and iron-deficiency anemia in infants and young children (0–3 years of age). Pediatrics, 126(5): 1040–1050. Available online: http://pediatrics.aappublications.org/cgi/content/full/126/5/1040.
Credits
- About This Page
- General Feedback
- Email Link
- Physical Activity Services
We appreciate your feedback. Comments submitted through the form below can help us fix errors in page content, get rid of interface bugs, and update the HealthLinkBC website to better suit the needs of the people who use it.
Comments submitted through the form below can help us fix errors in page content, get rid of interface bugs, and update the HealthLinkBC website to better suit the needs of the people who use it.
To submit feedback about this web page, please enter your comments, suggestions, compliments or questions in the form below. To submit general feedback about the HealthLink BC website, please click on the General Feedback tab.
Page
Content
Functionality
Message:
Your name:
Your email:
To submit general feedback about the HealthLink BC website, please enter your comments, suggestions, compliments or questions in the form below. To submit feedback about a specific web page, please click on the About This Page tab.
Please note that we are unable to provide general health information or advice about symptoms by email. For general health information or symptom advice, please call us at 8-1-1 any time of the day or night.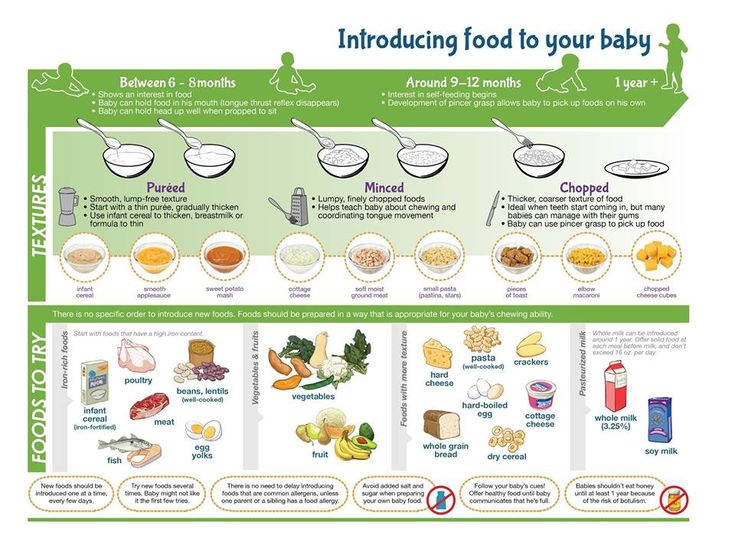
For questions about food and nutrition, please click on Email a HealthLinkBC Dietitian.
What is your message about? -- Select --8-1-1 Telephone ServicesBC Health Service Locater AppBrand Name Food List (BNFL)Website ContentTechnical ProblemsPrint media requirements / Web buttonsOther
Message:
Your name:
Your email:
History of milk exchange from Canada
I have been a breastfeeding mother for 4 years already and I realize all the beauty and sometimes difficulties that accompany this happiness. I have a lot to say on this topic, and without a doubt, this will be the first of many posts you will read about breast milk. I am a big proponent of breastfeeding, but more of an informed choice proponent, as you can see in my articles. Whether you are making decisions about how to feed your child, education, health decisions, or other important challenges we face in our lives, making informed choices is essential. How can a person make the right decision without knowing all the facts? I will add - facts that can be easily manipulated and distorted for the sake of the interests of corporations trying to capitalize on our children and our families.
How can a person make the right decision without knowing all the facts? I will add - facts that can be easily manipulated and distorted for the sake of the interests of corporations trying to capitalize on our children and our families.
It's no secret that "breasts are better."
According to the World Health Organization, “Infants should be exclusively breastfed – receiving only breast milk – for the first 6 months of life to achieve optimal growth, development and health. “Exclusive breastfeeding” means not giving other foods or drinks, not even water, anything but breast milk. Breast milk is an ideal food for the healthy growth and development of babies, and breastfeeding is also an integral part of the reproductive process, which is of great importance for the health of mothers.” All major health organizations support and acknowledge these facts.
… but what happens if mother and baby have difficulty breastfeeding? And although some hospitals are quite progressive in the process of establishing and supporting breastfeeding, they are very quick to offer a bottle of formula to an exhausted and desperate mother, so subsequent breastfeeding attempts may be unsuccessful.
Contrary to popular belief, if a mother cannot breastfeed, artificial milk for infant formula (better known as infant formula) is not the best choice for a baby, and it is not the only option, as many believe.
If the baby needs extra milk, the World Health Organization (WHO) advises giving infant formula only as a last resort. WHO recommendations for infant feeding are as follows:
1) breastfeeding;
2) breast milk expressed manually or with a breast pump using a mug, spoon or special tube for infant feeding; do not use a bottle with a nipple for feeding, because. this can lead to problems with breastfeeding;
3) donor milk;
4) as a last resort, artificial infant formula (World Health Organization (WHO), 2003).
What if you cannot breastfeed yourself? Whether you choose donated milk, infant formula, or a combination of all options, it is without a doubt your personal choice and, ultimately, your difficult path.
There are currently only 2 certified milk banks in Canada, one in Vancouver and the other in Toronto, both with huge waiting lists and mainly for sick children. But shouldn't mother's milk be available to any mother who wants her baby to get it? I think it should, and so do most mothers.
But shouldn't mother's milk be available to any mother who wants her baby to get it? I think it should, and so do most mothers.
Over the past few years, thanks to social media, the informal sharing of mother's milk through communities has gained immense popularity. HumanMilkforHumanBabies and EatsonFeets, two such communities easily found on Facebook, are created by a group of local mothers, both donors and recipients, who want to share, interact and do what they think is best for their children. (These communities operate in the US and Canada; in Russia, you can find and donate breast milk through the Dairy Mom website - ed.) And again, an informed choice is a decisive moment in such groups. Women who give milk give a full description of their lifestyle, drug treatment, etc. and show copies of blood tests upon request. Women who take breastmilk, like me, are passionately interested in giving human milk to a human baby.
Our history of milk exchange - both receiving and donating
I was happy when I had a very strong bond with my first child from the very beginning. Even before he was born, I knew that I wanted to breastfeed. It seemed natural to me. Despite the fact that I was 26 years old, I was a little scared, because. I was the first of all my friends to have a baby, and I had never seen a baby being breastfed. It may sound funny, but I purposefully watched YouTube videos of mothers breastfeeding their babies in order to mentally (and technically) prepare for breastfeeding, and it really helped! Thanks to skin-to-skin contact and being at the breast immediately after birth, my son and I entered into a breastfeeding routine very quickly.
Even before he was born, I knew that I wanted to breastfeed. It seemed natural to me. Despite the fact that I was 26 years old, I was a little scared, because. I was the first of all my friends to have a baby, and I had never seen a baby being breastfed. It may sound funny, but I purposefully watched YouTube videos of mothers breastfeeding their babies in order to mentally (and technically) prepare for breastfeeding, and it really helped! Thanks to skin-to-skin contact and being at the breast immediately after birth, my son and I entered into a breastfeeding routine very quickly.
Skin-to-skin contact and plenty of time at the breast helped my first son and me successfully breastfeed
A few months have passed. I was happy with a lot of milk, I expressed it daily and froze it. 4 months after the birth of my first son, I was surprised to find out that I was expecting a child again! (Don't believe grandma's stories about not getting pregnant while breastfeeding, because it happened to me!). I was excited and continued to feed.
I was excited and continued to feed.
I didn't realize at the time that women who are pregnant and breastfeeding at the same time can have difficulty producing milk. I was lucky - for a while we had no problems; but when a friend asked me if I was experiencing any changes with milk, I began to study this topic. In most women, the hormones produced during pregnancy can suppress the hormones a woman needs for lactation. Since our hormones are constantly changing during pregnancy, breastfeeding, or both, it is understandable why the amount of milk can change.
With this knowledge, I made the decision to continue breastfeeding - breastfeeding as often as possible, pumping between feeds, and taking natural lactation boosters such as More Milk Two, which were safe to take during pregnancy to support milk production. milk. (At the moment, there are no natural drugs whose effectiveness for stimulating lactation has been proven in the course of studies. However, mothers can take one or another drug, since different countries have different traditions in this regard - ed. note)
note)
In the third trimester, I began to notice a significant decrease in milk production, it became clear that something had to be done about it. Luckily, I had frozen milk while my son was still small and didn't eat solid foods, he was still dependent on his mother's milk as his main food (remember, eating from a common table for up to a year is entertainment).
I didn't know anything about milk exchange then, but being a true breastfeeding advocate at heart, I needed to know if I had exhausted my options before resorting to formula. First of all, I reached out to a member of my family who I knew was breastfeeding. I was a little confused, and honestly, I had no idea how she would react to my request to express some milk for my baby. I was afraid to address her with such a request, I did not know how to do it. As formal as it sounds, I emailed her with my thoughts and request. Since this was not an ordinary request, I felt it would take her some time to digest what I had written before responding.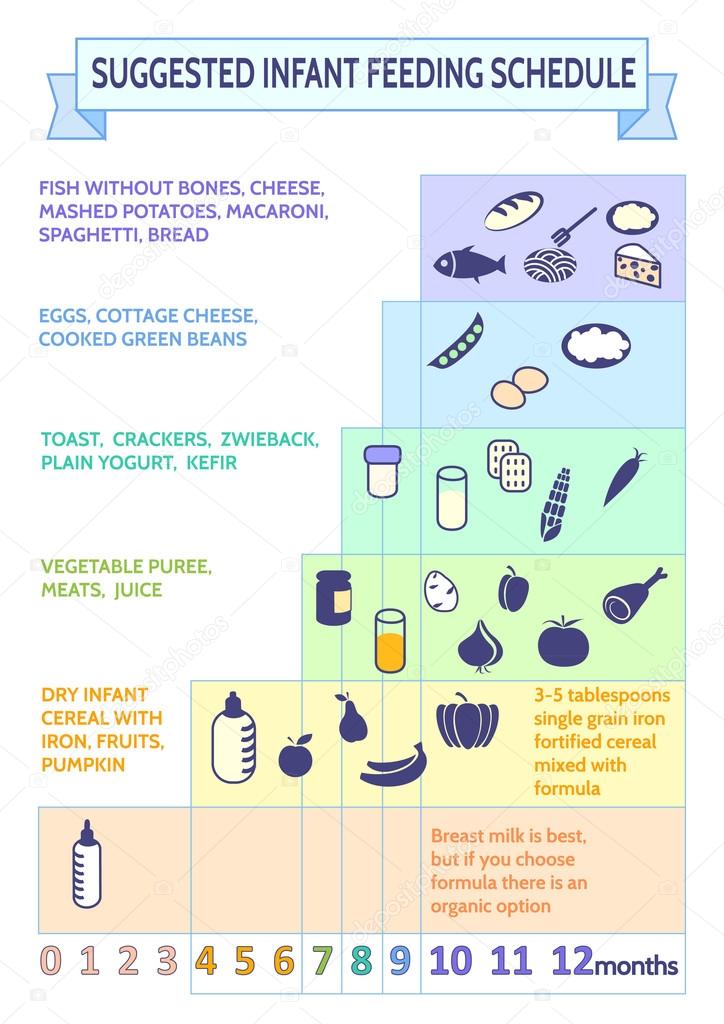 We were SO lucky that she was happy to help! For a while, I could continue to breastfeed and give her extra milk and my frozen supply, but still we needed more milk. At the same time, I came across an article in a local Toronto newspaper that talked about a new trend among mothers: an informal community for the exchange of mother's breast milk was gaining strength through social networks.
We were SO lucky that she was happy to help! For a while, I could continue to breastfeed and give her extra milk and my frozen supply, but still we needed more milk. At the same time, I came across an article in a local Toronto newspaper that talked about a new trend among mothers: an informal community for the exchange of mother's breast milk was gaining strength through social networks.
I immediately consulted the information I could find on the Internet and joined the local milk exchange community. There I found several mothers in my area who became great friends and milk donors for my little boy. With their help, I could continue to feed my son for the rest of the pregnancy with my own milk, which was becoming less and less, and also gave donor milk. This is a gift that I will always be grateful for.
My boys were 13 months apart when my youngest was born, I was still breastfeeding my oldest and tandem feeding seemed like the next natural step for me. Tandem feeding is when two half-brothers (or sisters) of different ages breastfeed together. It may give you some trouble, but personally in my case it was amazing, and it was the best choice for all of us (I think this will be in another post!).
It may give you some trouble, but personally in my case it was amazing, and it was the best choice for all of us (I think this will be in another post!).
Tandem feeding my boys, age difference between them 13 months, was the next natural step in our life journey again rejoiced at its large number. I tandem fed and continued to pump extra. After the amazing support I received through informal milk exchange groups such as HumanMilkforHumanBabies and EatsonFeets, I wanted to give back, to share the gift that every child should receive.
After the birth of my second son in 2011, I was able to give milk to more than 8 babies and older children in my community. Since I am now pregnant again and still breastfeeding, lately I have not been able to give milk because it "rebuilds" for the newborn, but I plan to be a milk donor as soon as my body allows it. I believe this is one of the greatest gifts you can give to a child, a mother, a family. In a world where the feeling of togetherness can be so distant and invisible, the simple act of donating something real, like mother's milk, connects, restores and regenerates the soul.
Milk exchange with my children, as well as with other children, is the most precious and humble gift I have received as a mother. Study information. Go to sites. Read books. Communicate with those you trust. And most importantly, do what feels right for you and your family. You will never know what gift is waiting for you around the corner until you open your soul and your heart. Whatever you need, you will get it, whether you need help or have a desire to help. Every act of sincere giving and receiving will bring you closer to yourself, your family, and the world around you in ways you never imagined.
The full period of breastfeeding and milk exchange is good for your family. This is just a small part of our milk exchange story that I shared with you today. I fully support all mothers as we are all unique and in different situations. I want to share my experience and inspiration with others - to tell about everything that I learned and how I felt. Helping each other is what it's all about.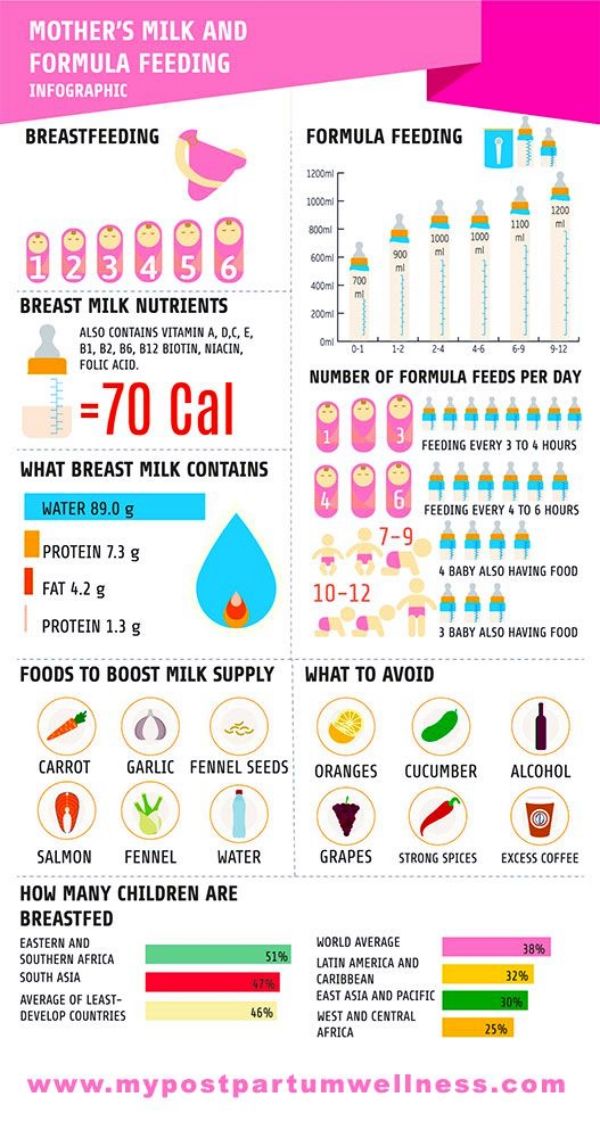 Particularly through milk exchange, we all grow and develop together.
Particularly through milk exchange, we all grow and develop together.
Our history of breast milk exchange continues to this day. Did you have it? Have you ever given or received donor milk? Or maybe both?
With love, Rebecca.
Original: http://consciouscrunch.com/milk-sharing-story/
Translation: Olga E. for Milk Mom
Various Breastfeeding Positions
the one that works best for you and your baby. You can see the options in our selection of photos
Share this information
There is no right or wrong way to hold the baby while
feeding, and mom and baby are sure to find their favorite position.
It is important that both you and your child feel comfortable. 1.2 It's good to learn a few different breastfeeding positions and techniques because life's circumstances often require us to be flexible, especially as your baby gets older and you start to leave the house more often.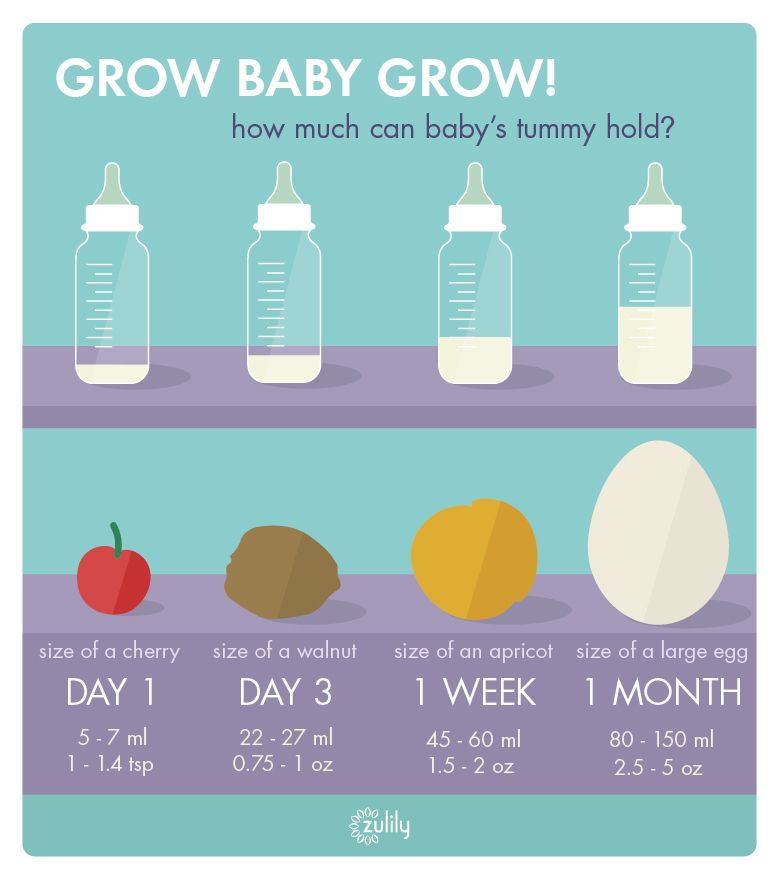
Whatever position you choose to breastfeed your baby, remember a few simple rules.
- Prepare everything you need before feeding, including drinks, food, mobile phone, TV remote control, book or magazine. And do not forget to go to the toilet - the feeding process can take a long time!
- Make sure your baby is comfortable. Whichever position you choose, it's important to keep your baby strong, level, and provide good support for their head, neck, and spine.
- You should also be comfortable. Don't stress. If necessary, use pillows of different sizes or rolls of towels to support your back or arms.
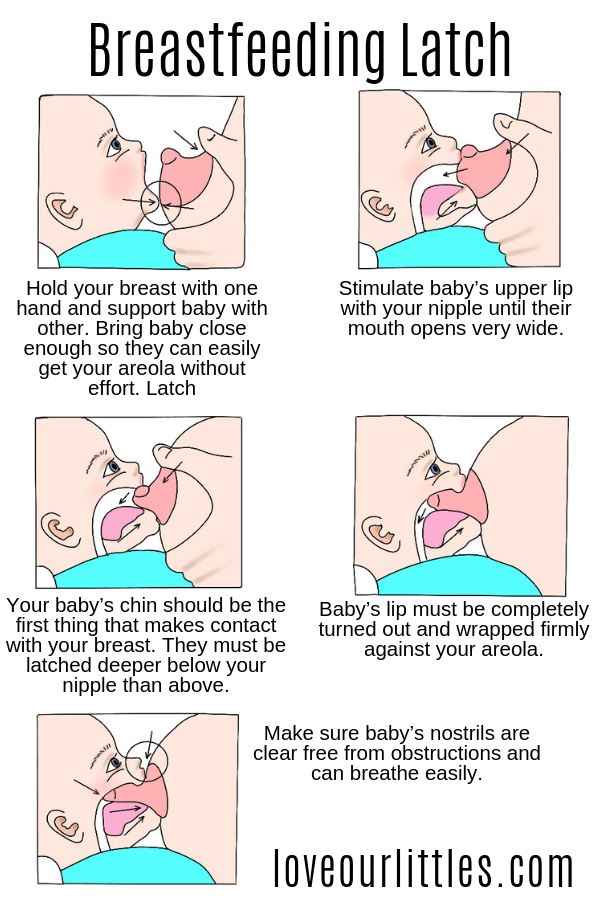
- Make sure your baby is latching on correctly. Proper grip is the key to comfort when breastfeeding.
- If your baby does not latch on well or you experience pain while feeding, contact a lactation consultant for help. The specialist will also be able to show you how to hold your baby more comfortably.
1. Relaxed feeding or reclining position
The relaxed feeding position, also known as biological feeding, 1 is often the first position for most mothers. If, immediately after birth, the baby is placed on the mother’s chest or stomach, normally, he instinctively reaches for the breast and tries to grab the nipple. This phenomenon is known as the breast seeking reflex. Skin-to-skin contact stimulates the infant's feeding instinct, and gravity helps him to latch onto the breast and maintain balance.
If, immediately after birth, the baby is placed on the mother’s chest or stomach, normally, he instinctively reaches for the breast and tries to grab the nipple. This phenomenon is known as the breast seeking reflex. Skin-to-skin contact stimulates the infant's feeding instinct, and gravity helps him to latch onto the breast and maintain balance.
But it's not just newborns that can be fed in the reclining position - this position is great for babies of all ages. It can be especially helpful if your baby does not latch well in other positions or does not like to be touched during feeding, and also if you have too much milk flow or too large breasts. Isabelle, a mother from the UK, shares her experience: “I had large breasts, and the baby was born small - 2.7 kg, so it was not easy to find a comfortable position at first. After a few weeks, it became clear that there was no “correct” posture for me. As a result, I most often fed lying down, putting the baby on my chest. ”
It is more convenient to feed not lying flat on your back, but half-sitting, leaning on pillows.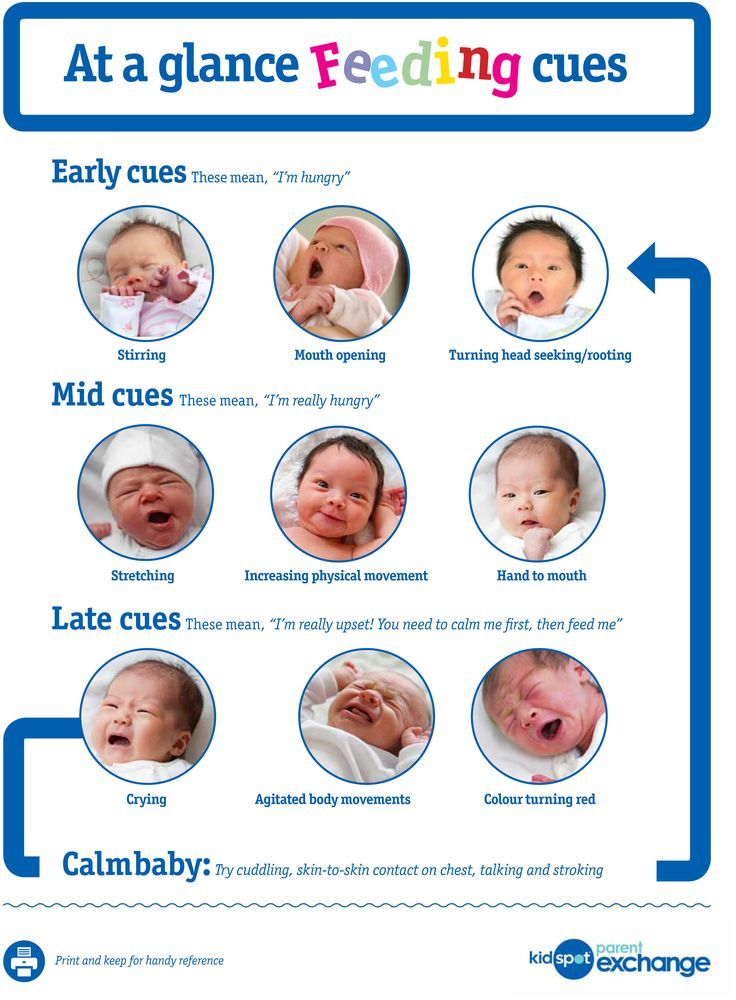 So you will have a back support and you will be able to watch the baby during feeding.
So you will have a back support and you will be able to watch the baby during feeding.
2. Cradle position
This is the classic
first thought of breastfeeding. Mom sits
straight, and the baby lies on her side on her arm, pressing her stomach against her stomach. 3 Although this is a very popular position, it is not always easy to master with newborns because it gives the baby less support. Try putting a pillow under your back, and put a special breastfeeding pillow on your knees and lean on it with your hands. So you can more reliably support the child, without overstraining your back and shoulders. Just make sure that the baby does not lie too high on the pillow for feeding. The breast should remain at a natural level so that the baby can grab it without effort, otherwise sore nipples cannot be avoided.
“I breastfed in the cradle position because it suited me perfectly! It was comfortable and I loved just sitting and looking at my little one,” recalls Rachel, a mother of two from Italy.
3. Cross Cradle
This breastfeeding position looks almost exactly like the cradle, but the baby is on the other arm. 3 This gives your baby support around the neck and shoulders so he can tilt his head to latch on. This position is great for breastfeeding newborns and small babies, as well as for babies who do not latch well. Since the baby lies completely on the other hand, it becomes easier to control his position and you can adjust the chest with your free hand.
Julie, a UK mother of two, finds this position very practical: “I usually breastfeed my youngest in the cross cradle position. So I have a free second hand, and I can take care of an older baby at the same time. ”
Do not hold the baby's head at first, otherwise you may inadvertently press his chin against his chest. Because of this, the child will not be able to take the breast deeply, because the nipple will rest against the base of the tongue, and not against the palate, which will lead to inflammation of the nipples. As the child grows, this position becomes more comfortable, and he can rest his head on your palm (as shown in the photo above).
As the child grows, this position becomes more comfortable, and he can rest his head on your palm (as shown in the photo above).
4. Underarm breastfeeding
In this position, also known as the "ball grip", the mother sits and the baby lies along her arm at the side, legs towards the back of the chair (or any other seat). 3 Another comfortable position for newborn breastfeeding, you can give your baby good support, full control of the position and a good view of his face. And the baby feels safe in close contact with the mother's body. This position is especially good for those who have had a caesarean section or a premature birth, as well as mothers of twins and women with large breasts.
“When I breastfed my first daughter, I had very large K-sized breasts—twice the size of her head,” recalls Amy, an Australian mother of two. - I put rolls of towels under each breast, because they were very heavy, and fed my daughter in a pose from under the arm, but only sitting straighter so as not to crush her. This position was also convenient because I had a caesarean section and could not put the baby on my stomach.”
This position was also convenient because I had a caesarean section and could not put the baby on my stomach.”
5. Side-lying position
The side-lying position is ideal for a relaxed
nighttime feeding in bed or on the couch. If you had a
caesarean section or ruptures during childbirth, this position may be more comfortable than sitting down. 3 In this position, mother and baby lie side by side, tummy to tummy.
“It was difficult for me to sit during endless night feedings, firstly because of the caesarean section, and secondly because of lack of sleep,” recalls Francesca, a mother from the UK. “And then I discovered that you can feed your baby lying on your side and rest at the same time.”
“Because of the short tongue frenulum, Maisie could only properly latch on to her breasts while lying on her side. The lactation consultant showed me how it's done. In this position, the flow of milk was optimal for my daughter, and it was easier for her to keep the nipple in her mouth.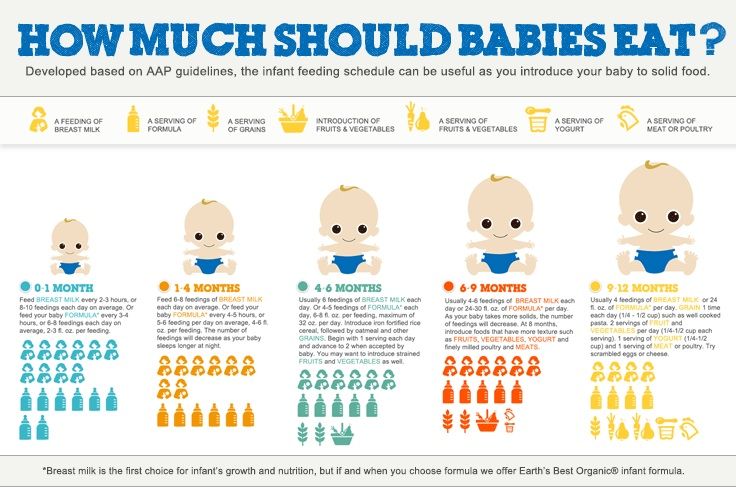 As she got older, she became much better at grabbing her breasts in normal positions,” says Sarah, mother of two from Australia.
As she got older, she became much better at grabbing her breasts in normal positions,” says Sarah, mother of two from Australia.
6. Relaxed breastfeeding after caesarean section
If you can't find a comfortable position for breastfeeding after caesarean section, 3 try to hold the baby on the shoulder while reclining - this does not put pressure on the postoperative suture and allows you to breastfeed the baby comfortably. You can also try side feeding.
7. Sitting upright breastfeeding or “koala pose”
When breastfeeding in an upright position or “koala pose”, the baby sits with a straight back and a raised head on the mother's hip. 4 This position can be tried even with a newborn if it is well supported, but it is especially convenient for feeding a grown child who can already sit up by himself. The upright sitting position, or “koala pose,” is great for toddlers who suffer from reflux or ear infections and feel better sitting. In addition, this pose may be suitable for children with a shortened frenulum of the tongue or reduced muscle tone.
In addition, this pose may be suitable for children with a shortened frenulum of the tongue or reduced muscle tone.
“When my daughter got a little older, I would often feed her in an upright position, which was more comfortable for both of us, and I could still hold her close,” recalls Peggy, a mother from Switzerland. “Besides, it was possible to discreetly breastfeed her in public places.”
8. Overhanging position
In this position, the baby lies on his back, and the mother bends over him
on all fours so that the nipple falls directly into his mouth. 4 According to some mothers, this breastfeeding position is good to use from time to time for mastitis, when touching the breast is especially unpleasant. Some say that this breastfeeding position helps with blockage of the milk ducts, although there is no scientific evidence for this yet. You can also feed in the “overhanging” position while sitting, kneeling over the baby on a bed or sofa, as well as reclining on your stomach with support on your elbows. Pillows of various sizes that you can lean on will help you avoid back and shoulder strain.
Pillows of various sizes that you can lean on will help you avoid back and shoulder strain.
“I have breastfed several times in the 'overhang' position for clogged milk ducts when no other means of dissolving the blockage worked. And this pose seems to have helped. I think it's because of gravity, and also because the breasts were at a completely different angle than with normal feeding, and my daughter sucked her differently, ”says Ellie, a mother of two from the UK.
Feeding in the "overhanging" position is unlikely to be practiced regularly, but in some cases this position may be useful.
“I used to breastfeed in the overhang position when my baby was having trouble latch-on,” says Lorna, mother of two in the UK. - This, of course, is not the most convenient way, but then I was ready for anything, if only he could capture the chest. We succeeded and have been breastfeeding for eight months now!”
9. Feeding a baby in a sling or "on the fly"
Breastfeeding in a sling takes some practice, but it can be used to go out of the house, look after older children or even do a little household chores.
The sling is also useful if the baby does not like to lie down or is often attached to the breast. Lindsey, a mother of two in the US, notes: “I used the carrier frequently for both of my children. When we were out, I tied the sarong around my neck and covered the carrier with it. Under such a cape, the baby can eat as much as he wants until he falls asleep.
This breastfeeding position is best when the baby is already good at breastfeeding and can hold his head up by himself. Any slings are suitable for breastfeeding, including elastic and rings, as well as carrying bags. Whatever option you choose, the main thing is that you can always see the face of the child, and his chin does not rest against his chest.
10. Double hand-held breastfeeding
Double hand-held breastfeeding (or “double-ball gripping”) is great for mothers of twins—you can breastfeed both at the same time while keeping your arms relatively free. 4 When feeding in this position, it is advisable to use a special pillow for breastfeeding twins, especially at first. It will provide extra support and help keep both babies in the correct position, as well as reduce the burden on the abdomen if you had a caesarean section. In addition, the hands are freer, and if necessary, you can deal with one child without interfering with the second.
It will provide extra support and help keep both babies in the correct position, as well as reduce the burden on the abdomen if you had a caesarean section. In addition, the hands are freer, and if necessary, you can deal with one child without interfering with the second.
“My twins were born very tiny and had to be fed every two hours at any time of the day or night. Very soon it became clear: if I want to do anything besides feeding, I need to feed them both at the same time, - says Emma, mother of two children from the UK. “I breastfed them two by hand using a breastfeeding pillow.”
Other good positions for breastfeeding twins are two criss-cross cradles, one baby in the cradle and the other close at hand, reclining feeding, or sitting upright (one baby on one side, the other on the other).
11. Feeding in the “hand-supported breast” or “dancer's hand” position
muscle tone (which is typical for premature babies, children suffering from various diseases or Down syndrome), try supporting his head and your chest at the same time.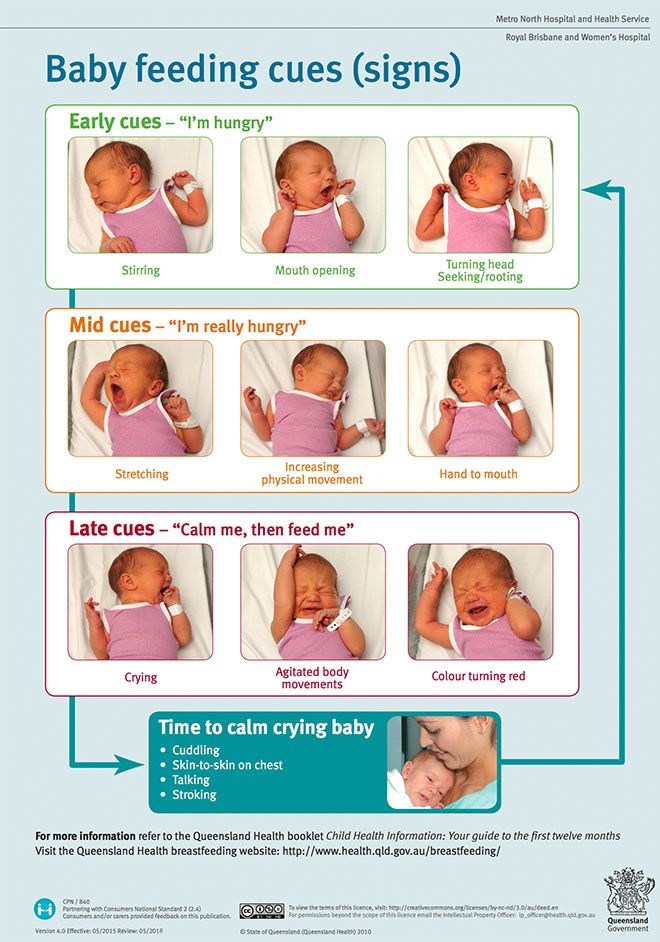 4 Grab your chest with your palm underneath so that your thumb is on one side and all the others are on the other. Move your hand slightly forward so that your thumb and forefinger form a "U" just in front of your chest. With the other three fingers, continue to support the chest. With your thumb and forefinger, hold the baby's head while feeding so that his chin rests on the part of the palm between them, your thumb gently holds the baby on one cheek, and your index finger on the other. So the baby gets excellent support, and you can control his position and see if he is holding his breast.
4 Grab your chest with your palm underneath so that your thumb is on one side and all the others are on the other. Move your hand slightly forward so that your thumb and forefinger form a "U" just in front of your chest. With the other three fingers, continue to support the chest. With your thumb and forefinger, hold the baby's head while feeding so that his chin rests on the part of the palm between them, your thumb gently holds the baby on one cheek, and your index finger on the other. So the baby gets excellent support, and you can control his position and see if he is holding his breast.
Literature
1 Colson SD et al. Optimal positions for the release of primitive neonatal reflexes stimulating breastfeeding. Early Hum Dev . 2008;84(7):441-449. - Colson S.D. et al., "Optimal Positions for Provoking Primitive Innate Reflexes to Induce Breastfeeding." Early Hume Dev. 2008;84(7):441-449.
2 UNICEF UK BFHI [ Internet ].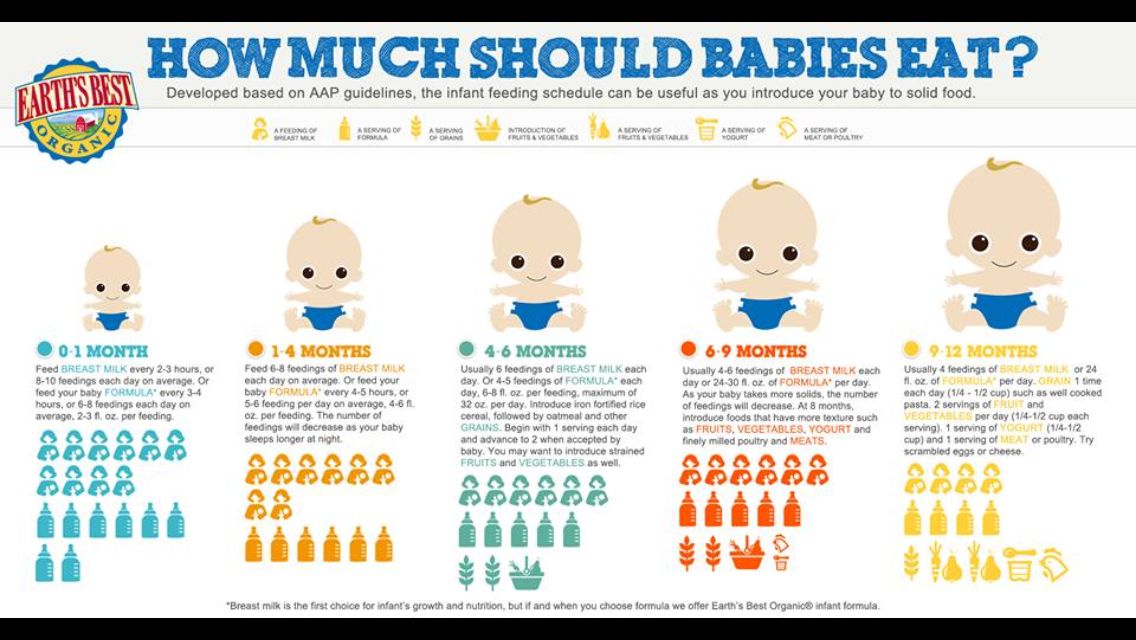

 Otherwise, they will fill up and won’t want to eat solid foods. Too much milk can also lead to iron deficiency anemia.
Otherwise, they will fill up and won’t want to eat solid foods. Too much milk can also lead to iron deficiency anemia.